Abstract
This study tests competing models of the relation between depression and polysubstance use over the course of adolescence. Participants included a nationwide sample of adolescents (N=3,604), ages 12 to 17 at study Wave 1, assessed annually for 3 years. Models were tested using cohort-sequential latent growth curve modeling to determine whether depressive symptoms at baseline predicted concurrent and age-related changes in drug use, whether drug use at baseline predicted concurrent and age-related changes in depressive symptoms, and whether initial levels of depression predicted changes in substance use significantly better than vice versa. The results suggest a transactional model such that early polysubstance use promotes early depressive symptoms, which in turn convey elevated risk for increasing polysubstance use over time, which in turn conveys additional risk for future depressive symptoms, even after accounting for gender, ethnicity, and household income. In contrast, early drug use did not portend risk for future depressive symptoms. These findings suggest a complicated pattern of interrelations over time and indicate that many current models of co-occurring polysubstance use and depressive symptoms may not fully account for these associations. Instead, the results suggest a developmental cascade, in which symptoms of one disorder promote symptoms of the other across intrapersonal domains.
Adolescence is a critical period for the development of myriad psychological symptoms and disorders. Alongside this rise in pathology is a parallel increase in both the initiation and the escalation of drug use. Among eighth graders, 21% of students report having used an illicit drug; by the age of 18, this figure more than doubles, with nearly 50% of youth stating they have taken one or more illicit drugs (Johnston, O’Malley, Bachman, & Schulenberg, 2011). Drug use during this period of development is particularly troubling given its strong developmental continuity and association with multiple deleterious consequences. Specifically, a large proportion of drug-using adolescents will continue to use drugs into their early adult years and beyond, and are two to five times more likely to develop disorders of abuse and dependence (Lynskey, Coffey, Degenhardt, Carlin, & Patton, 2003). Adolescent polysubstance use, or using multiple classes of drugs over a discrete period, may portend increased vulnerability to a variety of negative mental and physical health outcomes. Polysubstance users are more likely than their single-substance using peers to engage in problematic drug use, relapse from drug treatment, and evidence serious mental illness in adulthood (Barnett et al., 2007; Ciesla, 2010; Trenz et al., 2012). Thus, understanding the trajectory of polysubstance use over this period and identifying factors associated with this progression has substantial implications for health across the life span.
Depressive symptoms are one factor consistently associated with illicit drug use in adult and adolescent populations. A recent review of substance use and internalizing disorders in children found estimates of comorbidity that ranged from 9% to 48% (O’Neil, Connor, & Kendall, 2011). Rates of depressive symptoms among adolescent polysubstance users may be even higher. Research suggests that using a variety of substances, regardless of the frequency of this use, may confer specific risk for depressive symptoms and suicidality compared to single-substance use (Conway et al., 2013; Kandel, Davies, Karus, & Yamaguchi, 1986). Co-occurring depressive symptoms and substance use are linked also to a host of physical health outcomes, including elevated physical symptoms, self-injury, and suicide (Fergusson, Horwood, & Swain-Campbell, 2002; Lewinsohn, Rohde, & Seeley, 1995, 1998). Further, co-occurring depressive symptoms impact the course of substance use treatment and recovery, leading to slower recoveries and increasing the likelihood of relapse following interventions (Rohde, Clarke, Lewinsohn, Seeley, & Kaufman, 2001; White et al., 2004). To develop targeted intervention and prevention efforts, we need a clearer understanding of the processes associated with the development of these co-occurring symptoms and behaviors, as well as how these interrelated symptoms affect each other longitudinally. To date, however, the temporal relation between drug use and depressive symptom development remains uncertain (for a review, see O’Neil et al., 2011).
Temporal Precedence of Depressive Symptoms and Substance Use
Many of the earliest theories regarding the relation between psychopathology and substance use suggest that depressive symptoms precede increases in substance use (e.g., Wilker, 1948). These negative reinforcement theories of drug use etiology suggest that substance use problems result from behavioral attempts to use substances to remove aversive stimuli (i.e., depressive symptoms). For example, the negative affect regulation model proposes that individuals use drugs to cope with existing depressive symptoms. Specifically, this model posits that adolescents experiencing depressive symptoms may attempt to avoid these distressing feelings and improve their mood by engaging in illicit substance use (e.g., Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Cooper, 1994; Cooper, Frone, Russell, & Mudar, 1995). Thus, according to these models, initiation of substance use functions as a method for decreasing depressive symptoms; the alleviation of negative affect in turn serves to reinforce and maintain the substance use.
In support of key components of these models, recent research on motivation to use substances found that coping with negative affect significantly predicted dependence and drug-related problems, controlling for age, sex, frequency and duration of use, and other motives for use (Fox, Towe, Stephens, Walker, & Roffman, 2011). Further evidence for this temporal model comes from findings that depressive symptoms during early adolescence predict increases in substance use over the course of development (e.g., Mason, Hitchings, & Spoth, 2007; Repetto, Zimmerman, & Caldwell, 2008; Saules et al., 2004); however, this relation may be complicated by other factors, such as gender. For instance, this pattern held for girls only in Mason et al.’s (2007) findings, and for boys only in the Repetto et al. (2008) study.
Conversely, other theories of drug use suggest that initial substance use may increase risk for the development of depression. Specifically, repeated substance use over time may engender physiological changes, including increases in depressed mood and negative affect. For instance, the opponent process model of addiction predicts that individuals who experiment with substances experience an immediate boost in positive feelings (the “appetitive process”), followed by a slow decrease in mood (the “opponent process”) that returns the users to their baseline mood. After repeated substance use, the opponent process becomes stronger than the appetitive process, yielding a net negative effect on mood over time (for a review, see McCarthy, Curtin, Piper, & Baker, 2010). This negative physiological effect is compounded by the association between substance use and multiple adverse long-term outcomes, including increased problems with peers, family interactions, and academic performance, all of which predict further increases in depressive symptoms (Newcomb & Bentler, 1988). Opponent process theories would therefore hypothesize that substance use during early adolescence would predict increases in depressive symptoms over development.
Support for this model comes largely from adult populations; however, there is limited evidence for this model among adolescent populations. Cross-sectional research on adolescents with dual diagnoses suggests that substance use disorders are typically diagnosed prior to depressive disorders (e.g., Brook, Cohen, & Brook, 1998; Fergusson, Boden, & Horwood, 2009, 2011; Windle & Windle, 2001). Further, a prospective study by Stice, Burton, and Shaw (2004) examining adolescent girls over the course of 5 years found that substance abuse was a significant risk factor for the onset of depression across waves (while the reverse relation did not appear to hold). However, studies that examine the pattern of emerging disorders on the symptom level have been far less consistent (e.g., Fleming, Mason, Mazza, Abbott, & Catalano, 2008; Hesselbrock & Hesselbrock, 1997).
Finally, some recent research has suggested there may be a reciprocal relation between these disorders, such that increases in the symptoms of one disorder increases the likelihood of the other simultaneously (e.g., Chinet et al., 2006; Marmorstein, 2009). Synchronous increases in symptoms of both substance use and depressive symptoms may point to the existence of multiple pathways to the development of comorbid conditions. Alternatively, a strong but non-directional (i.e., correlational) relation between age-related increases in both symptom clusters may indicate a common underlying vulnerability (e.g., genetic diathesis) or third-variable explanation that simultaneously increases risk for developing symptoms of both disorders. In support of the nondirectional model, a small number of researchers have found simultaneous increases in drug use and depression (e.g., Fleming et al., 2008; Needham, 2007); however, replication of these findings is needed.
Thus far, the preponderance of studies examining these relations have looked at temporal relations between depressive symptoms and single-substance use. To our knowledge, only one study has examined the prospective relations between depressive symptoms and polysubstance use. Trudeau, Spoth, Randall, and Azevedo (2007) examined a treatment sample of rural adolescents and found that baseline internalizing symptoms predicted age-related changes (slope) in pastmonth polysubstance use for girls but not for boys. However, these results are limited in their generalizability because the authors utilized a treatment sample, looked only at pastmonth polysubstance use, and used a single subscale from a larger assessment to measure internalizing symptoms.
Predictors of the Developmental Course of Comorbid Symptoms
Further complicating our understanding of the progression of co-occurring polysubstance use and depressive symptoms is evidence that the temporal course of these disorders may be contingent on other factors, including gender, ethnicity, and family socioeconomic status. Gender has long been understood to play an important role in the onset and course of both depressive symptoms and substance use across development. Specifically, boys and girls have similar, low rates of depression during childhood; during adolescence, however, rates of depressive symptoms increase disproportionately for girls relative to boys (Kofler et al., 2011; Twenge & Nolen-Hoeksema, 2002). Gender differences are also found in rates of substance use, wherein adolescent boys have higher rates of substance use overall and evince steeper age-related increases in their pattern of use (Chen & Jacobson, 2012; Johnston et al., 2011). The effect of gender on the developmental course of each disorder in the context of the other (e.g., the pattern of substance use controlling for depressive symptoms and vice versa) is inconsistent and less well understood. For example, Deykin, Buka, and Zeena (1992) reported that, among their sample of 223 adolescents aged 15 to 19 currently in treatment for illicit drug use, girls endorsed higher initial levels of depressive disorders and were more likely to be diagnosed with a depressive disorder preceding a diagnosis of substance misuse. The authors found the reverse trend among males. Conversely, Stice et al. (2004) studied prospective relations between depression and substance use disorders in a community sample of female adolescents ages 11–15 at baseline and found substance abuse predicted subsequent onset of depression (with only a weak relation in the reverse direction). Consistent with findings from Tradeau et al. (2007) reviewed above, another sample of older female adolescents (ages 17–19) also found prior substance use increased risk for depression (Rao, Daley, & Hammen, 2000). Clark et al. (1997) found that the temporal sequencing of depression and substance use in an adolescent clinical sample showed a unidirectional pattern only in male adolescents (substance use preceding depression), while female adolescents evidenced bidirectional relations. However, results from a younger sample of children, ages 9 to 16, suggest that the developmental course of each disorder was similar in both genders, despite mean differences in the frequency of substance use and the severity of depression symptoms for boys and girls (Costello, Angold, & Keeler 1999; Hallfors, Waller, Bauer, Ford, & Halpern, 2005; Waller et al., 2006). More systematic research on the effects of gender on the temporal sequencing of these co-occurring conditions is clearly warranted.
