Abstract
OBJECTIVE
We examined whether the experience of a “pregnancy scare” is related to subsequent changes in contraceptive use that increase the risk of unintended pregnancy.
METHODS
We used data from the Relationship Dynamics and Social Life (RDSL) study, which interviewed a random, population-based sample of 1,003 young women weekly for 2.5 years. We used multivariate regression models to predict the effect of experiencing a pregnancy scare on change in contraceptive use.
RESULTS
We found pregnancy scares are associated with changes in contraceptive use that increase the risk of pregnancy. Experiencing a pregnancy scare is related to discontinued contraceptive use, change from consistent to inconsistent use of contraception, and change from a more effective to a less effective method of contraception. We also found pregnancy scares are associated with continued inconsistent use of contraception.
CONCLUSIONS
Our findings suggest that the experience of a pregnancy scare does not serve as a “wake-up call” to start using contraception, to start using it consistently, or to switch to a more effective method to reduce the risk of unintended pregnancy. Instead, contraceptive use after a pregnancy scare typically remains the same or worsens.
IMPLICATIONS
Clinicians should be aware that young women who have experienced pregnancy scares may be at increased risk of unintended pregnancy, relative to young women who did not experience a pregnancy scare.
1. Introduction
The rate of unintended pregnancy in the U.S. remains persistently high [1], and is unlikely to decrease without new policy or interventions. In particular, a more comprehensive understanding of the precursors of unintended pregnancy is essential to formulate new approaches that reduce the unintended pregnancy rate [2]. This study explores one possible pathway - the relationship between experiencing a pregnancy scare and subsequent changes in contraceptive use.
The term “pregnancy scare” describes when a woman who wants to avoid pregnancy believes she is pregnant, but later learns that she is not. According to national surveys, more than half of young women experience a pregnancy scare [3,4]. Women from less advantaged backgrounds are more likely to experience a pregnancy scare than those from more advantaged backgrounds [5], and the demographic correlates of pregnancy scares are similar to the demographic correlates of unintended pregnancy [5,6]. Furthermore, experiencing a pregnancy scare is strongly associated with subsequent unintended pregnancy, independent of background factors [5,7].
Although it seems possible that a pregnancy scare would be a “wake-up call” to start using contraception or to switch to a more effective method, the positive association between a pregnancy scare and later unintended pregnancy does not support this theory. Or, if a pregnancy scare is in fact a “wake-up call”, any improvement in contraceptive use is only temporary. It could even be that experiencing a pregnancy scare increases pregnancy desire, or increases tolerance of an undesired pregnancy, so that women become less likely to use contraception or more likely to switch to a less-effective method. That is, even women who wanted to avoid pregnancy quickly adjust their feelings to be more positive about pregnancy when they think they are probably pregnant, and those feelings remain positive to some degree even after they realize they are not actually pregnant. Of course, there is also the possibility that experiencing a pregnancy scare is not related to any change in contraceptive use at all.
In this study we estimate the effect of experiencing a pregnancy scare on subsequent changes in: 1) contraceptive use; 2) consistency of contraceptive use; and 3) effectiveness of the contraceptive method used.
2. Methods
We use data from the Relationship Dynamics and Social Life (RDSL) study, which interviewed a random, population-representative sample of 1,003 young women ages 18–19, residing in a Michigan county. The RDSL study selected women from the state driver’s license and personal identification card databases. Professional interviewers conducted a 60-minute face-to-face baseline survey between March 2008 and July 2009. Women then participated in a 2.5-year follow-up study consisting of brief weekly online or telephone surveys about contraceptive use, relationships, and pregnancy. The follow-up study concluded in 2012 and yielded 58,594 weekly interviews. The response rate for the baseline interview was 84%, 99% of baseline respondents participated in the follow-up study, and 75% participated for at least 18 months. Of the 953 women who completed more than one follow-up interview, 604 (63%) completed their final interview at 900 or more days after enrollment (2.47 years). The study was approved by the University of Michigan’s Institutional Review Board.
