Abstract
Background
Septic shock therapies that shorten the time to physiologic and clinical recovery may result in financial savings. However, the financial implications of improving these nonmortal outcomes are not well characterized. Therefore, we quantified hospital charges associated with four outcomes: ICU length of stay, duration of invasive mechanical ventilation, duration of vasopressor use, and new renal replacement therapy.
Methods
This was an observational study using administrative data from a large academic hospital in the United States. The analysis included adults treated with vasopressors for septic shock in a medical ICU. Linear regression modeling with ordinary least square was used to estimate the incremental hospital charges associated with 1 day of ICU length of stay, 1 day of mechanical ventilation, 1 day of vasopressor use, and new renal replacement therapy.
Results
The study population included 587 adults with septic shock, including 180 (30.7%) who died in the hospital. The median charge for a septic shock hospitalization was $98,583 (interquartile range [IQR], $61,177-$136,672). Decreases in ICU length of stay, mechanical ventilation duration, and vasopressor duration of 1 day were associated with charge reductions of $15,670 (IQR, $15,023-$16,317), $15,284 (IQR, $13,566-$17,002), and $17,947 (IQR, $16,344-$19,549), respectively. Avoidance of new renal replacement therapy was associated with a charge reduction of $36,051 (IQR, $22,353-$49,750).
Conclusions
Septic shock therapies that reduce the duration of organ support and ICU care have the potential to lead to substantial financial savings.
Key Words: cost, outcomes, resource utilization, sepsis, shock
Abbreviation: IQR, interquartile range
Clinical trials investigating new pharmaceutical agents and treatment algorithms in patients with septic shock have historically used mortality as the primary outcome.1, 2, 3, 4, 5, 6 However, the critical care community is increasingly exploring nonmortal outcomes in clinical studies.7, 8, 9, 10, 11 Outcomes such as quality of life, cognition, length of stay, ventilator-free days, and vasopressor-free days are important to patients, families, the health-care system, and society.7, 8, 9, 10, 11 Therefore, improvements in these nonmortal outcomes could potentially provide justification for approval and use of new treatments. However, experience with nonmortal outcomes in septic shock studies remains limited, and a greater understanding of these outcomes would help guide outcome selection in future trials.
Sepsis is the most costly diagnosis in hospitals in the United States, with expenditures for sepsis reaching > $20 billion in 2011.12 The financial implications of improving nonmortal outcomes, such as shortening the duration of organ support, are largely unknown. Therefore, we analyzed hospital charges for a cohort of patients hospitalized with vasopressor-dependent septic shock and estimated savings associated with shortening ICU length of stay, mechanical ventilation, and vasopressor use and avoiding renal replacement therapy.
Methods
Design and Setting
We conducted a single-center retrospective observational study using data collected for administrative and clinical purposes. The study was performed at a large tertiary care, academic medical center in the United States with a 34-bed medical ICU. The study was approved by the Vanderbilt University institutional review board (protocol No. 160861) with waiver of informed consent.
Study Population
The study population included adults with community-onset vasopressor-dependent septic shock who presented to the ED and were admitted to the medical ICU between January 1, 2011, and October 31, 2015. Inclusion criteria included the following: ≥ 18 years of age; an International Classification of Diseases, Ninth Revision code for septic shock (785.52); administration of a vasopressor by continuous infusion for ≥ 1 h; initial presentation to the ED; and direct admission from the ED to the medical ICU. Patients with nosocomial sepsis and those treated in surgical ICUs were not included. The unit of analysis was each hospitalization, with individual patients potentially contributing multiple hospitalizations.
Study Variables and Data Collection
All data were extracted from the electronic data warehouse at the study institution, which houses clinical and administrative data, including each line item charge incurred during hospitalization. Each item (goods and services) used in the study hospital during the care of a patient is assigned a charge amount (eg, the charge amount for a chest radiograph in 2015 was $272). The charge amount associated with each item varied over time during the study period (eg, the charge for a chest radiograph in 2011 was $231). We standardized charges in this study to the amount charged in 2015; hence, charges for all patients were described in 2015 equivalent dollars. For example, a chest radiograph was assigned the same dollar amount ($272) for this analysis regardless of whether it was completed in 2011 or 2015.