Even less is known about the role of other demographic factors such as ethnicity and family socioeconomic status in the development of co-occurring substance use and depressive symptoms. There is, however, evidence specific to each disorder, suggesting that ethnicity and family income play important roles in understanding the phenomenology of these behavioral and affective problems. For instance, Rohde, Beevers, Stice, and O’Neil (2009) found that non- Caucasian adolescents were at greater risk for developing depressive symptoms, and developing these depressive symptoms earlier than their Caucasian counterparts. Conversely, Caucasian/non-Hispanic adolescents used substances more than their Latino, Asian, and African American peers (Wu, Woody, Yang, Pan, & Blazer, 2011). Family income has also been associated separately with both depressive symptoms (e.g., Goodman, Slap, & Huang, 2003) and substance use (e.g., Goodman & Huang, 2002). For example, lower income levels are correlated with greater number of symptoms of depression, cigarette use, and alcohol consumption (Goodman & Huang, 2002; Goodman et al., 2003). Despite these established links, race/ethnicity and household income are rarely reported in studies of comorbidity (Armstrong & Costello, 2002), and little is known about the role they play in predicting onset and age-related increases in symptoms of both conditions concurrently.
Discrepancies in the Existing Literature
One explanation for the discrepancies regarding temporal precedence of these disorders may be the different methodologies employed by researchers. First among these differences is the use of cross-sectional and retrospective reporting versus prospective, longitudinal methods. Cross-sectional studies do not allow for examination of changes in behavior over time and retrospective reporting may be particularly inappropriate for gathering detailed information regarding age of first substance use, mood symptom onset, and frequency of substance use (Kazemian & Farrington, 2005). For example, Jolliffe et al. (2003) found that when children were asked to recall when they had used substances, they reported significantly earlier dates retrospectively as compared to their own prospective reports. Second, the preponderance of studies reviewed above used measures of single substances. Further, many considered only substances that are common (e.g., marijuana), legal (cigarettes), or both (alcohol). Given that adolescents engaging in polysubstance use represent a uniquely vulnerable population (Trudeau et al., 2007), further research on this group is warranted. Third, most of the research reviewed above utilized samples with truncated age ranges. Given the sharp rise in rates of depressive symptoms for girls (compared to boys) between the ages of 13 and 17 (Kofler et al., 2011; Twenge & Nolen-Hoeksema, 2002), and similar increases in illicit drug use over this age group (Johnston et al., 2011), it is possible that studies focusing exclusively on late childhood and early adolescence (e.g., Costello et al., 1999) may omit key aspects of the adolescent developmental picture. Fourth, research consistently supports the need to examine the function of other demographic factors in the emergence of co-occurring depressive symptoms and substance use. While there is sufficient evidence to suggest that gender plays an important (albeit not completely understood) role in the development of these symptom clusters, almost no research has looked at the impact of ethnicity and family income on depression/polysubstance use covariation, despite their relation to depressive symptoms and substance use independently.
The current study addressed these limitations by employing a prospective, nationwide, accelerated longitudinal (“cohort sequential”) sample of adolescent boys and girls ages 12–17 (at the initial assessment) to test opposing predictions stemming from models of depressive-symptom precedence, polysubstance use precedence, and nondirectional models of polysubstance use/depressive symptom covariation. Specifically, competing models were tested using cohort-sequential latent growth curve modeling (LGM) to determine whether depressive symptoms at age 12 (baseline) predict concurrent and age-related changes in polysubstance use, whether the opposite pattern is apparent (polysubstance use predicting depressive symptoms), and whether initial levels of depressive symptoms predict changes in polysubstance use significantly better than vice versa. The use of this structural equation modeling approach has the additional advantage of explicitly controlling for measurement error, while allowing age-related symptom changes to simultaneously serve as predictors and indicators of other variables (Byrne, 2010). These methodological refinements also allowed us to examine demographic influences (gender, ethnicity, and household income) on depressive symptoms and polysubstance use, as well as control for the potential impact of additional demographic variables such as community type (urban/rural).
We expected significant relations between depressive symptoms and polysubstance use across all concurrent time points (e.g., Fleming et al., 2008). Consistent with the negative affect regulation model, early depressive symptoms were expected to predict age-related changes in polysubstance use, whereas early polysubstance use was not expected to predict age-related changes in depressive symptoms. Conversely, models emphasizing opponent processes suggest the opposite pattern: early polysubstance use should predict age-related increases in depressive symptoms, whereas early depressive symptoms should not predict age-related increases in polysubstance use after accounting for the impact of early polysubstance use. We hypothesized also that gender would significantly predict age-related changes in both symptoms clusters, whereas gender differences in initial depressive symptoms were not expected (Kofler et al., 2011; Twenge & Nolen-Hoeksema, 2002). Specifically, girls were expected to report disproportionate increases in depressive symptoms over time, whereas boys were expected to demonstrate higher baseline and steeper age-related increases in polysubstance use. Finally, because there is very little information about the role of family income and ethnicity in the development of co-occurring disorders, we also explored these relations in the analyses presented below.
Method
Sample and procedure
Institutional review board approval was obtained prior to data collection. The 2005 National Survey of Adolescents— Replication was a nationwide standardized telephone interview of households with adolescents between the ages of 12 and 17, including an oversample of urban households. Sample selection and computer-assisted interviewing were conducted by Schulman, Ronca, and Bucuvalas, Inc., a survey research firm with extensive experience conducting sensitive interviews. A multistage, stratified, area probability, random digit dial, six-stage procedure was used to construct the initial probability sample (see Kilpatrick et al., 2000). Once it was determined that a household had at least one youth in the targeted age range, screening and introductory interviews were conducted with parents to establish rapport. Verbal consent from a caregiver or legal guardian was obtained before interviewing the adolescents; all youth gave verbal assent. Strategies were used to ensure adolescent comfort when responding to interview questions. Interviewers verified adolescents were in a private area where they could answer freely. In addition, the interviews were designed to include closed-ended questions requiring only “yes,” “no,” or other one-word answers. Thus, if someone in the home were listening, they would be unlikely to hear anything that would violate the adolescent’s privacy. Adolescents were offered $10 to complete the interview. Schulman, Ronca, and Bucuvalas, Inc., supervisors conducted random checks of interviewer adherence to assessment procedures.
Given the sensitive nature of some interview questions, several additional steps were taken to increase participant protection. Adolescents who reported during the interview that they (a) had been assaulted by a family member in the past year and (b) had not disclosed the assault to anyone were interviewed by a clinician on the project team to determine if they were in current danger. Those judged to be in danger were encouraged to make a voluntary report to Child Protective Services. The clinician was prepared to make the report if the adolescent was unwilling to do so. All adolescents also were provided with the number to Child Help, a national telephone counseling program for at-risk youth.
During recruitment, 6,694 households were contacted. Of these, 1,268 (18.9%) parents refused adolescent participation, 188 (2.8%) adolescents refused after their parents consented, 119 (1.8%) adolescent interviews were initiated but not completed, and 1,505 (22.5%) parent interviews were completed but the eligible adolescent was not available at any of our callbacks. The remaining 3,614 cases resulted in completed parent and adolescent interviews. Ten cases were excluded due to age at initial interview, resulting in a Wave 1 sample size of 3,604 adolescents ages 12–17. The sample included adolescents from all four US Census regions. Specifically, 34.3% of the adolescents resided in the South, 25.4% resided in the Midwest, 24.2% resided in the West, and 16.1% resided in the Northeast. Participant demographics are similar to national population estimates and are shown in Table 1.
Table 1.
Demographic characteristics of participants in the National Survey of Adolescents replication
| Ethnicity |
Wave 1 Annual Household Income |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Cohort | N | Girls | Caucasian | African Amer. | Hispanic | Native Amer./ Alaskan | Asian/ Pacific Isl. | <$20K | $20K to $50K | >$50K | Not Sure/ Refused |
| 12 | 488 | 47.5% | 65.4% | 16.0% | 10.7% | 2.9% | 5.0% | 14.8% | 32.4% | 48.2% | 4.7% |
| 13 | 573 | 48.2% | 65.0% | 17.3% | 11.5% | 3.6% | 2.6% | 13.1% | 31.2% | 48.3% | 7.3% |
| 14 | 631 | 47.4% | 66.9% | 15.9% | 13.1% | 2.1% | 1.9% | 13.5% | 30.1% | 50.1% | 6.3% |
| 15 | 641 | 50.1% | 66.5% | 15.8% | 11.9% | 2.6% | 3.2% | 12.8% | 30.4% | 50.9% | 5.9% |
| 16 | 647 | 52.1% | 66.6% | 16.8% | 11.7% | 1.6% | 3.3% | 10.8% | 27.4% | 53.2% | 8.7% |
| 17 | 624 | 53.7% | 72.0% | 13.7% | 10.7% | 2.1% | 1.5% | 11.7% | 26.3% | 53.7% | 8.3% |
| Total | 3604 | 49.8% | 67.0% | 15.9% | 11.6% | 2.5% | 2.9% | 12.8% | 29.6% | 50.7% | 6.9% |
| National est.a | — | 48.7% | 60.6% | 15.2% | 17.3% | 3.3% | 3.6% | 12.9% | 27.8% | 59.3% | — |
Note: Demographic variables were assessed using standard questions employed by the US Bureau of the Census (1988). Age was measured as the current age in years at the time of the Wave 1 interview (range=12–17 years). No significant differences in gender, ethnicity, or income were found across cohorts (all χ2 ps>.10).
National estimates reflect US Census estimates of the adolescent population in 2005.
Waves 2 and 3 involved attempts approximately 1 year apart to recontact all adolescents included in the original survey. Methods for locating participants who had moved/ changed phone numbers included asking about planned moves during the previous year’s interview, acquiring updated contact information from directory assistance, and sending letters to last known addresses. As expected, based on the random digit dialing method for participant selection, attrition across study waves was moderately high (33.5% between waves). Attrition was also slightly higher among non-Caucasian relative to Caucasian/non-Hispanic adolescents. Two sets of analyses examined whether attrition was systematically related to the primary study variables, including depressive symptoms and polysubstance use. First, participants completing versus not completing all three waves were compared. Effect size confidence interval analysis revealed no differences for depressive symptoms or age (95% confidence intervals [CIs] include 0.0) and small magnitude differences for polysubstance use (Cohen = –0.10; 95% CI=–0.17 to –0.04), with study completers endorsing slightly lower polysubstance use at Wave 1 relative to noncompleters. Second, 200 participants who could not be located at Wave 2 were located and reinterviewed during Wave 3. Effect size confidence interval analysis revealed no differences between this group and completers for age, depressive symptoms, or polysubstance use for this follow-up (all 95% CIs contained 0.0).
