Abstract
Nearly half of Americans are employed by small businesses, and future projections suggest that the number of those employed by small businesses will rise. Despite this, there is relatively little small business intervention research on the integration of health protection and health promotion, known as Total Worker Health® (TWH). We first discuss the importance of studying small businesses in TWH research and practice. Second, we describe an example of a small business TWH intervention, Health Links™ plus TWH owner/senior manager leadership training, that we are evaluating via the Small+Safe+Well (SSWell) study. Key features of the intervention and the SSWell study include attention to multi-level influences on worker health, safety and well-being; organizational change; and dissemination and implementation science strategies via the RE-AIM model. We offer several considerations for future small business TWH research and practice both in terms of the small business context as well as intervention development and evaluation. Our goal is to provide TWH researchers and practitioners with a framework and an example of how to approach small business TWH interventions. Ultimately, through the SSWell study, we aim to provide small businesses with strong evidence to support the use of TWH strategies that are practical, effective and sustainable.
Keywords: Occupational health intervention, Organizational climate, Health promotion, Worker safety, Occupational health and safety, Dissemination and implementation science
INTRODUCTION
Total Worker Health® (TWH) is defined as policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being (NIOSH, 2017b). Because it is relatively new, TWH is still at an early stage of being defined and conceptualized (Hymel et al., 2011; Schill & Chosewood, 2013; Sorensen et al., 2013). Indeed, recent reviews highlight gaps in TWH research. Overall, both Anger et al. (2015) and Feltner et al. (2016) noted a paucity of high quality intervention research and inconsistent acknowledgment and application of theoretical frameworks. Most of the TWH intervention studies identified in their reviews focused on single interventions designed for single, large companies and for a single category of workers. Few examples of small business TWH interventions studies exist (Healthier Workforce Center of the Midwest, 2017; Sorensen et al., 2005; Sorensen et al., 2016). Thus, there is a need to consider how TWH applies and is operationalized in small businesses.
The purpose of this paper is two-fold. First, we discuss the importance of studying small businesses in TWH research and practice. Second, we describe an example of a small business TWH intervention and evaluation strategy, the Small+Safe+Well (SSWell) study. Our goal is to provide a strong conceptual foundation for future research on TWH intervention efficacy, implementation, and maintenance, specific to implementing and measuring TWH in small businesses.
Why Small Business?
Nearly half of Americans are employed by small businesses, and future projections suggest that the number of those employed by small business will rise. In 2014, 57.9 million US workers, representing 48 percent of the workforce, were employed by small businesses, defined by the US Small Business Administration as <500 employees, with the vast majority (89%) of the firms having fewer than 20 employees (United States Census Bureau, 2016). Future estimates indicate that there is a trend for new small businesses to start small and stay small due to the changing nature of work (Choi & Spletzer, 2012). Choi and Spletzer hypothesize that this trend is due to greater emphasis on technology rather than labor modes of production.
Workers in small businesses bear a disproportionate burden of occupational fatalities, illnesses, and injuries. Across all private industries in 2015, the average total recordable injury and illness incidence rate was higher among businesses with 50–249 employees (3.7 per 100 employees) than among businesses with 1000+ employees (3.3 per 100 employees). The rate was even higher for 50–249 employee sized businesses in specific industries, such as manufacturing (4.5 per 100) and nursing and residential care (7.2 per 100) (Bureau of Labor Statistics, 2015). It is likely that these data underestimate the burden of occupational injury and illness among small businesses due to issues such as underreporting and difficulty of maintaining accurate records (Dong et al., 2011).
Additionally, small business workers bear a high burden of chronic health conditions. For example, we studied 260 small businesses in Colorado and found that many small business employees suffer from chronic illness and poor health behaviors. Over one-third exercised less than three times per week, 26% were obese, 22% experienced depression, 20% had chronic fatigue/sleeping problems, 16% were current smokers, 10% had chronic back pain, and 4% had diabetes (Newman et al., 2015). Other small business worksite wellness studies found similar, or worse, health status among small business workers (Merrill, 2013; Sorensen et al., 2005).
Both injury prevention and health promotion present some unique challenges for small businesses (Institute of Medicine, 2014). Small businesses often do not have adequate levels of safety protections in place (Sinclair & Cunningham, 2014). They employ large numbers of temporary, part-time, economically disadvantaged, and precarious workers who may not receive proper safety training and oversight (Cunningham, Sinclair, & Schulte, 2014) – a trend that is increasing in the most recent US economic recovery. Small businesses are also less likely to offer wellness resources and healthcare insurance coverage (Crimmel, 2013; Harris, Hannon, Beresford, Linnan, & McLellan, 2014; McCoy, Stinson, Scott, Tenney, & Newman, 2014). Compounding this problem, small businesses often hire from the demographic of workers who already suffer from health disparities due to race, ethnicity, low health literacy, economic, language, and social and structural barriers to prevention (Harris et al., 2014).
The challenge in understanding the TWH needs and solutions for small business starts with consideration of how business size, as measured by number of employees, may affect a company’s ability to address TWH. While this paper and much of the literature rely on definitions based on company head count, it is important to acknowledge that over-reliance on employee number to define small business may interfere with the ability to understand how to foster meaningful improvements in occupational safety, health and well-being (Cunningham et al., 2014). The current work of the NIOSH Small Business Assistance and Outreach Program (Cunningham et al., 2014; Sinclair, Cunningham, & Schulte, 2013) highlights that while company size and annual revenue are convenient metrics, they set arbitrary cut-offs that may miss the importance of contextual factors that influence the spectrum of TWH. Characteristics that need to be considered may include business structure, age and maturity of the business, management systems, wages, benefit plans, characteristics of the workforce, management and leadership, culture of the organization, access to financial and other resources, support in the business community including intermediary organizations, geographic location, among other factors (Cunningham et al., 2014; Harris et al., 2014). The second challenge in understanding TWH needs of small businesses is to determine whether the needs of small businesses differ from those of large organizations, since there has been relatively more intervention research done in the later (Institute of Medicine, 2014). At present, it is difficult to know whether lessons from TWH research in large businesses are generalizable. For example, smaller businesses may face greater barriers to investing time and money in TWH activities, but they often are better positioned to leverage their core business strategy to integrate TWH.