In this study, we analyze the weeks in which women had sexual intercourse. The result is an analytic sample of 16,737 interviews with 702 women. We compare change in contraceptive use between interviews with an intervening pregnancy scare and change in contraceptive use between adjacent interviews that were completed without an intervening pregnancy scare. That is, change in contraceptive use from the interview before a pregnancy scare to the interview after a pregnancy scare is compared to typical week-to-week change in contraceptive use. We use the interview before the scare because a young woman’s recent discovery that she might be pregnant may have affected her contraceptive use leading up to the report of the pregnancy scare. We use the interview after the scare in order to measure immediate change in contraceptive use. However, we also conducted sensitivity analyses using the interviews at the 2nd, 3rd, and 4th weeks after the scare. These analyses were necessary because we do not know exactly when it became clear to the respondent that she was not really pregnant, and there is the possibility that it takes women longer than one week to adjust their contraceptive use in reaction to a pregnancy scare.
2.1. Dependent Variables
Change in contraceptive use.
Each week, respondents were asked “did you use or do anything that can help people avoid becoming pregnant, even if you did not use it to keep from getting pregnant yourself?” Based on this question at the before and after interview (or week 1 and week 2 in the comparison group), respondents were coded as 1) continued use (use before, use after); 2) discontinued use (use before, no use after); 3) continued non-use (no use before, no use after); or 4) began using (no use before, use after).
Change in consistency of contraceptive use.
Each week, respondents who used a contraceptive method were asked “did you or your partner(s) use some method of birth control every time you had intercourse (even if you are not trying to prevent pregnancy)? This could be a method you mentioned earlier, or a method you haven’t mentioned such as condoms, pills, or another method.” Based on the response to this question provided in both weeks, respondents were coded as 1) continued consistent use (consistent before, consistent after); 2) became inconsistent (consistent before, inconsistent after); 3) continued inconsistent use (inconsistent before, inconsistent after); or 4) became consistent (inconsistent before, consistent after).
Change in effectiveness of contraceptive method used.
Each week, respondents who used contraception were asked a series of yes/no questions regarding their use of specific contraceptive methods. These methods included non-coital types (birth control pills, birth control patch, NuvaRing, Depo-Provera or any other type of contraceptive shot, Implanon or another contraceptive implant, IUD, or avoidance of sex during a time of the month that the respondent could get pregnant) and coital types (condom, diaphragm or cervical cap, spermicide, female condom, or withdrawal). For this study, we combine the contraceptive methods into the following mutually exclusive categories, listed from more to less effective: (a) IUD, implant, or Depo-Provera (referred to as LARC/Injectable hereafter), (b) birth control pills, birth control patch, or NuvaRing (referred to as Pill/Other Hormonal hereafter), (c) condom only, and (d) withdrawal only. Contraceptive methods were included in the more effective pregnancy-prevention category when multiple methods were reported (e.g., weeks of condom and birth control pills were grouped as Pill/Other Hormonal). Based on the contraceptive method at the before and after interview (or week 1 and week 2 for the comparison group), respondents were coded as 1) switched to more effective method; 2) switched to less effective method; or 3) continued same method or effectiveness. Change in dual method use is also accounted for in this measure. That is, a respondent that used the same method is coded as switched to a more or less effective method if a second method was added or subtracted.
2.2. Independent Variables
Pregnancy scare.
Each week, respondents were asked about their pregnancy status, and were coded as “not pregnant,” “probably not pregnant,” “probably pregnant,” or “pregnant.” “Pregnant” is defined as a positive pregnancy test (self-reported). An uncertain reply of “probably not pregnant” or “probably pregnant” that was not subsequently confirmed by a pregnancy test (or, eventually, a birth, miscarriage, or abortion) is considered a “pregnancy scare” if the pregnancy was not desired. The variable is dichotomous where 1=pregnancy scare and 0=otherwise.
Note that we used two weekly time-varying prospective questions to define when women were at risk of undesired pregnancy. The first question asked respondents how much they wanted to get pregnant during the next month. The second question asked respondents how much they wanted to avoid getting pregnant during the next month. Both questions used a response scale from 0 to 5. All pregnancy scares occurred to respondents during weeks when they reported anything other than the strongest desire to become pregnant and the weakest desire to avoid pregnancy. We also conducted sensitivity analyses with a stricter definition of undesired where pregnancy scares could occur only to women with the weakest desire for pregnancy and the strongest desire to avoid pregnancy. Another sensitivity analysis uses a version of the same two questions above, but in reference to the respondent’s current partner.
