Abstract
Hypertensive disorders represent some of the most common medical complications during pregnancy, but it can lead to severe complications, among which the HELLP syndrome is one of the most serious. HELLP syndrome is a rare disease that affects pregnant women and approximately 0.2-0.6% of all births.
It is considered to be a severe form of preeclampsia occurring during either the third trimester of pregnancy or the postpartum period. Approximately 4-12% of the women diagnosed with preeclampsia will develop HELLP syndrome. HELLP syndrome may affect patients as a singular disease, or it may be associated with preeclampsia. This medical condition was described for the first time in 1982, by Dr. Louis Weinstein, as distinctive from preeclampsia.
We report here the case of a 25 year old patient, 37 weeks pregnant, who was admitted to “Elena Doamna” Clinical Hospital of Obstetrics and Gynecology, Iasi, Romania, for uterine contractions, spontaneous ruptured membranes, lower-extremity edema, high blood pressure (180/115 mm Hg), and a large amount of ascitic fluid.
In order not to endanger the life of the pregnant woman and her fetus, emergency cesarian delivery was performed. Intrapartum, 3.5 Liters (L) of ascetic fluid were extracted, which were sent to the laboratory for additional investigations, along with the placenta. Postoperative abdominal drainage consisted in a total of 8.5 L of fluid within a six day period.
After a thorough clinical examination associated with the laboratory results, the presumptive diagnosis of HELLP syndrome is suspected. The patient is compatible with the profile due to the risk factors, clinical examination, laboratory results and complications she developed during the hospitalization, all of these being specific for this syndrome. During admission, several complications affected the patient’s status, but they have been all overcome by collaborating with other specialties.
Keywords:pregnancy, ascitic fluid, gestational hypertension, preeclampsia, HELLP syndrome.
INTRODUCTION
As obstetrician-gynecologist physicians, it is mandatory to follow up pregnancy as early as possible by all available “tools”, in order to avoid any potential complications that may occur during this condition. Moreover, for an appropriate monitoring of both pregnancy and mother and fetus life, a multidisciplinary approach is essential.
A pregnancy can be associated with various conditions which, according to their gravity, could endanger the life of both pregnant women and fetus if discovered late. Pregnant women are susceptible to develop most of the medical and surgical conditions specific for women of fertile age.
Considering that HELLP syndrome is a rare complication of preeclampsia and sometimes women experience worsening of gestational arterial hypertension without manifestations of preeclampsia, it is very important to monitor the health of pregnant women and furthermore, to increase patient’s awareness of the importance of attending antenatal consultations as early as possible.
MATERIALS AND METHODS
We report the case of a 25 year old patient, 37 weeks pregnant, who was admitted on 18.03.2018 to “Elena Doamna” Clinical Hospital of Obstetrics and Gynecology, Iasi, Romania, for birth assistance. The patient presented with painful uterine contractions, spontaneous ruptured membranes (the vaginal exam revealed that the cervix was 4 cm dilated), lower-extremity edema, high blood pressure (180/115 mm Hg), and a large amount of ascitic fluid revealed by ultrasound examination. In January 2018, the patient had a double-J ureteral catheter inserted to relieve a right kidney third degree ureterohydronephrosis.
Fetal monitoring is performed, showing fetal heartbeat of 130 bpm, presence of uterine contractions and a blood pressure level of 180/115 mm Hg. Laboratory tests revealed blood type and Rh factor, monocytosis, hepatic failure signs, hepatic cytolysis, anemia, low platelets, proteinuria, cholestatic syndrome, and mesenchymal inflammatory syndrome associated with pregnancy. The ultrasound examination confirms 37 weeks of pregnancy and the presence of ascitic fluid in a large amount in all four quadrants of the abdomen, including the subphrenic, perisplenic and intervesicouterine spaces.
According to clinical examination and laboratory results, the final diagnosis was made: VG VP, 37 weeks of pregnancy, single fetus, cranial presentation, spontaneous ruptured membranes, active labour, HELLP syndrome, right third degree ureterohydronephrosis. Due to the high obstetrical risk, it was decided to proceed to caesarean surgery. Intraoperative, a high amount of colorless, clear ascitic fluid is observed, 3.5 L being drained with a small sample of 20 mL sent for further laboratory investigations: cytology, biochemistry and microbiology. A female fetus, weighing 2430 g, Apgar-9 was safely delivered. A bilateral tubal ligation is also performed and a right parietocolic drain is placed. The placental consistency was tough, rugged, with multiple areas of infarction, and green colored membranes; therefore, an anatomopathological examination was requested.