Evolving Frameworks for TWH in Small Business
Conceptual frameworks proposed by TWH researchers have been designed for and tested mainly in large businesses, not small businesses. A different approach may be needed to consider the contextual factors that may facilitate or hinder effectiveness of TWH strategies among small business. One of the first TWH conceptual models was proposed by Punnett et al. (2013). Their participatory ergonomics approach to TWH addresses the multi-level systems can that support workers in their efforts to protect and promote their health. A key feature of their model is their discussion of how to achieve change through a worker participation process, but their model does not specifically address how the process may work within small businesses. Similarly, in Sorensen et al.’s (2016) model of TWH, organizational characteristics, such as business structure and leadership, are included as upstream factors that directly affect the type of policies, programs, and practices, the conditions of work, and worker proximal outcomes. However, an explanation of how TWH interventions should be designed and delivered based on the needs of small business warrants further development.
Our approach to testing small business interventions draws elements from two theoretical frameworks in the fields of occupational health psychology and organizational change management. We theorize that TWH interventions impact worker health, safety, and well-being through attention to both the multilevel influences of workplace health, safety and the transformational and transactional changes organizations undergo. Like some prior TWH intervention studies, we generally draw upon the socioecological model (Anger et al., 2015). Specifically, from an occupational health psychology perspective, we draw upon Burke and Signal’s (2010) multi-level model of safety. According to Burke and Signal, workplace safety is a social construction that has origins at the regional/national, organization and worker level.
However, unlike other TWH interventions to date, ours also incorporates Burke and Litwin’s model of organizational behavior change (W. Burke & Litwin, 1992). This model adapts transformational and transactional leadership theories to organizational behavior change (Bass, 1990). Transformational change is defined by changes in leadership support, mission and strategy, and a supportive organizational culture. Transactional change, on the other hand, is defined as changes in structures, management practices, and systems that support the day-today management of business activities. Thus, as a generalization, transformational organizational change reflects a change in leadership, and transactional organizational change reflects change in management.
THE SMALL+SAFE+WELL STUDY
In the following section, we offer an example of a small business TWH intervention that we are evaluating via the Small+Safe+Well (SSWell) study. The SSWell study focuses on organizational behavior change among approximately 200 small businesses (<500 employees) in high, medium, and low hazard industries in various regions of Colorado. We aim to determine how a community-based, organizational-level TWH intervention facilitates organizational change through modified TWH practices, safety climate, and health climate. In addition, we will determine whether organizational adoption of TWH policies, programs, and practices at the business level impact individual workers’ safety, health, and well-being.
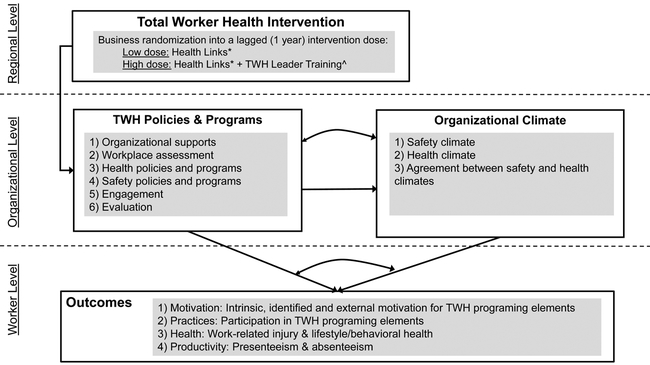
As illustrated in Figure 1, the SSWell study examines several key relationships. The intervention facilitates transactional change of TWH policies and programs through the use of an established intervention, called Health Links™, which provides assessment, advising, certification, and recognition to participating businesses. It also facilitates transformational change through senior-level leadership training. Ultimately, through successful implementation and evaluation of this intervention, we aim to positively influence employee health, safety, and well-being.
Figure 1.
Small+Safe+Well (SSWell) conceptual model
Note. *Transactional change, ^Transformational change
A key element of this model is attention to both safety climate and health climate. Organizational climates for safety and health may be enhanced after businesses participate in the intervention. Organizational climate perceptions stem from shared employee perceptions of their work environment, and observations about what kinds of behaviors get rewarded and supported on the job (Schneider, 1975; Zohar, 2011). When referring to safety and health at work, these shared perceptions can reflect whether or not the organization values and supports practices that protect and enhance employee safety, health and well-being (Zohar, 2011). These climate perceptions represent a check on whether or not business TWH programs are actually being supported on the job.
We would expect to observe a positive impact of our intervention on both climates for safety and health at the organizational level. In other words, the employees of these businesses will perceive that their company supports their safety, health and well-being (Zohar, 2011). The distinction between the two climates is important, because they represent conceptually distinct constructs. A business may have supportive safety policies, but may lack supportive health promoting policies, or vice versa (Zweber, Henning, Magley, & Faghri, 2015). Indeed, Basen- Engquist et al. (1998) found that a health promotion intervention had a positive impact on health climate, but not on safety climate. As a TWH intervention, we aim to impact both safety climate and health climate positively through Health Links and the TWH leadership training. Importantly, our study will enable us to test for convergence of these climates, and test whether companies that display a predominant climate type (safety v. health) enhances -- or in some cases possibly diminishes -- the safety of employees.
The ultimate test of a TWH intervention is its ability to improve individual level outcomes. However, many organizations make decisions that they assume will benefit their employees with little or no evidence to prove that adoption of either safety or “wellness” activities, wellness or safety committees, or corporate policies will have the desired effect. Research on TWH interventions has rarely looked at how organizational changes affect employee level outcomes either positively or negatively (Feltner et al., 2016). When impact assessments have been performed, they have mostly focused on measures of employee health and well-being, not safety (Anger et al., 2015).
At the individual employee level, businesses that enroll in Health Links and that complete the TWH Leadership Training (described below), may adopt TWH programs that are likely to influence several employee safety, health and well-being outcomes. This may be especially true for businesses that experience a positive change in safety and health climates, as it reflects not only businesses that have adopted TWH programs but also businesses that are supporting them in practice (Griffin & Neal, 2000; Neal & Griffin, 2006).
