Primary malignant melanoma is extremely rare. Most of the cases are from Western countries and Japan. Here we report the first case of primary malignant melanoma of the esophagus from Saudi Arabia.
Case Report
In September 1992 a 47-year-old Saudi male from Hail was referred from Jeddah to the Gastroenterology Department, Riyadh Armed Forces Hospital (RAFH). He presented with a five month history of abdominal discomfort mainly in the epigastrium, progressive dysphagia, weight loss (about 10 kg) and recent history of melena.
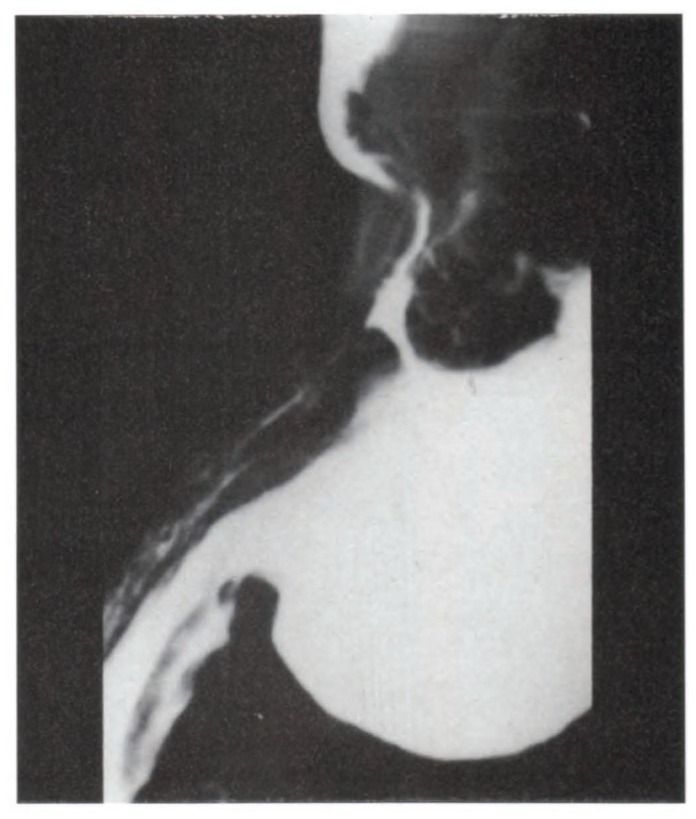
Physical examination was unremarkable except for mild tenderness in the epigastrium. Hematological and biochemical results were within normal limits. Barium swallow revealed a large polypoid lesion at the most distal part of the esophagus, cardia and probably fundus of the stomach (Figure 1).
FIGURE 1.
Barium showing large polypoid lesion at most distal part of esophagus, cardia and fundus of stomach.
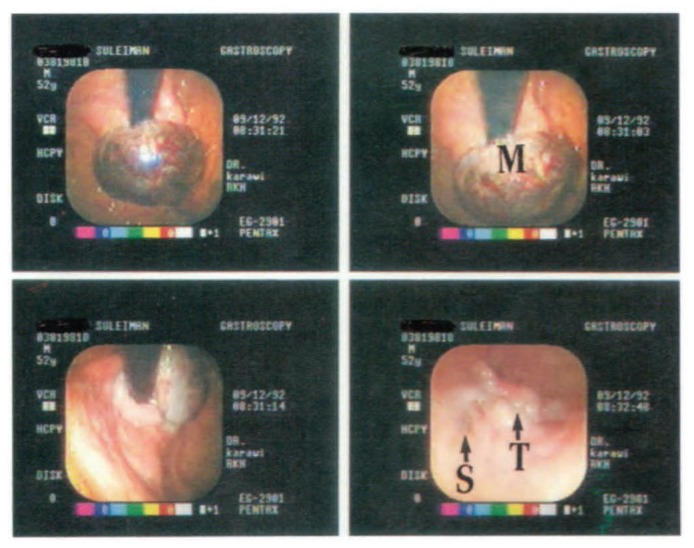
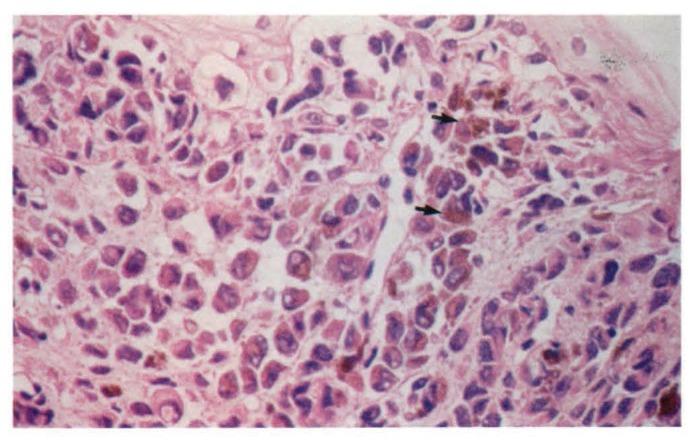
Gastroscopic examination showed a small submucosal spot at 30 cm, multiple dark spots at 35 cm, stricture of cardia, a mass hanging from the cardia in the fundus, dark in color, which bled easily (Figure 2). Multiple biopsies were taken. Histologically malignant melanoma was proven from all biopsies; even the small spots at mid esophagus showed the presence of melanoma (Figure 3).
