Abstract
Problematic drinking is a serious and persistent problem among U.S. military service members and veterans, who face barriers to seeking help and are less likely to seek help than the civilian population. One way to reach this population is through spouses or partners who are concerned about the service members’ drinking (concerned partners [CPs]). CPs of military service members were recruited for a web-based intervention, Partners Connect, that aimed to improve patterns of communication about the service members’ drinking. Participants were 234 CPs (95% female; 71% White; 89% married; average age 32 years) who completed a baseline survey, were randomized to a four-session web-based intervention or a waitlist control group, and completed a follow-up assessment five months later. Three measures reported by CPs assessed perceived partner drinking (drinks per week, highest number of drinks across a typical week, and frequency of drinking in the past month) and CP behaviors were assessed using the Significant-other Behavior Questionnaire (SBQ) and the State-Trait Anger Expression Inventory (STAXI-2). Results demonstrated that the intervention did not have a main effect on CP behaviors relative to control. However, changes in CP punishment of partner drinking and behaviors supporting sobriety were significantly associated with decreased perceived partner drinking and improved relationship quality over time. Furthermore, compared to the control group, to the extent that CPs in the treatment group reduced their negative behaviors, perceived partner drinking declined and relationship quality improved. The results reinforce the importance of considering CP behaviors when designing interventions to reduce drinking.
Keywords: military spouse, alcohol, mental health, service member, veteran, relationships
1.1. Introduction
U.S. military service members and veterans often struggle with problem drinking (Institute of Medicine, 2012), including frequent episodes of heavy drinking (Bray et al., 2009; Stahre, Brewer, Fonseca, & Naimi, 2009). Problematic drinking is associated with numerous consequences in the military, including fitness for duty, absenteeism, depression, anxiety (LeardMann et al., 2013; Mattiko, Olmsted, Brown, & Bray, 2011), and suicide (LeardMann et al., 2013). Despite the significant impacts of problematic drinking on this population, service members and veterans are disproportionately less likely to seek help than the civilian population. Help-seeking is seen as stigmatizing among service members (Gibbs, Rae Olmsted, Brown, & Clinton-Sherrod, 2011; Institute of Medicine, 2012; Kulesza, Pedersen, Corrigan, & Marshall, 2015; Osilla et al., 2016), and administrative rules that require commanding officer’s involvement in treatment deter many from seeking help for fear of job repercussion (Burnett-Zeigler et al., 2011; Department of Defense Instruction, 2014). There is evidence that these barriers continue after active service ends, even though the risk of harming one’s career by seeking help is diminished (Ouimette et al., 2011; Vogt, 2011).
One solution to circumvent these barriers is to work around the traditional military health care system and use alternative methods for delivering alcohol interventions to service members and veterans, such as through stand-alone self-help approaches that can be delivered over the Internet on computers, tablets, or mobile phones. Yet, adoption of these approaches may be difficult if an individual with problem drinking does not consider the need to change their behavior. Concerned partners (CPs) of service members and veterans may be an ideal intervention target because s/he is likely a first-line identifier of their partner’s alcohol-related problems (Sobell & Sobell, 1993). As such, CPs can communicate with their partners about how their drinking affects their family, as well as be a support system if they do decide to pursue treatment (Marshal, 2003; Smith & Meyers, 2007; Steinglass & Robertson, 1983). However, how this communication is executed has a significant effect on partner drinking and relationship outcomes. Research suggests that negative interaction patterns such as the CPs punishing their partner when they drink (e.g., expressing anger, threatening them) is associated with poorer outcomes such as heavier drinking and poorer relationship satisfaction (Overall & Fletcher, 2010; Rodriguez, DiBello, & Neighbors, 2013; Rodriguez, DiBello, & Wickham, 2016). This pattern is consistent with domain-specific models of social control, which specify that attempts to change a partner’s behavior based on positive reinforcement are more effective and linked with better relationship outcomes than are attempts to change a partner’s behavior based on punishment (Craddock, vanDellen, Novak, & Ranby, 2015). Thus, a major component of CP-focused interventions targets CP behaviors towards their partner with the theory that changes in CP behaviors can affect partner problem behaviors (Rhule-Louie & McMahon, 2007).
The Community Reinforcement and Family Training (CRAFT) intervention was developed specifically to help concerned significant others, family members, or partners engage treatment-resistant problem drinkers with alcohol treatment by teaching supportive and non-confrontational skills to cope with problematic drinking through positive communication and rewarding sobriety (e.g., planning pleasant activities that do not involve drinking). Research supports the efficacy of CRAFT in increasing entry into treatment for alcohol use disorder (Miller, Meyers, & Tonigan, 1999).
Although communication and interaction are key components of CRAFT and thought to influence the drinker’s treatment initiation (Roozen, de Waart, & van der Kroft, 2010), studies have yet to formally evaluate whether intervention-related changes in CP behaviors are associated with changes in partner drinking. The current study addresses this gap in research by examining the relationship between changes in CP behaviors in response to a web-based adaptation of CRAFT and partner changes in drinking. This study is a secondary data analysis of a randomized controlled trial that compared the efficacy of a web-based intervention (WBI), Partners Connect, to a waitlist control condition among CPs of service members or veterans (Osilla, Pedersen, Gore, Trail, & Howard, 2014; Osilla et al., 2017). Previous research using this dataset found that WBI CPs had reduced anxiety and increased social support five months after the intervention compared to control (Osilla et al., 2017), WBI CPs with heavy drinking had greater improvements in their depression (Rodriguez, Osilla, Trail, Gore, & Pedersen, 2017), and in qualitative interviews CPs reported improved communication from the WBI (Osilla et al., 2016).
The current research examines how changes in CP behavior as a result of the WBI are linked with changes in perceived partner drinking and relationship functioning. We focus on changes in three key CP behavioral strategies emphasized in the WBI: reducing behaviors that punish or negatively reinforce partner drinking, increasing behaviors supporting partner sobriety, and decreasing the ineffective expression of anger. We also examined changes in CP behaviors that support partner drinking and CP withdrawal from partners (such as leaving the house), when they are drinking. Thus, we examined three research questions (RQs):
RQ1: On average, was the WBI associated with changes in CP behaviors?