SSWell Study Intervention Components
Health Links™
Health Links was started in 2013 at the Center for Health, Work & Environment in the Colorado School of Public Health (Health Links, 2017). Researchers and faculty developed Health Links to serve as a community-based intervention that seeks to help businesses – especially small and medium sized businesses – create a culture of both safety and health. Health Links does this by helping business incorporate TWH programming into their business practices through assessment, advising, and certification. After engaging with businesses for the past four years, we have observed that Health Links can have a “Trojan horse” effect whereby businesses that start with more emphasis on one TWH element (e.g. “health promotion/wellness”) and subsequently adopt other elements that we introduce at the same time (e.g. safety systems) (Institute of Medicine, 2014). Health Links Certified Healthy Businesses ultimately become advocates for organizational values related to employee safety, health and well-being.
The Health Links Assessment Tool is an online self-assessment survey that benchmarks and measures transactional activities reflecting organizational level health and safety policies and practices. It is based on six benchmarks: 1) organizational supports, 2) workplace assessments, 3) health policies and programs, 4) safety policies and programs, 5) engagement, and 6) evaluation. The assessment is administered to businesses through https://www.healthlinkscertified.org and represents the first step of the Health Links intervention.
This tool was developed by adapting and distilling constructs from TWH Centers of Excellence (McLellan, Moore, Nagler, & Sorensen, 2017b), the CDC Worksite Health ScoreCard (Centers for Disease Control, 2015), and the WHO Healthy Workplace Framework and Model (Burton, 2010). Early focus groups conducted with small business leaders helped us determine that the assessment tool needed to be evidence-based, avoid jargon, be informative, provide specific calls-to-action for participating in the program, and, above all, be brief. This led to a significant process of distilling the questionnaire into 35 questions to capture information in the six benchmarks. The online assessment provides educational tips and FAQs to clarify definitions and language throughout the process. It takes approximately 30–60 minutes to complete and provides an immediate set of scores that are algorithm-based and presented as an easy-to-read report card. It is completed annually at the organizational level and is used to determine Health Links certification level. The validity and reliability of the assessment tool has been demonstrated through formative research, including focus groups, and using a verification checklist at the time of onsite advising that helps assess the accuracy of answers and confirm specific organizational behaviors (Health Links, 2017).
Upon completion of the online assessment, employers are provided with a report card that identifies areas where they are successful and other areas where they can improve, along with evidence-based recommendations on each benchmark. Businesses are then offered up to two in-person advising sessions conducted by a Health Links advisor. Health Links advisors are community members that are trained by the Health Links team to consult with participating businesses to review their Health Links assessment, the report card, and collaborate with the businesses to set tailored goals that result in a Healthy Business Action Plan. Advisors remain available to provide ongoing follow-up to answer questions and support re-assessment every year. To date, Health Links has trained and worked with twelve advisors throughout the state of Colorado who are assigned to conduct business outreach and advising sessions based on geographical regions. Businesses are also connected to local providers of services that can enhance a business’s ability to achieve its defined goals (e.g., ergonomic assessment, safety audit, biometric screening vendors) and to local public health programs for disease management (Health Links, 2017).
The online assessment and advising sessions both evaluate how organizations are implementing and changing TWH activities over time within each of the six benchmarks, and in response to action plan goals. Results of the assessment are automatically used to determine whether a business is recognized in one of four levels of Health Links Certification: Kick-Start, Certified, Certified Partner, or Certified Leader. Participation in Health Links qualifies businesses for both local and statewide recognition, including an annual Governor’s Award for Healthiest Business (Colorado Governor’s Council for Active and Healthy Lifestyles, 2017) as well as opportunities to connect with local business-public health coalitions that have made TWH a regional priority.
TWH leadership training
Leadership is an important component of any TWH intervention, regardless of business size (Sorensen et al., 2013). Thus, as part of this study, we are also offering small business owners/senior managers TWH leadership training, in addition to what they receive as part of Health Links.
One can look to the organization’s espoused TWH values to begin to understand the leader’s overall level of concern for health and safety at work. Small business owners and senior management play major roles in setting these values, and bear the ultimate responsibility for ensuring that business practices align with these values. This includes facilitating management-level TWH leadership. Senior leaders can facilitate transformational change by thinking more broadly about business values, mission, and strategy to achieve a high level of health, safety, and well-being. This intervention presents an important opportunity to evaluate how transformational change around TWH happens when these leaders take action (Avolio & Gardner, 2005; Barling, Loughlin, & Kelloway, 2002; Kouzes & Posner, 2012; Sirota, Mischkind, & Meltzer, 2005; Uhl-Bien, 2006; van Dierendonck, 2011). TWH leaders communicate shared values and the ultimate vision for health, safety, and well-being at work. Leaders engage their workforce in TWH policies and programs and actively participate in them by leading by example. They help promote continual learning and growth by setting expectations and evaluating efforts, and they serve as cheerleaders for their business’s and employees’ efforts to achieve TWH goals. Ultimately, senior TWH-conscious leaders play a pivotal role in influencing the stability, depth, breadth, and integration of TWH into their business, i.e., their TWH culture (Schein, 2010). TWH culture helps guide management and employee decisions about when and how to carry out work while maintaining good health, safety, and well-being.
To be eligible for the TWH leadership training, the individual must be a key decision maker within the company. This includes owners, vice presidents, or other members of the small business’s senior leadership team. Safety managers or human resources managers, who most often are our main contact through Health Links, are not eligible for the training. However, when owners/senior leaders sign up for the training via an online enrollment form, they are permitted to nominate one additional person from their company for the training. This often includes their safety or human resource manager. Thus, a maximum of 2 leaders per company are eligible to take the training.
The TWH leadership training includes in-person and virtual components, and is based on validated leadership theories and best practices (Avolio & Gardner, 2005; Barling et al., 2002; Kouzes & Posner, 2012; Sirota et al., 2005; Uhl-Bien, 2006; van Dierendonck, 2011). Small business owners/senior leaders will spend a total of 10 hours in the TWH leadership training over the course of four months. To facilitate attendance at the in-person training, we are offering small group trainings along the Colorado Front Range as well as in the western, more rural areas of Colorado, at least four times per year. The class size is limited to 15 businesses. The goal of the training is to promote transformational behavioral change around workplace health, safety, and well-being.