Postoperatively, the patient was transferred to the Intensive Care Unit. During the first 24 hours there was a 4400 mL drainage, the laboratory results of the intraoperative ascitic fluid showing a total protein value of 0.51 g/dL, confirming the transudate type, and no cytological atypia. The microbiological tests were negative for the samples of amniotic and intraperitoneal fluids.
The pathological macroscopic examination of the placenta reveals a placental disc weighing 1170 g, measuring 13/11/3.5 cm, and presenting on the entire surface of the maternal part a large area of haemorrhage. Several white-yellow areas, located between the fetal and maternal surfaces, were found on the section. The fetal membranes were ruptured, opaque, yellow-green, with insertion at the edge of the placental disc.
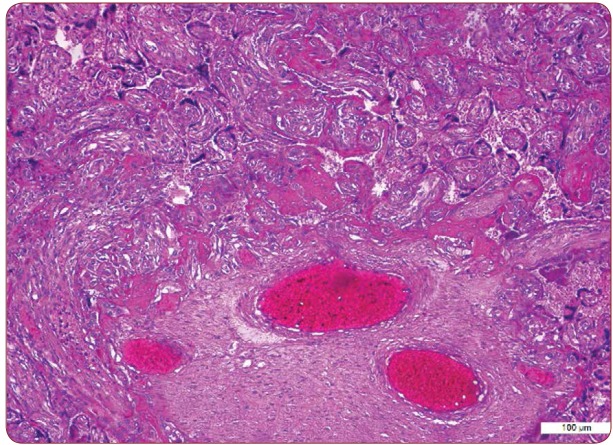
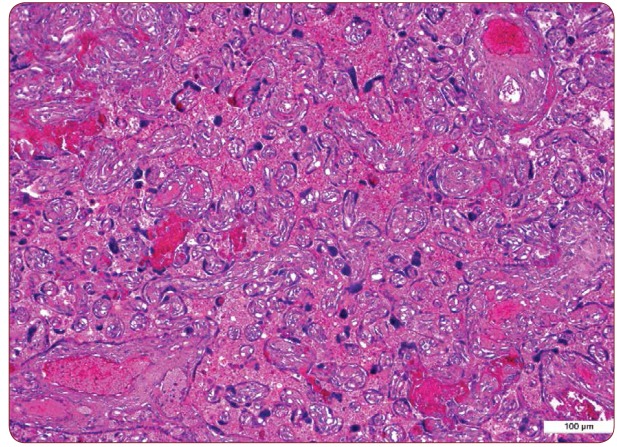
Umbilical cord has a length of 30 cm, eccentric insertion, with three vascular lumens per section, occupied by blood clots. The histopathological exam revealed vascular thrombosis (Figure 1), with dense perivillous fibrinoid, microcalcifications (Figure 2), intervillous haemorrhage, with increased syncytial knots (Figure 3), placental infarction represented by areas of is chemic villous necrosis with ghost-like villous remnants.
Although the patient had a favorable postoperative outcome, she continued to drain approximately 3150 mL of bloody ascitic fluid. Due to the significant amount of the antepartum and intrapartum fluid within the peritoneal cavity associated with diffuse postoperative pain, a surgical consultation is recommended, where no sign of peritoneal irritation was noticed.
Abdominal ultrasound revealed first degree ureterohydronephrosis of the left kidney, lumbar ureter measuring 13 mm, third degree ureterohydronephrosis of the right kidney with the presence of the double-J catheter, left pleural liquid measuring 5 mm and moderate amount of ascitic fluid. Summing up the investigations performed during the general surgery consultation the diagnosis of post-caesarean state, right third degree ureterohydronephrosis with double-J catheter, and ascites due to HELLP syndrome is set. Diuretic therapy is recommended, as well as the exclusion of other causes of ascites or the infection of the peritoneal fluid (ADA-ascites TB, cytology, cultures), and careful supervision of the abdominal-pelvic drainage.
Two days postoperative the patient’s status continues to improve, the drainage is approximately 1000 mL, and she was transferred from the ICU to the postcaesarian sector. Samples of ascitic fluid sent to the pneumophtisiology section were negative for Koch’s Bacillus infection. Six days postoperatively, the drainage decreased to 120 mL and therefore, removal of the drain tube was decided.
