Abstract
Background:
While family interventions have shown efficacy in improving mood symptoms and family functioning in pediatric bipolar disorder, few studies have examined the effects of comorbid psychiatric conditions on patients’ symptomatic or functional responses to treatment.
Methods:
145 adolescents with bipolar I or II disorder were randomly assigned to family-focused therapy (FFT-A) or a brief psychoeducational therapy (enhanced care; EC) and followed over 2 years. Participants received pharmacotherapy for the study’s duration. We examined whether comorbid anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), and disruptive behavior disorders (DBDs; i.e., oppositional defiant and conduct disorder) predicted the proportion of weeks that participants experienced mood symptoms during follow-up, and whether comorbid disorders moderated the effects of treatment assignment on mood symptoms and family conflict.
Results:
Comorbid anxiety was associated with a greater proportion of weeks with depressive symptoms, more severe (hypo)manic symptoms during follow-up, and greater family conflict over the 2-year study. Comorbid ADHD was associated with a greater proportion of weeks with (hypo)manic symptoms, more severe (hypo)manic symptoms, and greater family conflict. Additionally, comorbid ADHD moderated the effects of psychosocial treatments on (hypo)manic symptoms and family functioning. Comorbid DBDs were consistently associated with more severe depressive symptoms and greater family conflict throughout the study.
Limitations:
Randomization to treatments was not stratified on comorbid disorders, and the course of anxiety, attentional, and disruptive behavior symptoms were not examined.
Conclusions:
The course of bipolar disorder in adolescents is strongly affected by comorbid disorders. Future research should examine whether adolescents with more complex presentations of bipolar disorder should be treated with different or more intensive psychosocial protocols than adolescents without these presentations.
Keywords: Family focused therapy (FFT), anxiety, attention-deficit/hyperactivity disorder (ADHD), disruptive behavior disorders (DBD), oppositional defiant disorder (ODD), conduct disorder (CD), pediatric bipolar disorder
1. Introduction
Bipolar spectrum disorders (BSDs) - i.e., bipolar I/II, cyclothymia, and other specified bipolar disorder - are highly recurrent illnesses, especially when onset is in childhood or adolescence (APA, 2013). The lifetime prevalence of bipolar I and II disorder is 2% and increases to 4–5% when including spectrum disorders (Merikangas et al., 2007; Merikangas et al., 2011b). More than 50% of patients experience initial onset of their illness before age 18 (Perlis et al., 2004). In addition, a majority of bipolar youth suffer from one or more comorbid disorders, including anxiety disorders (54%), attention-deficit/hyperactivity disorder (ADHD; 48%), disruptive behavior disorders (DBDs [i.e., oppositional defiant and conduct disorders]; 31%), and substance/alcohol abuse or dependence disorders (31%; Frías et al., 2015).
Comorbid conditions are associated with a wide range of negative outcomes in pediatric BSDs. Youth with BSDs and comorbid anxiety, ADHD, or DBDs have greater psychosocial impairment cross-sectionally and longitudinally compared to bipolar youth without a comorbid diagnosis (e.g., Arnold et al., 2011; DelBello et al., 2007; Joshi et al., 2010; Masi et al., 2012). In youth with BSDs, comorbid disorders are associated with more severe mood symptoms, higher frequencies of mood episodes, and less time well over periods of 1 to 5 years (e.g., Cummings and Fristad, 2012; DelBello et al., 2007; Sala et al., 2014). Some have theorized that the presence of early psychiatric disorders like ADHD may lead to greater family conflict and poorer psychosocial functioning, posing an increased risk for the development and/or worsening of pediatric bipolar disorder (Youngstrom et al., 2010). Comorbid ADHD and anxiety disorders are also associated with poorer response to psychiatric medications in child and adolescents with bipolar I/II disorder (e.g., Consoli et al., 2007; Vitiello et al., 2012). Given that the majority of youth seeking treatment meet criteria for multiple mental health conditions (Merikangas et al., 2011a), a better understanding of the effects of comorbid conditions on the response of bipolar youth to psychosocial treatments is essential.
In recent years, several studies have evaluated manualized interventions for youth with or at risk for BSDs (Fristad et al., 2009; Goldstein et al., 2014; Miklowitz et al., 2008; Miklowitz et al., 2013). In adult samples, family-focused treatment (FFT) in combination with pharmacotherapy has been shown to be efficacious in reducing mood symptoms, hastening time to recovery, and increasing time in remission compared to less intensive treatments such as brief family education with pharmacotherapy (Miklowitz and Chung, 2016). In an adolescent sample conducted in three sites, we reported that (1) FFT and a brief family educational treatment (enhanced care, or EC) did not differ on time to recovery from index study episodes or time until recurrence; (2) patients in FFT-A had greater improvements in manic but not depressive symptoms compared to those in EC in the post-treatment year; and (3) patients with comorbid anxiety disorders and ADHD had earlier mood recurrences, regardless of treatment condition (Miklowitz et al., 2014). A separate report from this study found that FFT-A was associated with greater improvements in self-reported quality of life compared to the EC treatment (O’Donnell et al., 2017). However, these studies did not investigate the role that comorbid disorders may play in moderating the effects of family interventions. More specifically, it is unclear whether family interventions are equally effective in bipolar adolescents with and without ADHD, anxiety disorders, or DBDs, important considerations when trying to identify patients who are most likely to respond to these time-intensive treatment protocols.