Before the in-person training, leaders are asked to spend one hour on their own reflecting on their business’s current TWH strategy as well as their own personal health. Leaders are emailed their Health Links Assessment Report Card and results from an employee health and safety culture survey conducted by our research team. While reviewing these reports, they are asked to reflect on the demands, resources, and supports for TWH at their business. Finally, they are also asked to complete an online TWH leadership self-assessment survey, which includes 27 questions about their TWH leadership practices as well as 12 questions about their personal health and well-being. The TWH leadership practices questions correspond directly to the content discussed in the training. Personal health and well-being questions pertain to behavioral and lifestyle health. Leaders are asked to complete the survey again 3 months after the in-person training and follow-up activities (see below). Pre-in-person training survey results are given to each leader during the training; these results are used to help leaders drive their own behavior change. Post-training survey results are emailed to the leader to review on their own time.
The in-person, six-hour training content focuses on three areas of TWH: the leader, their employees, and their business. Leaders learn about 1) what is meant by TWH and are educated on both the return on investment and value on investment, 2) TWH leadership best practices, 3) their employees’ view of a healthy and safe business, and 4) TWH policy and program management. Throughout the training, leaders reflect on their organizational policies and programs, their own self-reported TWH leadership practices, and their employees’ perceptions of organizational commitment to health and safety (i.e., climate). During the training, leaders develop at least 3 specific goals to help them to transfer what they have learned into their business practice (Johnson, Garrison, Hernez-Broome, Fleenor, & Steed, 2012).
To ensure that goals are achieved, leaders create a profile in an online, social goalsetting platform that they can access by computer or mobile device, and that we maintain. All leaders are trained on how to use the platform and input their goals before the in-person training ends. This platform allows users to create their own login, input specific goals, and set an incentive or disincentive for meeting or not meeting the goal. A key feature of this platform is its social functions. Leaders are matched with a fellow leader and are asked to support each other until the goal period ends. Leaders have the option of supporting other leaders who participated in their training cohort. As supporters, leaders monitor the progress of their peers to hold them accountable. Additionally, the platform allows leaders to engage in discussions with each other and with the research team to discuss progress and questions. We expect leaders to spend a minimum of 1.5 hours using the platform after the in-person training.
In addition to the goal-setting platform, leaders sign up for virtual one-on-one coaching sessions with a member of the research team. The purpose of the sessions is to provide leaders with additional help to discuss progress and strategies to overcome barriers. Each leader is eligible for 3, 30-minute sessions over a period of 3 months after the in-person training. Ultimately, these virtual follow-ups, the goal setting platform, and coaching sessions, provide leaders a chance to be mentored by not only the researchers, but also each other, contributing to creation of an informal social network that could help sustain the impact of participation over time (Balkundi & Kilduff, 2005).
Recruitment
One of the main challenges of conducting small business TWH research is recruitment. Our recruitment strategy focuses on key partnerships. Strategic partners including the Colorado Small Business Administration, the Colorado Small Business Development Centers Network, local chambers of commerce, economic development centers, workforce centers and the Colorado Society for Human Resource Managers are helping recruit participant companies through member communications, networking events and direct outreach. We leverage existing collaborations with local public health agencies, safety organizations, trade associations, and Pinnacol Assurance, the state-based workers’ compensation insurer, to recruit policyholders. We have established direct referral pathways with Pinnacol to encourage policyholders to apply for Health Links. Health Links is also included as a partner resource program in the risk and recommendation reports that high-risk clients receive from Pinnacol Assurance’s safety consultants after a safety audit.
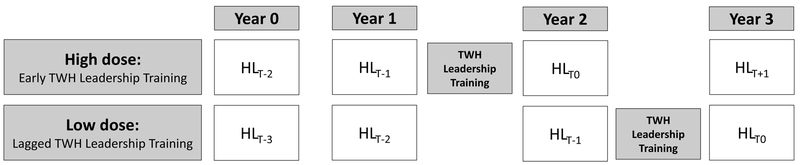
Upon enrollment, businesses are randomly assigned to one of two groups, either an early or a lagged intervention group. Businesses in the early condition receive the high dose of the intervention (Health Links + TWH leadership training) after their 2nd baseline, and businesses in the lagged condition receive the high dose after their 3rd baseline (see Figure 2).
Figure 2.
Small+Safe+Well lagged intervention design
Evaluation
TWH research and interventions are rarely translated into small business applications (Dugan & Punnett, 2017). While certain programs and practices may work well in isolated and very controlled settings, it is important to understand more broadly how research is disseminated and implemented to small businesses in the field (Schulte et al., 2017). Thus, we believe it is important to determine how well the intervention performs in practice, akin to what other investigators have done to evaluate a participatory ergonomics tool kit (Nobrega et al., 2017).
One evaluation method frequently utilized to assess public health interventions is the RE-AIM framework, originally proposed by Glasgow and colleagues (2007; 1999). This framework addresses five areas of public health impact: Reach – participation and representativeness of individuals, Efficacy – impact of specific outcome criteria, Adoption – participation and representativeness of organizations, Implementation – consistency and quality of program execution, and Maintenance – the sustainability of the change.
We are applying this framework by collecting efficacy and maintenance measures at multiple organizational levels. Using the Health Links Assessment, we are collecting data on business practices. Using an employee health and safety culture survey, we are collecting employee health and safety climate perceptions as well as self-report information on health, safety, well-being, absenteeism, and presenteeism. Using the surveys briefly described in the TWH leadership training section above, we are collecting information on small business owner/senior manager TWH leadership practices and health. Finally, we are linking these data at the organizational level to workers’ compensation claims. All other program evaluation data is being collected to ensure that we can understand program reach, adoption and implementation. By evaluating the intervention using the RE-AIM framework, we hope to demonstrate that this TWH intervention is effective, scalable, and sustainable in a wide range of business settings. Details regarding the specific measures and analytical strategies used in evaluation are beyond the scope of this paper, although the authors would be happy to provide any pertinent information to interested readers.
DISCUSSION
There is a clear need for TWH researchers and practitioners to consider strategies to facilitate health, safety and well-being among small businesses. Small business workers are at risk for significant occupational injuries, illnesses and fatalities as well as poor health. While small businesses may face significant challenges in implementing TWH initiatives, there are many opportunities to advance small business TWH policies and programs that ultimately improve employee health, safety and well-being. When given external help from the community, small businesses may be able to undergo organizational changes at both leadership and management levels that ultimately contribute to improved safety and health of workers.
