Abstract
Osteoporosis and its associated fragility fractures are becoming a severe burden in the healthcare system globally. In the Asian-Pacific (AP) region, the rapidly increasing in aging population is the main reason accounting for the burden. Moreover, the paucity of quality care for osteoporosis continues to be an ongoing challenge. The Fracture Liaison Service (FLS) is a program promoted by International Osteoporosis Foundation (IOF) with a goal to improve quality of postfracture care and prevention of secondary fractures. In this review article, we would like to introduce the Taiwan FLS network. The first 2 programs were initiated in 2014 at the National Taiwan University Hospital and its affiliated Bei-Hu branch. Since then, the Taiwan FLS program has continued to grow exponentially. Through FLS workshops promoted by the Taiwanese Osteoporosis Association (TOA), program mentors have been able to share their valuable knowledge and clinical experience in order to promote establishments of additional programs. With 22 FLS sites including 11 successfully accredited on the best practice map, Taiwan remains as one of the highest FLS coverage countries in the AP region, and was also granted the IOF Best Secondary Fracture Prevention Promotion award in 2017. Despite challenges faced by the TOA, we strive to promote more FLS sites in Taiwan with a main goal of ameliorating further health burden in managing osteoporotic patients.
Keywords: Asia-Pacific region, Taiwan, Fracture Liaison Service, Best Practice Framework, Osteoporosis
1. Introduction
Osteoporosis remains one of the most common bone disease encountered worldwide. It is primarily characterized by bone mass reduction and bone quality deterioration, and increased risks bone fragility and/or fracture [1]. The aging population is being recognized widely as a serious health burden in the 21th century, especially in the Asian-Pacific (AP) region due to the enormous population base [2]. In 2004, the World Health Organization estimated that osteoporosis would cause approximately 9 million fracture incidents worldwide, with 2.5 millions & 1.6 millions in the Western Pacific and Southeast Asia, respectively [2]. In fact, it is projected about half of the hip fracture occurring worldwide will be further identified in Asia [3,4].
Although osteoporosis and its associated fragility fractures continue to pose a heavy health care burden, their lack of quality care remains prominent in the AP region. Previous study demonstrated that only less than one-third of the patients with fragility fracture worldwide received a comprehensive osteoporotic evaluation and the proper treatments [5].
The lifetime fracture risks in either vertebrate, hip, or waist are 33% and 20% for female and male in Taiwan, respectively [6,7]. The hip fracture year-incidence rate in Taiwan is being recognized as one of the highest in the world, being 392/100,000 and 196/100,000 in female and male, respectively [6]. In fact, the 1-year mortality rate after a hip fracture was found to be 15% in female, and 22% in male in 2002 [6]. These figures somewhat improved in 2009 to 11% in female, and 18% in male [8]. The Asia-gap study conducted in 2007 showed that in hip fractures, while 70% of the patients themselves were aware that they had osteoporosis, only 25% were evaluated with a bone mineral density (BMD), and 30% received the proper medications to treat osteoporosis [9].
In 2013, as an effort to provide better care for osteoporosis, the International Osteoporosis Foundation (IOF) advocated Capture the Fracture campaign in order to raise awareness on secondary fracture prevention [5]. Fracture Liaison Service (FLS) is promoted as a coordinated, multidisciplinary program that not only helps identify but also treat fracture patients systematically [5]; In addition, the IOF also constructed the Best Practice Framework (BPF) with thirteen specific standards providing reference guidance for institutions to follow and implement in their individualized FLS programs [5]. These FLS programs have shown be cost-effective [10], and to improve both secondary fracture incidence [11] and mortality rates [11].
The first 2 FLS programs in Taiwan were established at the National Taiwan University Hospital Healthcare System in 2014. Subsequently, the number FLS programs providing care for osteoporotic patients continued to increase rapidly nationwide. As of March 2018, there were a total 22 FLSs in Taiwan with 11 being accredited on the Map of Best Practice. More details regarding these FLS sites can be found on the Capture the Fracture website (http://capturethefracture.org/map-of-best-practice). This review article focuses on the development of FLS network in Taiwan.