FIGURE 2.
Gastroscopic view. M-mass hanging from cardia dark in color. S-multiple dark spots. T-tumor.
FIGURE 3.
Histologically melanin granules under high power (arrows). Hematoxylin and eosin stain 200x.
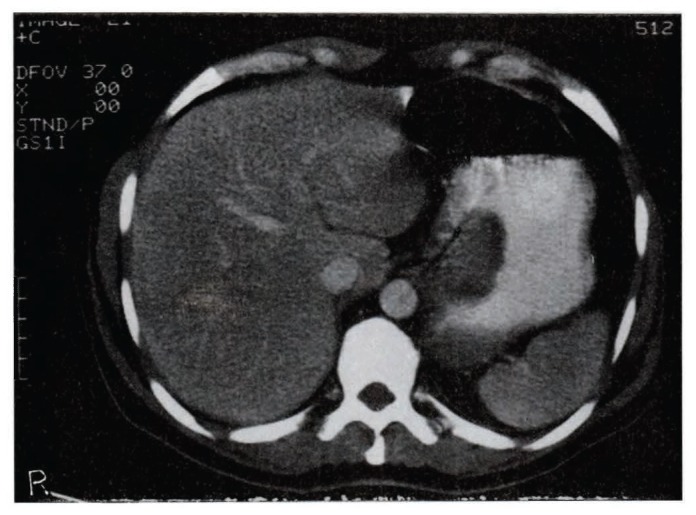
Computed tomography (CT) of the chest and abdomen revealed no evidence of mediastinal, hilar or para-aortic lymphadenopathy. Spleen, kidneys and liver were normal (Figure 4).
FIGURE 4.
Computed tomography - no evidence of lymphadenopathy.
Biopsy from a mole on the left cheek showed intradermal nevus. No other lesions were found and diagnosis of primary malignant melanoma of the esophagus was established.
In view of the extent of the lesion, we recommended total esophagectomy and management in a center with special interest and expertise in esophageal surgery. Subsequently, the patient had a total esophagectomy in Germany, with final diagnosis of primary malignant melanoma of the esophagus. Six months following surgery, we were informed that the patient died in Germany due to extensive metastases to the lungs and abdomen as a natural course of primary malignant melanoma of the esophagus, as it is a highly malignant tumor and the prognosis is very poor.
Discussion
Baur1 described primary malignant melanoma of the esophagus in 1906. However, in 1952, Garfinkle and Cahan2 reported the first case, although its existence was doubted since melanocytes had not been identified within the esophageal wall. When De La Pava et al.3 showed typical melanoblasts in four out of 100 esophagi from necropsy materials, the diagnosis was accepted in 1992.
It is a rare tumor4 accounting for only 0.1% to 0.2% of all esophageal tumors.5,6 Out of 2100 cases of esophageal carcinoma treated at Memorial Hospital, Pawtucket, Rhode Island, USA from 1920 to 1979, five were melanomas (0.2%).5,7 Turnbull et al. reviewed 1918 cases of esophageal tumors between 1926 and 1968 and found only two cases of malignant melanoma.5 To date, 139 cases have been published worldwide.6,8 This is a rare tumor with very little known about it. Male to female ratio is 2:19 and it generally occurs from the fifth decade onward, although one case has been reported in a seven-year-old child.13 In our department, this is the only case diagnosed out of more than 200 cases of esophageal carcinoma.