The SSWell study represents our approach to test this hypothesis. First, we have developed and are testing how theoretical constructs apply to small businesses. Second, we are employing traditional research methods based on randomized controlled trial intervention design to rigorously assess the evidence of effectiveness. Finally, we are simultaneously evaluating the intervention through the lens of dissemination and implementation science (Dugan & Punnett, 2017). Ultimately, our goal is to provide small businesses with strong evidence to support the use of TWH interventions that are practical, effective and sustainable.
Further understanding context for small business TWH
Understanding the contextual factors associated with how TWH is implemented in small businesses is important. The communities in which work happens, the business that people work for, and peoples’ engagement all influence health, safety and well-being. When all levels are aligned, we would expect to observe positive outcomes.
There are many business characteristics that can influence organizational level adoption and implementation of TWH policies and programs, a number of which are described by Schill and colleagues (2013). Type of industry may influence the types of TWH policies and programs offered. For example, highly hazardous industries that are resource-poor may have more robust safety programs than low hazard industries by necessity. This may be especially apparent among small businesses (SmartMarket Report, 2017). Another example is the shift towards temporary, vulnerable work arrangements. For example, the “gig” workforce is largely classified as independent contract workers, and as such, are small businesses (Tran & Sokas, 2017). In this type of work environment, standard labor laws do not apply, such as health and safety regulations and workers’ compensation, and contract workers bear the primary responsibility for health and safety. Research demonstrates that these workers often lack knowledge and resources to protect their health (Howard, 2017). Community supports for health, safety and well-being may be important for this type of work environment. This may include education, assistance with organizing, and portable benefits (Bonney et al., 2017; Forst et al., 2013; Tran & Sokas, 2017).
Compared to large businesses, small businesses may be better equipped to undertake organizational change. In our systematic review of literature on small business worksite wellness programs, we found that they often have an easier time implementing initiatives, incorporating employee suggestions, holding people accountable, generating teamwork, and achieving high participation rates (McCoy et al., 2014). Indeed, in our past research with 314 businesses enrolled in a externally supported, health promotion program, we observed higher employee participation rates amongst small business employees than large business employees (Schwatka et al., in press). Small business founders and early leaders can be a major source of guidance for how the business should operate (Schein, 2010). Even at early stages of business development, small businesses may choose to offer TWH-like programs to attract and retain workers. Family-owned small businesses may also be especially poised to take action as they are characterized by quality relationships, trust, senior leadership commitment, and pride (Eddleston & Morgan, 2014). Similarly, even among non-family owned small businesses it is common for the organization’s culture to be focused on employee relationships (Cunningham et al., 2014). Thus, if small businesses choose to change and are provided with the resources to implement TWH programs through community supports, they may be better positioned to undertake organizational change compared to larger businesses.
At the regional level, community resources can be valuable for small business. Indeed, Sinclair et al. (2013) specifically highlight the importance of intermediary organizations in facilitating intervention diffusion to small businesses. They note that these organizations have strengths such as their knowledge of the small business context, experience selecting services that are relevant to small business, and the ability to help with intervention implementation. These organizations can help small businesses create policies and programs, improve management practices around health and safety, and make changes to the work environment that support health and safety (Newman et al., 2015).
Community resources exist to help small businesses implement elements of TWH and assist workers who want to improve their health and well-being, although in a siloed way. Chambers of commerce, regional business coalitions, industry, trade, and labor organizations provide assistance, education, and networking opportunities for businesses and worker organizations. Safety consultation services from the Occupational Safety and Health Administration (OSHA) or workers’ compensation carriers (Schofield, Alexander, Gerberich, & MacLehose, 2017) can help small businesses develop their safety programs, admittedly with a primary focus on safety as they rarely integrate health promotion programs. Local safety organizations can also provide access to knowledge, safety vendors, and peer mentoring. Small businesses can utilize community services to enhance their health promotion programs, such as employee assistance program vendors, community health fairs, state and local public health agencies, and other health services providers, although, these resources generally focus on wellness and rarely integrate health protection.
While we traditionally think of the integrative aspects of TWH happening at the organizational and individual levels, there is a potential for integration to occur at the regional level as well. Recently, NIOSH, the TWH Centers of Excellence, and the TWH Affiliates have been offering practical solutions for addressing TWH integrative strategies (McLellan, Moore, Nagler, & Sorensen, 2017a; NIOSH, 2016, 2017a). Additionally, at least three of the state-based workers’ compensation insurers (Colorado, Oregon, Ohio) have taken steps to integrate their safety and health promotion services (Newman et al., 2015; Ohio Bureau of Workers’ Compensation, 2017; SAIF Corporation, 2017). Some labor unions also offer health protection as well as health promotion services to their members (Laborers Health and Safety Fund of North America, 2017).
The external environment in which organizations and their workers operate also play an important role in the quality of TWH efforts and employee health and safety. Burke and Signal (2010) offer a detailed description of how cultural values and the political economy impact safety at work. The economic, business, and regulatory climate likely plays a role in influencing whether businesses adopt and implement TWH initiatives. For example, health promotion practices are influenced by regulations pertaining to the Affordable Care Act, paid parental leave, and wages. Likewise, health protection practices are influenced by the Occupational Safety and Health Act, workers’ compensation laws, and other federal, state and local regulations. These regulations may not apply to all businesses, as the smallest businesses are exempt from some of these laws depending on jurisdiction and business sector. Other regulations pertain when the model is applied in other countries. Compared to the US, other countries that have more or less robust social safety nets and unemployment policies that may influence how businesses engage in TWH strategies.
Further understanding intervention design for small business TWH
An implication of the literature and our research is that TWH interventions may need to be multidimensional. Most previous TWH interventions have been designed to be highly specific and target particular groups of workers and industries, which may limit generalizability (Anger et al., 2015). For example, there are few examples of TWH interventions that intentionally target not only transactional but also transformational contributions to organizational change (Anger et al., 2015; Bradley, Grossman, Hubbard, Ortega, & Curry, 2016). None have focused on developing the TWH leadership skills of business owners/senior managers, as proposed in our intervention, while concomitantly assessing adoption of TWH practices, policies and programs.