Hospital admissions were divided into calendar day intervals (midnight to midnight). Each charge was classified into one of the following categories: room occupancy and professional fees, pharmacy, laboratory, radiology, procedures, anesthesia, ED, therapy, supplies, and devices. Hospital charges incurred during each day and for the entire hospitalization were calculated by summing line item charges.
An ICU day was defined as a hospital day with a charge for occupancy of an ICU bed. A ventilator day was defined as a day in which the patient received invasive mechanical ventilation through an endotracheal tube or tracheostomy. Invasive mechanical ventilation did not include noninvasive ventilation or continuation of chronic mechanical ventilation that was present before the onset of sepsis. A vasopressor day was defined as a day in which the patient received a vasopressor by continuous infusion for ≥ 1 h. Eligible vasopressors included norepinephrine, epinephrine, dopamine, phenylephrine, and vasopressin. New renal replacement therapy was defined as initiation of hemodialysis or continuous renal replacement therapy after hospital admission. Patients with end-stage renal disease on chronic renal replacement therapy prior to their sepsis were not eligible for new renal replacement therapy.
Analysis
Initially, total hospital charges for an entire hospitalization were compiled and summarized. Both patients who died in the hospital and those who survived to discharge contributed to total hospital charges. To demonstrate differences in hospital charges between those who died and survived, calculations were also stratified by in-hospital death status (died vs survived).
Then, daily charges were evaluated. These daily charges were divided into charges that occurred on calendar days in which the patient was managed in the ICU and days managed on a hospital floor. This provided a summary for the typical charges for an ICU day and hospital floor day. Daily charges for an ICU stay were also divided into charges based on the number of days a patient had been in the ICU. This calculation provided a summary for charges on the first day of ICU care and each subsequent day. Patients contributed to daily ICU charges only for the days they were treated in the ICU. For example, a patient who remained in the ICU for 1 day contributed to daily ICU charges for ICU day 1 only; meanwhile, a patient who remained in the ICU for 3 days contributed to daily charges for ICU days 1, 2, and 3. For patients with multiple ICU stays during one hospitalization, only the first ICU stay was used for analysis of daily charges.
To guide our statistical approach for calculating charge reductions associated with shortening ICU length of stay, trajectory plots of daily ICU charges (ie, scatterplots with daily charges on the y axis and days since admission on the x axis), with loess curves by quartile groups of ICU length of stay, were created. Different trajectory patterns across quartile groups of ICU length of stay would indicate that changes in daily charges over time vary by ICU length of stay, and charge reductions associated with shortening ICU length of stay should be calculated by modeling daily ICU charges (to account for the charge associated with a 1-day reduction in the ICU varying, dependent on the ultimate duration of ICU stay). As visualized on the trajectory plot (e-Fig 1), daily ICU charges decreased over time, and the decline rate did indeed vary by duration of ICU length of stay (ie, the longer the ICU length of stay, the slower the decline rate). Hence, we estimated charge reductions associated with a 1-day reduction in ICU length of stay by modeling daily charges against days since admission, total ICU length of stay, and their interactions using a generalized least squares linear regression model with first-order autoregressive correlated errors to account for correlation between ICU days within the same ICU stay. The interaction term was included to account for a slower decline rate with increased ICU length of stay.
For a given ICU length of stay, the charge reduction associated with shortening ICU length of stay by 1 day was calculated with the following four steps. First, daily charges on ICU day 1 were estimated. Second, the decline rate corresponding to the specific ICU length of stay (interaction term in the model) was used to calculate each subsequent daily charge and the corresponding total ICU charges. Third, the total ICU charges were estimated again using the same approach but with a decline rate corresponding to an ICU length of stay of 1 day shorter. Fourth, the charge reduction associated with shortening ICU length of stay by 1 day was estimated by taking the difference between the total ICU charges calculated in steps 2 and 3 (e-Appendix 1).