2. The National Taiwan University Hospital Healthcare System fracture liaison program
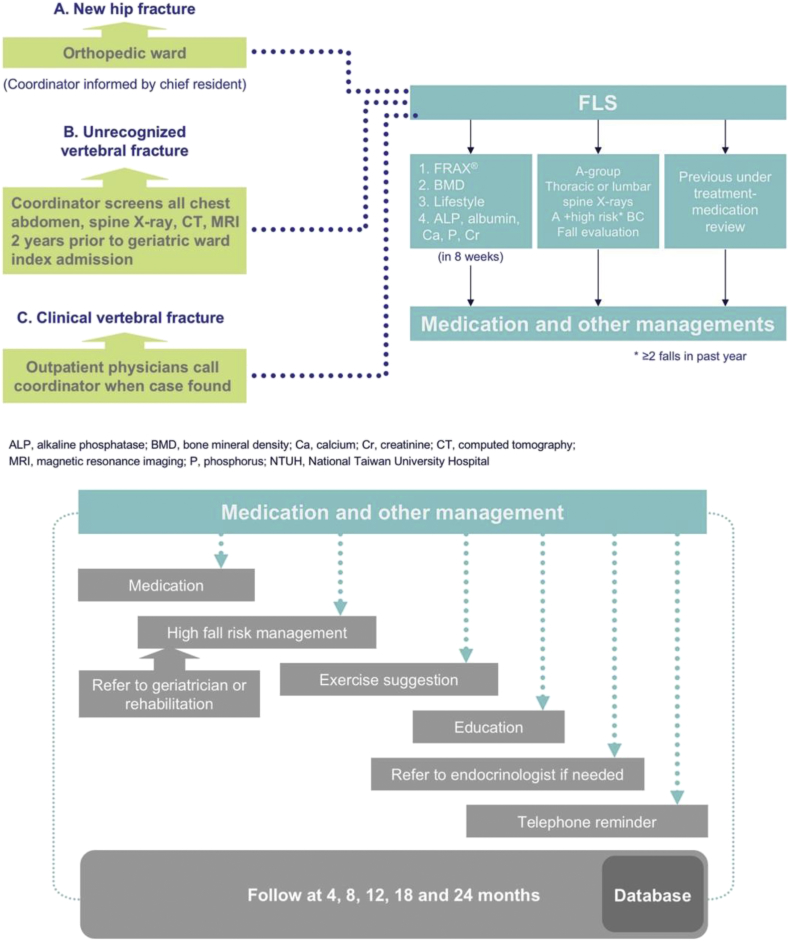
Established in 2014, the first FLS program Taiwan was developed by the National Taiwan University Hospital (NTUH) with its model being served as the primary framework for many other similar fracture caring programs which later ensued. The FLS initially operated as a research project at both NTUH and its affiliated branch in Bei-Hu. Clinical cases were evaluated from both inpatient and outpatient settings at our main branch. Bei-Hu branch, on the other hand, employed the same study protocol but only involved recruitments from outpatient setting because it lacks an Emergency Department or orthopedic/trauma ward. The flow-chart from the NTUH FLS model is demonstrated in Fig. 1.
Fig. 1.
The flow chart of National Taiwan University Hospital fracture liaison service model. FLS, fracture liaison service.
The NTUH model consists of patients from 3 groups: Those newly diagnosed hip fractures from orthopedic ward (group A), previously unrecognized vertebral compression fractures from the geriatrics ward (group B), and clinical vertebral compression fractures without previous treatment from the outpatient clinic setting (group C).
Evaluation is based on the Taiwanese Guidelines for the Prevention and Treatment of Osteoporosis published by the Health Promotion Administration and The Taiwanese Osteoporosis Association (TOA) [6]. According to the guideline, fragility fracture patients should receive multifaceted evaluation within eight weeks after identification. They include the following: Estimation of 10-year fracture risk by FRAX (fracture risk assessment tool), BMD, evaluation of life style behaviors (amount of supplemental calcium and vitamin D3 intake, protein intake, exercise, smoking, and alcohol, etc.), fall risk assessment & prevention, and blood test to screen for possible underlying secondary endocrine causes osteoporosis. If the patient has received prior treatment for osteoporosis, evaluation of the medication dosage, side effects, compliance, and contraindications were also carefully analyzed. Case coordinators would also provide a comprehensive education on the disease of osteoporosis, its treatment involving medications or other nonpharmcological management options to participants of our program when indicated.