Respondent characteristics.
The RDSL study measured sociodemographic and other personal characteristics during the baseline interview. We created dichotomous variables from these measures. We coded respondents who reported a high school Grade Point Average (GPA) at or greater than one standard deviation below the mean as having a low high school GPA.
2.3. Data Analysis
First we calculated descriptive statistics for the independent variables at the respondent level for the total sample, as well as two subsamples: women who never experienced a pregnancy scare and women who experienced a pregnancy scare. We calculated the descriptive statistics for the dependent variables at the week level for the total sample and the two subsamples: weeks without a pregnancy scare and weeks with a pregnancy scare. Next we used regression models to estimate the effect of experiencing a pregnancy scare on change in contraceptive use reported before and after the pregnancy scare. We used two dichotomous dependent variables (logistic regression) indicating change in: 1) contraceptive use; 2) consistency of contraceptive use; and 3) a trichotomous variable indicating whether respondents switched to a more effective method, switched to a less effective method, or continued using the same method/a method of approximately the same effectiveness. Because person-weeks are the unit of analysis, and they are nested within women, all analyses were conducted using Stata/SE 15.1 with the cluster option, which adjusted the standard errors to account for this multilevel structure. For the first two dependent variables, we stratified the models by contraceptive use at the interview before the pregnancy scare (rather than using interaction terms) to more clearly illustrate whether contraceptive users and nonusers respond differently to a pregnancy scare (and consistent users versus inconsistent users in the models of change in consistency). All models controlled for respondent characteristics. For ease of interpretation, we present the results as predicted probabilities in Figures 1 through 3, holding the variables for respondent characteristics constant at their means. We present the results of the multinomial logistic regression models in the appendix.
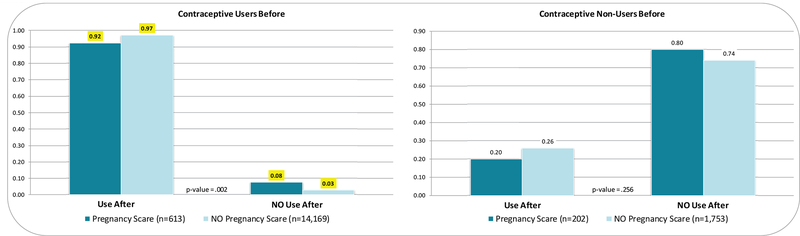
Figure 1.
Change in Contraceptive Use
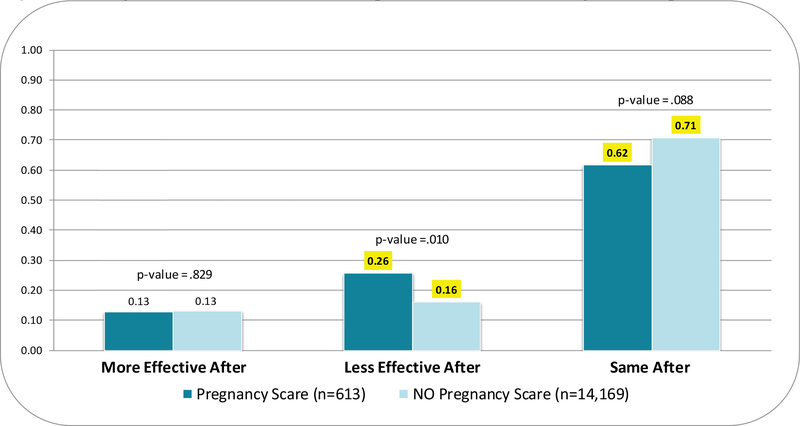
Figure 3.
Change in Effectiveness of Contraceptive Method Used among Contraceptive Users
3. Results
3.1. Respondent Characteristics
During the follow-up study, 33% (234/702) of the women in the sample reported a pregnancy scare, and among those who did, 49% experienced one pregnancy scare, 17% experienced two, and 34% experienced three or more. Table 1 shows that a third of the sample (33%) reported their race as African American. Over a third (37%) of the sample reported their mother was a teen parent, and 52% reported growing up without two parents. Nearly a quarter of the sample (21%) reported a low high school GPA. Age at first sex was 16 years or younger for 60% of the sample. At the time of the baseline interview, 68% of the sample reported having a total of two or more sexual partners in the past.
