1. Background
Child undernutrition is one of the global public health concerns, as it results in irreversible damage to the physical and mental health of children. Undernutrition further impacts adult health and human capital. It accounts for morbidity and premature mortality in developing countries [1]. Undernutrition is known to severely impact children in the first two years of life marked as the critical period [2]. Globally, over a hundred million children are undernourished [3]. India is home to highest proportion of undernourished children in the world [4]. One third of children under the age of five years in the country are stunted, another one third are underweight and about 21% are wasted. A major concern in child undernutrition in the Indian subcontinent is that despite a considerable decline in the prevalence of stunting, the magnitude of wasting has significantly increased across the states [5]. In particular, data on prevalence of undernutrition are scarce among children under two years of age. According to National Family Health Survey 3, the prevalence of stunting was 45% and wasting 23% among children under three years of age [6]. The prevalence of stunting and underweight rapidly increases between 20 and 23 months peaking at 20 months indicating poor infant and young child feeding practices [7]. National Nutrition Monitoring Bureau (NNMB) 2006 identifies undernutrition between 0 and 6 months as 26% that increased to 39% in 12–23 months [8]. It is therefore evident that children in this critical age group manifest growth faltering. Undernutrition if uncorrected during these years may have lasting impact on the development of children.
Conventional indicators used for assessment of undernutrition are stunting, wasting and underweight. These indices reflect distinct metabolic changes and are used in determining appropriate nutritional interventions [9]. Developmental economist Peter Svedberg indicated that the conventional indices used for measuring undernutrition overlap and are insufficient for measuring the overall prevalence of undernutrition among children. He suggested that if children with stunting, wasting and underweight are all considered being in a state of anthropometric failure, an aggregate indicator is needed that incorporates all categories of undernourished children. This aggregate indicator, known as the Composite Index of Anthropometric Failure (CIAF) comprises of six categories under which children experiencing one or more forms of anthropometric failure are grouped [10]. This assessment method has been used by several workers to study undernutrition [[9], [10], [11], [12], [13]], and concluded that CIAF identifies a greater percentage as undernourished compared to traditional indices. However, this method too does not address wasting masked by edema or fat [14].
To further assess the type of undernutrition that is widespread and its severity, Mandal and Bose [15] proposed three other indices viz, Stunting Index (SI), Wasting Index (WI) and Underweight Index (UI), to emphasize the significance of each manifest relative to CIAF. These indices are calculated using the conventional measures of stunting, wasting and underweight along with CIAF.
Most prevalence studies assessing undernutrition in India have used Z scores to classify the various forms and severity. Limited studies have used CIAF that assess both the magnitude and severity identifying a combination of two or three manifests coexisting in children. In a developing country setting where the prevalence of undernutrition is high, there is a need to determine the true burden and severity of undernutrition using composite index.
This work aimed to assess the prevalence and severity of undernutrition using CIAF and conventional anthropometric indices among children 12–23 months of age. It also evaluated SI, WI and UI to recognize the significance of each manifest of undernutrition relative to CIAF.