Telephone conversations and outpatient interviews were conducted at 4th, 8th, and 12th months from enrollment. Case managers involve interactions with the patient to provide education regarding osteoporosis as well as review of medication dosage, side effects, adherence, and monitoring for possible new falls, fractures, if applicable. Upon completion of the twelfth month interview, subsequent long-term osteoporosis follow-up process is implemented. The follow-up period then extends to every 6 months in the second year then annually up to a total of ten years. The FLS database is then meticulously collected for further analysis.
3. The development of FLS network in Taiwan
In 2015, both programs were accredited by IOF on the Map of Best Practice (NTUH main branch awarded Gold, and the Bei-hu branch awarded Silver). Subsequently, several other medical centers in Taiwan have cooperated with NTUH with similar protocol and flowchart in hopes of establishing mutual database. The National Yang-Ming University Hospital, on the other hand, has designed their own protocol but is collaborating with NTUH programs by sharing of their clinical experience.
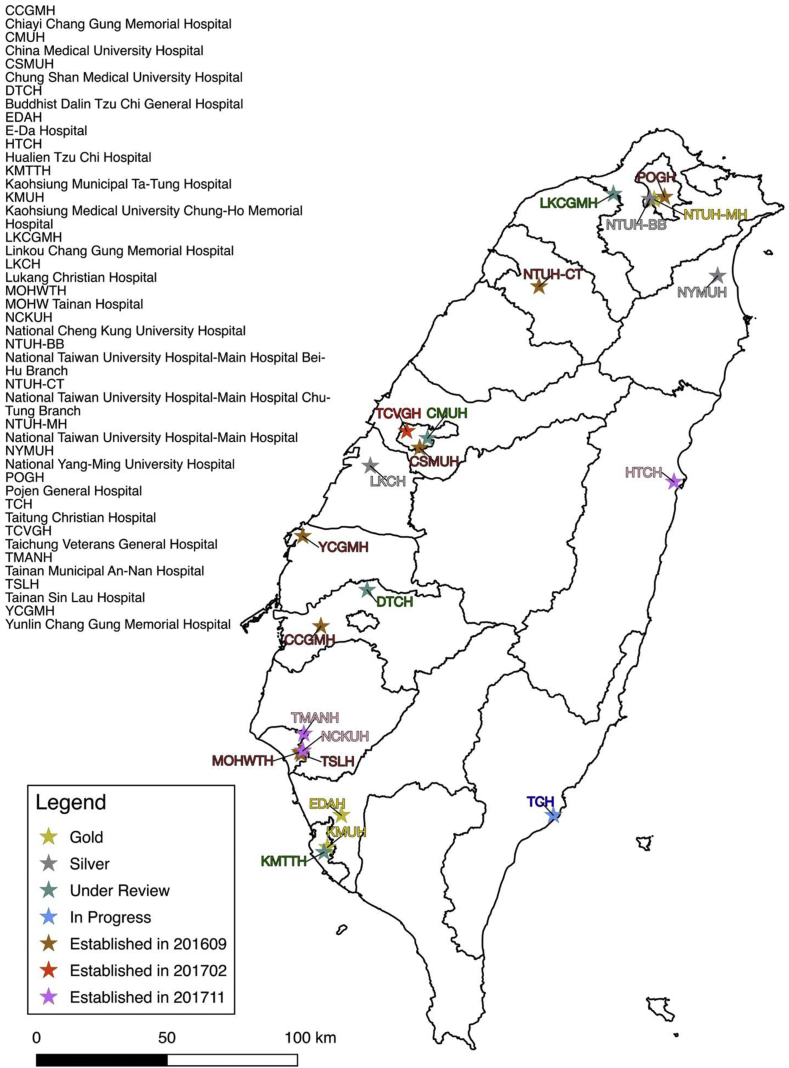
In 2016, the TOA started hosting serial workshops with a primary goal to promote further FLS expansion in Taiwan. The first workshop was held in September 2016, where experts from the 2014–2015 programs were invited to act as clinical instructors and coordinators to share their experience with corresponding mentee institutes. After this meeting, 12 additional institutions started to develop their own FLS programs (n = 18, Fig. 2). TOA at that time also encouraged all established programs to aim for the best practice recognition whenever possible. The second workshop was later held in January 2017. All new programs were invited to discuss their interim progress along with comments provided by experienced mentors. Obstacles and challenges encountered were also discussed. Consequently, a new program (Taichung Veterans General Hospital) joined (n = 19, Fig. 2). Efforts of TOA were well recognized by IOF at the 2017 World Congress for Osteoporosis, Osteoarthritis and Musculoskeletal Diseases held in Florence and granted the Best Secondary Fracture Prevention Promotion award. The third workshop was held in September 2017. Besides sharing clinical experience, one of the main theme at this workshop was to display close interactions between health care providers and patients at osteoporosis promotion events held at each participating hospital. During that time, 3 additional programs (Hualien Tzu Chi Hospital, National Cheng Kung University Hospital, and Tainan Municipal An-Nan Hospital) joined the network. As of March 2018, a total of 22 FLSs were established in Taiwan. Among them, 11 were accredited on the Map of Best Practice (3 gold, 4 silver, 1 bronze, 2 currently under-review, 1 in-progress) (Fig. 2). Considering the relatively small population size of the island itself [12] (ca. 23.5 million, 2016), Taiwan probably has the highest density of the FLS programs in the AP region.