Collectively, these analyses suggest that the impact of missing data was likely modest. In addition, the cohort-sequential design employed in the current study uses full information maximum likelihood estimation to include all participants and provides estimates based on multiple cohorts, which minimizes the impact of missing data at any individual wave (Byrne, 2010; Duncan, Duncan, & Strycker, 2006). Thus, all 3,604 participants contributed data to at least one chronological age group regardless of their pattern of missing data, with a total of 7,500 data points each for the depressive symptom and polysubstance use variables (2,304 participants provided data for at least two waves of data collection and 1,592 adolescents provided data for all three waves). Nevertheless, we elected to describe the sample as “nation-wide” rather than “nationally representative” to acknowledge the potential impact of participant refusal and attrition.
Measures
Demographic data.
Demographic variables, including child age, sex, ethnicity, and family income, were assessed using standard questions from the US Census Bureau (DeNavas-Walt, Proctor, & Smith, 2007). Community type was assessed by asking parents of participants to report if they live in an urban, suburban, or rural area. The results suggest that the sample is highly reflective of the US population (Table 1). No significant differences in any demographic variables were found between cohorts (all x2 ps>.10).
Major depressive symptoms.
Major depressive symptoms were assessed using the National Survey of Adolescents (NSA) Depression Module, a structured diagnostic interview that targets DSM-IV major depressive episode criteria over the past year (Table 2). Psychometric data support the internal consistency (Kilpatrick et al., 2003) and convergent validity (Boscarino et al., 2004) of the scale. Thirteen questions were used to assess each of the DSM-IV symptoms of depression over the preceding year, with thoughts of death and suicide separated into two items. The NSA Wave 1 depression module probed for lifetime and past 6-month symptom occurrence, whereas past-year and 6-month symptom occurrence were assessed at Waves 2 and 3. To maintain a consistent metric across variables and study waves, past year depressive symptom endorsement at Wave 1 was estimated based on past 6-month symptom endorsement at Wave 1 by solving regression equations derived from predicting past-year depressive symptoms from 6-month depressive symptoms at Waves 2 and 3 (both R2>.88) as recommended (Kofler et al., 2011).
Table 2.
Descriptive statistics for the depressive symptoms and polysubstance use variables by cohort, wave, and gender
| Depressive Symptoms |
Polysubstance Use |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort | Wave 1 |
Wave 2 |
Wave 3 |
Wave 1 |
Wave 2 |
Wave 3 |
|||||||
| Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | ||
| 12 | M | 0.92 | 0.96 | 0.83 | 1.03 | 0.50 | 1.22 | 0.04 | 0.01 | 0.10 | 0.07 | 0.15 | 0.14 |
| SD | 1.51 | 1.71 | 1.99 | 1.89 | 1.09 | 2.09 | 0.27 | 0.11 | 0.55 | 0.43 | 0.73 | 0.42 | |
| 13 | M | 0.86 | 1.45 | 0.69 | 1.88 | 0.84 | 2.02 | 0.07 | 0.07 | 0.11 | 0.08 | 0.39 | 0.19 |
| SD | 1.32 | 2.43 | 1.33 | 2.79 | 1.76 | 3.04 | 0.31 | 0.31 | 0.62 | 0.34 | 1.34 | 0.52 | |
| 14 | M | 1.25 | 2.05 | 0.97 | 1.47 | 1.03 | 1.47 | 0.20 | 0.30 | 0.23 | 0.17 | 0.43 | 0.14 |
| SD | 2.04 | 2.91 | 1.97 | 2.36 | 2.04 | 2.39 | 0.65 | 1.24 | 0.68 | 0.78 | 1.03 | 0.42 | |
| 15 | M | 1.28 | 2.16 | 1.019 | 2.41 | 1.12 | 2.30 | 0.45 | 0.43 | 0.37 | 0.28 | 0.51 | 0.59 |
| SD | 2.08 | 2.92 | 2.21 | 3.19 | 2.12 | 3.25 | 1.36 | 1.32 | 0.88 | 0.82 | 1.24 | 1.40 | |
| 16 | M | 1.42 | 2.36 | 1.34 | 2.03 | 1.30 | 1.94 | 0.48 | 0.53 | 0.48 | 0.44 | 0.59 | 0.49 |
| SD | 2.00 | 3.04 | 2.24 | 2.97 | 2.24 | 3.12 | 1.09 | 1.24 | 1.03 | 1.11 | 1.27 | 1.01 | |
| M | 1.44 | 2.73 | 1.08 | 2.04 | 1.26 | 1.81 | 0.83 | 0.75 | 0.51 | 0.61 | 0.78 | 0.56 | |
| SD | 2.17 | 3.22 | 2.18 | 2.84 | 2.36 | 2.70 | 1.82 | 1.49 | 1.23 | 1.34 | 1.65 | 1.13 | |
| Total | M | 1.21 | 2.02 | 1.03 | 1.84 | 1.03 | 1.82 | 0.35 | 0.38 | 0.31 | 0.29 | 0.48 | 0.36 |
| SD | 1.92 | 2.85 | 2.02 | 2.76 | 2.05 | 2.84 | 1.11 | 1.16 | 0.88 | 0.91 | 1.24 | 0.94 | |
Polysubstance use.
Past-year polysubstance use was evaluated using the NSA Substance Use Module. Research on this module has provided solid evidence of reliability as well as associations in expected directions with relevant constructs, including interpersonal victimization, mental health problems, and familial drug use (Kilpatrick et al., 2000, 2003). This portion of the interview asks adolescents if they have used each of the 16 specific drugs shown in Table 3 since the prior-year interview. In line with findings from Kirisci, Vanyukov, Dunn, and Tarter (2002), we created a polysubstance use index by summing the number of different drugs endorsed by each adolescent at each wave. This approach has demonstrated strong predictive validity in relation to substance use behaviors and psychiatric disorders in other adolescent samples (e.g., Smit, Monshouwer, & Verdurmen, 2002; Trudeau et al., 2007), and may be a better predictor of adolescent problematic drug use and relapse from drug treatment, adult serious mental illness (Barnett et al., 2007; Ciesla, 2010; Trenz et al., 2012), and adolescent depressive symptoms and suicidality compared to single drug frequency counts (Conway et al., 2013; Kandel et al., 1986).
Table 3.
Percentage of engagement in each of 16 illicit substances by age cohort and study wave
| Age 12 |
Age 13 |
Age 14 |
Age 15 |
Age 16 |
Age 17 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| W1 | W2 | W3 | W1 | W2 | W3 | W1 | W2 | W3 | W1 | W2 | W3 | W1 | W2 | W3 | W1 | W2 | W3 | |
| Prescription drug misuse | ||||||||||||||||||
| Tranquilizers | 0.2 | 0.3 | 0.5 | 0 | 1.5 | 1.4 | 1.6 | 1.3 | 2.3 | 2.7 | 3.1 | 3.9 | 4.0 | 2.8 | 4.3 | 5.6 | 4.8 | 4.0 |
| Barbiturates | 0.8 | 0 | 0 | 0.5 | 0 | 1.4 | 1.4 | 1.8 | 2.0 | 2.8 | 1.1 | 2.3 | 2.3 | 1.3 | 0 | 3.4 | 1.8 | 2.7 |
| Amphetamines | 0 | 0.3 | 0.5 | 0.2 | 0.5 | 2.4 | 1.7 | 1.3 | 2.0 | 4.2 | 3.1 | 2.6 | 4.2 | 2.8 | 4.6 | 5.1 | 5.0 | 5.8 |
| Pain medication | 0.4 | 1.5 | 1.4 | 1 | 0.7 | 3.8 | 3.3 | 1.6 | 2.6 | 3.6 | 3.3 | 6.5 | 4.3 | 5.6 | 5.6 | 9.6 | 5.3 | 4.5 |
| Steroids | 0 | 0 | 0.5 | 0.2 | 0 | 0.7 | 0.2 | 0 | 0 | 0.5 | 0.4 | 0.7 | 0.3 | 0 | 0 | 0.2 | 0.3 | 0.4 |
| Common street drugs | ||||||||||||||||||
| Marijuana | 0.8 | 3.6 | 8.1 | 3.7 | 5.7 | 12.9 | 10.1 | 9.8 | 16 | 16.7 | 17.6 | 24.4 | 24.3 | 22.6 | 27.5 | 33.2 | 24.4 | 27.7 |
| Crack/cocaine | 0 | 0.3 | 0.5 | 0.2 | 0.2 | 1.0 | 0.6 | 0.2 | 0 | 1.9 | 0.7 | 2.6 | 2.5 | 3.0 | 2.3 | 5.4 | 4.3 | 4.9 |
| Angel dust/PCP | 0 | 0 | 0.5 | 0 | 0.2 | 0.3 | 0.3 | 0 | 0 | 0.8 | 0 | 0.7 | 0.3 | 0 | 0 | 0.8 | 0 | 0 |
| Methadone/heroin | 0 | 0 | 0 | 0.2 | 0 | 0.7 | 0.3 | 0.2 | 0.3 | 0.5 | 0.2 | 1.0 | 0.5 | 0.4 | 0.7 | 0.8 | 0.5 | 0.4 |
| Inhalants | 0.2 | 0.9 | 0.5 | 1.2 | 0.2 | 0.3 | 1.6 | 0.7 | 0.3 | 3.0 | 0.7 | 1.3 | 1.5 | 0.4 | 1.3 | 2.7 | 1.0 | 1.3 |
| Club drugs | ||||||||||||||||||
| Ecstasy | 0.2 | 0.6 | 0.9 | 0 | 0.5 | 1.4 | 1.1 | 1.6 | 1.6 | 1.7 | 1.5 | 4.2 | 1.9 | 2.6 | 3.0 | 3.5 | 2.8 | 5.4 |
| GHB | 0 | 0.3 | 0 | 0 | 0 | 0 | 0.5 | 0.2 | 0.3 | 0.2 | 0.2 | 0.3 | 0 | 0.2 | 0.3 | 0.6 | 0.3 | 0 |
| Ketamine | 0 | 0 | 0 | 0 | 0 | 0 | 0.3 | 0 | 0 | 0.6 | 0 | 0.7 | 0.3 | 0.2 | 0.7 | 0.3 | 0.5 | 0 |
| Rohypnol | 0 | 0 | 0 | 0 | 0 | 0 | 0.2 | 0 | 0 | 0.2 | 0 | 0 | 0.2 | 0.2 | 0 | 0.2 | 0.3 | 0 |
| Metamphetamine | 0 | 0.3 | 0.5 | 0 | 0.2 | 0.7 | 0.8 | 0.4 | 0.3 | 1.9 | 0.7 | 0.7 | 1.2 | 0.9 | 1.0 | 2.7 | 1.0 | 1.8 |
| Hallucinogens | 0 | 0.6 | 0.9 | 0.2 | 0.2 | 2.1 | 1.3 | 0.9 | 1.6 | 2.7 | 1.5 | 3.3 | 2.9 | 3.0 | 4.6 | 5.1 | 4.3 | 7.1 |
Data analysis
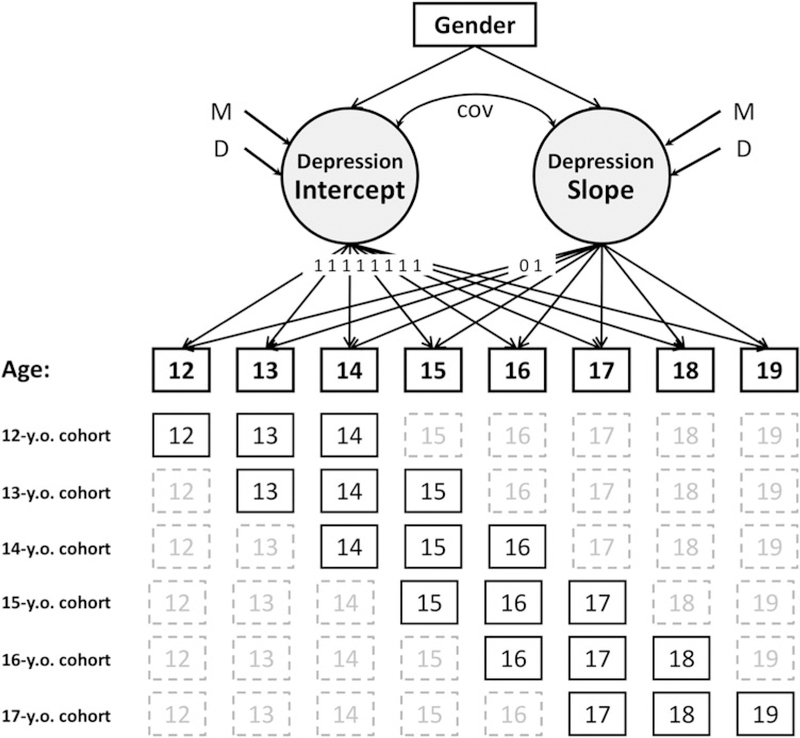
Cohort-sequential LGM was used to examine the interrelations among initial (baseline) levels and age-related changes in depressive symptoms and polysubstance use (Figure 1). Individuals were 12 to 17 years of age during the initial interview and were reinterviewed two additional times at approximately 1-year intervals, resulting in six temporally overlapping cohorts, each providing data for three adjacent ages (e.g., 12-year-old cohort and 13-year-old cohort). The cohort-sequential design combines data across these cohorts to approximate a traditional longitudinal design of adolescents from ages 12 to 19, while minimizing potential cohort effects by estimating symptoms at each age based on multiple cohorts across different years (Duncan et al., 2006).