In this study, we investigated whether the most common comorbidities in pediatric bipolar disorder (anxiety disorders, ADHD, and DBDs) moderated adolescents’ response to family treatments (patients with active substance abuse disorders were excluded from the study at its outset). The main goals of FFT-A are (a) teaching illness management skills such as identifying environmental stressors and changes in mood symptoms that anticipate mood recurrences; and (b) enhancing family functioning through teaching communication and problem-solving to reduce criticism and conflict in daily interactions; Miklowitz, 2010). We focused our investigation on on these outcomes. First, we examined the effects of comorbid diagnoses, treatment, and their interaction on the overall percentage of time patients experienced depressive and manic symptoms over two years, based on weekly mood ratings. Next, we examined the effects of treatment and comorbidity on the mean severity of mood symptoms and the level of family conflict at each 3- or 6-month follow-up assessment over the 24-month study. We hypothesized that bipolar adolescents with comorbid disorders (i.e., anxiety disorders, ADHD, and DBDs) would have more severe and protracted mood symptoms and more family conflict over time than adolescents without these comorbid disorders. Furthermore, we predicted that treatment condition would moderate these relationships, such that adolescents with comorbid conditions who were in FFT-A would have faster and more sustained benefits in mood symptoms and functioning compared to adolescents with comorbid conditions who received the EC treatment.
2. Methods
2.1. Participants
The study was conducted at three sites – University of Colorado, the University of Pittsburgh School of Medicine, and the Cincinnati Children’s Hospital Medical Center. Participants were adolescents between the ages of 12 and 18 years, 1 month, with (1) a DSM-IVTR diagnosis of bipolar I or II disorder; (2) a hypomanic/manic or mixed episode lasting at least one week or a major depressive episode lasting at least 2 weeks within the 3 months prior to randomization; (3) symptoms of at least moderate severity (a score of ≥ 17 on the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) Mania Rating Scale (Axelson et al., 2003) or a score of ≥ 16 on the K-SADS Depression Rating Scale (Chambers et al., 1985) for at least 1 week over the previous month; (4) willingness to engage in pharmacotherapy with a study psychiatrist; and (5) at least one caregiver (usually a parent) willing to participate in family treatment. Exclusion criteria included meeting a current DSM-IV-TR diagnosis for a substance use or pervasive developmental disorder or being in a family where the child was a victim of current physical or sexual abuse (in which case appropriate notifications to the Department of Child Services and referrals for care were made).
2.2. Study Design
Participants were first prescreened over the telephone; those who appeared eligible were invited for an initial intake. Adolescent participants were interviewed with at least one parent using the K-SADS (Kaufman et al., 1997) to assess for DSM-IV-TR diagnoses, including bipolar I or II as well as comorbid diagnoses (including anxiety disorders [generalized anxiety disorder, panic disorder, social anxiety disorder, separation anxiety disorder, simple phobia, agoraphobia, obsessive-compulsive disorder, post-traumatic stress disorder, acute stress disorder], ADHD, oppositional defiant disorder [ODD], and conduct disorder [CD]). Diagnoses were based on consensus ratings of separate K-SADS assessments with adolescents and parent(s) and a diagnosis made by a board-certified psychiatrist. For this study, only comorbid disorders that were present at the time of the intake assessment were included in the data analyses. The KSADS mood modules were replaced with the K-SADS Mania Rating Scale and Depression Rating Scale, which rate symptoms on 6- or 7-point scales of severity and impairment. Reliabilities (intraclass r values) across the three sites (12 K-SADS tapes rated by an average of 12 raters each) were 0.89 for Depression Rating Scale scores and 0.81 for Mania Rating Scale scores.
Following the intake interview, eligible participants were randomly assigned to one of two treatment conditions – 21 sessions family-focused therapy (FFT) with pharmacotherapy or 3 sessions of psychoeducation (Enhanced Care; EC) with pharmacotherapy. Random assignment balanced the groups on study site, bipolar subtype (I or II), and index episode polarity (depressed, mixed, (hypo)manic). All psychosocial sessions were 50 minutes in length and included the patient participant, parents, and siblings when possible. FFT consisted of three consecutive modules: psychoeducation about the nature of bipolar illness, relapse prevention planning, and lifestyle management (e.g., importance of daily and nightly routines); communication enhancement training to alter negative dyadic or triadic interactional patterns; and problem-solving skills training to identify and generate solutions to problems in the family’s day-to-day life. EC consisted of three sessions of family psychoeducation focused on relapse prevention planning. The first 9 months were considered the active treatment phase, whereas months 10 – 24 were considered the post-treatment follow-up. All patients met with a studyaffiliated psychiatrist for the full 24-month study duration, and received medications based on good practice treatment protocol (for details, see Miklowitz et al., 2014).