Table 1.
Respondent Characteristics and Change in Contraceptive Use
| Total Sample (n=702 women) | Women without pregnancy scares (n=468) | Women with pregnancy scares(n=234) | p-value | |
|---|---|---|---|---|
| Independent Variables | ||||
| Respondent Characteristics | ||||
| African American | .33 | .34 | .30 | |
| Biological mother <20 years old at 1st birth | .37 | .36 | .38 | |
| Non-two-parent childhood family structure | .52 | .53 | .51 | |
| Low high school GPA | .21 | .19 | .24 | |
| Age at first sex ≤ 16 years | .60 | .60 | .59 | |
| Two or more sexual partners | .68 | .66 | .72 |
| Total Sample (n=16,737 iws) | Interviews without pregnancy scares(n=15,922) | Interviews with pregnancy scares(n=815) | p-value | |
|---|---|---|---|---|
| Dependent Variables | ||||
| Change in Contraceptive Use | ||||
| Continued use | .85 | .86 | .69 | *** |
| Discontinued use | .03 | .03 | .07 | *** |
| Continued non-use | .09 | .08 | .20 | *** |
| Began using | .03 | .03 | .05 | ** |
| Change in Consistency of Contraceptive Use1 | ||||
| Continued consistent use | .72 | .73 | .55 | *** |
| Became inconsistent | .08 | .08 | .12 | *** |
| Continued inconsistent use | .14 | .14 | .27 | *** |
| Became consistent | .06 | .06 | .07 | |
| Change in Effectiveness of Contraceptive Method Used1 | ||||
| Switched to more effective method | .06 | .06 | .07 | |
| Switched to less effective method | .10 | .10 | .18 | *** |
| Continued same method or effectiveness | .83 | .84 | .73 | *** |
p < 0.10
p < 0.05
p < 0.01
p < 0.001 (two-tailed independent samples t-tests for significant differences between the two subsamples)
Among Contraceptive Users: Total Sample (n=691 women, 14,782 iws); Without pregnancy scares (n=466 women, 14,169 iws); With pregnancy scares (n=225 women, 613 iws)
3.2. Change in Contraceptive Use
Pregnancy scares were reported in 5% (815/16,737) of the interviews. Most of the time, respondents continued using contraception from week-to-week (85%). Respondents discontinued use in 3% of weeks, continued non-use in 9% of weeks, and began using contraception in 3% of weeks. Respondents reported continued consistent use from week-to-week in 72% of the interviews. Respondents became inconsistent in 8% of the weeks, continued their inconsistent use in 14% of weeks, and became consistent in 6% of weeks. Respondents switched to a more effective method in 6% of interviews, switched to a less effective method in 10% of interviews, and continued with the same method or a method of the same effectiveness in 83% of interviews. Overall, changes in contraceptive use associated with increased risk of pregnancy are overrepresented in the subsample of interviews with an intervening pregnancy scare, and continuing contraceptive use/consistency/effectiveness are overrepresented in non-pregnancy scare interviews. However, the initiation of contraceptive use is slightly overrepresented in interviews with an intervening pregnancy scare (5%) compared to interviews without an intervening pregnancy scare (3%).
3.3. Multivariate Models
Figure 1 summarizes the results of the multivariate models estimating the effect of experiencing a pregnancy scare on changes in contraceptive use. We present the predicted probabilities stratified for contraceptive users (on the left) and contraceptive non-users (on the right), for the interviews with an intervening pregnancy scare (darker blue) versus the interviews without an intervening pregnancy scare (lighter blue). Although the coefficients for users and non-users do not significantly differ for any of the models (based on interaction terms in pooled models), we present stratified models because the predicted probabilities are so different between the two groups. Among contraceptive users, young women who experienced a pregnancy scare were less likely than those who did not experience a pregnancy scare to continue use (92% vs. 97%) and correspondingly more likely to discontinue use (8% vs. 3%). Among contraceptive non-users, young women who experienced a pregnancy scare do not significantly differ from those who did not experience a pregnancy scare. Thus, among contraceptive users, pregnancy scares were associated with an increase in the risk of subsequent unintended pregnancy.