Figure 1.
Cohort-sequential latent growth curve model for depressive symptoms. Variables represent baseline symptom levels at age 12 (intercept) and age-related increases from 12 to 19 (slope). Solid age boxes represent collected data, whereas dashed lines reflect data missing by design. Asterisks indicate that pathways were allowed to vary freely, with the exception that regression weights at each age are equal across cohorts. The intercept (age 12) is based on data from all ages across all cohorts, as notated by the “1s.” An identical procedure was used to model the polysubstance use variable. Cov, covariance; D, variance; y.o., year old.
LGM provides estimates of means and variances for two primary metrics: intercept and slope. The intercept is estimated based on data from all participants across all waves, and modeled such that the intercept mean reflects the initial level of symptom endorsement (i.e., baseline at age 12). In contrast, slope means reflect the rate of change of these symptoms over time (Duncan et al., 2006). Significant variances in intercept and slope indicate individual differences in initial symptom level and rate of change over time, respectively, and support the analysis of potential predictors of these differences.
In LGM, regression weights for the intercept are all set to 1.0, which allows the intercept to be interpreted as the initial (baseline) level of a variable. For the slope factor, the first two regression weights (i.e., ages 12 and 13) are set to 0.0 and 1.0. Regression weights for all other ages are allowed to be estimated freely to capture both linear and nonlinear change over time, with the restriction that regression weights at each age are equal across cohorts.1 The intercept and slope for each variable are set to covary, which is necessary for model specification (Duncan et al., 2006). Amos 18.0 structural equation modeling software was used for all analyses.
Three commonly used fit indices were used to estimate how well each model fit the data: chi-square (x2), comparative fit index (CFI), and the root mean square error of approximation (RMSEA). Nonsignificant x2 values indicate good fit, but this index is heavily impacted by sample size. CFI values of>0.95 and RMSEA values of<0.05 indicate excellent fit; CFI values of>0.90 and RMSEA values of<0.08 indicate acceptable fit (Schweizer, 2010).
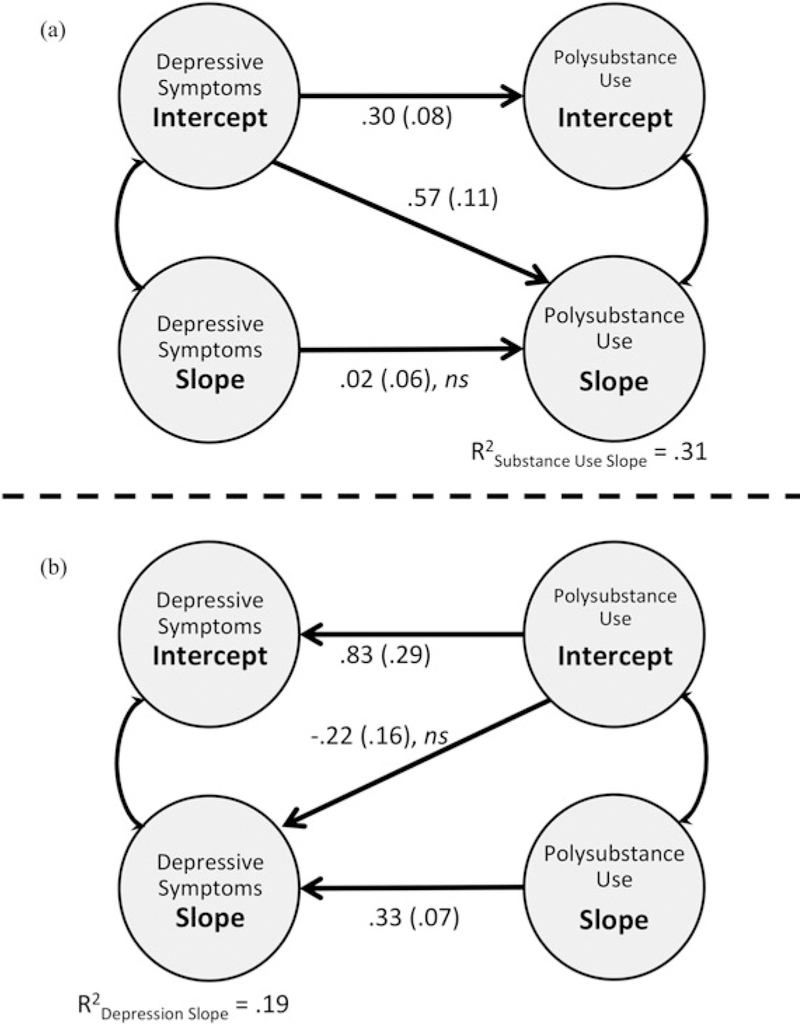
A three-tier data analytic approach was adopted to examine predictions from the theoretical models of depression– polysubstance use covariation described above. In the first tier (Figure 1), separate depression and polysubstance use models were created to examine initial levels (intercept) and age-related changes (slope) for these variables, and determine the need to examine potential predictors of these changes. Symptom counts for depression and polysubstance use across adolescence are shown in Figure 2. In Tier II, the depression and polysubstance use models were combined, and two hypotheses were tested. The first combined model (Figure 3a) tests negative affect regulation model predictions, such that initial levels of depressive symptoms were modeled to predict initial levels of polysubstance use and age-related changes in polysubstance use. In addition, age-related changes in depressive symptoms were modeled to predict age-related changes in polysubstance use. The second combined model (Figure 3b) reverses these predictors based on opponent process model predictions: initial levels of polysubstance use were modeled to predict initial levels of depressive symptoms and age-related changes in depressive symptoms. In addition, age-related changes in polysubstance use were modeled to predict age-related changes in depressive symptoms.
Figure 2.
Depressive symptoms and polysubstance use endorsement between ages 12 and 19, across three cohorts in the National Survey of Adolescents. Values reflect mean number of symptoms endorsed (depression; left vertical axis) and mean number of substances used (polysubstance use; right vertical axis). Error bars reflect standard errors.
Figure 3.
Cohort-sequential latent growth models. Model (a) tests the negative affect regulation model, with depression intercept predicting polysubstance use intercept and slope, and depression slope predicting polysubstance use slope. Model (b) tests the opponent process model, with polysubstance use intercept predicting depression intercept and slope, and polysubstance use slope predicting depression slope. Variables represent baseline symptom levels at age 12 (intercept) and age-related increases from 12 to 19 (slope). Single-headed arrow values reflect standardized b weights; double-headed arrow values reflect correlations (r). Regression pathways for both models are all significant at p ≤ .004 unless marked nonsignificant (ns, all ps ≥ .17). Gender, ethnicity, and household income are included in both models but not depicted for readability. Values in parentheses reflect standard error. Adapted from “Depression and Delinquence Covaration in an Accelerated Longitudinal Sample of Adolescents,” by M. J. Kofler, M. R. McCart, K. Zajac, K. J. Ruggiero, B. E. Saunders, and D. G. Kilpatrick, 2011, Journal of Consulting and Clinical Psychology, 79, 458–469. Copyright 2011 by American Psychological Association. Adapted with permission.
An additional set of analyses (Tier III) used z score tests for equality of regression coefficients (Paternoster, Mazerolle, & Piquero, 1998) and comparison of nonnested model fit indices to test directionality of effects by determining whether one model fit the data significantly better than the other model, in terms of both relative model fit and the magnitude of prediction. Finally, the Tiers II and III results were used in Tier IV to create a new model of the relation between depressive symptoms and polysubstance use across adolescence (Figure 4). The Tier IV model thus reflects the cumulative findings of Tiers I–III, and reflects a new, data-driven model of temporal interrelations among depressive symptoms and polysubstance use across adolescence while controlling for gender, ethnicity, and family income.