Our evaluation approach suggests that outcomes should be assessed at multiple levels, and that researchers should measure potential confounders and mediators, where possible. Feltner et al. (2016) notes some promising evidence that TWH interventions impact smoking cessation, fruit and vegetable consumption and less sedentary work. However, there is relatively little evidence that TWH interventions impact intermediary outcomes, such as safety compliance, or health outcomes, such as stress and injury rates. Thus, there remains a lack of information on how TWH programs influence attitudes, motivation, knowledge, behavior, and work-related and non-work-related health outcomes. The approach we are using in the SSWell study will allow us to test how various combinations of TWH policies and programs impact several important employee health, safety, and well-being outcomes. Importantly, we will also be able to measure factors such as productivity and engagement, which are probably key metrics to share with small business owners to help promote the sustainability of interventions.
While the SSWell study seeks to understand whether the success of TWH small business interventions hinges on their ability to impact climate perceptions, we urge other TWH researchers to examine the influence of climate as well as other mechanisms that might account for TWH program success. This is especially important in the small business context as researchers have noted a relative lack of small business organizational climate research (Cunningham et al., 2014). Climate researchers note that employees’ perceptions of their work environments serve as cues for how to speak and act at work (Denison, 1996). In the context of safety and health, employees can discern the relative importance of safety and health as compared to other competing organizational goals such as productivity. They can also perceive how many of the policies and programs are used in practice, how consistently they are used, and how committed management are to them (Zohar, 2010, 2011). Thus, we believe that TWH interventions for small businesses must ensure effective policy and program implementation such that their use is perceived by employees to be supported in practice. Employees may be more willing to reciprocate their businesses’ genuine concern for them and treatment of them by being motivated and engaged in TWH programming (Hofmann & Morgeson, 1999). Anecdotally, such employees often become TWH champions within their organizations, creating a path for improving the diversity of workers participating through peer-to-peer engagement (Sorensen et al., 2005). Furthermore, employees will be motivated to participate in TWH programming, if they believe that it will be rewarded and supported (Neal & Griffin, 2006).
CONCLUSIONS
In this paper, we outline the gaps in and the need for small business TWH intervention research. While small businesses may face barriers to implementing TWH strategies, we believe that with community support they can overcome these barriers. Our community-based, organizational-level study aims to test the impact of a TWH intervention that assists small businesses in their efforts to undergo both transactional and transformational organizational change. By applying the RE-AIM program evaluation framework, we hope to highlight the importance of applying best-practices in dissemination and implementation science to TWH interventions. Finally, we have emphasized the importance of recognizing both contextual and intervention design factors to consider when researchers design and evaluate small business TWH interventions. Through the SSWell study, we offer an example of how to test both a theoretical framework and practical solution, in order to provide small businesses with strong evidence to support the use of TWH strategies that are practical, effective and sustainable.
Acknowledgements:
This publication was supported by the Cooperative Agreement number, 1 U19 OH 011227, funded by the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Footnotes
Conflict of Interest Statement: On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- Anger WK, Elliot DL, Bodner T, Olson R, Rholman DS, Truxillo DM, … Montgomery D (2015). Effectiveness of Total Worker Health Interventions Journal of Occupational Health Psychology, 20(2), 226–247. doi: 10.1037/a0038340.supp [DOI] [PubMed] [Google Scholar]
- Avolio BJ, & Gardner WL (2005). Authentic leadership development: Getting to the root of positive forms of leadership. The Leadership Quarterly, 16(3), 315–338. doi: 10.1016/j.leaqua.2005.03.001 [DOI] [Google Scholar]
- Balkundi P, & Kilduff M (2005). The ties that lead: A social network approach to leadership. The Leadership Quarterly, 16(6), 941–961. doi: 10.1016/j.leaqua.2005.09.004 [DOI] [Google Scholar]
- Barling J, Loughlin C, & Kelloway EK (2002). Development and test of a model linking safety-specific transformational leadership and occupational safety. Journal of Applied Psychology, 87, 488–496. [DOI] [PubMed] [Google Scholar]
- Basen-Engquist K.e. a. (1998). Worksite Health and Safety Climate: Scale Development and Effects of a Health Promotion Intervention. Preventative Medicine, 27, 111–119. doi: 10.1006/pmed.1997.0253 [DOI] [PubMed] [Google Scholar]
- Bass B (1990). From transactional to transformational leadership: Learning to share the vision. Organizational Dynamics, 18(3), 19–31. [Google Scholar]
- Bonney T, Forst L, Rivers S, Love M, Pratap P, Bell T, & Fulkerson S (2017). Occupational Safety and Health in the Temporary Services Industry: A Model for a Community-University Partnership. NEW SOLUTIONS:A Journal of Environmental and Occupational Health Policy, 27(2), 246–259. doi: 10.1177/1048291117712545 [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Grossman DC, Hubbard RA, Ortega AN, & Curry SJ (2016). Integrated interventions for improving Total Worker Health: A panel report from the National Institutes of Health Pathways to Prevention Workshop: Total Worker Health—What’s work got to do with it? Annals of Internal Medicine, 1–7. doi: 10.7326/M16-0740 [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. (2015). TABLE Q1. Incidence rates of total recordable cases of nonfatal occupational injuries and illnesses by quartile distribution and employment size, 2015. Retrieved from https://www.bls.gov/iif/oshwc/osh/os/ostb4748.pdf
- Burke MJ, & Signal SM (2010). Workplace safety: A multilevel, interdisciplinary perspective In Liao H, Martocchio J, & Joshi A (Eds.), Research in Personnel and Human Resources Management (Vol. 29, pp. 1–47): Emerald Group Publishing Limited. [Google Scholar]