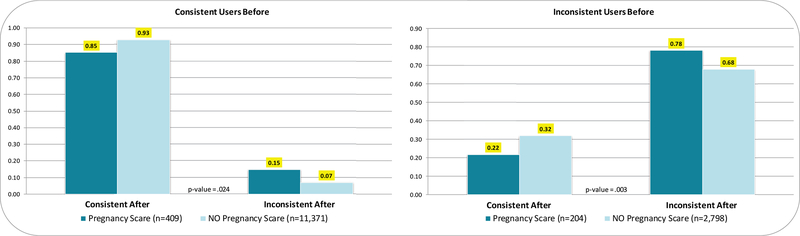
Figure 2 summarizes the multivariate models estimating the effect of experiencing a pregnancy scare on changes in consistency of contraceptive use. Among women who consistently used contraception, those who experienced a pregnancy scare were less likely to continue consistent use (85% vs. 93%) and more likely to become inconsistent (15% vs. 7%), relative to young women who did not experience a pregnancy scare. Among inconsistent contraception users, women who experienced a pregnancy scare were less likely to become consistent users (22% vs. 32%) than women who did not experience a pregnancy scare. Inconsistent contraception users who experienced a pregnancy scare were also more likely to remain inconsistent users (78% vs. 68%), relative to those who did not experience a pregnancy scare. Overall, both consistent and inconsistent users who experienced pregnancy scares experienced greater increase in unintended pregnancy risk than those who did not experience a pregnancy scare.
Figure 2.
Change in Consistency of Contraceptive Use among Contraceptive Users
Figure 3 summarizes the multivariate models estimating the relationship between experiencing a pregnancy scare and changes in the effectiveness of the contraceptive method used. Young women who experienced a pregnancy scare were nearly twice as likely to switch to a less effective method (26% vs. 16%), and correspondingly less likely to continue using a method of the same effectiveness (62% vs. 71%), relative to women who did not experience a pregnancy scare.
Overall, young women who experience a pregnancy scare experience a clinically significant increase in unintended pregnancy risk. Contraceptive users, who are a much larger group of young women than contraceptive nonusers (e.g., 88% of the total week-level sample includes contraceptive use), are more likely to be in contact with clinicians than non-users. Our models estimate that 8% of contraceptive users will become non-users, 15% of consistent users will become inconsistent users, and 26% of contraceptive users will switch to a less effective method after a pregnancy scare. Clinicians who encounter contraceptive non-users who have recently experienced a pregnancy scare – perhaps for regular health screening or pregnancy/sexually transmitted infection (STI) testing – have an even bigger opportunity to reduce pregnancy risk in this population. Our models estimate that 80% of non-users will remain non-users after a pregnancy scare.
3.4. Sensitivity Analyses
First, we conducted sensitivity analyses for all three dependent variables using the interviews at the 2nd, 3rd, and 4th weeks after the pregnancy scare to compare to contraceptive use the week before the pregnancy scare. The coefficients in all but one of these analyses were significant and in the same direction as those presented in the figures and appendix tables. The model predicting consistent contraceptive use 4 weeks after the pregnancy scare among the inconsistent users was the only exception. The results were in the same direction, but the coefficient for experiencing a pregnancy scare was no longer significant. Thus, the increased risk of unintended pregnancy continues beyond the first week after the pregnancy scare, through at least the first month.
Second, we compared women who had only one pregnancy scare to women who had no pregnancy scares. Again, the results were similar in terms of statistical significance and direction as those presented in the figures. However, in the model replicating Figure 2/Appendix Table 2 for the inconsistent users, the association between experiencing a pregnancy scare and change in consistent contraceptive use is no longer significant. This may be due to the dramatically reduced sample size and the resulting reduced power to detect differences. Nonetheless, even women who experienced only one pregnancy scare changed their contraceptive use in ways that increased their risk of pregnancy.