Fig. 2.
Taiwan Fracture Liaison Service (FLS) Map in Mar., 2018 (FLS sites = 22). The progress after 3 Taiwanese Osteoporosis Association workshops was shown as well.
Despite the BPF being successfully implemented in Taiwan as well as other AP region countries, there remains some challenged faced in the region due to limitations set by certain unique characteristics in the healthcare systems which in turn fail to meet certain standards listed by the original BPF. As a result, the TOA held the Consensus Meeting for the Best Practice Framework Standards for Fracture Liaison Service in the Asia-Pacific Region in October 2017 in Taipei Taiwan. At both experts around the AP region and representative from IOF were invited. The original thirteen standards of BPF were reviewed and some minor modifications to better accommodate the unique AP population [13].
4. Characteristics of FLSs in Taiwan
Among the 11 IOF accredited programs listed from the BPF map, we managed to acquire individual accreditation application questionnaire from 9 of them. A summary of 9 IOF accredited FLS programs in Taiwan is shown on Table 1.
Table 1.
Summary of 9 International Osteoporosis Foundation accredited fracture liaison services in Taiwan.
| Name | Service population size | Year FLS started | Past 12 months new FLS patients | Institute type | FLS coordinator | Patient identification restriction | DXA availability | DXA restriction |
|---|---|---|---|---|---|---|---|---|
| National Taiwan University Hospital | ca. 8,000,000 | 2014 | 407 | Teaching/university | Researcher | ≥50 yr; hip or vertebral fracture only | Yes | Nontraumatic fracture |
| Buddhist Dalin Tzu Chi General Hospital | ca. 350,000 | 2014 | 655 | Private not for profit | Dedicated coordinator | No | Yes | Nontraumatic fracture |
| National Taiwan University Hospital Bei-Hu Branch | ca. 100,000 | 2014 | 40 | District | Dedicated coordinator | ≧50 yr; vertebral fracture only | Yes | Nontraumatic fracture |
| Linkou Chang Gung Memorial Hospital | ca. 2,117,000 | 2015 | 107 | Teaching/University | Dedicated coordinator | ≥50 yr; hip or vertebral fracture only | Yes | ≥50 yr or postmenopausal women; hip or vertebral fracture only |
| Kaohsiung Medical University Chung-Ho Memorial Hospital | ca. 300,000 | 2015 | 150 | Teaching/University | Researcher | ≥50 yr; hip or vertebral fracture only | Yes | Nontraumatic fracture |
| China Medical University Hospital | ca. 100,000 | 2015 | 130 | Teaching/University | Dedicated coordinator | ≥50 yr | Yes | No |
| E-Da Hospital | ca. 1,000,000 | 2016 | 2849 | Teaching/University | Dedicated coordinator | No | Yes | No |
| Taitung Christian Hospital | ca. 223,000 | 2016 | 42 | Private not for profit | Clinician | ≥50 yr; hip fracture only | Yes | ≥50 yr; hip or vertebral fracture only |
| Lukang Christian Hospital | ca. 75,000 | 2016 | 1318 | District | Dedicated coordinator | ≥50 yr; hip or vertebral fracture only | Yes | ≥18 yr |
FLS, fracture liaison service; DXA, dual-energy x-ray absorptiometry.