2. Methodology
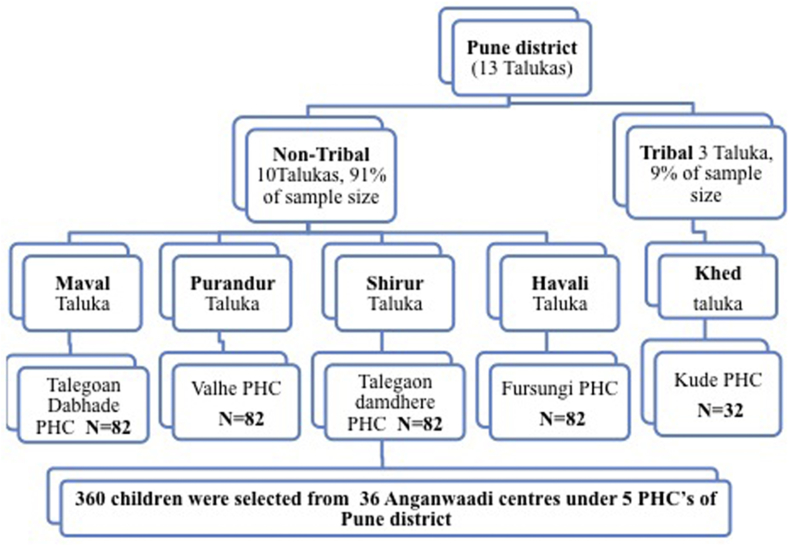
A cross-sectional study was conducted in government pre-school centers among children aged 12–23 months in Pune district, Maharashtra, India. Considering 36% prevalence of underweight children in Maharashtra, (NFHS-4, 2016) [13] with 5% precision and 95% confidence interval, the sample size estimated was 360 children. Ethics clearance was obtained from Savitribai Phule Pune University's institutional ethics committee. Permission from the authorities was taken to work in various anganwadis under Public Health Centres (PHC). Informed consent from parents was obtained before the commencement of the study. Fig. 1 explains the multistage random sampling technique. Participants both boys and girls were recruited using multistage random sampling technique. Pune district comprises of 13 talukas of which 10 correspond to non-tribal areas. A sample of 328 children representing 10 talukas and 30 anganwadis (government run preschool centers) were recruited. From the remaining three tribal talukas, 32 children representing five anganwadi centers were recruited to achieve the estimated sample size. In all, the study covered seven villages in Pune district. Kuppuswamy scale was used to categorize the socioeconomic status [16]. Infantometer was used to measure length and digital weighing scalewas used to record weight. Z scores for Weight for height (WHZ) height for age (HAZ) and weight for age (WAZ) were calculated as per WHO international growth standards using Anthro Software [17]. The anthropometric measures were further categorized as per CIAF [10,11] provided in Table 1. According to this classification children who have normal HAZ,WAZ, WHZ scores were included under category A. Secondly, children with any one manifest of undernutrition i.e., either stunting or wasting or underweight were categorized under B,C and D respectively. Further, children with any two manifests combined such as wasting and underweight; or stunting and wasting were categorized in divisions E and F respectively. All three manifestations of undernutrition i.e., stunting, wasting and underweight are indicated as G. Further, to identify the rates of prevalence of stunting, underweight and wasting relative to the overall prevalence, three more indicators Stunting Index (SI), Wasting Index (WI) and Underweight Index (UI) were calculated using the formulas: Wasting Index = Wasting/CIAF; Stunting Index = Stunting/CIAF; and Underweight Index = Underweight/CIAF.
Fig. 1.
Multistage random sampling of children from Pune district, Maharashtra including tribal and non tribal talukas.
Table 1.
Classification of anthropometric failure as per CIAF and distribution of participants as per CIAF categories.
| Categories of undernutrition [8] | Wasting | Stunting | Underweight | N = 360 |
||
|---|---|---|---|---|---|---|
| N | % | |||||
| A | No failure | No | No | No | 89 | 24.7 |
| B | Underweight | No | No | Yes | 0 | 0 |
| C | Wasting | Yes | No | No | 39 | 10.8 |
| D | Stunting | No | Yes | No | 111 | 30.8 |
| E | Stunting and underweight |
No | Yes | Yes | 57 | 15.8 |
| F | Wasting and underweight |
Yes | No | Yes | 26 | 7.2 |
| G | Wasting, stunting and underweight |
Yes | Yes | Yes | 38 | 10.6 |
3. Results
The sample consisted of 55% (n = 200) boys and 44% (n = 160) girls. Majority of the children belonged to the lower socio economic status as per Kuppuswamy scale. Distribution of participants as per the categories of undernutrition in CIAF is provided in Table 1. Nearly one fourth (25%) of the children studied were free from any form of undernutrition. Underweight as a single manifest was not observed among any of the children. Wasting was observed among 11%, while stunting was observed among 31% of the children. Combinations of two manifests of undernutrition i. e, stunting and underweight, as well as wasting and underweight were observed among 16% and 7% respectively. A combination of three manifests of undernutrition was observed among 11% of the children.