Third, we used a stricter definition of pregnancy scares, as occurring only when young women reported zero desire to become pregnant and the strongest possible desire to avoid pregnancy. Again, the results were very similar, with two exceptions. In the models replicating Figure 1/Appendix Table 1, the contraceptive non-users who experienced a pregnancy scare were more likely to begin using and less likely to continue non-use than those who didn’t experience a pregnancy scare. That is, the contraceptive non-users who most strongly wanted to avoid pregnancy decreased their subsequent risk of unintended pregnancy. In the models replicating Figure 3/Appendix Table 3, the association between experiencing a pregnancy scare and use of the same contraceptive method is no longer significant. However, again due to the reduced sample size, our power to detect differences in these models is low. Subsequent research should use larger samples to verify this result.
Fourth, we re-defined pregnancy scares based on pregnancy desire with the current partner rather than pregnancy desire in general. The coefficients in all of these analyses were significant and in the same direction as those presented in the figures and appendix tables.
Fifth, we re-defined pregnancy scares as occurring only to respondents who believed they were “probably pregnant” (eliminating those who thought they were possibly, but “probably not” pregnant). We were unable to estimate stratified models due to the reduced sample size, but the results were consistent with the stratified models.
Lastly, to explore whether women who experienced a pregnancy scare use abstinence as a method of pregnancy prevention, we estimated models of the effect of a pregnancy scare on whether women had sexual intercourse in subsequent weeks. Women with pregnancy scares were not less likely to have sex in the 1st, 2nd, 3rd, or 4th weeks following a pregnancy scare, compared to women who did not experience a pregnancy scare.
4. Discussion
Pregnancy scares are associated with changes in contraceptive use that increase the risk of unintended pregnancy. These results suggest that a pregnancy scare is not a “wake-up call” to start using contraception, to increase contraceptive consistency, or to switch to a more effective method. Furthermore, these changes in contraceptive use occurred in the very short-term – the week after the pregnancy scare, when memory of the scare is still likely strong – as well as in the longer-term – at least four weeks after the pregnancy scare. Thus, contraceptive users who experienced pregnancy scares experienced increased unintended pregnancy risk, relative to young women who did not experience a pregnancy scare. The effect of experiencing a pregnancy scare on subsequent change in contraceptive use among contraceptive non-users is less clear. More research is needed to better understand how pregnancy scares affect women who are not using contraception.
It is also important to note that most women continued the same contraceptive behavior between interviews with an intervening pregnancy scare and between adjacent interviews without an intervening pregnancy scare. That is, most of the time respondents continued using or not using contraception, they continued using contraception consistently or inconsistently, and they continued using the same contraceptive method, whether they experienced a pregnancy scare or not.
It is beyond the scope of the current study to explore why contraceptive use after a pregnancy scare worsens, but future research should examine whether pregnancy desire, attitudes toward contraception, or perceptions of infertility change after this experience. It is possible that pregnancy scares normalize the experience of pregnancy, and may even increase desire for pregnancy. It is also possible that pregnancy scares decrease confidence in contraception or increase self-perceptions of subfecundity, which in turn affects contraceptive behavior. Adolescents who perceive themselves as unable to conceive use contraceptives less frequently than other adolescents [9].
It could also be that the experience of a pregnancy scare worsens contraceptive use through strengthening fatalistic beliefs about pregnancy. It is not uncommon for women to believe that pregnancy “just happens” or is “just meant to be” [10–14]. Women with fatalistic beliefs tend to use contraception less [13,15] and tend to use less effective methods when they do use contraception [16]. A woman with fatalistic beliefs may interpret a pregnancy scare as a “sign” indicating that her time to become pregnant has arrived, even if she does not want to become pregnant.
This study has several limitations. The single county sample design may decrease the generalizability of the results. The sample does, however, hold constant the geographic differences that may influence pregnancy scares and contraceptive use, as well as geographic factors (e.g., media, policy, etc.) that are not a focus in this study. There are very few Latinas in the county, and in our sample, so this precludes assessing them as a separate category. Our measure of pregnancy scare is not particularly detailed, and respondents’ concern about their pregnancy status may vary substantially. Lastly, the question about consistency of contraceptive use is vague. Although it lists specific possible methods (“condoms, pills, or another method”), it also uses the term “birth control,” which could be interpreted differently by different respondents.