Trajectory plots were also created for duration of mechanical ventilation and vasopressor use (e-Fig 2). The decline rate of daily charges did not appear to vary by duration of mechanical ventilation or vasopressor use. Therefore, charge reductions associated with 1-day reduction in mechanical ventilation and vasopressor use were estimated by modeling total hospital charges (not daily charges) against mechanical ventilation or vasopressor use while adjusting for the following: duration of hospital floor length of stay, and duration of ICU stay while not on mechanical ventilation (for the mechanical ventilation model) or duration of ICU stay while not using vasopressors (for the vasopressor model). Linear regression modeling with ordinary least square estimates was used for total hospital charge models where charge reductions associated with 1-day reductions in mechanical ventilation or vasopressor use were obtained as the corresponding parameter estimates.
Charge reductions associated with avoidance of renal replacement therapy were estimated by modeling total hospital charges against renal replacement therapy, while adjusting for duration of ICU stay and floor stay using a linear regression model with ordinary least square estimates.
Analyses were conducted with R version 3.2.0 (R Foundation for Statistical Computing) and STATA version 14 (StataCorp).
Results
The study population included 587 hospitalizations for community-onset, vasopressor-dependent septic shock; 568 unique patients accounted for these 587 hospitalizations. The mean age was 60 years; 180 patients (30.7%) died during the hospitalization (Table 1). Patients stayed in the hospital a mean of 9.8 days, with 6.3 days in the ICU and the remaining 3.5 days on a medical floor (e-Fig 3). The median ICU length of stay was 4 days (interquartile range [IQR], 2-8 days).
Table 1.
Patient Characteristics by In-Hospital Death Status
| Characteristic | Full Study Population (N = 587) | Survived to Hospital Discharge (n = 407) | In-Hospital Death (n = 180) |
|---|---|---|---|
| Age, y | 60 ± 15 | 58 ± 15 | 63 ± 15 |
| Female | 285 (48.6) | 198 (48.7) | 87 (48.3) |
| Race | |||
| White | 477 (81.3) | 332 (81.6) | 145 (80.6) |
| Black | 98 (16.7) | 66 (16.2) | 32 (17.8) |
| Asian | 7 (1.2) | 5 (1.2) | 2 (1.1) |
| Other | 5 (0.9) | 4 (1.0) | 1 (0.6) |
| Year of hospitalization | |||
| 2011 | 105 (17.9) | 73 (17.9) | 32 (17.8) |
| 2012 | 103 (17.6) | 73 (17.9) | 30 (16.7) |
| 2013 | 134 (22.8) | 102 (25.1) | 32 (17.8) |
| 2014 | 151 (25.7) | 98 (24.1) | 53 (29.4) |
| 2015 (10 mo) | 94 (16.0) | 61 (15.0) | 33 (18.3) |
| Length of stay, d | |||
| ICU length of stay | 6.3 ± 6.7 | 6.8 ± 6.6 | 5.3 ± 6.8 |
| Hospital floor length of stay | 3.5 ± 5.8 | 4.4 ± 6.3 | 1.2 ± 3.5 |
| Total length of stay | 9.8 ± 9.4 | 11.2 ± 9.6 | 6.4 ± 8.2 |
| Organ support | |||
| Invasive mechanical ventilation | 252 (42.9) | 127 (31.2) | 125 (69.4) |
| New renal replacement therapy | 49 (8.4) | 27 (6.6) | 22 (12.2) |
| Disposition from hospital | |||
| Home | 244 (41.6) | … | … |
| Long-term care facility | 125 (21.3) | … | … |
| Hospice | 30 (5.1) | … | … |
| Acute care hospital | 8 (1.4) | … | … |
| Death | 180 (30.7) | … | … |
| Total hospital charges | $137,556 ± $127,788 | $145,006 ± $129,200 | $120,711 ± $123,234 |
| Median total hospital charges (interquartile range) | $98,583 ($61,177-$136,672) | $103,077 ($69,321-$170,971) | $84,680 ($47,986-$150,990) |
Values are mean ± SD, No. (%), or as otherwise indicated.