RQ2: Compared to control CPs, were changes in CP behaviors in the WBI condition associated with decreased perceived partner drinking over time?
RQ3: Compared to control CPs, were changes in CP behaviors associated with changes in relationship quality over time?
2.1. Method
2.2. Participants
We recruited 483 CPs of military service members or veterans through Facebook advertisements (Pedersen, Osilla, Helmuth, Tolpadi, & Gore, 2017). CPs completed a 10-item online screening survey assessing their eligibility for the study. Eligibility criteria were adapted from those used in previous CRAFT trials (Meyers, Miller, Smith, & Tonigan, 2002; Miller et al., 1999). To be eligible for the study, CPs needed to live with a romantic partner who was a current or former service member in the U.S. military and was rated by the CP as having an alcohol problem (i.e., when asked if their partner had an alcohol problem, they responded with a value of “3” or more on scale from “1 not at all” to “7 very much”). CPs had to be at least 18 years old, not currently be in the military themselves, and have Internet access (additional eligibility criteria are detailed in Osilla et al., 2017). Participants consented to be randomly assigned to receive the intervention immediately or after their 5-month follow-up survey. Control participants were then sent an email with a link and instructions to access the intervention. CPs meeting the eligibility criteria advanced to the consent form and baseline survey, and then were randomized to condition.
Of the 483 CPs recruited, 312 screened eligible for the study and completed the baseline survey. CPs were then randomized to either the WBI or a waitlist control condition. An error in the randomization procedure erroneously assigned 24 CPs to the WBI instead of the control group. Checks on demographic characteristics and the results reported in this paper found no differences between the erroneously assigned CPs and the truly randomized WBI participants, so we included them in the analyses as WBI participants. Data verification checks identified six CPs (one control, 5 WBI) with inconsistent demographic through a series of data verification checks (e.g. partner’s pay grade and reported rank did not match), which gave us a baseline sample of 306 (181 WBI and 125 control) participants. Most participants (N=306) were female (95%); White (71%); married to their partner (89%, M=7.5 years, SD=4.9), had children (77%), and had not attended any college (59%). Average participant age was 32 years (SD=6.5). Of the 306 who completed the baseline survey, 234 completed the follow-up (76.5%) survey emailed to them five months after baseline, resulting in 136 WBI and 98 control CPs in our final analytic sample. The rate of attrition and factors associated with attrition did not differ between groups.
2.3. Procedure
Participants who clicked through the Facebook ad were directed to the study website to find out more information and complete the screener survey to determine their eligibility for the study. CPs were compensated for completing the baseline ($50) and follow-up ($50) surveys. To encourage follow-up survey completion among CPs who were hard-to-reach or about to time out of the 60-day follow-up window (n = 50), we increased the follow-up survey incentive to $75 near the end of the study. After completing the baseline survey, a computer algorithm randomly assigned CPs to the WBI or the control condition using permuted block randomization with random size blocks (Pocock, 1984). Participants completed a five-month follow-up survey, after which control participants were offered the intervention (see Osilla et al., 2017).
2.3.1. Partners Connect Intervention
We developed a web-based adaptation of CRAFT called Partners Connect for military and veteran CPs that consisted of four 30–45 minute sessions spaced one week apart and was accessible by CPs at any time (Osilla et al., 2016). Partners Connect included the Motivational Interviewing and Cognitive Behavioral Therapy techniques used in CRAFT to engage CPs in self-care and help-seeking by building self-efficacy and intrinsic motivation to change and to help CPs learn to modify their behaviors and actions to improve their psychological functioning. The overall objective of the intervention was to equip CPs with increased self-care and positive communication strategies regarding their partner’s drinking, and to serve as a first step for engaging CPs that could encourage their partner to seek additional care later, if needed. Out of the four available sessions, CPs completed an average of 1.8 sessions (SD = 1.86) with 13% completing no sessions and 65% completing all four sessions.
2.4. Measures
2.4.1. Partner’s alcohol consumption
Given that CPs were recruited independently from their partners and may not have wanted to share their participation with their partner, we relied on CPs’ reports of their partner’s alcohol use. We purposefully designed the study to avoid collecting data directly from service members because this would have deterred CPs from participating and might have led to mandated reporting. CPs reported their perceptions of their partners’ alcohol consumption using two measures. CPs completed the Drinking Norms Rating Form (Baer, Stacy, & Larimer, 1991)—a modified version of the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985)—which assessed CP perceptions of how much their partner drank each day in a typical week during the past month. From this assessment, we calculated two measures of partner drinking (Collins et al., 1985). First, we used the highest number of drinks consumed on any day in a typical week. Second, we summed the number of drinks in a typical week in the past 30 days to form a measure of average total number of drinks per week. In addition to the DDQ, we assessed partner frequency of past month drinking by having CPs report the number of days their partner drank one or more drinks in the last 30 days. Collateral report of frequency and quantity of partner drinking has been documented with high reliability (97%) (Babor, Steinberg, Anton, & Del Boca, 2000) and used extensively in many studies (e.g., Carroll, 1995; Roozen et al., 2010).
2.4.2. Relationship quality
CP perceptions of the quality of their relationship with their partner was measured using the 6-item Quality of Marriage Index (QMI; Norton, 1983; α = .96). Example items include, “Our relationship is strong” and “I really feel like part of a team with my partner.”
2.4.3. CP behaviors towards partner drinking
CPs self-reported their behaviors toward their partner’s drinking and abstinence using the Significant-other Behavior Questionnaire (SBQ; Love, Longabaugh, Clifford, Beattie, & Peaslee, 1993). SBQ subscales include five items assessing CP punishment of partner’s drinking (e.g., trying to stop a partner’s drinking by getting angry, α = .84); eight items assessing CP support of partner sobriety (e.g., spending more time with a partner when he/she was not drinking, α = .85); three items assessing CP support for partner drinking (e.g., bringing alcoholic beverages home, α = .66); and four items assessing CP withdrawal from partner’s drinking (e.g., refusing to be home with a partner when he/she was drinking, α = .70). Items were rated on a four-point scale ranging from “Never” to “Always/Almost Always” and were summed to form four measures of CP behavior: Punishment, Support Sobriety, Support Drinking, and Withdrawal.