Table 2 presents the sexwise distribution of rates of wasting, stunting and underweight and their respective indices among the children. It also provides the sexwise prevalence of anthropmetric failure using CIAF. According to the WHO Z score classification total prevalence of wasting was 29%. Of this nearly 58% boys were wasted, compared to 42% girls. Total prevalence of stunting was 58% of whom 59% boys and 41% girls were stunted. Similar observation of high prevalence of underweight was observed among boys (63%) as compared to girls (37%). As per CIAF too, greater percent boys suffered anthropometric failure (57%) as compared to girls (43%). According to CIAF, 75% children suffered from anthropometric failure. Undernutrition relative to CIAF revealed higher stunting index (76) followed by underweight index (47) and wasting index (38).
Table 2.
Sexwise distribution of rates of stunting, wasting, underweight, and CIAF among children 12–23 months.
| Categories of malnutrition | Boys N = 200 |
Girls N = 160 |
Total N = 360 |
|---|---|---|---|
| Wasting | 60 (58%) | 43(42%) | 103 (29%) |
| Stunting | 123 (59%) | 84(41%) | 207 (58%) |
| Underweight | 76 (63%) | 45(37%) | 121 (34%) |
| CIAF | 154 (57%) | 117(43%) | 271 (75%) |
| Wasting index (WI) | 60/154 = 0.389 | 43.5/117 = 0.371 | 103/271 = 38 |
| Stunting Index (SI) | 123/154 = 0.798 | 84/117 = 0.717 | 207/271 = 76.38 |
| Underweight index (UI) | 76/154 = 0. 0.493 | 45/117 = 0.384 | 121/271 = 46.64 |
WI= Wasting/CIAF; SI= Stunting/CIAF; UI= Underweight/CIAF.
4. Discussion
While comparing WHO standards and CIAF to assess undernutrition, this work also indirectly addresses the limitation of a single measure for assessing undernutrition. In contrast to the conventional indices, relative approach used in this study identified the overall magnitude of undernutrition. To the best of our knowledge ours is the first study to assess anthropometric failure using CIAF among children in the critical age group of 12–24 months in India. In this study, we estimated the magnitude of undernutrition using CIAF as 75% which is higher than Z score observations. This high prevalence was not unexpected, as earlier work using composite index have also provided similar results [[11], [12], [13]]. CIAF among preschool children shows prevalence ranging from 26% in Kashmir [18], to 73% in West Bengal [15]. Recent evidence shows > 50% prevalence of anthropometric failure raising public health concern [[19], [20], [21]]. High prevalence of anthropmetric failure indicates simultaneous coexistance of acute and chronic forms of undernutrition in this critical group. The characteristic outcome in this group is growth faltering that has been attributed to the extent and severity of ponderal growth faltering [22]. The outcome of different levels of severity would manifest either as mortality or developmental delay. Non-fatal outcomes due to undernutrition among children are a serious public health concern globally. The Lancet maternal and child health series has quantified deaths as well as disability adjusted life years (DALY) as a consequence of undernutrition emphasing the need for immediate interventions [1,23].
As observed in other Indian studies [13,15], in our work too stunting emerges as the commonly prevalent type of undernutrition. This calls for strengthening long term interventions to address the intergenerational perpetuation of undernutrition. Between boys and girls in our study, boys showed higher prevalence of stunting, wasting and underweight. Gender differences in nutritional status have been reported in earlier studies as well [[24], [25], [26]]. Culturally if women are given emphasis for their agricultural productivity there is a likelihood for increased attention to female children. There seems to be no biological explanation for male children being more undernourished. Morbidity both symptomatic and asymptomatic has been reported among male children under five years which perhaps could explain the high prevalence of undernutrition among them [27].