Total Hospital Charges and Daily Charges
The median total hospital charge for a septic shock hospitalization was $98,583 (IQR, $61,177-$136,672) (e-Fig 4). Because of longer lengths of stay for patients who survived to discharge, total charges were higher for hospitalizations ending in discharge (median, $103,077) than death (median, $84,680); P < .01). Room occupancy and professional charges (32.9%) accounted for the largest portion of charges, followed by pharmacy, laboratory, and procedure charges (Table 2).
Table 2.
Distribution of Hospital Charges for 587 Hospitalizations for Vasopressor-Dependent Septic Shock
| Charge Category | Charges | % of Total Charges |
|---|---|---|
| Room occupancy and professional charges | $26,542,750 | 32.9 |
| Pharmacy | $16,743,609 | 20.7 |
| Laboratory | $13,080,382 | 16.2 |
| Procedure/surgery | $10,166,187 | 12.6 |
| Radiology | $7,836,692 | 9.7 |
| Anesthesia | $3,280,104 | 4.1 |
| ED | $1,851,725 | 2.3 |
| Other | $1,243,951 | 1.5 |
| Total | $80,745,399 | 100 |
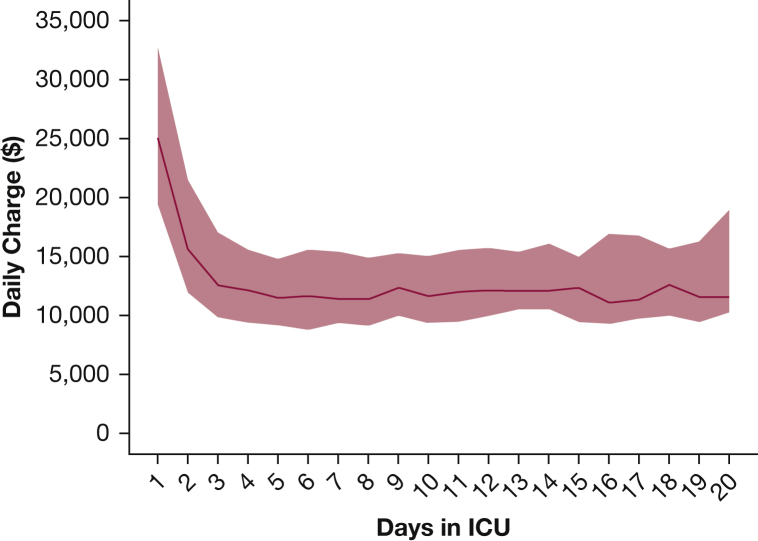
The median daily charge for an ICU day was $13,922 (IQR, $10,271-$20,139). Daily ICU charges were highest on the first ICU day (median, $25,074) and then decreased over the next several days for patients remaining in the ICU, before stabilizing around ICU day 4 at a median of approximately $11,000 (e-Table 1, Fig 1). The median daily charge for a hospital floor day was $5,484 (IQR, $4,285-$7,448) (e-Fig 5).
Figure 1.
Daily charges in the ICU by ICU day. The center curve represents the median daily charge by ICU day number. The red band represents the interquartile range. Data for this figure are reported in e-Table 1.