2.4.4. Anger expression
We measured CPs’ expression of anger toward other persons, objects, or anger directed inward using the State-Trait Anger Expression Inventory (STAXI-2; Spielberger, 1999). We calculated an anger expression index using the sum of all items on the scale (α = .76) where higher values indicated more intense anger that is suppressed, expressed aggressively, or both. Example items include, “I feel like cursing out loud” and, “I am a hotheaded person.”
2.5. Analysis Plan
We used linear regression models to estimate the effect of the WBI on CP behaviors (RQ1) and to estimate whether changes in CP behaviors were associated with changes in partner drinking (RQ2) and CP relationship quality (RQ3) over time. For RQ1, we constructed models predicting behaviors at the five-month follow-up (time 2) from WBI condition, controlling for baseline (time 1) behaviors and the covariates (described below). RQ2 and RQ3 required a different approach. Since we predicted that changes in outcomes would depend on changes in CP behavior, and that this relationship would differ between WBI and control groups, we constructed regression models predicting changes in outcomes from baseline to follow-up from changes in CP behaviors and the interaction between WBI condition and CP behavior change. Changes in CP behaviors from baseline to follow-up were calculated using the difference score between time 1 and time 2 measures (i.e., time 1 behaviors – time 2 behaviors), where higher numbers represent decreased frequency of behaviors at time 2 compared to time 1. CP behaviors were the four SBQ subscales (punishing drinking, supporting sobriety, supporting drinking, withdrawing) and CP anger expression. Outcomes were perceived partner drinking behavior (drinks per week, highest number of drinks across a typical week, and frequency of drinking in the past month) and CP ratings of relationship quality.
Separate models were run for each behavior and outcome, and models regressed the outcome at time 2 on the outcome at time 1, the CP behavior at time 1, the difference score between time 1 and time 2 CP behaviors, a dummy variable indicating WBI condition, and the interaction between WBI condition and the CP behavior difference score. The CP behavior at time 1 was included to control for initial levels of behavior, which could impact the level of change found in the CP behavior difference score (e.g., CPs with low levels of behaviors at time 1 would be more likely to show an increase in behaviors at time 2 than would CPs with higher levels of behaviors at time 1). A significant interaction between WBI condition and the CP behavior difference score indicated that the association between changes in CP behaviors and changes in perceived partner drinking differed between the WBI and control conditions.
We included the following set of covariates in all models: age, CP education (college graduate or higher vs. less than college graduate), military status (veteran vs. active duty/reserve/guard) and enlisted status (enlisted vs. officer). The literature suggests that younger active duty service members drink more heavily than older active duty service members (Institute of Medicine, 2012; Seal et al., 2011), and veterans engage in more frequent episodic drinking than active or reserve/guard service members (Ramchand et al., 2011). In addition, active duty service members face barriers to help-seeking that veterans may not face (e.g., mandated reporting guidelines; Institute of Medicine, 2012), so we controlled for age and partner military status (veteran vs. active duty/reserve/guard).. We controlled for the presence of children because couples with children generally report lower marital quality compared to couples without children (e.g., Doss, Rhoades, Stanley, & Markman, 2009). Finally, we controlled for CP education because CPs in the control condition were significantly more educated than WBI CPs.
Because we were interested in reductions in partner drinking from baseline to follow-up, we deleted partners who, according to their CP, had not drank alcohol in the past 30 days at baseline (n = 6). The results reported below do not differ when these participants are included in the models. We checked the data for univariate and multivariate outliers. Univariate outliers were found for both measures of partner drinking, and these were trimmed to the next highest value. No multivariate outliers that had a disproportionate influence on the models were found.
3.1. Results
3.2. RQ1: On average, was the WBI associated with changes in CP behaviors?
Table 1 shows the means and standard deviations for variables in the study across conditions. Overall, the intervention was not associated with a significant change in CP behaviors relative to the control group. None of the CP behaviors significantly differed over time between the WBI and control groups (all ps ≥ .10).
Table 1.
Means and standard deviations for outcome and predictor variables in models.
| Condition | ||||
|---|---|---|---|---|
| Web-Based Intervention (WBI) | Delayed Web-Based Intervention (control) | |||
| Variable | Baseline Mean (SD) | Follow-Up Mean (SD) | Baseline Mean (SD) | Follow-Up Mean (SD) |
| Highest number of drinks on a typical day | 7.78 (4.75) | 5.03 (4.19) | 7.14 (4.51) | 5.41 (4.76) |
| Total number of drinks in a typical week | 27.18 (16.98) | 17.60 (16.78) | 28.55 (20.16) | 20.84 (20.83) |
| Number of drinking days in the past month | 20.34 (8.84) | 14.61 (11.03) | 20.31 (9.10) | 16.03 (11.62) |
| Relationship quality | 34.03 (13.38) | 38.18 (14.77) | 37.05 (13.43) | 38.29 (14.82) |
| Punishing Drinking | 11.12 (3.90) | 8.70 (3.89) | 10.72 (3.74) | 8.31 (3.56) |
| Supporting Sobriety | 22.30 (4.86) | 22.54 (6.15) | 22.50 (5.47) | 21.10 (6.82) |
| Supporting Drinking | 5.48 (1.91) | 5.25 (1.82) | 5.70 (2.11) | 4.98 (1.85) |
| Withdraw When Drinking | 7.02 (2.61) | 6.52 (2.73) | 6.56 (2.51) | 6.06 (2.49) |
| Anger Expression | 36.91 (13.53) | 35.82 (15.78) | 33.73 (13.38) | 35.01 (12.28) |
3.3. RQ2: Compared to control CPs, were changes in CP behaviors in the WBI condition associated with decreased perceived partner drinking over time?