The origin of such a tumor remains largely speculative. Four percent of the normal population showed melanocytes in the epidermal basal layer of the esophagus3 so it has been suggested that the tumor arises within ectopic melanocyte precursors that migrate down the upper two-thirds of the esophagus during development. In 25% of affected cases, melanosis of the esophagus is present.10,11 It could be a predisposing factor.
Common presenting symptoms are dysphagia, loss of weight, loss of appetite, and abdominal discomfort, mainly retrosternal, although one asymptomatic patient has been reported.12 Average duration of symptoms is three to five months. The most common location of the tumor is middle and lower third of the esophagus.14 Piccone et al. reported the first case involving the entire esophagus.15 However, partial involvement of the esophagus with melanosis is common.17,18
Macroscopically, the typical lesion is a lobulated, firm, black, rounded polypoid tumor mass.4 On touch, it is friable and bleeds easily.16 Smaller “daughter” metastases are common in the mucosa around the main tumor. The tumor in our patient had this typical presentation. Tumor extent is often underestimated on gross examination, as growth and spread occur mainly within the submucosa and, despite the size of a large tumor, they can be covered with intact squamous mucosa. Microscopic criteria established by Raven and Dawson16 in 1964, based on the proposal of Allen and Spitz,17 suggests that the tumor should have the structure of melanoma containing melanin granules and should arise from an area of junctional change. However, this criteria is met in only 40% of cases reviewed by Kreuser,18 although he suggested that rapid tumor growth may obliterate junctional change.20,21
Some pathologists still consider all melanomas of the esophagus as metastatic but several facts support the finding that malignant melanoma can arise primarily in the esophagus. This is confirmed as Burnett and St. John19 reviewed 22,000 autopsies at Johns Hopkins, Baltimore, MD, USA and found 25 malignant melanomas at various sites, but they did not find a single metastasis or a primary in the esophagus. Mofatt et al.14 found that the literature contained only two cases of melanoma metastasizing to the esophagus and De La Pava et al.3 demonstrated the presence of melanoblasts and granules in 4% of the population, establishing the presence of cells from which a primary tumor might develop.
When the diagnosis is known or suspected, a thorough physical examination should include other possible primary sites with special attention to nail beds, soles of feet, scrotum and nasal sinuses. Evidence of meningeal involvement should be sought; rectal, respiratory and funduscopic examinations are essential. Barium swallow will show a large polypoid, lobulated, ulcerating mass. Gastroscopy should be done to see the lesion and to take biopsies, as diagnosis is made histologically. CT should be done to recognize the lesion’s size, shape, local spread and lymph node involvement.
Treatment
The treatment is mainly: Surgery - if the lesion appears operable, Raven and Dawson16 recommended partial esophagogastrectomy with esophagogastrostomy. The majority of resected lesions in literature seem to have been treated in this fashion. Radiotherapy - melanoma is considered to be radio resistant.22 However, some authors still advocate postoperative radiotherapy.7,9 Chemotherapy - adjuvant irradiation and chemotherapy have been used but have not improved survival.23 Prognosis - the prognosis is very poor, as it is a highly malignant tumor. Average survival is seven to 12 months. Five year survival is 4.2%.24 A case of primary malignant melanoma of the esophagus in a 40-year-old female who survived 12 years after surgery has been reported from Northern General Hospital, Sheffield, U.K. Our report is the first case to our knowledge of primary melanoma of the esophagus reported from Saudi Arabia. Metastases were not detected; thus, the hope was for a long survival but the patient subsequently died within six months, as average survival is seven to 12 months.