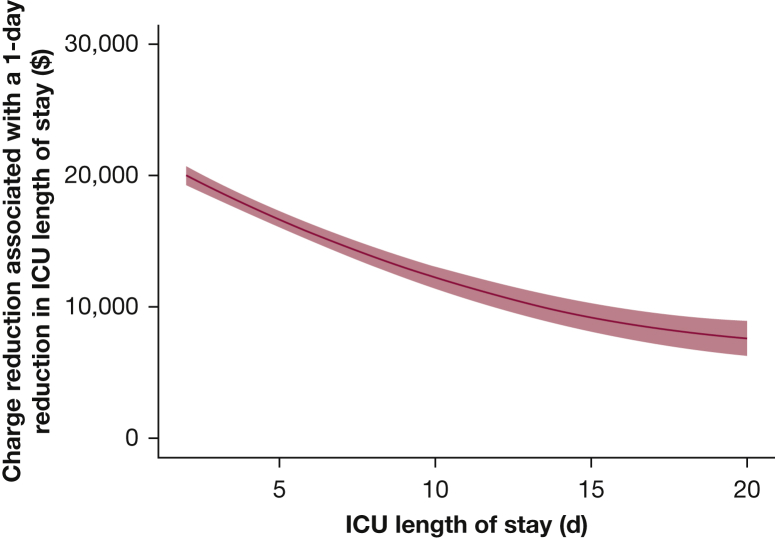
Charge Reductions Associated With Shorter ICU Length of Stay
Total hospital charges were strongly correlated with ICU length of stay (Spearman correlation coefficient = 0.87) (e-Fig 6). Because daily charges in the ICU varied by how long a patient had been in the ICU, the charge reduction associated with a 1-day shortening of ICU length of stay was dependent on ICU length of stay (e-Table 2, Fig 2). For example, shortening ICU length of stay from 3 days to 2 days was associated with a charge reduction of $18,842 (95% CI, $18,174-$19,509), whereas shortening from 10 days to 9 days was associated with a charge reduction of $12,233 (95% CI, $11,396-$13,070). The median ICU length of stay was 4 days. A 1-day reduction in ICU length of stay from 5 days to this median of 4 days was associated with a reduction in total hospital charges of $16,671 (95% CI, $16,042-$17,300) (Table 3).
Figure 2.
Reduction in total hospital charges associated with a 1-day reduction in ICU length of stay by ICU length of stay. The center curve represents the point estimate, and the shaded band represents the 95% CI. Data for this figure are reported in e-Table 2.
Table 3.
Reductions in Total Hospital Charges Associated With Shorter Times to Recovery in Vasopressor-Dependent Septic Shock
| Type of Shortened Recovery | Reduction in Total Hospital Charges (95% CI) |
|---|---|
| Reduction in ICU length of stay by 1 da | $16,671 ($16,042-$17,300) |
| Reduction in duration of invasive mechanical ventilation by 1 d | $15,284 ($13,566-$17,002) |
| Reduction in duration of vasopressor use by 1 d | $17,947 ($16,344-$19,549) |
| Avoidance of new renal replacement therapy | $36,051 ($22,353-$49,750) |
Assumes a 5-d ICU length of stay with reduction to a 4-d ICU length of stay.
Charge reductions associated with shortening ICU length of stay originated from two sources: reducing the total time spent in hospital and reducing daily charges for days patients were in the hospital, reflecting earlier improvement of sepsis resulting in smaller charges each day (e-Fig 7, e-Table 2).
Charge Reductions Associated With Shorter Mechanical Ventilation and Vasopressor Use and Avoidance of Renal Replacement Therapy
A total of 252 patients (42.9%) received invasive mechanical ventilation, with a median duration of mechanical ventilation of 3 days (IQR, 2-6 days). A 1-day reduction in the duration of invasive mechanical ventilation was associated with a reduction in total hospital charges of $15,284 (95% CI, $13,566-$17,002).
All patients in the study received vasopressors. The median duration of vasopressor use was 2 days (IQR, 1-3 days). A 1-day reduction in the duration of vasopressor use was associated with a reduction in total hospital charges of $17,947 (95% CI, $16,344-$19,549).
New renal replacement therapy was used in 49 patients (8.4%), including 15 (2.6%) with intermittent hemodialysis and 34 (5.8%) with continuous renal replacement therapy. Avoidance of renal replacement therapy was associated with a reduction in total hospital charges of $36,051 (95% CI, $22,353-$49,750).
Discussion
In this study of adults with community-onset septic shock, we demonstrated a high financial burden for septic shock, with a median charge for a septic shock hospitalization of approximately $100,000. Additionally, we quantified large potential savings associated with shortening the duration of ICU length of stay, mechanical ventilation, and vasopressor use, with a 1-day reduction in any of these variables associated with a charge reduction of approximately $15,000 to $20,000. We estimated avoidance of new renal replacement therapy would reduce hospital charges by about $36,000.