As noted elsewhere (Osilla et al., 2017), the intervention was not associated with a decrease in perceived partner drinking, although partner drinking did decline over time for both WBI and control groups (see Table 1). To examine whether changes in CP behaviors were associated with changes in partner drinking, we analyzed the relationship between CP behaviors in the WBI and control groups and partner drinking behaviors (as perceived by the CP). We examined the overall association between changes in behaviors and partner drinking over time, and then tested whether these associations differed between the WBI and control conditions.
3.3.1. Perceived highest number of drinks on a typical day
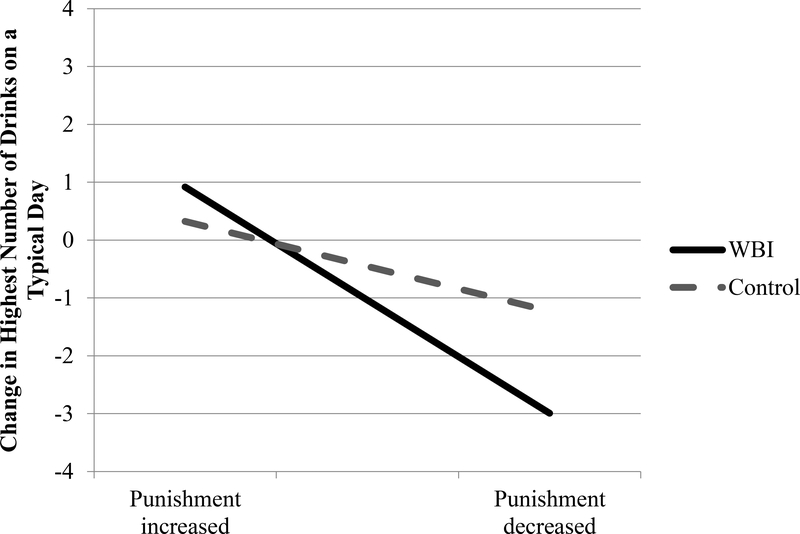
Regression results are shown in Table 2, with Model 1 displaying the association between decreases in behaviors from time 1 to time 2 and outcomes, and Model 2 displaying the moderation of this effect by WBI condition. Examining the association between CP punishing behaviors and perceived highest number of drinks that their partner had on a typical day, we found that decreases in CP punishing behaviors from time 1 to time 2 were associated with significant reductions in perceived partner drinking over time, and that this relationship was significantly moderated by WBI condition. As shown in Figure 1, decreases in punishment from time 1 to time 2 were significantly associated with decreases in partner’s perceived highest number of drinks on a typical day for the WBI group (b = −0.51, SE = 0.09, t[109] = −5.49, p < .001), but not for the control group (b = −0.25, SE = 0.14, t[65] = −1.82, p = .07).
Table 2.
Regression main effects for behavior change over time and interactions with intervention condition.
| Punishing Drinking | Supporting Sobriety | Supporting Drinking | Withdraw When Drinking | Anger Expression | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Main Effect | Interaction with WBI | Main Effect | Interaction with WBI | Main Effect | Interaction with WBI | Main Effect | Interaction with WBI | Main Effect | Interaction with WBI | |
| b | b | b | b | b | b | b | b | b | b | |
| Outcome | (SE) | (SE) | (SE) | (SE) | (SE) | (SE) | (SE) | (SE) | (SE) | (SE) |
| Highest number of drinks on a typical day | −0.42*** | −0.031* | 0.10* | 0.05 | −0.31* | −0.01 | −0.02 | −0.01 | −0.01 | −0.14** |
| (0.08) | (0.14) | (0.14) | (0.07) | (0.04) | (0.25) | (0.12) | (0.22) | (0.02) | (0.05) | |
| Total number of drinks in a typical week | −1.39*** | −0.76 | 0.43** | 0.28 | −0.38 | −0.83 | −0.26 | −0.57 | 0.01 | −0.48** |
| (0.31) | (0.58) | (0.16) | (0.29) | (0.59) | (1.01) | (0.45) | (0.87) | (0.10) | (0.19) | |
| Number of drinking days in the past month | −0.87*** | −0.28 | 0.35** | 0.20 | −0.94* | 0.72 | −0.63* | 0.44 | −0.07 | −0.25† |
| (0.21) | (0.38) | (0.11) | (0.20) | (0.40) | (0.69) | (0.30) | (0.56) | (0.07) | (0.14) | |
| Relationship quality | 1.54*** | 1.22** | −0.61*** | −0.28 | −0.52 | 1.21 | 1.74*** | 0.25 | 0.33*** | 0.30† |
| (0.26) | (0.47) | (0.14) | (0.25) | (0.51) | (0.87) | (0.38) | (0.71) | (0.09) | (0.17) | |
Note: WBI = Web-Based Intervention. Models controlled for age, CP education, military status, and enlisted status.
p < .10
p < .05
p < .01
p < .001
Figure 1. Relationship between changes in punishment of partner drinking from time 1 to time 2 and changes in partner’s highest number of drinks on a typical day.
Note: Following Aiken and West (1991) and Cohen, Cohen, West, and Aiken (2003), lines are graphed at 1 SD above and below the mean change in punishment from baseline. Simple slopes tests for difference from 0 were: WBI b = −0.51, SE = 0.09, t(109) = −5.49, p < .001; Control b = −0.25, SE = 0.14, t(65) = −1.82, p = .07.
We found that increases in supporting partner sobriety were significantly associated with decreases in the partner’s perceived highest number of drinks on a typical day. This relationship was not significantly moderated by WBI condition. Increases in supporting partner drinking were significantly associated with increases in the partner’s perceived highest number of drinks on a typical day, and this relationship was also not moderated by WBI condition. Changes in withdrawal from partner when drinking were not significantly associated with changes in partner’s perceived highest number of drinks on a typical day, and this relationship was also not moderated by WBI condition.