References
- 1.Baur EH. Ein Fall Von Primarem melanom des oesphagus. Arb Geb Path Anat Inst Tubingen. 1906;5:343–54. [Google Scholar]
- 2.Garfinkle JM, Cahan WC. Primary melanocarcinoma of the esophagus: first histologically proved case. Cancer. 1952;5:921. doi: 10.1002/1097-0142(195209)5:5<921::aid-cncr2820050508>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 3.De La Pava S, Nigogosyan G, Pickren JW, Cabrera A. Melanosis of the esophagus. Cancer. 1963;16:48–50. doi: 10.1002/1097-0142(196301)16:1<48::aid-cncr2820160107>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 4.Boyd DP, Meissner WA, Velkoff CL, Gladding TC. Primary melanocarcinoma of the esophagus: report of a case. Cancer. 1954;7:266. doi: 10.1002/1097-0142(195403)7:2<266::aid-cncr2820070209>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 5.Turnbull AD, Rosen PP, Goodner T, Beattie EJ. Primary malignant tumors of the esophagus other than typical epidermoid carcinoma. Ann Thorac Surg. 1973;15:463–73. doi: 10.1016/s0003-4975(10)65333-7. [DOI] [PubMed] [Google Scholar]
- 6.Chalkiadakis G, Wihlm JN, Morand G. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1985;39:472. doi: 10.1016/s0003-4975(10)61963-7. [DOI] [PubMed] [Google Scholar]
- 7.McCormack PM, Nascimento AG, Baino MS, et al. Primary melanocarcinoma of the esophagus. Clin Bull. 1979;9:162–4. [PubMed] [Google Scholar]
- 8.Baulafendis D, Damiani M, Sie E, et al. Primary malignant melanoma of the esophagus in a young adult. Am J Gastroenterol. 1985;80:417–20. [PubMed] [Google Scholar]
- 9.Rosech W, Roher HG. Primary malignant melanoma of the esophagus. Endosc. 1984;16:186–8. doi: 10.1055/s-2007-1018578. [DOI] [PubMed] [Google Scholar]
- 10.DiCastanzo DP, Urmacher C. Primary malignant melanoma of the esophagus. Am J Sur Pathol. 1987;11:46–52. doi: 10.1097/00000478-198701000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Ludwig ME, Shaw R, de Suto-Nagy G.Primary malignant melanoma of the esophagus. Cancer 1981482528–34. [DOI] [PubMed] [Google Scholar]
- 12.Assor D, Santa Cruz D. Multifocal malignant melanoma of the esophagus. S Med J. 1980;72:1009–12. doi: 10.1097/00007611-197908000-00034. [DOI] [PubMed] [Google Scholar]
- 13.Basque GJ, Boline JE, Holyoke JB. Malignant melanoma of the esophagus: first reported case in a child. Am J Clin Pathol. 1970;53:609. doi: 10.1093/ajcp/53.5.609. [DOI] [PubMed] [Google Scholar]
- 14.Moffat RC, Richard LB, Gnass JE. Primary malignant melanoma of the esophagus: a case report. Can J Surg. 1972;15:306. [PubMed] [Google Scholar]
- 15.Piccone VA, Klopstock R, LeVeen HH, Sika J. Primary malignant melanoma of the esophagus associated with melanosis of entire esophagus: first case report. J Thorac Cardiovasc Surg. 1970;59:864–70. [PubMed] [Google Scholar]
- 16.Raven RW, Dawson A. Malignant melanoma of the esophagus. Br J Surg. 1964;51:551. doi: 10.1002/bjs.1800510723. [DOI] [PubMed] [Google Scholar]
- 17.Allen AC, Spitz S. Malignant melanoma: a clinicopathological analysis of the criteria for diagnosis and prognosis. Cancer. 1953;6:1–45. doi: 10.1002/1097-0142(195301)6:1<1::aid-cncr2820060102>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 18.Kreuser ED. Primary malignant melanoma of the esophagus. Virchows Arch (Pathol Anat) 1979;385:49–52. doi: 10.1007/BF00433540. [DOI] [PubMed] [Google Scholar]
- 19.Burnett JM, St John E. Primary malignant melanocarcinoma of the esophagus. Radiol. 1951;57:868. doi: 10.1148/57.6.868. [DOI] [PubMed] [Google Scholar]
- 20.Loring WE, Zeppa R. Melanocarcinoma of the esophagus. J Thorac Surg. 1956;32:35–45. [PubMed] [Google Scholar]
- 21.Robertson JW. Malignant melanoma of the esophagus as one of the multiple malignant tumors. Gastroenterol. 1954;27:121–6. [PubMed] [Google Scholar]
- 22.Ackerman LV. Surgical Pathology. St Louis: C.V. Mosby; 1953. [Google Scholar]
- 23.Jawalker K, Tretter P. Primary malignant melanoma of the esophagus: report of two cases. J Surg Oncol. 1979;12:19–25. doi: 10.1002/jso.2930120104. [DOI] [PubMed] [Google Scholar]
- 24.Simpson NS, Spence RA, Biggart JD. Primary malignant melanoma of the esophagus. J Clin Path. 1990;43:82–4. doi: 10.1136/jcp.43.1.82-b. [DOI] [PMC free article] [PubMed] [Google Scholar]