Ventilator-free days, vasopressor-free days, and organ failure-free days are increasingly used as outcomes in critical care trials.13, 14, 15 These outcomes have advantages and disadvantages. The advantages include the association of organ failure with mortality, and the ability to power trials with fewer patients than would be needed using mortality as the primary outcome.7, 16 Our data provide further rationale for the use of these outcomes based on potential financial savings. The disadvantages of these outcomes include their composite make-up, equating prolonged organ support with death, and the subjective nature of decisions about when to transition patients off organ support.7
From a clinical perspective, these results suggest that improvement in nonmortal outcomes can be an important goal in the management of patients who are critically ill with septic shock. Reducing the duration of organ support and ICU care appear to conserve substantial resources that could be invested toward the care of additional patients.
We reported hospital charge data in this study. Charges are the dollar amounts hospitals invoice to payers (eg, insurance companies, patients); charges are list prices provided by hospitals. Costs are the expenses incurred to deliver health-care goods and services; costs reflect true resource consumption. Although charges are typically higher than costs, costs are challenging to ascertain for many health-care activities because of the complexities of allocating specific dollar amounts for labor and facilities. In some studies, cost-to-charge ratios are applied to adjust charge data to generate estimated costs.17 However, cost-to-charge ratios have several limitations. First, cost-to-charge ratios are usually calculated based on facility charges without considering professional charges, and may significantly underestimate professional costs when applied to professional charges.18 Second, cost-to-charge ratios are typically calculated by dividing the amount reimbursed to hospitals by the amount charged by a hospital; however, reimbursement does not necessarily reflect true costs.19 Finally, there is wide variation in cost-to-charge ratios across facilities.20 Therefore, reporting charge data may be the most transparent method of presenting information on the financial impact of changes in health-care delivery.21 With raw charge data reported in this study, readers can apply facility-specific cost-to-charge ratios, or use an average cost-to-charge ratio reported by the Centers for Medicare and Medicaid Services22 (approximately 0.34), as desired to estimate costs based on various cost-to-charge ratio assumptions.
Our results are consistent with and add to the prior literature on the cost of septic shock hospitalizations.23, 24, 25 Using administrative data from severe sepsis and septic shock hospitalizations in five US states in 1995, Angus et al23 reported a median hospital cost of $27,600 for patients managed in the ICU of teaching hospitals. This adjusts to $45,266 in 2015 equivalent dollars using the Personal Consumption Expenditures health-care price index.26, 27 Lagu et al24 reported a mean hospitalization cost of $34,142 for US adults with severe sepsis in 2007 (adjusted to $39,946 in 2015 equivalent dollars). Jones et al25 reported a mean cost for severe sepsis and septic shock hospitalizations of $20,289 at a single US hospital in 2006 (adjusted to $24,509 in 2015 equivalent dollars). These prior studies reported costs for the combined group of severe sepsis and septic shock, whereas we focused only on septic shock. After considering the inclusion of patients who were less severely ill in the prior studies, reporting of cost estimates instead of charges, and inflation since the prior studies, our estimate for median charges for a septic shock hospitalization ($98,583) appears consistent with these prior studies. Prior work did not estimate cost savings associated with shortening ICU care, mechanical ventilation, or vasopressor use.
The strengths of our study include the detailed charge data for each ICU day and charges associated with specific therapies, such as mechanical ventilation and vasopressor use. The granularity of these data, which was largely absent from prior studies,23, 24, 25 enabled us to estimate expected savings associated with more rapid improvement in septic shock, which is important for understanding the financial implications of improving clinical outcomes, such as ventilator-free days and vasopressor-free days.
The limitations of our study include a single-center setting and retrospective design. The reported charges reflect pricing from one academic hospital in the United States. Although trends in the charge data are expected to be generalizable, specific dollar amounts may vary among hospitals. As previously noted, we reported charges in this study, not costs. A prospective, multicenter study that collects information on resource utilization (costs) in real time (eg, measuring the time a nurse spends with each patient) would add to these findings by directly measuring resource utilization rather than relying on hospital charge data. Additionally, patients with septic shock were retrospectively identified by International Classification of Diseases, Ninth Revision code, potentially leading to some misclassification. Alternative statistical approaches that considered dynamic decision-making, such as decision trees or influence diagrams, could have been used. Our study population only included adults with vasopressor-dependent community-acquired septic shock; hence, we are unable to comment on sepsis without shock, nosocomial sepsis, and sepsis in children. Evaluating which patient characteristics are associated with more rapid clinical recovery and lower hospital charges are important topics for future investigation.