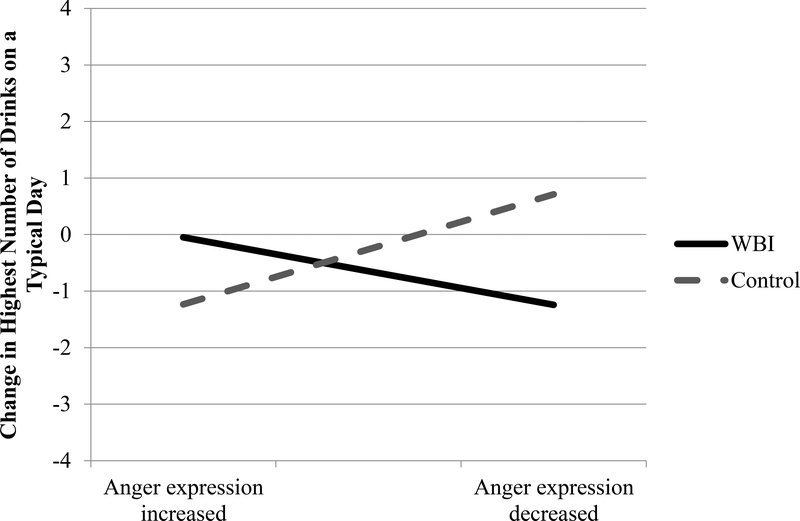
Analyses revealed that decreases in CP anger expression from time 1 to time 2 was not significantly associated with decreases in partners’ perceived highest number of drinks on a typical day over time. However, WBI condition significantly moderated this relationship. As shown in Figure 2, decreases in CP anger expression from time 1 to time 2 were marginally significantly associated with decreases in the partner’s perceived highest number of drinks on a typical day for the WBI group (b = −0.05, SE = 0.03, t[108] = −1.91, p = .059). Decreases in CP anger expression were associated with a significant increase in partner’s perceived highest number of drinks on a typical day for the control group (b = 0.09, SE = 0.05, t[69] = 2.02, p = .045).
Figure 2. Relationship between changes in CP anger expression from time 1 to time 2 and changes in partner’s highest number of drinks on a typical day.
Note: Following Aiken and West (1991) and Cohen, Cohen, West, and Aiken (2003), lines are graphed at 1 SD above and below the mean change in anger expression from baseline. Simple slopes tests for difference from 0 were: WBI b = −0.05, SE = 0.03, t(108) = −1.91, p = .059; Control b = 0.09, SE = 0.05, t(69) = 2.02, p = .045.
3.3.2. Perceived total number of drinks in a typical week
We next examined the relationship between perceived total number of drinks and CP punishment of partner drinking. As shown in Table 2, we found that decreases in CP punishment of partner drinking was significantly associated with decreased perceived partner drinks per week from time 1 to time 2. The relationship between punishment of drinking and perceived partner drinks per week was not significantly moderated by WBI condition.
We next examined CP behaviors supporting partner sobriety and found that, controlling for baseline behaviors, increases in CP behaviors supporting partner sobriety were significantly associated with decreased perceived partner drinks per week from time 1 to time 2. This relationship was not moderated by WBI condition. Changes in supporting partners drinking were not significantly associated with perceived partner drinks per week, and this relationship was not moderated by WBI condition. Withdrawing from partner when drinking was also not significantly associated with perceived partner drinks per week, and this relationship was also not moderated by WBI condition.
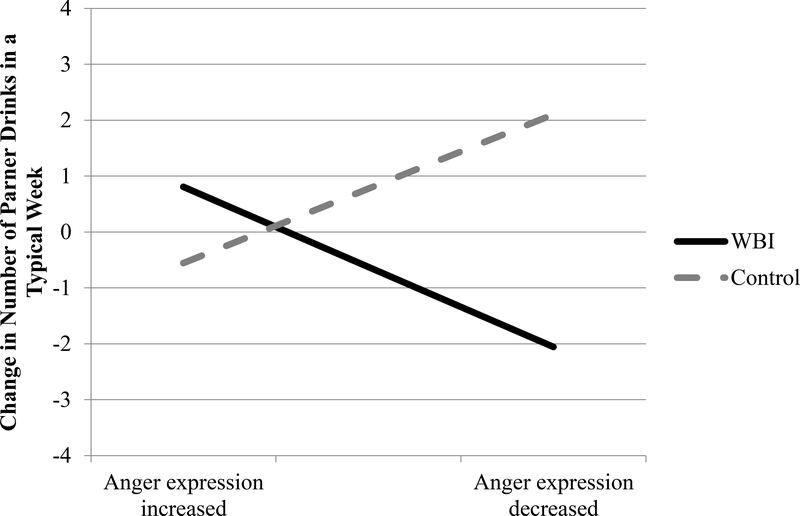
Anger expression was not significantly associated with perceived partners’ sum total number of drinks in a typical week, but this relationship was significantly moderated by WBI condition. As shown in Figure 3, decreases in CP anger expression from time 1 to time 2 were not significantly associated with decreases in perceived partners’ drinks per week for the WBI group (b = −0.13, SE = 0.11, t[103] = −1.11, p = .27), but decreases in CP anger expression were marginally significantly associated with increases in perceived partners’ drinks per week for the control group (b = 0.36, SE = 0.18, t[65] = 2.00, p = .05).
Figure 3. Relationship between changes in CP anger expression from time 1 to time 2 and changes in partner’s total number of drinks in a typical week.
Note: Following Aiken and West (1991) and Cohen, Cohen, West, and Aiken (2003), lines are graphed at 1 SD above and below the mean change in anger expression from baseline. Simple slopes tests for difference from 0 were: WBI b = −0.13, SE = 0.11, t(103) = −1.11, p = .27; Control b = 0.36, SE = 0.18, t(65) = 2.00, p = .05.