Most IOF accredited FLS programs in Taiwan are currently established at Teaching Hospitals/University Medical Centers. They are supported under research program grants along with well-trained FLS coordinators who are dedicated to providing best possible service to osteoporotic patients. Programs vary significantly from one another in terms in numbers of patients recruited (n = 40–2849). However, some programs have a relatively small sample size (e.g., n = 40 for NTUH Bei-Hu) when submitted data. All of the 9 accredited FLS programs have at least one dual-energy x-ray absorption (DXA) machine in the institute to facilitate BMD evaluation. However, most programs are limited to enrollment of patients with either hip or vertebra fractures because the Taiwanese National Health Insurance (NHI) only reimburse medications for those patients who have already suffered from either one of these two types of fracture. By analyzing the map (Fig. 2) and the summary table (Table 1), we found that those patients residing on the western part of the main island of Taiwan have relatively adequate FLS coverage; but those living on the offshore islands or eastern Taiwan are at a disadvantage due to the lack of support and access to FLSs.
5. Challenges in implementing FLSs in Taiwan
Although the numbers of FLS center have increased exponentially in Taiwan throughout 5 years, there continues to be many difficulties and challenges faced by many hospitals. The Taiwanese NHI, while compulsory but at the same time offers accessible social health insurance to patients, covers over 99% of our population [6]. Unfortunately, it does not provide reimbursement for FLS coordination fees. More importantly, regulations set by the Taiwanese NHI for reimbursements of DXA and osteoporosis medications are much stricter than those suggested by National guideline recommended by the academic society (e.g., reimbursements are provided only restricted to either hip or vertebral fractures not other type of fragility fractures) [6]. Lack of funding is considered one of the biggest obstacles for not only initiation but also maintenance of FLS programs Many programs have taken the advantage of research grants or sponsorship offered by certain pharmaceutical companies to initiate their programs. However, those funding are often limited and only temporary. In fact, several FLS programs in 2015 were forced to cease enrolment of new patients due to the lack of funding. Some programs compromise by using coordinators who were initially employed and reimbursed by NHI to manage other tasks such as diabetes mellitus. Consequently, these programs are unable to enrol more patients because coordinators are faced with multiple job obligations. In order to integrate FLS as part of a routine healthcare services, TOA is currently negotiating with the Department of Health and Welfare to obtain additional payment scheme from NHI to fund several pilot FLS programs. In order to have a better understanding of benefits to be gained from FLS programs, more randomized studies are required. Some programs have already begun enroll patients in RCT designed studies, with outcomes to be published in near future.
6. Conclusion
The number of FLS programs has been growing rapidly in Taiwan over the past 5 years and their established network is being recognized internationally. With an increasingly aging population not only found in Taiwan but also worldwide, implementing successful FLSs is crucial to provide postfracture care, prevent secondary fracture, and therefore a better quality of life for patients. It will also hopefully help us achieve the ultimate goal of lightening the extraordinary health burden imposed by fragility osteoporotic fracture.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgments
The authors would like to thank all the coordinators who have not only dedicated their hard work but also devoted endless hours to the FLS program: Ms. Dicha Wang, Ms. Chian-Hei Hong, Ms. I-Shan Lee, Ms. Min-Ru Yang, Ms. Feng-Chu Yen, Ms. Yen-Tzu Lee, Ms. Fang-Ju Lin, Ms. I-Fen Hsu, Ms. Ya-Ru Chang, and Ms. Tzu-Jung Chiu. The authors also thank Dr. Chuck Huang for English editing.