Figure 4.
Final developmental cascade model of depressive symptoms and polysubstance use. Variables represent baseline symptom levels at age 12 (intercept) and age-related increases from ages 12 to 19 (slope). Single-headed arrow values reflect standardized β weights; double-headed arrow values reflect correlations (r). Regression pathways are significant at p ≤ .0005 unless marked nonsignificant (ns, p>.05). Indirect effects: POLY_Intercept → DEP_Intercept → POLY_Slope: αβ = 0.12, p= .008; DEP_Intercept → POLY_Slope → DEP_Slope: αβ= 0.17, p=.008.
Given that gender, ethnicity, and household income are correlates of polysubstance use and mental health problems among youth (Kilpatrick et al., 2003; Martinez & Richters, 1993; Turner, Finkelhor, & Ormrod, 2006), these variables were included in Tier I as time-invariant predictors, and significant predictors were retained in the Tier II, III, and IV models. Gender was coded as boys=0, girls=1, and race/ ethnicity was coded as Caucasian/non-Hispanic=0, non- Caucasian=1. Annual household income was assessed using 10 ordered categories ranging from 1 (>$5000/year) to 10 (<$100,000/year). To address one potential confound associated with nationwide studies, we entered community type as a potential time-invariant predictor, coded as urban versus suburban/rural.2 Significance levels were set at p < .05 for all analyses; “trends” toward significance were not interpreted given the large sample size.
Results
Tier I. Separate depression and polysubstance use models
In Tier I, initial levels and age-related changes in depressive symptoms and polysubstance use were modeled separately. Data for these initial models are not shown in tables due to space limitations. Magnitude and significance levels are equivalent to those reported in the Tier II–IV combined models unless noted otherwise. Both Tier I models fit the data significantly better when demographic variables (gender, ethnicity, and household income) were allowed to predict intercept and slope (both x2 difference tests ps<.0005).
The depression model demonstrated excellent fit (CFI=0.95, RMSEA=0.01, 90% CIRMSEA=0.011–0.018). Model fit for the polysubstance use variable was slightly below acceptable levels for the CFI (0.85) but excellent based on the RMSEA (0.03, 90% CIRMSEA=0.027–0.034); therefore, overall model fit was determined to be acceptable. For both models, significant demographic predictors were retained for all Tier II, III, and IV models (Figure 4; all other pathways p>.05). Collectively, the impact of these time-invariant predictors on age-related increases in depressive symptoms (R2=.05) and polysubstance use (R2=.01) was modest.
Tier IIa. Depressive symptoms predicting polysubstance use (e.g., negative affect regulation model)
In Tier IIa, the depression and polysubstance use models were combined to test negative affect regulation model predictions regarding the extent to which baseline depressive symptoms predict age-related increases in polysubstance use after accounting for demographic variables and baseline levels of both depression and polysubstance use (Figure 3a). The model fit was acceptable for the CFI (0.85), and excellent based on the RMSEA (0.025, 90% CIRMSEA=0.023– 0.027); therefore, overall model fit was determined to be acceptable. All regression pathways were significant (all ps≤.0005) unless noted and are described below.
Concurrent symptom relations (intercept predicting intercept and slope predicting slope).
Baseline depressive symptoms were significantly associated with baseline polysubstance use (β 0.30). In contrast, age-related increases in depressive symptoms were not significantly related to age-related increases in polysubstance use (p=.74) after accounting for demographic variables and baseline levels of depressive symptoms and polysubstance use.
Temporal predictions (intercept predicting slope).
It is important that baseline depressive symptoms significantly predicted age-related increases in polysubstance use (β=0.57), even after accounting for early polysubstance use, gender, household income, and ethnicity. The polysubstance use slope variance remained significant ( p<.0005), indicating that individual differences in age-related increases in polysubstance use remained after accounting for baseline polysubstance use, baseline and age-related changes in depressive symptoms, gender, ethnicity, and household income.
Collectively, the model explained 31% of the variance in age-related increases in polysubstance use (R2=.31), relative to the 1% of variance explained by the Tier I polysubstance use model. These findings indicate that early depressive symptoms represent a significant risk factor for future increases in polysubstance use, even after accounting for the impact of early polysubstance use, gender, ethnicity, and household income.
Tier IIb. Polysubstance use predicting depressive symptoms (e.g., opponent process model)
In Tier IIb, regression pathways from Tier IIa were reversed to test opponent process model predictions regarding the extent to which baseline polysubstance use predicts age-related increases in depressive symptoms after accounting for demographic variables and baseline levels of depressive symptoms (Figure 3b). All regression pathways were significant at p ≤ .0005 unless noted and are described below.
Concurrent symptom relations (intercept predicting intercept and slope predicting slope).
Baseline polysubstance use was significantly associated with baseline depressive symptoms (β 0.83, p<.01), as expected. In addition, age-related increases in polysubstance use were significantly related to age-related increases in depressive symptoms (β=0.33, p< .0005) after accounting for demographic variables and baseline levels of depressive symptoms and polysubstance use.
Temporal predictions (intercept predicting slope).
It is important that baseline polysubstance use did not significantly predict age-related increases in depressive symptoms ( p=.17) after accounting for early depressive symptoms, gender, household income, and ethnicity. The depressive symptom slope variance remained significant ( p<.0005), indicating that individual differences in age-related depressive symptom increases remained after accounting for base-line depressive symptoms, baseline and age-related changes in polysubstance use, and demographic variables.
Collectively, the model explained 19% of the variance in age-related increases in depressive symptoms (R2=.19), relative to the 5% of variance explained by the Tier I depressive symptom model. These findings indicate that polysubstance use represents a significant risk factor for concurrent depressive symptoms at any age but that early polysubstance use does not portend increased risk for age-related depressive symptom increases after accounting for the impact of early depressive symptoms, gender, ethnicity, and household income.
Tier III: Model comparison
Model comparison.
Additional analyses were conducted to inform the interpretation of the results by determining whether one model fit the data significantly better than the other (in other words, if depressive symptoms predicted changes in polysubstance use, or vice versa). Three indices that can be used to compare nonnested models were examined: the Akaike information criterion (AIC), the Browne– Cudeck criterion (BCC), and the expected cross-validation index (ECVI), with smaller values indicating better fit (Byrne, 2010). AIC (944 vs. 939), BCC (946 vs. 941), and ECVI (0.26, 90% CIECVI=0.24–0.29 for both models) values were approximately equivalent across models, suggesting that both models adequately fit the data, with neither model demonstrating clear superiority. Interpretations were there- fore based on the findings of both models.
Magnitude of prediction.
Standardized regression weights were subsequently compared to examine the relative strength of prediction across models (“depression predicting polysubstance use” model vs. “polysubstance use predicting depression” model). Specifically, the absolute values of the standardized β weights and standard errors (Figure 3a and b) are used to calculate a z score to test the equality of regression coefficients (Paternoster et al., 1998). Directionality of effects is suggested when one variable predicts a second variable significantly better than vice versa; two variables that predict each other approximately equally well suggest covariation rather than causation (e.g., Alderson, Rapport, Hudec, Sarver, & Kofler 2010). The results reveal that the polysubstance intercept predicted the depression intercept (β=0.83, SE=0.29) significantly better than the depression intercept predicted the polysubstance intercept (β=0.30, SE=0.08; z=–1.76, p=.039). This pattern is consistent with models suggesting that early polysubstance use conveys increased risk for concurrent depressive symptoms more so than vice versa, such as the opponent process model.
In contrast, examination of temporal predictions suggests that the depression intercept predicted age-related polysubstance use increases (β=0.57, SE=0.11) significantly better than the polysubstance use intercept predicted age-related increases in depressive symptoms (β=–0.22, SE=.16; z=1.80, p=.035), consistent with the negative affect regulation model. In other words, early depressive symptoms portend increased risk for future polysubstance use, whereas early polysubstance use does not increase an adolescent’s risk for future depressive symptoms. This pattern again reverses when examining co-occurring changes in both syndromes across adolescence (slope predicting slope) and suggests support for models proposing polysubstance use precedes depression, such as the opponent process model. The polysubstance use slope predicted the depression slope (β=0.33, SE=0.07) significantly better than the depression slope predicted the polysubstance use slope (β=0.02, SE=0.06; z=3.36, p=.004). This pattern of results suggests that age- related increases in polysubstance use portend increased risk for concurrent age-related increases in depressive symptoms.
Tier IV: Final, combined model of depressive symptom/ substance use covariation
Collectively, the Tier II and III findings indicate that polysubstance use predicts concurrent depressive symptoms significantly better than depressive symptoms predict concurrent polysubstance use, based on both intercept-intercept and slope-slope comparisons. In contrast, early depressive symptoms, but not age-related increases in depressive symptoms, portend increased risk for future increases in polysubstance use.
These conclusions were tested by fitting a final model based on the evidence for covariation and directionality found in Tier III. Specifically, the polysubstance intercept was modeled to predict the depression intercept, and the polysubstance slope was modeled to predict the depression slope. In addition, the depression intercept was modeled to predict the polysubstance use slope, whereas no relation was modeled between the polysubstance use intercept and the depression slope (Figure 4). Model fit was slightly below acceptable levels for the CFI (0.85) but excellent based on the RMSEA (0.024, 90% CIRMSEA=0.022–0.026), with AIC (938), BCC (929), and ECVI (0.26, 90% CIECVI=0.24–0.29) values similar to the Tier II models; model fit was therefore determined to be acceptable. The results are shown in Figure 4. As expected, early polysubstance use predicted concurrent depressive symptoms (β=0.30, p<.0005). In turn, early depressive symptoms conveyed increased risk for age-related increases in polysubstance use (β=0.41, p <.0005), and in turn these age-related increases in polysubstance use portended increased risk for increased depressive symptoms over the same time period (β=0.42, p<.0005).
In addition, age-related increases in polysubstance use mediated the relation between baseline depressive symptoms and age-related changes in depressive symptoms, αβ=0.17; Sobel test (SE)=2.65 (0.06), p=.008, such that the depression intercept and slope were no longer related significantly in this model ( p .06). In other words, consistent with negative affect regulation model predictions, the relation between early and age-related increases in depressive symptoms is attributable partially to the increased risk for future polysubstance use associated with early depressive symptoms, which in turn strongly predicts additional increases in depressive symptoms over time.