Understanding how pregnancy scares are related to change in contraceptive use can inform the development of new strategies to reduce the rate of unintended pregnancy. One fourth of adolescent girls who have a negative pregnancy test may be identified by the healthcare system in time to prevent early childbearing through counseling [8]. Such counseling increases contraceptive use [17,18], particularly when it is personalized [19]. Asking young women about recent pregnancy scares has the potential to help clinicians identify patients who may be at increased risk of unintended pregnancy and may benefit from counseling or some other kind of intervention. Future studies should collect survey data with more complete measures of the pregnancy scare experience, and qualitative data to better understand the dynamics of pregnancy scares and subsequent changes in contraceptive use from the perspectives of women. This knowledge could lead to new and effective approaches to reduce the rate of unintended pregnancy in the U.S.
Acknowledgements
This research was supported by grants from the National Institute of Child Health and Human Development (NICHD) (R01 HD050329, R01 HD050329-S1, PI Barber; R01-HD078412, PI Guzzo) and a population center grant from the NICHD to the University of Michigan’s Population Studies Center (P2CHD041028). We gratefully acknowledge the Survey Research Operations (SRO) unit at the Institute for Social Research for their help with the data collection, particularly Vivienne Outlaw, Sharon Parker, and Meg Stephenson. We also gratefully acknowledge the contributions of the other members of the original RDSL team, including William Axinn, Mick Couper, and Steven Heeringa, as well as the Advisory Committee: Larry Bumpass, Elizabeth Cooksey, Kathie Harris, and Linda Waite.
Appendix
Appendix Table 1.
Logistic Regression Models of the Effect of a Pregnancy Scare on Contraceptive Use, Stratified for Contraceptive Users and Non-Users (n=702 women)
| Contraceptive Users Before | Contraceptive Non-Users Before | |
|---|---|---|
| Independent Variables | ||
| Pregnancy scare experience | −1.04*** (0.21) | −0.34 (0.32) |
| African American | −0.33 (0.20) | 0.28 (0.25) |
| Biological mother <20 years old at 1st birth | −0.06 (0.18) | 0.12 (0.24) |
| Non-two-parent childhood family structure | 0.38* (0.18) | −0.03 (0.26) |
| Low high school GPA | −0.55** (0.21) | −0.34 (0.27) |
| Age at first sex ≤ 16 years | −0.47* (0.20) | 0.28 (0.33) |
| Two or more sexual partners | −0.11 (0.23) | −0.19 (0.37) |
Notes: Coefficients are effects on log-odds. Standard errors in parentheses.
p<0.10
p<0.05
p<0.01
p<0.001 (two-tailed tests)
Appendix Table 2.
Logistic Regression Models of the Effect of a Pregnancy Scare on Consistent Contraceptive Use Among Contraceptive Users, Stratified for Consistent and Inconsistent Contraceptive Users (n=691 women)
| Consistent Users Before | Inconsistent Users Before | |
|---|---|---|
| Independent Variables | ||
| Pregnancy scare experience | −0.83** (0.27) | −.53** (.20) |
| African American | −0.55** (0.18) | −.03 (.18) |
| Biological mother <20 years old at 1st birth | −0.29+ (0.15) | −.14 (.17) |
| Non-two-parent childhood family structure | 0.30+ (0.16) | .08 (.16) |
| Low high school GPA | −0.34+ (0.20) | −.24 (.17) |
| Age at first sex ≤ 16 years | −0.07 (0.19) | .10 (.19) |
| Two or more sexual partners | −0.23 (0.19) | −.33 (.22) |
Notes: Coefficients are effects on log-odds. Standard errors in parentheses.
p<0.10
p<0.05
p<0.01
p<0.001 (two-tailed tests)
Appendix Table 3.
Multinomial Logistic Regression Models of the Effect of a Pregnancy Scare on Effectiveness of Contraceptive Method Used Among Contraceptive Users (n=691 women)
| Switched to more effective method | Switched to less effective method | |
|---|---|---|
| (Reference: Continued same method or effectiveness) | ||
| Independent Variables | ||
| Pregnancy scare experience | .10 (.26) | .61** (.23) |
| African American | .36** (.11) | .39*** (.11) |
| Biological mother <20 years old at 1st birth | −.01 (.11) | .05 (.10) |
| Non-two-parent childhood family structure | −.17+ (.10) | −.21* (.10) |
| Low high school GPA | −.20 (.15) | −.01 (.14) |
| Age at first sex ≤ 16 years | −.03 (.12) | .04 (.12) |
| Two or more sexual partners | .10 (.13) | .13 (.12) |
Notes: Coefficients are effects on log-odds. Standard errors in parentheses.