In conclusion, the median charge for septic shock hospitalizations in 2015 equivalent dollars was approximately $100,000. Shortening the duration of ICU care, mechanical ventilation, and vasopressor use and avoiding new renal replacement therapy all appear to be associated with a substantial reduction in charges. New septic shock therapies that shorten the time of ICU care and organ support have the potential to lead to substantial savings.
Acknowledgments
Author contributions: W. H. S. takes responsibility for the paper as a whole. W. H. S., D. L., and M. W. S contributed to study concept and design. W. H. S., D. L., N. S., and S. R. contributed to acquisition of data. W. H. S., D. L., and N. S. contributed to statistical analysis. W. H. S., S. R., M. J. W., N. I. S., T. W. R., and M. W. S. contributed to interpretation of data. W. H. S. drafted the initial manuscript. D. L., N. S., S. R., M. J. W., N. I. S., T. W. R., and M. W. S. critically revised the manuscript. W. H. S. obtained funding. W. H. S., S. R., M. J. W., and M. W. S. provided study supervision.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: W. H. S. reported serving on advisory boards for Venaxis Inc, Cempra Pharmaceuticals, Ferring Pharmaceuticals, and BioTest AG; serving as a consultant for Abbott Point of Care; and receiving travel funds from Gilead Pharmaceuticals. T. W. R. reported receipt of personal fees from Cumberland Pharmaceuticals, Inc and Avisa Pharma, LLC; and chairs a DSMB for a study sponsored by Millenial Pharmaceuticals, Inc. None declared (D. L., N. S., S. R., M. J. W., N. I. S., M. W. S.).
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Additional information: The e-Appendix, e-Figures, and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: Funding for this investigator-initiated study was provided by Ferring Pharmaceuticals. W. H. S. was supported in part by a grant from the National Institute of General Medical Sciences [Grant K23GM110469]. M. J. W. was supported in part by a grant from the National Heart, Lung, and Blood Institute [Grant K23HL127130]. T. W. R. was supported in part by a grant from the National Heart, Lung and Blood Institute [Grant R34HL105869]. M.W. S. was supported in part by a grant from the National Heart, Lung and Blood Institute [Grant K12HL133117].
Supplementary Data
References
- 1.De Backer D., Biston P., Devriendt J. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010;362(9):779–789. doi: 10.1056/NEJMoa0907118. [DOI] [PubMed] [Google Scholar]
- 2.Ranieri V.M., Thompson B.T., Barie P.S. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366(22):2055–2064. doi: 10.1056/NEJMoa1202290. [DOI] [PubMed] [Google Scholar]
- 3.Bernard G.R., Vincent J.L., Laterre P.F. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344(10):699–709. doi: 10.1056/NEJM200103083441001. [DOI] [PubMed] [Google Scholar]
- 4.Rivers E., Nguyen B., Havstad S. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Eng J Med. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 5.ProCESS Investigators. Yealy D.M., Kellum J.A. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683–1693. doi: 10.1056/NEJMoa1401602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaukonen K.M., Bailey M., Suzuki S. Mortality related to severe sepsis and septic shock among critically ill patient in Australia and New Zealand, 2000-2011. JAMA. 2014;311(13):1308–1316. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 7.Spragg R.G., Bernard G.R., Checkley W. Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. 2010;181(10):1121–1127. doi: 10.1164/rccm.201001-0024WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schoenfeld D.A., Bernard G.R. Statistical evaluation of ventilator-free days as an efficacy measure in clinical trials of treatments for acute respiratory distress syndrome. Crit Care Med. 2002;30(8):1772–1777. doi: 10.1097/00003246-200208000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Pandharipande P.P., Girard T.D., Jackson J.C. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferguson N.D., Scales D.C., Pinto R. Integrating mortality and morbidity outcomes: using quality-adjusted life years in critical care trials. Am J Respir Crit Care Med. 2013;187(3):256–261. doi: 10.1164/rccm.201206-1057OC. [DOI] [PubMed] [Google Scholar]
- 11.Harhay M.O., Wagner J., Ratcliffe S.J. Outcomes and statistical power in adult critical care randomized trials. Am J Respir Crit Care Med. 2014;189(12):1469–1478. doi: 10.1164/rccm.201401-0056CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pfunter A, Wier LM, Steiner C. Costs for hospital stays in the United States, 2011. HCUP statistical brief #168. www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.jsp. Accessed November 20, 2017.