3.3.3. Frequency of perceived partner drinking in the past month
As shown in Table 2, controlling for baseline levels of punishment behaviors, decreases in CP punishment of partner drinking was significantly associated with decreased frequency of perceived partner past month drinking from time 1 to time 2, and this relationship was not significantly moderated by WBI condition. Increases in CP behaviors supporting partner sobriety were also significantly associated with decreased frequency of perceived partner past month drinking over time, and this relationship was not moderated by WBI condition. Decreases in supporting partners drinking were significantly associated with decreased frequency of perceived partner past month drinking over time, and this relationship was not moderated by WBI condition. Decreases in withdrawing from partner when drinking were significantly associated with decreased frequency of perceived partner past month drinking over time, and this relationship was not moderated by WBI condition.
Finally, changes in anger expression were not significantly associated with changes in frequency of perceived partner past month drinking over time, and this relationship was marginally significantly moderated by WBI condition. The simple slopes for changes in frequency of perceived partner past month drinking on decreased CP anger expression were in the expected directions for the WBI (b = −0.12, SE = 0.08) and DWI (b = 0.03, SE = .13) groups, but neither effect approached significance (ps = .14 and .83, respectively).
3.4. RQ3: Compared to control CPs, were changes in CP behaviors associated with changes in relationship quality over time?
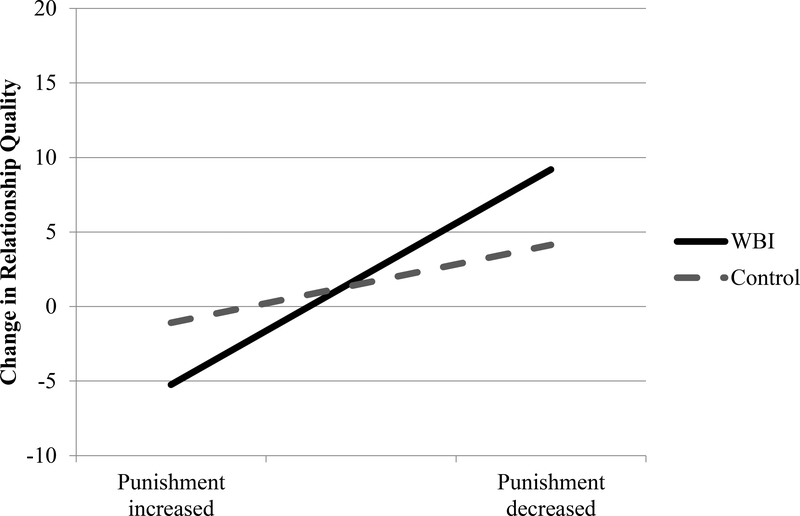
Next, we examined the relationship between changes in CP behaviors and CP perceptions of relationship quality over time. As noted elsewhere (Osilla et al., 2017), the WBI did not change overall CP perceptions of relationship quality. As shown in Table 2, we found that decreases in CP punishment of partner drinking was significantly associated with increased relationship quality from time 1 to time 2. Further, the relationship between punishment of drinking and relationship quality was significantly moderated by WBI condition. As shown in Figure 4, decreases in punishment from time 1 to time 2 were significantly associated with increases in relationship quality for the WBI group (b = 1.93, SE = 0.33, t[108] = 5.91, p < .001), but not for the control group (b = 0.77, SE = 0.44, t[64] = 1.74, p = .09).
Figure 4. Relationship between changes in punishment of partner drinking from time 1 to time 2 and changes in CP perceptions of relationship quality.
Note: Following Aiken and West (1991) and Cohen, Cohen, West, and Aiken (2003), lines are graphed at 1 SD above and below the mean change in punishment from baseline. Simple slopes tests for difference from 0 were: WBI b = 1.93, SE = 0.33, t(108) = 5.91, p < .001; Control b = 0.77, SE = 0.44, t(64) = 1.74, p = .09.
We next examined CP behaviors supporting partner sobriety and found that, controlling for baseline behaviors, increases in CP behaviors supporting partner sobriety were significantly associated with increased CP perceptions of relationship quality from time 1 to time 2. This relationship was not moderated by WBI condition. Changes in supporting partner drinking were not significantly associated with CP perceptions of relationship quality, and this relationship was not moderated by WBI condition. Decreased withdraw from partner when drinking was significantly associated with greater relationship quality over time, and this relationship was not moderated by WBI condition.
Finally, decreases in CP anger expression were significantly associated with increased relationship quality from time 1 to time 2. This relationship was marginally significantly moderated by WBI condition. Decreases in CP anger expression from time 1 to time 2 were significantly associated with increases in relationship quality for the WBI group (b = 0.37, SE = 0.11, t[106] = 3.43, p < .001), and this association was marginally significant for the control group (b = 0.26, SE = 0.14, t[67] = 1.78, p = .08).
4.1. Discussion
The current research sought to examine whether changes in CP behaviors were associated with decreased partner drinking and improved relationship quality, and if these associations were moderated by a CP-focused web-based intervention. Across conditions, changes in CP behaviors over time were significantly associated with decreased partner drinking and improved relationship quality. We found that the WBI was not significantly associated with changes in CPs’ mean levels of behaviors toward their partners’ drinking or their expression of anger. However, WBI CPs who did change their behavioral strategies (i.e., punishing drinking or anger expression) also reported a significant decrease in perceived partner drinking over the course of the study. This was not the case for CPs in the control group, which suggests that the WBI was associated with better communication patterns between CPs and their partners about their drinking, and that changes in behavior without the aid of the WBI did not have as strong of an association with perceived partner drinking. Furthermore, decreases in CP punishing behavior and anger expression were associated with improved relationship quality over time for WBI CPs, but not for control CPs. Thus, changes in CP behaviors in the WBI condition were associated with both decreased perceived partner drinking and improved relationship quality.
These findings help clarify how interventions targeting negative social control (Craddock et al., 2015) may have the potential to decrease partner drinking while also improving their relationship quality. Previous research has documented an association between negative CP interaction patterns and poorer outcomes such as heavier partner drinking and poorer relationship satisfaction (Overall & Fletcher, 2010; Rodriguez et al., 2013). The current research adds to this literature by demonstrating that changes in CP behaviors over time are associated with decreased partner drinking and improved relationship quality. In particular, changes in CP behaviors supporting sobriety were associated with decreased partner drinking and improved relationship quality for both WBI and control participants. These findings are particularly important for the military population who face pervasive help-seeking barriers for problem drinking and offer innovative strategies for reaching them through their partners.