In addition, early depressive symptoms served as a significant mediator of the relation between early polysubstance use and age-related increases in polysubstance use, αβ=0.12; Sobel test (SE)=2.67 (0.05), p=.008. In other words, consistent with opponent process predictions, one mechanism through which early polysubstance use portends increased risk for future polysubstance use is by increasing risk for early depressive symptoms. Thus, examining portions of the model in isolation provides support for both opponent process and negative affect regulation models; in contrast, examining the patterns of interrelations across adolescence reveals a more complex picture not accounted for fully by extant models. Specifically, the current analyses appear to suggest a developmental cascade model (Masten & Cicchetti, 2010), wherein early polysubstance use increases risk for early depressive symptoms, which in turn increase risk for increased polysubstance use over time, which in turn increases risk for concurrent depressive symptom increases.
Gender continued to predict age-related depressive symptom increases (girls had steeper increases; β=0.25, p<.0005), and household income predicted baseline depressive symptoms (lower income predicted higher depressive symptoms; β=–0.13, p<.0005). Finally, ethnicity continued to predict base-line depressive symptoms (β=–0.08, p<.0005), baseline polysubstance use (β=0.08, p<.047), and age-related polysubstance use increases (β=–0.11, p=.002), with Caucasian/ non-Hispanic adolescents reporting somewhat lower early depressive symptoms and polysubstance use but steeper increases in polysubstance use across adolescence.
Discussion
This study examined the co-occurring development of polysubstance use and depressive symptoms from late childhood to late adolescence. Specifically, we tested competing predictions from models suggesting that either depressive symptoms would precede polysubstance use or polysubstance use would precede depressive symptoms, while controlling for gender, ethnicity, family income, and community type. The results from this study suggest four important findings. First, baseline depressive symptoms at age 12 predicted age-related changes in polysubstance use. Second, polysubstance use appears to predict concurrent depressive symptoms better than depressive symptoms predicted concurrent polysubstance use. Third, the relation between depressive symptoms and polysubstance use during adolescence appears to be transactional due to evidence that (a) the relation between early and age-related increases in depressive symptoms is conveyed partially by the increased risk for future polysubstance use associated with early depressive symptoms, and (b) the relation between early and age-related increases in polysubstance use is conveyed partially by the increased risk for early depressive symptoms associated with early polysubstance use. Fourth, demographic factors including gender, family income, and ethnicity all significantly influenced the relation between polysubstance use and depressive symptoms. We elaborate on these results below as well as their developmental implications for understanding the co-occurrence of polysubstance use and depressive symptoms.
The overarching aim of the current study was to examine the interplay between depressive symptoms and polysubstance use across adolescent development. Previous research, much of which employed cross-sectional methods or utilized narrow age ranges, reported conflicting findings, suggesting depressive symptoms precede substance use (e.g., negative affect regulation; cf. Colder, 2001), substance use precedes depressive symptoms (e.g., opponent processes; cf. Schuckit, 2006), or symptoms of both disorders increase simultaneously (e.g., Fleming et al., 2008). The current study was able to rigorously test the directionality of these relations because of its longitudinal design, which allowed us to account for the stability of these constructs over time (as recommended by Cole & Maxwell, 2003). Further, our use of cohort sequential LGM provided an error-free measure of within-and between-person changes over time while controlling for cohort effects.
Our findings suggest support for an amalgam of existing models. Specifically, early depressive symptoms predicted age-related increases in polysubstance use, a finding consistent with negative affect regulation models hypotheses suggesting that substance use may stem from attempts to cope with uncomfortable feelings and low affect (e.g., Fox et al., 2011). In contrast, age-related increases in depressive symptoms did not convey increased risk for concurrent increases in polysubstance use. Instead, and consistent with models like the opponent process model, polysubstance use predicted concurrent depressive symptoms, both at baseline and concurrently over time. This finding appears to contradict predictions made by models similar to the negative affect model, or at minimum suggests that any relief from low mood conveyed by substance use is either short-lived or wholly unsuccessful (Lembke, 2012). Taken together, these findings suggest that while negative affect reduction may playan important role in initial risk for increasing polysubstance use over time, polysubstance-related increases in depressive symptoms appears to represent an important mechanism in maintaining the relation between symptoms of these disorders during adolescence.
Collectively, these results suggest a more complex model, in which early polysubstance use promotes early depressive symptoms, which in turn convey elevated risk for increasing polysubstance use over time, which in turn conveys additional risk for future depressive symptoms (Figure 4). Our findings provide initial evidence that the relation between these disorders may be best understood as a developmental cascade, in which conceptually distinct domains of development, including psychological functioning and behavior, influence each other both within and across development (Masten & Cicchetti, 2010). Masten and Cicchetti (2010) and Masten et al. (2005) describe developmental cascades as the sum total of a series of interactional and transactional effects, both directional and reciprocal, that affect development across the life span. In support, models of cascades from internalizing disorders to externalizing problems have highlighted the bidirectional and interactive nature of these disorders specifically (e.g., Capaldi, 1992). Our own results add to this burgeoning field by explicating the pathways by which symptoms of depression and polysubstance use may predict one another.
In addition to understanding the pattern of changes in depressive symptoms and polysubstance use across adolescence, this study also evaluated the impact of gender, house- hold income, and ethnicity on the emergence of co-occurring symptoms of these disorders. As expected, girls demonstrated greater increases in depressive symptoms over time. How-ever, contrary to our hypothesis, gender was not a significant predictor of age-related changes in polysubstance use. While several studies have found higher mean levels of substance use in males (Johnston et al., 2011; Svensson, 2003), it is possible that this effect was attenuated in the current study by sampling a broader range of adolescent development (ages 12–19), assessing the impact of additional demographic factors such as family income, ethnicity, and community type, and controlling for the impact of depressive symptoms. In line with previous research, household income and ethnicity were also associated with baseline depressive symptoms even when controlling for polysubstance use, such that children from lower income homes and those who identified as non-Caucasian evidenced greater levels of depressive symptoms (e.g., Chen & Jacobson, 2012; Goodman & Huang, 2002). Only ethnicity was associated with polysubstance use, indicating that Caucasian/non-Hispanic adolescents endorsed steeper age-related increases in polysubstance use relative to non-Caucasian youth, consistent with previous research (Chen & Jacobson, 2012).
Limitations
This study employed a large, nationwide, random sample of adolescents to examine associations between depressive symptoms and polysubstance use. However, despite these and other methodological strengths (e.g., controlling for measurement error and cohort effects and use of LGM mediation), the following limitations must be considered when interpreting the results. First, the study relied exclusively on adolescent self-report interviews, which may be subject to reporting bias and shared method variance. The findings may have differed if data were collected from different sources; however, past studies have found adolescents to be more accurate reporters of their internalizing problems compared to parents or teachers (e.g., Cantwell, Lewinsohn, Rohde, & Seeley, 1997). In addition, parent and adolescent symptom ratings are highly correlated over time, and self-reports appear to be more sensitive to early symptom emergence compared to parent reports (Cole et al., 2002). Further, our depressive symptom questionnaire assessed each DSM-IV symptom’s presence/absence; this format is less widely used relative to standardized clinical interviews for children, such as the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (Kaufman et al., 1997) and the Diagnostic Interview Schedule for Children (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). While the current assessment tools have been found to be concurrently and prospectively associated with theoretically related variables and yield prevalence rates similar to those seen in other epidemiological studies (e.g., Begle et al., 2011; Costello, Egger, & Angold, 2005; Kilpatrick et al., 2003), replication of these findings using standardized clinical interviews will be important in future research. In addition, our choice to examine polysubstance use using an index approach did not allow for us to examine relations between the frequency of individual substances and depressive symptoms. While there is support for our summative approach in the literature (cf. Zapert, Snow, & Tebes, 2002), future research should also examine the effect of single substances on depressive symptoms over time.
Second, another limitation was the moderately high refusal and attrition rates and the use of telephone survey methodology that excludes youth residing in households without landline telephone service. We note, however, that refusal rates were similar to or lower than those reported in other studies (Cole et al., 2002), and missing data analysis indicated that attrition was either unrelated or weakly related to our primary variables of interest. Further, the pattern of age-related symptom changes for all syndromes was consistent with the literature (Bukstein, Glancy, & Kaminer, 1992; Wolff & Ollendick, 2006). Nevertheless, it is impossible to know whether noncompleters differed from completers during waves at which the former were not assessed. In addition, our method for examining age-related changes across adolescence did not allow more fine-grained assessment of when during adolescence these mechanisms exert maximum effects. While the current analyses allowed us to examine change over time, future research should consider employing a panel-model approach to examine at what age or grade changes may be occurring. Regarding telephone survey methodology, epidemiological data indicate that only 7.3% of US children lived in households without a landline phone (i.e., households that had only cellular service or no phone service) in the first half of 2005 (Blumberg & Luke, 2007), which was the year of initial study recruitment. It should be noted that this national percentage increased over the study period, with 16.5% of children living in households without landlines by the second half of 2007 (Blumberg & Luke, 2009). Thus, although the exclusion of adolescents living in households without land- lines has the potential to bias results, this issue was more prevalent during the latter part of the study, when it would have a greater influence on attrition (see previous discussion) than recruitment.
Third, third variable explanations for our finding that early depressive symptoms predict and temporally precede future polysubstance use cannot be ruled out conclusively, despite our control for gender, ethnicity, household income, and early polysubstance use. Future studies of the cascading interrelation between adolescent depressive symptoms and polysubstance use would benefit from assessment of a wider variety of systems, including biological factors, parental and peer influences, and other risky behaviors. For example, it will be important for future research to consider the role of puberty, given the notable associations among substance use, depression, and normative pubertal development occurring during the adolescent developmental period (e.g., Graber, 2013; Lanza & Collins, 2002; Wiesner & Ittel, 2002). In addition, recent research has suggested a complex pattern of relations that emerges when considering the role of externalizing problems in the association between depressive symptoms and illicit drug abuse. Specifically, externalizing behaviors, such as oppositional defiance and hyperactivity, may moderate the relation between depressive symptoms and substance use, such that children with co-occurring depressive symptoms and externalizing problems may be at the greatest risk for the onset of drug use (e.g., Colder et al., 2013). Future research should include assessment of behavioral problems to further explore possible interactive relations.