- 13.Huang D.T., Angus D.C., Moss M. Design and rationale of the reevaluation of systemic early neuromuscular blockade trial for acute respiratory distress syndrome. Ann Am Thorac Soc. 2017;14(1):124–133. doi: 10.1513/AnnalsATS.201608-629OT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kawazoe Y., Miyamoto K., Morimoto T. Effect of dexmedetomidine on mortality and ventilator-free days in patients requiring mechanical ventilation with sepsis: a randomized clinical trial. JAMA. 2017;317(13):1321–1328. doi: 10.1001/jama.2017.2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferring Pharmaceuticals . National Institutes of Health; Bethesda, MD: 2015. Selepressin Evaluation Programme for Sepsis-Induced Shock - Adaptive Clinical Trial (SEPSIS-ACT). NCT02508649. ClinicalTrials.gov.https://clinicaltrials.gov/ct2/show/NCT02508649 Updated. [Google Scholar]
- 16.Seymour C.W., Liu V.X., Iwashyna T.J. Assessment of clinical criteria for sepsis for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315(8):762–774. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dasta J.F., McLaughlin T.P., Mody S.H., Piech C.T. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266–1271. doi: 10.1097/01.ccm.0000164543.14619.00. [DOI] [PubMed] [Google Scholar]
- 18.Rogowski J. Cost-effectiveness of care for very low birth weight infants. Pediatrics. 1998;102(1 Pt 1):35–43. doi: 10.1542/peds.102.1.35. [DOI] [PubMed] [Google Scholar]
- 19.Peterson C., Xu L., Florence C. Professional fee ratio for US hospital discharge data. Med Care. 2015;53(10):840–849. doi: 10.1097/MLR.0000000000000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bai G., Anderson G.F. Extreme markup: the fifty US hospitals with the highest charge-to-cost ratios. Health Aff (Millwood) 2015;34(6):922–928. doi: 10.1377/hlthaff.2014.1414. [DOI] [PubMed] [Google Scholar]
- 21.Chalfin D.B., Holbein M.E., Fein A.M., Carlon G.C. Cost-effectiveness of monoclonal antibodies to gram-negative endotoxin in the treatment of gram-negative sepsis in ICU patients. JAMA. 1993;269(2):249–254. [PubMed] [Google Scholar]
- 22.Centers for Medicare & Medicaid Services. FY2017 Final Rule and Correction Notice Data Files. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2017-IPPS-Final-Rule-Home-Page-Items/FY2017-IPPS-Final-Rule-Data-Files.html. Accessed January 5, 2018.
- 23.Angus D.C., Linde-Zwirble W.T., Lidicker J. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Lagu T., Rothberg M.B., Shief M.S. Hospitalizations, costs, and outcomes of severe sepsis in the United States, 2003 to 2007. Crit Care Med. 2012;40(3):754–761. doi: 10.1097/CCM.0b013e318232db65. [DOI] [PubMed] [Google Scholar]
- 25.Jones A.E., Troyer J.L., Kline J.A. Cost-effectiveness of an emergency department-based early sepsis resuscitation protocol. Crit Care Med. 2011;39(6):1306–1312. doi: 10.1097/CCM.0b013e31821201be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunn A., Grosse S.D., Zuvekas S.H. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res. 2018;53(1):175–196. doi: 10.1111/1475-6773.12612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bureau of Economic Analysis, US Department of Commerce. US Economic Accounts. https://www.bea.gov/index.htm. Accessed July 31, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.