Screening for undernutrition is an integral part of the programme of the Ministry of Women and Child Development (MWCD), Government of India [28]. National reports provide data for children under five years [5]. Carefully selected indicators provide right measures of undernutrition. Age appropriate screening and assessment methods are vital to estimate intervention needs. The screening techniques in existing programmes use WAZ to screen underweight, and Mid Upper Arm Circumference (MUAC) to identify extreme wasting. Although targeted interventions for wasting [Severe Acute Malnutrition (SAM) and Modern Acute Malnutrition (MAM)] has been operational in the State, there is a significant increase in wasting. The increased prevalence of wasting in the subcontinent has been attributed to poor maternal health, specifically low prepregnancy BMI, intrauterine growth restriction, acute and severe infections and food insecurity [29]. As the existing interventions follow a curative approach, the likelihood of lack continuum of care as a risk, from the programmatic view cannot be ignored. This could probably be a consequence of screening using single measure for targeted interventions, excluding significant proportions who demonstrate multiple manifests. This is apparent from the NFHS 4 [5] results where there is a decline in one manifest but increase in another. Composite indices for screening and assessment, entwined with continuum of care are likely to address the increase in prevalence of single manifest when another declines. Also, as the manifest of undernutrition varies with age it is important to assess the importance of composite index in different age groups to identify vulnerability and plan age appropriate interventions. Measures to identify common risk factors for any manifest would facilitate in addressing undernutrition relatively.
5. Conclusion
In India, interventions based on current screening appear to harbour a huge burden of undernourished children in the vulnerable group suggesting the need for a composite index for screening, assessment and intervention.
Ethical statement
The study was approved by the institutional ethics committee of Savitribai Phule Pune University. Informed consent was obtained from parents before commencement of the study.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Contributor Information
Waleed Rasheed, Email: washpm-do@iq.missions.acf.org.
Angeline Jeyakumar, Email: angejp@unipune.ac.in.
References
- 1.Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., De Onis M., Ezzati M. Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008 Jan 25;371(9608):243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 2.Victora C.G., Adair L., Fall C., Hallal P.C., Martorell R., Richter L. Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008 Feb 1;371(9609):340–357. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Estimates of global prevalence of underweight in 1990-2008. September 2016. Available in http://www.who.int/nutgrowthdb/publications/underweight1990_2015/en/ Accessed September 2016. [Google Scholar]
- 4.UNICEF the state of World's children report. UNICEF; New York: 2003. [Google Scholar]
- 5.NFHS -4 . International Institute for Population Sciences; 2016. National family health survey 4. Available in, rchiips.org/NFHS/factsheet_NFHS-4. Accessed February 2016. [Google Scholar]
- 6.NFHS-3, National Family Health Survey Available in rchiips.org/NFHS/nfhs3.shtmlAccessed December 2017.
- 7.Adhikari T, Vir SC, Pandey A, Yadav RJ, Jain R, Singh P, et al. Undernutrition in Children Under-Two Years (U2) in India–An Analysis of Determinants.
- 8.Survey - national nutrition monitoring bureau, NNMB, 2006 Available in nnmbindia.org/1_NNMB_Third_Repeat_Rural_Survey___Technicl_Report_26.pdf Accessed December 2017.
- 9.World Health Organization . vol.2014. WHO technical report series; Geneva: 1995. Physical status: the use and interpretation of anthropometry: report of a WHO Expert Committee; p. 854. [PubMed] [Google Scholar]
- 10.Svedberg P. Undernutrition overestimated. Econ Dev Cult Change. 2002 Oct;51(1):5–36. [Google Scholar]
- 11.Nandy S., Irving M., Gordon D., Subramanian S.V., Smith G.D. Poverty, child undernutrition and morbidity: new evidence from India. Bull World Health Organ. 2005 Mar;83(3):210–216. [PMC free article] [PubMed] [Google Scholar]