Clinical and research implications
The current study indicates that polysubstance use in adolescence conveys increased risk for concurrent depressive symptoms and that these depressive symptoms in turn convey increased risk for future polysubstance use (which in turn conveys additional risk for future depressive symptoms), even after accounting for early substance use, gender, ethnicity, and household income. This pattern of findings fails to provide evidence for a straightforward temporal precedence of either polysubstance use or depressive symptoms over this important developmental period. Instead, the current results suggest a developmental cascade, in which symptoms of one disorder promote symptoms of the other. Although we only examined a small subset of what is likely a complex pattern of interrelations among many constructs, this study provides initial evidence for a new, more comprehensive model of the co-occurrence of depressive symptoms and polysubstance use. This study is also among the first to examine the important role of polysubstances in changes in depressive symptoms. Given that polysubstance use is associated with a significantly greater number of negative outcomes than single-substance use (e.g., Kirisci et al., 2002), these results represent an important first step in understanding the development of this important risk factor. In light of these findings, it is recommended that clinicians screen for depressive symptoms and polysubstance use when adolescents present for treatment and, when detected, target these risk factors through the delivery of evidence-based interventions.
The results from this community sample suggest that treating depressive symptoms may decrease the risk of future polysubstance use, whereas treating current polysubstance use may impact concurrent depressive symptoms. Moreover, our findings support the notion that identifying younger adolescents with depressive symptoms may increase the efficacy of substance use prevention programs and protect against the onset of illicit drug use across middle and late adolescence. Recent research examining the efficacy of secondary prevention programs targeting personality vulnerabilities in adolescence have yielded promising results (e.g., Conrod, Stewart, Comeau, & Maclean, 2006); given the important link between early depression and later substance use, prevention efforts that target depressive symptoms specifically are warranted. Further, future research with adolescents should focus also on identifying additional mechanisms through which depressive symptoms convey increased risk for future polysubstance use, and vice versa. Another area for future research is the exploration of co-occurring depressive symptoms, polysubstance use, additional high-risk behaviors (e.g., delinquent behavior and high risk sexual behavior; Beyers & Loeber, 2003; Kofler et al., 2011), exposure to interpersonal trauma (McCart et al., 2011), and treatment effects (McKowen, Tompson, Brown, & Asarnow, 2013), all of which are likely mechanisms through which depressive symptoms and polysubstance use interact developmentally.
Acknowledgments
This research was partially supported by a grant from the National Institute of Child Health and Human Development (Grant R01HD046830; D.G.K., primary investigator). Julia W. Felton was supported by Training Grant MH079670 from the National Institute of Mental Health during the completion of this work.
Footnotes
Allowing these slope weights to be estimated freely resulted in significantly improved model fit relative to forcing a linear solution for all models tested (all x2 difference test ps<.0005).
Community type was also tested as an ordered categorical variable based on distance from urban areas (0=urban, 1=suburban, 2=rural). The results were unchanged when this variable was substituted for the dichotomous categorical variable described above.
References
- Alderson RM, Rapport MD, Hudec K, Sarver DE, & Kofler MJ (2010). Competing core processes in attention-deficit/hyperactivity disorder (ADHD): Do working memory deficiencies underlie behavioral inhibition deficits? Journal of Abnormal Child Psychology, 38, 497–507. [DOI] [PubMed] [Google Scholar]
- Armstrong TD, & Costello EJ (2002). Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology, 70, 1224–1239. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111, 33–51. doi: 10.1037/0033-295x.111.1.33 [DOI] [PubMed] [Google Scholar]
- Barnett JH, Werners U, Secher SM, Hill KE, Brazil R, Masson K, et al. (2007). Substance use in a population-based clinic sample of people with first-episode psychosis. British Journal of Psychiatry, 190, 515–520. doi: 10.1192/bjp.bp.106.024448 [DOI] [PubMed] [Google Scholar]
- Begle AM, Hanson RF, Danielson CK, McCart MR, Ruggiero KJ, Amstadter AB, et al. (2011). Longitudinal pathways of victimization, substance use, and delinquency: Findings from the National Survey of Adolescents. Addictive Behaviors, 36, 682–689. doi: 10.1016/j.addbeh.2010.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyers JM, & Loeber R (2003). Untangling developmental relations between depressed mood and delinquency in male adolescents. Journal of Abnormal Child Psychology, 31, 247–266. [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, & Luke JV (2007). Coverage bias in traditional telephone surveys of low-income and young adults. Public Opinion Quarterly, 71, 734–749. [Google Scholar]
- Blumberg SJ, & Luke JV (2009). Reevaluating the need for concern regarding noncoverage bias in landline surveys. American Journal of Public Health, 99, 1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Adams RE, Ahern J, Resnick H, & Vlahov D (2004). Mental health service and medication use in New York after the September 11, 2001, terrorist attack. Psychiatric Services, 55, 274–283. doi: 10.1176/appi.ps.55.3.274 [DOI] [PubMed] [Google Scholar]
- Brook JS, Cohen P, & Brook DW (1998). Longitudinal study of co-occurring psychiatric disorders and substance use. Journal of the American Academy of Child & Adolescent Psychiatry, 37, 322–330. [DOI] [PubMed] [Google Scholar]
- Bukstein OG, Glancy LJ, & Kaminer Y (1992). Patterns of affective comorbidity in a clinical population of dually diagnosed adolescent substance abusers. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 1195–1203. [DOI] [PubMed] [Google Scholar]
- Byrne BM (2010). Structural equation modeling with AMOS (2nd ed.). New York: Routledge. [Google Scholar]
- Cantwell DP, Lewinsohn PM, Rhode P, & Seeley JR (1997). Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 610–619. doi: 10.1097/00004583-199705000-00011 [DOI] [PubMed] [Google Scholar]
- Capaldi DM (1992). Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. A 2-year follow-up at Grade 8. Development and Psychopathology, 4, 125–144. doi: 10.1017/S0954579400005605 [DOI] [PubMed] [Google Scholar]
- Chen P, & Jacobson KC (2012). Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. Journal of Adolescent Health, 50, 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinet L, Plancherel B, Bolognini M, Bernard M, Laget J, Daniele G, et al. (2006). Substance use and depression: Comparative course in adolescents. European Child and Adolescent Psychiatry, 15, 149–155. [DOI] [PubMed] [Google Scholar]
- Ciesla JR (2010). Evaluating the risk of relapse for adolescents treated for substance abuse. Addictive Disorders and Their Treatment, 9, 87–92. doi: 10.1097/ADT.0b013e3181b8cd05 [DOI] [Google Scholar]
- Clark DB, Pollock N, Bukstein OG, Mezzich AC, Bromberger JT, & Donovan JE (1997). Gender and comorbid psychopathology in adolescents with alcohol dependence. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 1195–1203. [DOI] [PubMed] [Google Scholar]
- Colder CR (2001). Life stress, physiological and subjective indexes of negative emotionality, and coping reasons for drinking: Is there evidence for a self-medication model of alcohol use? Psychology of Addictive Behaviors, 15, 237–245. [PubMed] [Google Scholar]
- Colder CR, Scalco M, Trucco EM, Read JP, Lengua LJ, Wieczorek WF, et al. (2013). Prospective associations of internalizing and externalizing problems and their co-occurrence with early adolescent substance use. Journal of Abnormal Child Psychology, 41, 667–677. doi: 10.1007/s10802-012-9701-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, & Maxwell SE (2003). Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112, 558–577. doi: 10.1037/0021-843x.112.4.558 [DOI] [PubMed] [Google Scholar]
- Cole DA, Tram JM, Martin JM, Hoffman KB, Ruiz MD, Jacquez FM, et al. (2002). Individual differences in the emergence of depressive symptoms in childhood and adolescence: A longitudinal investigation of parent and child reports. Journal of Abnormal Psychology, 111, 156–165. doi: 10.1037/0021-843X.111.1.156 [DOI] [PubMed] [Google Scholar]
- Conrod PJ, Stewart SH, Comeau N, & Maclean AM (2006). Efficacy of cognitive–behavioral interventions targeting personality risk factors for youth alcohol misuse. Journal of Clinical Child and Adolescent Psychology, 35, 550–563. [DOI] [PubMed] [Google Scholar]
- Conway KP, Vullo GC, Nichter B, Wang J, Compton WM, Iannotti RJ, et al. (2013). Prevalence and patterns of polysubstance use in a nationally representative sample of 10th graders in the United States. Journal of Adolescent Health, 52, 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6, 117–128. doi: 10.1037/1040-3590.6.2.117 [DOI] [Google Scholar]
- Cooper ML, Frone MR, Russell M, & Mudar P (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69, 990–1005. doi: 10.1037/0022-3514.69.5.990 [DOI] [PubMed] [Google Scholar]
- Costello EJ, Angold A, & Keeler GP (1999). Adolescent outcomes of childhood disorders: The consequences of severity and impairment. Journal of the American Academy of Child & Adolescent Psychiatry, 38, 121–128. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger H, & Angold A (2005). 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. Journal of the American Academy of Child & Adolescent Psychiatry, 44, 972–986. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, & Smith J (2007). Income, poverty, and health insurance coverage in the United States: 2006 (US Census Bureau Current Population Reports, Series P60–233). Washington, DC: US Government Printing Office. [Google Scholar]
- Deykin EY, Buka SL, & Zeena TH (1992). Depressive illness among chemically dependent adolescents. American Journal of Psychiatry, 149, 1341–1347. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, & Strycker LA (2006). An introduction to latent variable growth curve modeling (2nd ed.). Mahwah, NJ: Erlbaum. [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2009). Situational and generalised conduct problems and later life outcomes: Evidence from a New Zealand birth cohort. Journal of Child Psychology and Psychiatry, 50, 1084–1092. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2011). Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Social Psychiatry and Psychiatric Epidemiology, 46, 933–942. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, & Swain-Campbell N (2002). Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction, 97, 1123–1135. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, & Catalano RF (2008). Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychology of Addictive Behaviors, 22, 186–197. [DOI] [PubMed] [Google Scholar]
- Fox CL, Towe SL, Stephens RS, Walker DD, & Roffman RA (2011). Motives for cannabis use in high-risk adolescent users. Psychology of Addictive Behaviors, 25, 492–500. doi: 10.1037/a0024331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E, & Huang B (2002). Socioeconomic status, depressive symptoms, and adolescent substance use. Archives of Pediatrics and Adolescent Medicine, 156, 448. [DOI] [PubMed] [Google Scholar]