Although the current study has many strengths, it also has limitations and the results should be interpreted with some caution. First, the measures used in this study were self-reported by CPs, so it is possible that CPs could have underreported their use of behavioral strategies and/or misreported their partners’ drinking behavior (e.g., because they did not witness all their partners’ drinking). However, it is likely that these biases would affect CPs in both the WBI and control conditions, so respondent bias would not completely explain the results reported in this paper. Future research should assess CP and partner behaviors through more objective measures (e.g., dyadic measures of behaviors). Second, several statistical tests were performed which could result in positive results by chance alone. Results should be interpreted with caution. Third, we cannot make causal statements about the results. There was no main effect of the WBI on partner drinking behavior or CP behaviors toward partner drinking, and our measures were collected at two time points, so the direction of causality is unclear. For example, it is possible that the military member’s drinking behavior may have reduced over time, which in turn resulted in less anger expression and punishment on the part of the CP. Also, many of the self-reported behaviors decreased from time 1 to time 2, possibly because of regression to the mean, and these changes may have hindered our ability to find differences between conditions over time. Future studies dismantling whether communication and behavioral skills in the WBI directly influences CP behaviors and partner drinking across a longer follow-up using more defined time periods (e.g., daily diaries, event sampling) is needed to understand the processes by which CP behaviors are associated with partner drinking.
4.2. Conclusions
CPs can be an important catalyst for changing their partner’s drinking, and this study explores one alternative to circumvent the challenge of preventing alcohol use disorders among military personnel. Reducing CP’s expression of anger and punishment with respect to partners’ drinking may be helpful in reducing military members’ drinking behavior. Learning effective and adaptive ways to interact with their partner—to avoid punishing them and to limit expressions of anger—are a potential key to helping CPs influence their partners’ drinking behaviors and enhance the quality of their relationship.
Highlights.
No effect of training on partners’ behaviors toward service member problem drinking
Partner drinking associated with less punishment and more support for sobriety
Partners drink less when participants decrease negative behaviors with training
Participants who decrease negative behaviors with training have better relationships
Acknowledgements
The current study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA; 1R34AA023123, Principal Investigator: Karen Chan Osilla). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAAA or the National Institutes of Health.
Footnotes
Trial registration
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LS, & West SG (1991). Multiple Regression: Testing and interpreting interactions. Thousand Oaks: Sage. [Google Scholar]
- Babor TF, Steinberg K, Anton R, & Del Boca F (2000). Talk is cheap: measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol, 61(1), 55–63. [DOI] [PubMed] [Google Scholar]
- Baer JS, Stacy A, & Larimer M (1991). Biases in the Perception of Drinking Norms among College-Students. Journal of Studies on Alcohol, 52(6), 580–586. [DOI] [PubMed] [Google Scholar]
- Bray RM, Pemberton MR, Hourani LL, Witt M, Olmsted KL, Brown JM, … Scheffler S (2009). Department of Defense survey of health related behaviors among active duty military personnel. Retrieved fromhttp://www.tricare.mil/2008HealthBehaviors.pdf
- Burnett-Zeigler I, Ilgen M, Valenstein M, Zivin K, Gorman L, Blow A, … Chermack S (2011). Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addictive Behaviors, 36(8), 801–806. [DOI] [PubMed] [Google Scholar]
- Carroll KM (1995). Methodological issues and problems in the assessment of substance use. Psychological Assessment, 7(3), 349–358. doi: 10.1037/1040-3590.7.3.349 [DOI] [Google Scholar]
- Cohen J, Cohen P, West SG, & Aiken LS (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ: Erlbaum. [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. doi: 10.1037/0022-006X.53.2.189 [DOI] [PubMed] [Google Scholar]
- Craddock E, vanDellen MR, Novak SA, & Ranby KW (2015). Influence in relationships: A meta-analysis on health-related social control. Basic and Applied Social Psychology, 37(2), 118–130. doi: 10.1080/01973533.2015.1011271 [DOI] [Google Scholar]
- Department of Defense Instruction. (2014). Problematic Substance Use by DoD Personnel, Number 1010.04. Retrieved from http://www.dtic.mil/whs/directives/corres/pdf/101004p.pdf
- Doss BD, Rhoades GK, Stanley SM, & Markman HJ (2009). The effect of the transition to parenthood on relationship quality: An 8-year prospective study. Journal of Personality and Social Psychology, 96(3), 601–619. doi: 10.1037/a0013969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs DA, Rae Olmsted KL, Brown JM, & Clinton-Sherrod AM (2011). Dynamics of stigma for alcohol and mental health treatment among army soldiers. Military Psychology, 23(1), 36–51. doi: 10.1080/08995605.2011.534409 [DOI] [Google Scholar]
- Institute of Medicine. (2012). Substance use disorders in the U.S. armed forces. Retrieved from https://www.nap.edu/resource/13441/SUD_rb.pdf
- Jackson SE, Steptoe A, & Wardle J (2015). The influence of partner’s behavior on health behavior change: the English longitudinal study of ageing. JAMA Internal Medicine, 175(3), 385–392. [DOI] [PubMed] [Google Scholar]
- Kulesza M, Pedersen ER, Corrigan PW, & Marshall GN (2015). Help-Seeking Stigma and Mental Health Treatment Seeking Among Young Adult Veterans. Military Behavioral Health, 3(4), 230–239. doi: 10.1080/21635781.2015.1055866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, … Hoge, C. W. (2013). Risk factors associated with suicide in current and former US military personnel. JAMA, 310(5), 496–506. [DOI] [PubMed] [Google Scholar]