The preoperative and the postoperative laboratory parameters (hemolysis, hemolytic anemia, high levels of hepatic enzymes, low platelets, cholestatic syndrome and proteinuria) and the clinical examination confirm the diagnosis of HELLP syndrome. The patient receives the recommendation to have a special high-protein diet, iron supplements and vitamins. Throughout the postcaesarian period the patient maintained uncontrolled blood pressure, therefore a cardiologic consult was requested for the adjustment of chronic hypertensive treatment. Because echocardiographic parameters were within normal range, an antihypertensive treatment with blood pressure and heart rate monitoring were recommended.
The patient is also examined in the urology department, where the removal of the double-J catheter is decided through cystoscopy. After the removal of the catheter, urine culture test is performed, showing negative results for urinary infections. After a 14 days hospitalization, the patient’s status was stable, laboratory analysis results where within normal limits, blood pressure was also maintained within normal limits – therefore, the patient’s discharge was decided.
RESULTS AND DISCUSSIONS
HELLP syndrome is one of the most frequent and severe complications, which can be diagnosed both during pregnancy (between 27 and 37 weeks) and postpartum period (30% of all cases) (2), irrespective of presence or absence of preeclampsia (10-20%) (3). HELLP syndrome is characterized by the presence of hypertension disorders that creates a specific triad: microangiopathic hemolysis, hepatocytolisys syndrome, thrombocytopenia (7).
HELLP syndromeoccurs most frequently in Caucasian multiparous patients (the risk is two times higher than in nulliparous women), with higher maternal age (more than 25 years old), preeclampsia or pregnancy-induced hypertension, and a previous pregnancy with HELLP syndrome (recurrence chances of 19-27% at each birth).
HELLP syndromeoccurs most frequently in Caucasian multiparous patients (the risk is two times higher than in nulliparous women), with higher maternal age (more than 25 years old), preeclampsia or pregnancy-induced hypertension, and a previous pregnancy with HELLP syndrome (recurrence chances of 19-27% at each birth).
Most obstetricians assume that HELLP syndrome is derived from an autoimmune reaction, accompanied by platelet aggregation, endothelial dysfunction, along with innate errors in fatty acid oxidation metabolism, leading to characteristic maternal-fetal imbalance-fatty acid oxidation metabolism (1).
Patients diagnosed with HELLP syndrome have associated complications that increase the maternal risk such as cerebral haemorrhage, eclampsia, retinal detachment, fetal distress, pulmonary edema, hematoma, hepatic rupture, ascites, acute renal failure, disseminated intravascular coagulation or placental abruption, all of these being possible causes for maternal death (7).
In our case, HELLP syndrome represented an emergency situation, the medical and surgical approach being prompt and correct. Considering this pathology associated to third trimester pregnancies, caesarian operation was performed in emergency in order to decrease maternal and fetal mortality and morbidity, according to the latest guidelines.
Being a particular case (the presence of ascites in a previous pregnancy), the cytological, biochemical and infectious investigations of the ascitic fluid, as well as the macroscopic and microscopic examination of the placenta and membranes were mandatory. Intraoperative a bilateral tubal ligation was performed in order to avoid another HELLP syndrome in case another pregnancy was conceived, taking in consideration the patient’s history of ascites in her previous pregnancy, that would have been highly possible. This procedure was performed with the patient’s approval, all medical-legal issues being clearly explained to her.
Laboratory results concerning the ascitic fluid confirmed the transudate type, cytological and microbiological tests being negative. The anatomopathological examination of the placenta showed important macroscopic and microscopic modifications that are specific to preeclampsia and thus, to HELLP syndrome too. In preeclampsia, an abnormal placental structure is described due to a second trophoblastic invasion of the decidua, leading to an inadequate blood perfusion of the placenta (6). Deterioration and hypoxia of the placental tissue determines an increased production of endothelial factors that are a cause of endothelial and placental dysfunction, resulting in gestational hypertension, proteinuria and platelet aggregation (4).
During her postpartum period, the patient underwent three consultations in three different units (general surgery, cardiology, and urology) in order to establish an effective antihypertensive Complicated HELLP Syndrome with Ascites in Pregnancy Maedica A Journal of Clinical Medicine, Volume 13, No. 4, 2018 335 treatment, remove the double-J catheter and correctly diagnose the origin of ascites. The patient’s favorable outcome (physiological involution of the uterus, moderate lochia, afebrile status, blood pressure values maintained under normal parameters and laboratory results within normal limits) enabled the discharge decision. HELLP syndrome is considered a complication of preeclampsia and a rare pathology affecting 0.2-0.6% of all births. The specific risk factors – maternal age over 25, Caucasian patient, multiparous, gestational hypertension diagnosed during previous pregnancies – were identified in our patient.