- Burke W, & Litwin G (1992). A causal model of organizational performance. Journal of Management, 18(3), 532–545. [Google Scholar]
- Burton J (2010). WHO healthy workplace framework and model: Background and supporting literature and practices. Retrieved from http://www.who.int/occupational_health/healthy_workplaces/en/
- Centers for Disease Control. (2015). Worksite health scorecard. Retrieved from http://www.cdc.gov/dhdsp/pubs/worksite_scorecard.htm
- Choi EJ, & Spletzer JR (2012). The declining average size of establishments: Evidence and explinations. Monthly Labor Review, 50–65. [Google Scholar]
- Colorado Governor’s Council for Active and Healthy Lifestyles. (2017). Colorado Governor’s Council Awards. Retrieved from http://www.coloradofitness.org/awards
- Crimmel BL (2013). Changes in self-insured coverage for employer-sponsored health insurance: Private sector, by firm size, 2001–2011. Retrieved from https://meps.ahrq.gov/data_files/publications/st412/stat412.pdf [PubMed]
- Cunningham TR, Sinclair R, & Schulte P (2014). Better understanding the small business construct to advance research on delivering workplace health and safety. Small Enterprise Research, 21(2), 148–160. doi: 10.1080/13215906.2014.11082084 [DOI] [Google Scholar]
- Denison DR (1996). What is the difference between organizational culture and organizational climate? A native’s point of view on a decade of paradigm wars. The Academy of Management Review, 21(3), 619–654. doi: 10.2307/258997 [DOI] [Google Scholar]
- Dong XS, Fujimoto A, Ringen K, Stafford E, Platner JW, Gittleman JL, & Wang X (2011). Injury underreporting among small establishments in the construction industry. American Journal of Industrial Medicine, 54(5), 339–349. doi: 10.1002/ajim.20928 [DOI] [PubMed] [Google Scholar]
- Dugan A, & Punnett L (2017). Dissemination and implementation research for occupational safety and health. Occupational Health Science, 1(1–2), 29–45. doi: 10.1007/s41542-017-0006-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddleston KA, & Morgan RM (2014). Trust, commitment and relationships in family business: Challenging conventional wisdom. Journal of Family Business Strategy, 5(3), 213–216. doi: 10.1016/j.jfbs.2014.08.003 [DOI] [Google Scholar]
- Feltner C, Peterson K, Weber RP, Cluff L, Coker-Schwimmer E, Viswanathan M, & Lohr KN (2016). The effectiveness of Total Worker Health interventions: A systematic review for a National Institutes of Health Pathways to Prevention Workshop. Annals of Internal Medicine, 165(4), 262–269. doi: 10.7326/M16-0626 [DOI] [PubMed] [Google Scholar]
- Forst L, Ahonen E, Zanoni J, Holloway-Beth A, Oschner M, Kimmel L, … Sokas RK, (2013). More than training: Community-based participatory research to reduce injuries among Hispanic construction workers. American Journal of Industrial Medicine, 56(8), 827–837. doi: 10.1002/ajim.22187 [DOI] [PubMed] [Google Scholar]
- Glasgow R, & Emmons K (2007). How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health, 28(1), 413–433. doi: 10.1146/annurev.publhealth.28.021406.144145 [DOI] [PubMed] [Google Scholar]
- Glasgow R, Vogt T, & Boles S (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89(9), 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin M, & Neal A (2000). Perceptions of safety at work: a framework for linking safety climate to safety performance, knowledge, and motivation. Journal of Occupational Health Psychology, 1, 347–358. [DOI] [PubMed] [Google Scholar]
- Harris JR, Hannon PA, Beresford SAA, Linnan LA, & McLellan DL (2014). Health promotion in smaller workplaces in the United States. Annual Review Public Health, 35(1), 327–342. doi: 10.1146/annurev-publhealth-032013-182416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Links Health. (2017). Health Links. Retrieved from https://www.healthlinkscertified.org/
- Healthier Workforce Center of the Midwest. (2017). Small business outreach project. Retrieved from https://www.public-health.uiowa.edu/hwcmw/outreach/small-business-outreach/
- Hofmann DA, & Morgeson FP (1999). Safety-related behavior as a social exchange: The role of perceived organizational support and leader–member exchange. Journal of Applied Psychology, 84(2), 286–296. doi: 10.1037/00219010.84.2.286 [DOI] [Google Scholar]
- Howard J (2017). NIOSH Science Blog: Nonstandard work arrangements. Retrieved from https://blogs.cdc.gov/niosh-science-blog/2017/01/03/nonstandard-work-arrangements/
- Hymel PA, Loeppke RR, Baase CM, Burton WN, Hartenbaum NP, Hudson TW,… Larson PW (2011). Workplace health protection and promotion. Journal of Occupational and Environmental Medicine, 53(6), 695–702. doi: 10.1097/JOM.0b013e31822005d0 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2014). Promising and Best Practices in Total Worker Health: Workshop Summary. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Johnson SK, Garrison LL, Hernez-Broome G, Fleenor JW, & Steed JL (2012). Go for the goal(s): Relationship between goal setting and transfer of training following leadership development. Academy of management learning and education, 11(4), 555–569. doi: 10.5465/amls.2010.0149 [DOI] [Google Scholar]
- Kouzes JM, & Posner BZ (2012). The leadership challenge: How to make extraordinary things happen in organizations (5th ed.). San Francisco: Wiley. [Google Scholar]
- Laborers Health and Safety Fund of North America. (2017). Laborders Health and Safety Fund of North America. Retrieved from https://www.lhsfna.org/
- McCoy K, Stinson K, Scott K, Tenney L, & Newman LS (2014). Health promotion in small business: A systematic review of factors influencing adoption and effectiveness of worksite wellness programs. Journal of Occupational and Environmental Medicine, 56(6), 579–587. doi: 10.1097/JOM.0000000000000171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan D, Moore W, Nagler E, & Sorensen G (2017a). Implementing an integrated approach: Weaving employee health, safety, and well-being into the fabric of your organization. Retrieved from http://centerforworkhealth.sph.harvard.edu
- McLellan D, Moore W, Nagler E, & Sorensen G (2017b). Implementing an integrated approach: Weaving employee health, safety, and well-being into the fabric of your organization. Retrieved from http://centerforworkhealth.sph.harvard.edu/guidelines
- Merrill RM (2013). A small business worksite wellness model for improving health behaviors. Journal of Occupational and Environmental Medicine, 55(8), 895–900. doi: 10.1097/JOM.0b013e31826eef83 [DOI] [PubMed] [Google Scholar]