- Goodman E, Slap GB, & Huang B (2003). The public health impact of socioeconomic status on adolescent depression and obesity. American Journal of Public Health, 93, 1844–1850. doi: 10.2105/ajph.93.11.1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graber JA (2013). Pubertal timing and the development of psychopathology in adolescence and beyond. Hormones and Behavior, 64, 262–269. doi: 10.1016/j.yhbeh.2013.04.003 [DOI] [PubMed] [Google Scholar]
- Hallfors DD, Waller MW, Bauer D, Ford CA, & Halpern CT (2005). Which comes first in adolescence —Sex and drugs or depression? American Journal of Preventive Medicine, 29, 163–170. [DOI] [PubMed] [Google Scholar]
- Hesselbrock MN, & Hesselbrock VM (1997). Gender, alcoholism, and psychiatric comorbidity. In Wilsnach RW & Wilsnach SC (Eds.), Gender and alcohol: Individual and social perspectives (pp. 49–71). Rutgers, NJ: Rutgers Center of Alcohol Studies. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2011). Monitoring the Future national results on adolescent drug use: Overview of key findings, 2010 Ann Arbor, MI: University of Michigan, Institute for Social Research. [Google Scholar]
- Jolliffe D, Farrington DP, Hawkins JD, Catalano RF, Hill KG, & Kosterman R (2003). Predictive, concurrent, prospective and retrospective validity of self-reported delinquency. Criminal Behaviour and Mental Health, 13, 179–197. doi: 10.1002/cbm.541 [DOI] [PubMed] [Google Scholar]
- Kandel DB, Davies M, Karus D, & Yamaguchi K (1986). The consequences in young adulthood of adolescent drug involvement: An over-view. Archives of General Psychiatry, 43, 746–754. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Kazemian L, & Farrington DP (2005). Comparing the validity of prospective, retrospective, and official onset for different offending categories. Journal of Quantitative Criminology, 21, 127–147. [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best C, & Schnurr PP (2000). Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology, 68, 19–30. doi: 10.1037/0022-006X.68.1.19 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders B, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology, 71, 692–700. doi: 10.1037/0022-006X.71.4.692 [DOI] [PubMed] [Google Scholar]
- Kirisci L, Vanyukov M, Dunn M, & Tarter R (2002). Item response theory modeling of substance use: An index based on 10 drug categories. Psychology of Addictive Behaviors, 16, 290–298. [PubMed] [Google Scholar]
- Kofler MJ, McCart MR, Zajac K, Ruggiero KJ, Saunders BE, & Kilpatrick DG (2011). Depression and delinquency covariation in an accelerated longitudinal sample of adolescents. Journal of Consulting and Clinical Psychology, 79, 458–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, & Collins LM (2002). Pubertal timing and the onset of substance use in females during early adolescence. Prevention Science, 3, 69–82. doi: 10.1023/a:1014675410947 [DOI] [PubMed] [Google Scholar]
- Lembke A (2012). Time to abandon the self-medication hypothesis in patients with psychiatric disorders. American Journal of Drug and Alcohol Abuse, 38, 524–529. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, & Seeley JR (1995). Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child & Adolescent Psychiatry, 34, 510–519. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, & Seeley JR (1998). Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review, 18, 765–794. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Coffey C, Degenhardt L, Carlin JB, & Patton G (2003). A longitudinal study of the effects of adolescent cannabis use on high school completion. Addiction, 98, 685–692. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR (2009). Longitudinal associations between alcohol problems and depressive symptoms: Early adolescence through early adulthood. Alcoholism: Clinical and Experimental Research, 33, 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez P, & Richters JE (1993). The NIMH community violence project: II. Children’s distress symptoms associated with violence exposure. In Reiss D & Ritchers JE (Eds.), Children and violence (pp. 21–34). New York: Guilford Press. [DOI] [PubMed] [Google Scholar]
- Mason WA, Hitchings JE, & Spoth RL (2007). Emergence of delinquency and depressed mood throughout adolescence as predictors of late adolescent problem of substance use. Psychology of Addictive Behaviors, 21, 13–24. [DOI] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and Psychopathology, 22, 491–495. [DOI] [PubMed] [Google Scholar]
- Masten AS, Roisman G, Long J, Burt K, Obradovic J, Riley JR, et al. (2005). Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology, 41, 733–746. [DOI] [PubMed] [Google Scholar]
- McCart MR, Zajac K, Danielson CK, Strachan M, Ruggiero KJ, Smith DW, et al. (2011). Interpersonal victimization, posttraumatic stress disorder, and change in adolescent substance use prevalence over a ten-year period. Journal of Clinical Child and Adolescent Psychology, 40, 136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy DE, Curtin JJ, Piper ME, & Baker TB (2010). Negative reinforcement: Possible clinical implications of an integrative model. In Kassel JD (Ed.), Substance abuse and emotion Washington, DC: American Psychological Association. [Google Scholar]
- McKowen JW, Tompson MC, Brown TA, & Asarnow JR (2013). Longitudinal associations between depression and problematic substance use in the Youth Partners in Care study. Journal of Clinical Child and Adolescent Psychology Advance online publication. doi: 10.1080/15374416.2012.759226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Needham BL (2007). Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Social Science and Medicine, 65, 1166–1179. doi: 10.1016/j.socscimed.2007.04.037 [DOI] [PubMed] [Google Scholar]
- Newcomb MD, & Bentler PM (1988). Impact of adolescent drug use and social support on problems of young adults: A longitudinal study. Journal of Abnormal Psychology, 97, 64–75. [DOI] [PubMed] [Google Scholar]
- O’Neil KA, Conner BT, & Kendall PC (2011). Internalizing disorders and substance use disorders in youth: Comorbidity, risk, temporal order, and implications for intervention. Clinical Psychology Review, 31, 104–112. [DOI] [PubMed] [Google Scholar]
- Paternoster R, Mazerolle P, & Piquero A (1998). Using the correct statistical test for the equality of regression coefficients. Criminology, 36, 859–866. [Google Scholar]
- Rao U, Daley SE, & Hammen C (2000). Relationship between depression and substance use disorders in adolescent women during the transition to adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 215–222. [DOI] [PubMed] [Google Scholar]
- Repetto PB, Zimmerman MA, & Caldwell CH (2008). A longitudinal study of depressive symptoms and marijuana use in a sample of inner-city African Americans. Journal of Research on Adolescence, 18, 421–447. [Google Scholar]
- Rohde P, Beevers CG, Stice E, & O’Neil K (2009). Major and minor depression in female adolescents: Onset, course, symptom presentation, and demographic associations. Journal of Clinical Psychology, 65, 1339–1349. doi: 10.1002/jclp.20629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, & Kaufman NK (2001). Impact of comorbidity on a cognitive–behavioral group treatment for adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry, 40, 795–802. [DOI] [PubMed] [Google Scholar]
- Saules KK, Pomerleau CS, Snedecor SM, Mehringer AM, Shadle MB, Kurth C, et al. (2004). Relationship of onset of cigarette smoking during college to alcohol use, dieting concerns, and depressed mood: Results from the Young Women’s Health Survey. Addictive Behaviors, 29, 893–899. [DOI] [PubMed] [Google Scholar]
- Schuckit MA (2006). Comorbidity between substance use disorders and psychiatric conditions. Addiction, 101, 76–88. [DOI] [PubMed] [Google Scholar]
- Schweizer K (2010). Some guidelines concerning the modeling of traits and abilities in test construction. European Journal of Psychological Assessment, 26, 1–2. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Smit F, Monshouwer K, & Verdurmen J (2002). Polydrug use among secondary school students: Combinations, prevalences and risk profiles. Drugs: Education, Prevention, and Policy, 9, 355–365. [Google Scholar]
- Stice E, Burton EM, & Shaw H (2004). Prospective relations between bulimic pathology, depression, and substance abuse: Unpacking comorbidity in adolescent girls. Journal of Consulting and Clinical Psychology, 72, 62–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svensson R (2003). Gender differences in adolescent drug use: The impact of parental monitoring and peer deviance. Youth and Society, 34, 300–329. doi: [DOI] [Google Scholar]
- Trenz RC, Scherer M, Harrell P, Zur J, Sinha A, & Latimer W (2012). Early onset of drug and polysubstance use as predictors of injection drug use among adult drug users. Addictive Behaviors, 37, 367–372. doi: 10.1016/j.addbeh.2011.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall GK, & Azevedo K (2007). Longitudinal effects of a universal family-focused intervention on growth patterns of adolescent internalizing symptoms and polysubstance use: Gender comparisons. Journal of Youth and Adolescence, 36, 725–740. [Google Scholar]
- Turner HA, Finkelhor D, & Ormrod R (2006). The effect of lifetime victimization on the mental health of children and adolescents. Social Science and Medicine, 62, 13–27. [DOI] [PubMed] [Google Scholar]
- Twenge JM, & Nolen-Hoeksema S (2002). Age, gender, race, socioeconomic status, and birth cohort, difference on the children’s depression inventory: A meta-analysis. Journal of Abnormal Psychology, 111, 578–588. [DOI] [PubMed] [Google Scholar]
- Waller MW, Hallfors DD, Halpern CT, Iritani BJ, Ford CA, & Guo G (2006). Gender differences in associations between depressive symptoms and patterns of substance use and risky sexual behavior among a nationally representative sample of U.S. adolescents. Archives of Women’s Mental Health, 9, 139–150. [DOI] [PubMed] [Google Scholar]
- White AM, Jordan JD, Schroeder KM, Acheson SK, Georgi BD, Sauls G, et al. (2004). Predictors of relapse during treatment and treatment completion among marijuana-dependent adolescents in an intensive outpatient substance abuse program. Substance Abuse, 25, 53–59. [DOI] [PubMed] [Google Scholar]
- Wiesner M, & Ittel A (2002). Relations of pubertal timing and depressive symptoms to substance use in early adolescence. Journal of Early Adolescence, 22, 5–23. doi: 10.1177/0272431602022001001 [DOI] [Google Scholar]
- Wilker A (1948). Recent progress in research on the neurophysiologic basis of morphine addiction. American Journal of Psychiatry, 105, 329–338. [DOI] [PubMed] [Google Scholar]
- Windle M, & Windle RC (2001). Depressive symptoms and cigarette smoking among middle adolescents: Prospective associations and intra- personal and interpersonal influences. Journal of Consulting and Clinical Psychology, 69, 215–226. [PubMed] [Google Scholar]
- Wolff JC, & Ollendick TH (2006). The comorbidity of conduct problems and depression in childhood and adolescence. Clinical Child and Family Psychology Review, 9, 201–220. [DOI] [PubMed] [Google Scholar]
- Wu L-T, Woody GE, Yang C, Pan J-J, & Blazer DG (2011). Racial/ ethnic variations in substance-related disorders among adolescents in the United States. Archives of General Psychiatry, 68, 1176–1185. doi: 10.1001/archgenpsychiatry.2011.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapert K, Snow DL, & Tebes JK (2002). Patterns of substance use in early through late adolescence. American Journal of Community Psychology, 30, 835–852. [DOI] [PubMed] [Google Scholar]