- 12.Savanur M.S., Ghugre P.S. Magnitude of undernutrition in children aged 2 to 4 years using CIAF and conventional indices in the slums of Mumbai city. J Health Popul Nutr. 2015 Jul 10;33(1):3. doi: 10.1186/s41043-015-0017-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seetharaman N., Chacko T.V., Shankar S.L., Mathew A.C. Measuring malnutrition-The role of Z scores and the composite index of anthropometric failure (CIAF) Indian J Community Med. 2007 Jan 1;32(1):35. [Google Scholar]
- 14.Biswas S., Bose K., Mukhopadhyay A., Bhadra M. Prevalence of undernutrition among pre-school children of Chapra, Nadia District, West Bengal, India, measured by composite index of anthropometric failure (CIAF) Anthropol Anzeiger. 2009 Sep 1:269–279. doi: 10.1127/0003-5548/2009/0025. [DOI] [PubMed] [Google Scholar]
- 15.Mandal G., Bose K. Assessment of overall prevalence of undernutrition using composite index of anthropometric failure (CIAF) among preschool children of West Bengal, India. Iran J Pediatr. 2009;19(3):237–243. [Google Scholar]
- 16.Gadhave S., Nagarkar A. Kuppuswamy Scale for measuring socio-economic status: revised monthly income figures for 2015. Indian J Pediatr. 2015 Dec 1;82(12):1175–1176. doi: 10.1007/s12098-015-1753-z. [DOI] [PubMed] [Google Scholar]
- 17.Blossner M., Siyam A., Borghi E., Onyango A., Onis M. World Health Organization, Department of Nutrition for health and development; Geneva: 2011. Software for assessing growth and development of the world's children. [Google Scholar]
- 18.Anjum F., Pandit M.I., Mir A.A., Bhat I.A. Z Score and CIAF–A comprehensive measure of magnitude of undernutrition in a rural school going population of Kashmir, India. Global J Med Publ Health. 2012 Nov 1;1(5):46–49. [Google Scholar]
- 19.Mukhopadhyay D.K., Biswas A.B. Food security and anthropometric failure among tribal children in bankura, West Bengal. Indian Pediatr. 2011;48:311–314. doi: 10.1007/s13312-011-0057-2. [DOI] [PubMed] [Google Scholar]
- 20.Acharya A., Mandal G.C., Bose K. Overall burden of under-nutrition measured by a Composite Index in rural pre-school children in Purba Medinipur, West Bengal, India. Anthropol Rev. 2013;76(1):109–116. [Google Scholar]
- 21.Goswami M. Prevalence of under-nutrition measured by composite index of anthropometric failure (CIAF) among the bhumij children of northern odisha, India. J Nepal Paediatr Soc. 2016 Oct 22;36(1):61–67. [Google Scholar]
- 22.Chaurasia A.R. Decomposition of body mass growth into linear and ponderal growth in children with application to India. Br J Nutr. 2017 Feb;117(3):413–421. doi: 10.1017/S0007114517000265. [DOI] [PubMed] [Google Scholar]
- 23.Blencowe H., Cousens S., Chou D., Oestergaard M., Say L., Moller A.B. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10(1):S2. doi: 10.1186/1742-4755-10-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asfaw M., Wondaferash M., Taha M., Dube L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Publ Health. 2015 Jan 31;15(1):41. doi: 10.1186/s12889-015-1370-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miah R.W., Apanga P.A., Abdul-Haq Z. Risk factors for undernutrition in children under five years old: evidence from the 2011 Ghana multiple indicator cluster Survey. J AIDS Clin Res. 2016;7(585):2. [Google Scholar]
- 26.Yadav S.S., Yadav S.T., Mishra P., Mittal A., Kumar R., Singh J. An epidemiological study of malnutrition among under five children of rural and urban Haryana. J Clin Diagn Res: J Clin Diagn Res. 2016 Feb;10(2) doi: 10.7860/JCDR/2016/16755.7193. LC07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wamani H., Åstrøm A.N., Peterson S., Tumwine J.K., Tylleskär T. Boys are more stunted than girls in sub-Saharan Africa: a meta-analysis of 16 demographic and health surveys. BMC Pediatr. 2007 Dec 1;7(1):17. doi: 10.1186/1471-2431-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Child development schemes . September, 2016. Ministry of women and child development.http://wcd.nic.in/schemes-listing/2404 GOI. Accessed September 2016. [Google Scholar]
- 29.Martorell R., Young M.F. Patterns of stunting and wasting: potential explanatory factors. Adv Nutr: An Int Rev J. 2012 Mar 1;3(2):227–233. doi: 10.3945/an.111.001107. [DOI] [PMC free article] [PubMed] [Google Scholar]