Besides the presence of antepartum and postpartum ascitic fluid during the present and previous pregnancy (investigated and confirmed through clinical and paraclinical investigations and anamnestic data), the amount of fluid from the intraperitoneal cavity, both intraoperatively and postoperatively, represented an important particularity of this case.
Managing HELLP syndrome requires a third level maternity with newborn and mother intensive care units (3). Diagnosing a pregnant patient with a 32 or more weeks of gestational age with HELLP syndrome is an indication for caesarian operation in order to avoid materno-fetal risks (3).
The effects of HELLP syndrome upon the newborn are significant; therefore, early risk recognition may help the doctor to establish proper conditions for deliverance, lowering the mortality and morbidity rates (2). Materno-fetal complications lead to a perinatal mortality of 7-70% and a rate of maternal mortality of 1-24% (5). In this regard, an important role in decreasing maternal mortality and morbidity caused by hypertension disorders during pregnancy and also in improving maternofetal prognostic is assigned to a correct and prompt diagnosis and treatment of HELLP syndrome as well as to a multidisciplinary aggressive approach and guiding of such patients towards experienced obstetrical centers (5).
CONCLUSIONS
HELLP syndrome is considered to be a complication of preeclampsia and a rare pathology. Besides the characteristic risk factors and clinical context, our case also presented, both intra- and postoperatively, a large amount of ascitic fluid as a peculiarity of this syndrome. Considering the serious materno-fetal consequences of this syndrome, a correct and early diagnosis as well as an appropriate therapy by using a multidisciplinary approach are required, with positive effects on the prognosis of both mother and fetus.
Conflicts of interest: none declared.
Financial support: none declared.
FIGURE 1.
Placenta with vascular thrombosis and perivillousfibrinoid, HE x 10
FIGURE 2.
Placenta with dense perivillous fibrinoid and microcalcifications, HE x 10
FIGURE 3.
Placenta with intervillous haemorrhage and proeminent syncytial knots, HE x 10
Contributor Information
Diana POPOVICI, 3rd Clinic of Obstetrics and Gynecology, Mother and Child Health Department, “Gr. T. Popa” University of Medicine and Pharmacy, Iasi, Romania.
Eduard CRAUCIUC, 3rd Clinic of Obstetrics and Gynecology, Mother and Child Health Department, “Gr. T. Popa” University of Medicine and Pharmacy, Iasi, Romania.
Raluca-Ancuta TIPERCIUC, ”Elena Doamna” University Hospital of Obstetrics and Gynecology, Department of Obstetrics and Gynecology, Iasi, Romania.
Georgiana-Alexandra BUZNEA, ”Elena Doamna” University Hospital of Obstetrics and Gynecology, Department of Obstetrics and Gynecology, Iasi, Romania.
Mona AKAD, ”Elena Doamna” University Hospital of Obstetrics and Gynecology, Department of Obstetrics and Gynecology, Iasi, Romania.
Loredana HURJUI, Morpho-Functional Sciences Department, University of Medicine and Pharmacy, Iasi, Romania.
Raluca BALAN, Morpho-Functional Sciences Department, University of Medicine and Pharmacy, Iasi, Romania.
REFERENCES
- 1.Aloizos S, Seretis C, Liakos N, Aravosita P, Mystakelli C, Kanna E, Gourgiotis S. HELLP syndrome: understanding and management of a pregnancy-specific disease. J Obstet Gynaecol. 2001;4:331–337. doi: 10.3109/01443615.2013.775231. [DOI] [PubMed] [Google Scholar]
- 2.Barnhart Lynette. HELLP Syndrome and the Effects on the Neonate. Neonatal Network. 2015;5:269–273 . doi: 10.1891/0730-0832.34.5.269. [DOI] [PubMed] [Google Scholar]
- 3.Beucher G, Simonet T, Dreyfus M. Management of HELLP syndrome. Gynecol Obstet Fertil. 2008;12:1175–1190. doi: 10.1016/j.gyobfe.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 4.Maureen O’Hara Padden. LCDR, MC, USN, Naval Hospital, Camp Pendleton, California. Am Fam Physician. 1999;3:829–836. [Google Scholar]
- 5.Pokharel SM, Chattopadhyay SK, Jaiswal R, Shakya P. HELLP syndrome-a pregnancy disorder with poor prognosis. Nepal Med Coll J. 2008;4:260–263. [PubMed] [Google Scholar]
- 6.Johnson Traci C. “HELLP Syndrome”. National Center for Advancing Translational Sciences, Genetic and Rare Diseases Information Center: . 2017; [Google Scholar]