p<0.10
p<0.05
p<0.01
p<0.001 (two-tailed tests)
References
- [1].Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Casterline JB, Sinding SW. Unmet need for family planning in developing countries and implications for population policy. Popul Dev Rev. 2000;26:691–723. [Google Scholar]
- [3].Hoff T, Greene L, Davis J. National survey of adolescents and young adults: Sexual health knowledge, attitudes and experiences. California: The Henry J. Family Foundation; 2003. [Google Scholar]
- [4].National Campaign to Prevent Teen and Unplanned Pregnancy. Contraception calling: why aren’t more young women listening?. https://thenationalcampaign.org/resource/contraception-calling;2013. [accessed 27 July 2017].
- [5].Gatny H, Kusunoki Y, Barber J. Pregnancy scares and subsequent unintended pregnancy. Demogr Res. 2014;31:1229–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Halpern CT, Lich KH, Anderson S. Demographic correlates of U.S. pregnancy scares from 2006–2013. Paper presented to Population Association of American Annual Meeting Chicago, IL; 2017. [Google Scholar]
- [7].Zabin LS, Emerson MR, Ringers PA, Sedivy V. Adolescents with negative pregnancy test results: an accessible at-risk group. JAMA. 1996;275:113–7. [PubMed] [Google Scholar]
- [8].Rainey DY, Stevens-Simon C, Kaplan DW. Self-perception of infertility among female adolescents. Am J Dis Child. 1993;147:1053–6. [DOI] [PubMed] [Google Scholar]
- [9].Borrero S, Nikolajski C, Steinberg JR, Freedman L, Akers AY, Ibrahim S, et al. “It just happens”: a qualitative study exploring low-income women’s perspectives on pregnancy intention and planning. Contraception. 2015;91:150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Higgins JA, Popkin RA, Santelli JS. Pregnancy ambivalence and contraceptive use among young adults in the United States. Perspect Sex Reprod Health. 2012;44:236–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jones RK, Frohwirth LF, Blades NM. “If I know I am on the pill and I get pregnant, it’s an act of God”: women’s views on fatalism, agency and pregnancy. Contraception. 2016;93:551–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jones RK, Tapales A, Lindberg LD, Frost J. Using longitudinal data to understand changes in consistent contraceptive use. Perspect Sex Reprod Health. 2015;47:131–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Moos M-K, Petersen R, Meadows K, Melvin CL, Spitz AM. Pregnant women’s perspectives on intendedness of pregnancy. Womens Health Issues. 1997;7:385–92. [DOI] [PubMed] [Google Scholar]
- [14].Frost Jennifer J, Singh Susheela, Finer Lawrence B. Factors associated with contraceptive use and nonuse, United States, 2004. Perspect Sex Reprod Health. 2007;39:90–9. [DOI] [PubMed] [Google Scholar]
- [15].Frost Jennifer J, Darroch Jacqueline E Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sex Reprod Health. 2008;40:94–104. [DOI] [PubMed] [Google Scholar]
- [16].Lee JK, Parisi SM, Akers AY, Borrerro S, Schwarz EB. The impact of contraceptive counseling in primary care on contraceptive use. J Gen Intern Med. 2011;26:731–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Liu J, Shen J, Diamond-Smith N. Predictors of DMPA-SC continuation among urban Nigerian women: the influence of counseling quality and side effects. Contraception 2018. [cited 2018 Apr 20]; Available from: https://www.contraceptionjournal.org/article/S0010-7824(18)30152-5/fulltext] [DOI] [PMC free article] [PubMed]
- [18].Weisman CS, Maccannon DS, Henderson JT, Shortridge E, Orso CL. Contraceptive counseling in managed care: preventing unintended pregnancy in adults. Womens Health Issues. 2002;12:79–95. [DOI] [PubMed] [Google Scholar]
- [19].Wekesa E, Askew I, Abuya T. Ambivalence in pregnancy intentions: The effect of quality of care and context among a cohort of women attending family planning clinics in Kenya. PLoS ONE. 2018;13:e0190473. [DOI] [PMC free article] [PubMed] [Google Scholar]