- Love CT, Longabaugh R, Clifford PR, Beattie M, & Peaslee CF (1993). The Significant other Behavior Questionnaire (SBQ): An instrument for measuring the behavior of significant others towards a person’s drinking and abstinence. Addiction, 88(9), 1267–1279. [DOI] [PubMed] [Google Scholar]
- Marshal MP (2003). For better or for worse? The effects of alcohol use on marital functioning. Clinical Psychology Review, 23(7), 959–997. doi: 10.1016/j.cpr.2003.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattiko MJ, Olmsted KL, Brown JM, & Bray RM (2011). Alcohol use and negative consequences among active duty military personnel. Addictive Behaviors, 36(6), 608–614. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Miller WR, Smith JE, & Tonigan JS (2002). A randomized trial of two methods for engaging treatment-refusing drug users through concerned significant others. Journal of Consulting and Clinical Psychology, 70(5), 1182–1185. doi: 10.1037//0022-006x.70.5.1182 [DOI] [PubMed] [Google Scholar]
- Miller WR, Meyers RJ, & Tonigan JS (1999). Engaging the unmotivated in treatment for alcohol problems: A comparison of three strategies for intervention through family members. Journal of Consulting and Clinical Psychology, 67(5), 688–697. doi:10.1037//0022-006x.67.5.688 [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. (2005). Helping patients who drink too much: A clinician’s guide (NIH Publication No. 05–3769). Retrieved from: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf [Google Scholar]
- Norton R (1983). Measuring marital quality: A critical look at the dependent variable. Journal of Marriage and the Family, 45(1), 141–151. [Google Scholar]
- Osilla KC, Pedersen ER, Gore K, Trail T, & Howard SS (2014). Study design to develop and pilot-test a web intervention for partners of military service members with alcohol misuse. Addiction Science & Clinical Practice, 9(1), 18. doi: 10.1186/1940-0640-9-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osilla KC, Pedersen ER, Tolpadi A, Howard SS, Phillips JL, & Gore KL (2016). The feasibility of a web intervention for military and veteran spouses concerned about their partner’s alcohol misuse. The Journal of Behavioral Health Services & Research, 45(1), 57–73. doi: 10.1007/s11414-016-9546-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osilla KC, Trail TE, Pedersen ER, Gore KL, Tolpadi A, & Rodriguez LM (2017). Efficacy of a Web-based Intervention for Concerned Spouses of Service Members and Veterans with Alcohol Misuse. Journal of Marital and Family Therapy, doi: 10.1111/jmft.12279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette P, Vogt D, Wade M, Tirone V, Greenbaum MA, Kimerling R, … Rosen CS (2011). Perceived barriers to care among veterans health administration patients with posttraumatic stress disorder. Psychological Services, 8(3), 212. [Google Scholar]
- Overall NC, & Fletcher GJO (2010). Perceiving regulation from intimate partners: Reflected appraisal and self-regulation processes in close relationships. Personal Relationships, 17(3), 433–456. doi: 10.1111/j.1475-6811.2010.01286.x [DOI] [Google Scholar]
- Pedersen ER, Osilla KC, Helmuth ED, Tolpadi A, & Gore K (2017). Reaching concerned partners of heavy drinking service members and veterans through Facebook. Military Behavioral Health, 5(3), 265–273. doi: 10.1080/21635781.2017.1316804 [DOI] [Google Scholar]
- Ramchand R, Miles J, Schell T, Jaycox L, Marshall GN, & Tanielian T (2011). Prevalence and correlates of drinking behaviors among previously deployed military and matched civilian populations. Military Psychology, 23(1), 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhule-Louie DM, & McMahon RJ (2007). Problem behavior and romantic relationships: Assortative mating, behavior contagion, and desistance. Clinical Child and Family Psychology Review, 10(1), 53–100. doi: 10.1007/s10567-006-0016-y [DOI] [PubMed] [Google Scholar]
- Rodriguez LM, DiBello AM, & Neighbors C (2013). Perceptions of partner drinking problems, regulation strategies and relationship outcomes. Addictive Behaviors, 38(12), 2949–2957. doi: 10.1016/j.addbeh.2013.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez LM, DiBello AM, & Wickham R (2016). Regulation strategies mediate associations between heavy drinking and relationship outcomes in married couples. Addictive Behaviors, 54(Supplement C), 64–69. doi: 10.1016/j.addbeh.2015.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez LM, Osilla KC, Trail TE, Gore K, & Pedersen E (2017). Alcohol use among concerned partners of heavy drinking service members and veterans. Journal of Marital and Family Therapy. doi: 10.1111/jmft.12261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roozen HG, de Waart R, & van der Kroft P (2010). Community reinforcement and family training: an effective option to engage treatment-resistant substance-abusing individuals in treatment. Addiction, 105(10), 1729–1738. doi: 10.1111/j.1360-0443.2010.03016.x [DOI] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, & Ren L (2011). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence, 116(1), 93–101. doi: 10.1016/j.drugalcdep.2010.11.027 [DOI] [PubMed] [Google Scholar]
- Smith JE, & Meyers RJ (2007). Motivating Substance Abusers to Enter Treatment: Working with Family Members. New York: The Guilford Press. [Google Scholar]
- Sobell MB, & Sobell LC (1993). Problem drinkers. New York: Guilford Press. [Google Scholar]
- Spielberger CD (1999). State-Trait Anger Expression Inventory-2 (STAXI-2). Odessa, FL: PAR/Psychological Assessment Resources. [Google Scholar]
- Stahre MA, Brewer RD, Fonseca VP, & Naimi TS (2009). Binge Drinking Among U.S. Active-Duty Military Personnel. American Journal of Preventive Medicine, 36(3), 208–217. doi: 10.1016/j.amepre.2008.10.017 [DOI] [PubMed] [Google Scholar]
- Steinglass P, & Robertson A (1983). The alcoholic family In Kissen B & Begleiter H (Eds.), The pathogenesis of alcoholism (pp. 243–307). New York: Plenum. [Google Scholar]
- Vogt D (2011). Mental health-related beliefs as a barrier to service use for military personnel and veterans: a review. Psychiatric Services, 62(2), 135–142. [DOI] [PubMed] [Google Scholar]