- Neal A, & Griffin MA (2006). A study of the lagged relationships among safety climate, safety motivation, safety behavior, and accidents at the individual and group levels. Journal of Applied Psychology, 91, 946–953. doi: 10.1037/00219010.91.4.946 [DOI] [PubMed] [Google Scholar]
- Newman LS, Stinson KE, Metcalf D, Fang H, Brockbank CV, Jinnett K,… Goetzel RG (2015). Implementation of a worksite wellness program targeting small businesses: The Pinnacol Assurance Health Risk Management Study. Journal of Occupational and Environmental Medicine, 57(1), 14–21. doi: 10.1097/JOM.0000000000000279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIOSH. (2016). Fundamentals of total worker health approaches: Essential elements for advancing worker safety, health, and well-being. By Lee MP, Hudson H, Richards R, Chang CC, Chosewood LC, Schill AL, on behalf of the NIOSH Office for Total Worker Health. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; DHHS (NIOSH) Publication No.2017-112. [Google Scholar]
- NIOSH. (2017a). NIOSH Total Worker Health Affiliate Program. Retrieved from https://www.cdc.gov/niosh/twh/affiliate.html
- NIOSH. (2017b). What is Total Worker Health? Retrieved from https://www.cdc.gov/niosh/twh/default.html
- Nobrega S, Kernan L, Plaku-Alakbarova B, Robertson M, Warren N, Henning R, & Team C-NR (2017). Field tests of a participatory ergonomics toolkit for Total Worker Health. Appl Ergon, 60, 366–379. doi: 10.1016/j.apergo.2016.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohio Bureau of Workers’ Compensation. (2017). Safety grants. Retrieved from https://www.bwc.ohio.gov/employer/services/SandH/SafetyGrants.asp
- Punnett L, Warren N, Henning R, Nobrega S, Cherniack M, & CPH-NEW Research Team. (2013). Participatory ergonomics as a model for integrated programs to prevent chronic disease. Journal of Occupational and Environmental Medicine, 55(12 Suppl), S19–24. doi: 10.1097/JOM.0000000000000040 [DOI] [PubMed] [Google Scholar]
- Corporation SAIF. (2017). Total Worker Health. Retrieved fromhttps://www.saif.com/safety-and-health/topics/promote-health.html
- Schein EH (2010). Organizational culture and leadership. San Francisco: JosseyBass. [Google Scholar]
- Schill AL, & Chosewood LC (2013). The NIOSH Total Worker Health™Program. Journal of Occupational and Environmental Medicine, 55, S8–S11. doi: 10.1097/JOM.0000000000000037 [DOI] [PubMed] [Google Scholar]
- Schneider B (1975). Organizational climates: An essay. Personnel Psychology, 28(4), 447–479. doi: 10.1111/j.1744-6570.1975.tb01386.x [DOI] [Google Scholar]
- Schofield KE, Alexander BH, Gerberich SG, & MacLehose RF (2017). Workers’ compensation loss prevention representative contact and risk of losttime injury in construction policyholders. Journal of Safety Research, 62(Supplement C), 101–105. doi: 10.1016/j.jsr.2017.06.012 [DOI] [PubMed] [Google Scholar]
- Schulte P, Cunningham T, Nickels L, Felknor S, Guerin R, Blosser F, … Menger-Ogle L (2017). Translation research in occupational safety and health: A proposed framework. American Journal of Industrial Medicine, 60(12), 10111022. doi: 10.1002/ajim.22780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwatka N, Smith D, Weitzenkamp D, Atherly A, Dally M, v.S. Brockbank C,… Newman L (in press). The impact of worksite wellness programs by size of business: A three-year longitudinal study of participation, health benefits, absenteeism, and presenteeism. Annals of Work Exposures and Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair R, & Cunningham T (2014). Safety activities in small businesses. Safety Science, 64, 32–38. doi: 10.1016/j.ssci.2013.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair R, Cunningham T, & Schulte P (2013). A model for occupational safety and health intervention diffusion to small businesses. American Journal of Industrial Medicine, 56(12), 1442–1451. doi: 10.1002/ajim.22263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirota D, Mischkind L, & Meltzer M (2005). The enthusiastic employee: How companies profit by giving workers what they want. Upper Saddle River, NJ: Wharton School Publishing. [Google Scholar]
- SmartMarket Report. (2017). Safety management in the construciton industry 2017. Retrieved from Dodge Data & Analytics: https://www.cpwr.com/sites/default/files/publications/Dodge_Safety_Report_2017.pdf
- Sorensen G, Barbeau E, Stoddard A, Hunt M, Kaphingst K, & Wallace L (2005). Promoting behavior change among working-class, multiethnic workers: Results of the Healthy Directions—Small Business Study. American Journal of Public Health, 95(8), 1389–1395. doi: 10.2105/AJPH.2004.038745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, McLellan D, Dennerlein J, Pronk N, Allen J, Boden L, … Wagner G (2013). Integration of health protection and health promotion: Rationale, Indicators, and Metrics. Journal of Occupational and Environmental Medicine, 55(12 Suppl), S12–S18. doi: 10.1097/JOM.0000000000000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, McLellan D, Sabbath E, Dennerlein J, Nagler E, Hurtado D, … Wagner G (2016). Integrating worksite health protection and health promotion: A conceptual model for intervention and research. Preventative Medicine, 91, 188–196. doi: 10.1016/j.ypmed.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran M, & Sokas RK (2017). The gig economy and contingent work: An occupational health assessment. Journal of Occupational and Environmental Medicine, 59(4), e63–e66. doi: 10.1097/JOM.0000000000000977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhl-Bien M (2006). Relational Leadership Theory: Exploring the social processes of leadership and organizing. The Leadership Quarterly, 17(6), 654–676. doi: 10.1016/j.leaqua.2006.10.007 [DOI] [Google Scholar]
- United States Census Bureau. (2016). Statistics of U.S. Businesses Main. Retrieved from http://www.census.gov/data/tables/2014/econ/susb/2014-susb-annual.html
- van Dierendonck D (2011). Servant leadership: A review and synthesis. Journal of Management, 37(4), 1228–1261. doi: 10.1177/0149206310380462 [DOI] [Google Scholar]
- Zohar D (2010). Thirty years of safety climate research: Reflections and future directions. Accident Analysis and Prevention, 42(5), 1517–1522. doi: 10.1016/j.aap.2009.12.019 [DOI] [PubMed] [Google Scholar]
- Zohar D (2011). Safety climate: Conceptual and measurement issues. In Quick JC & Tetrick LE (Eds.), (2nd ed.). Washington DC: APA. [Google Scholar]
- Zweber ZM, Henning RA, Magley VJ, & Faghri P (2015). Considering the differential impact of three facets of organizational health climate on employees’ well-being. The Scientific World Journal, 2015, 1–10. doi: 10.1155/2015/407232 [DOI] [PMC free article] [PubMed] [Google Scholar]