Some contents were modified based on reference obtained from the “Development of Fragility Fracture Liaison Service Network in Taiwan” article first published from the Formosan Journal of Medicine (2018); 22(2):152-60 with permission. (Content in Chinese).
Footnotes
Peer review under responsibility of The Korean Society of Osteoporosis.
Contributor Information
Rong-Sen Yang, Email: rsy0819@gmail.com.
Chih-Hsing Wu, Email: paulo@mail.ncku.edu.tw.
Ding-Cheng Chan, Email: dingchengchan@ntu.edu.tw.
References
- 1.NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy Osteoporosis prevention, diagnosis, and therapy. J Am Med Assoc. 2001;285:785–795. [Google Scholar]
- 2.World Health Organization . World Health Organization; Geneva (Switzerland): 2017. WHO Scientific Group on the assessment of osteoporosis at primary health care level. Summary meeting report. Brussels, Belgium, 5–7 May 2004. [Google Scholar]
- 3.Mithal A., Ebeling P., Kyer C. International Osteoporosis Foundation; Nyon (Switzerland): 2013. The Asia-Pacific regional audit: epidemiology, costs & burden of osteoporosis in 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheung C.L., Ang S.B., Chadha M., Chow E.S., Chung Y.S., Hew F.L. An updated hip fracture projection in Asia: the Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia. 2018;4:16–21. doi: 10.1016/j.afos.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akesson K., Marsh D., Mitchell P.J., McLellan A.R., Stenmark J., Pierroz D.D. Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013;24:2135–2152. doi: 10.1007/s00198-013-2348-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health Promotion Administration . Health Promotion Administration; Taipei (Taiwan): 2015. National health research institutes, the taiwanese osteoporosis association. Taiwan osteoporosis practice guidelines. [Google Scholar]
- 7.Hwang J.S., Chan D.C., Chen J.F., Cheng T.T., Wu C.H., Soong Y.K. Clinical practice guidelines for the prevention and treatment of osteoporosis in Taiwan: summary. J Bone Miner Metabol. 2014;32:10–16. doi: 10.1007/s00774-013-0495-0. [DOI] [PubMed] [Google Scholar]
- 8.Wang C.B., Lin C.F., Liang W.M., Cheng C.F., Chang Y.J., Wu H.C. Excess mortality after hip fracture among the elderly in Taiwan: a nationwide population-based cohort study. Bone. 2013;56:147–153. doi: 10.1016/j.bone.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Kung A.W., Fan T., Xu L., Xia W.B., Park I.H., Kim H.S. Factors influencing diagnosis and treatment of osteoporosis after a fragility fracture among postmenopausal women in Asian countries: a retrospective study. BMC Wom Health. 2013;13:7. doi: 10.1186/1472-6874-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu C.H., Kao I.J., Hung W.C., Lin S.C., Liu H.C., Hsieh M.H. Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int. 2018 Feb 19 doi: 10.1007/s00198-018-4411-2. [DOI] [PubMed] [Google Scholar]
- 11.Wu C.H., Tu S.T., Chang Y.F., Chan D.C., Chien J.T., Lin C.H. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone. 2018;111:92–100. doi: 10.1016/j.bone.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 12.Yuan Executive. Government Information Office; Taipei (Taiwan): 2016. The Republic of China yearbook. [Google Scholar]
- 13.Chan D.D., Chang L.Y., Akesson K.E., Mitchell P., Chen C.H., Michael Lewiecki E. Consensus on best practice standards for fracture liaison service in the Asia-Pacific region. Arch Osteoporos. 2018;13:59. doi: 10.1007/s11657-018-0463-3. [DOI] [PubMed] [Google Scholar]