2.2.1. Percentage of Time with Mood Symptoms.
To determine the percentage of time with mood symptoms, depressive and (hypo)manic, were assessed with weekly ratings on the Psychiatric Status Rating Scale (PSR) of the Adolescent Longitudinal Interval Follow-up Evaluation (ALIFE; Keller et al., 1987). The PSR depression, mania, and hypomania scales are rated on scales from 1 – 6, with 1 indicating that the patient has returned to “usual self” without any residual symptoms and scores of 5 and 6 indicating that the patient meets DSM-IV-TR criteria for a depressive, hypomanic or manic episode. The mania and hypomania subscales were combined into one (hypo)manic scale where 1 indicates no symptoms, 6 indicates full hypomania, and 7–8 indicates varying levels of fully syndromal mania. Percentages of time with subthreshold and full threshold mood symptoms were calculated by summing the total number of weeks the participants had a PSR score greater than 2, divided by the total number of weeks followed and multiplied by 100. Percentages of time with symptoms of depression and (hypo)mania were calculated separately.
2.2.2. Severity of Mood Symptoms
Participants were assessed at baseline, every 3 months during year 1, and every 6 months during year 2; severities of depression and (hypo)mania were measured at each assessment. Evaluators rated the worst week over the previous month using the ALIFE PSR depression, hypomanic and manic scales at baseline (for the 5 weeks leading up to random assignment) and each follow-up assessment (covering a 13-week period in year 1 and a 26-week period in year 2).
2.2.3. Family functioning
Family functioning was operationalized as the self-rated degree of family conflict as reported by the adolescent patient and separately by the primary caregiver via the Conflict Behavior Questionnaire (CBQ; Robin and Foster, 1995). The CBQ contains 20 true-false items that ask the respondent to rate items based on their relationship with a caregiver or with the child over the past three months. Sample items include, “My child is easy to get along with” and “I enjoy the talks we have.” The youth and parent scores were averaged to obtain a total family conflict score. Internal reliability for the CBQ was good (Cronbach’s α = 0.92).
2.3. Statistical Analyses
Statistical analyses were conducted using the Statistical Package for Social Sciences (SPSS 22). DBDs (ODD and CD) were examined as one group due to the small sample of participants with CD (see Table 1). However, based on research indicating differential effects of multifamily psychoeducational psychotherapy (MF-PEP) on ODD and CD symptoms in youth with mood disorders (Boylan et al., 2013), we conducted secondary analyses examining ODD only.
Table 1.
Sample Characteristics (N = 145)
| Family-Focused Treatment (FFT) | Enhanced Care (EC) | |
|---|---|---|
| Total Sample | n = 72 | n = 73 |
| Mean Age (SD) | 15.5 (1.4) | 15.7 (1.5) |
| Female (n, %) | 36 (50) | 43 (58.9) |
| Hispanic (n, %) | 7 (9.7) | 5 (6.8) |
| Nonwhite (n, %) | 12 (16.7) | 12 (16.4) |
| Bipolar I Disorder (n, %) | 40 (55.6) | 37 (50.7) |
| Bipolar II Disorder (n, %) | 32 (44.4) | 36 (49.3) |
| Patients with Comorbid Anxiety Disorder(s) | n = 27 | n = 30 |
| Mean Age (SD) | 15.4 (1.5) | 16.0 (1.4) |
| Female (n, %) | 14 (51.9) | 18 (53.3) |
| Hispanic (n, %) | 1 (3.7) | 3 (10.0) |
| Nonwhite (n, %) | 4 (14.8) | 6 (20.0) |
| Bipolar I Disorder (n, %) | 11 (40.7) | 14 (46.7) |
| Bipolar II Disorder (n, %) | 16 (59.3) | 16 (53.3) |
| Patients with Comorbid Attention-Deficit/Hyperactivity Disorder (ADHD) | n = 25 | n = 23 |
| Mean Age (SD) | 15.1 (1.3) | 15.6 (1.3) |
| Female (n, %) | 10 (40.0) | 10 (43.5) |
| Hispanic (n, %) | 2 (8.0) | 2 (8.7) |
| Nonwhite (n, %) | 5 (20.0) | 3 (13.0) |
| Bipolar I Disorder (n, %) | 13 (52.0) | 8 (34.8) |
| Bipolar II Disorder (n, %) | 12 (48.0) | 15 (65.2) |
| Patients with Comorbid Disruptive Behavior Disorders (DBDs) | n = 22a | n = 20 |
| Oppositional Defiant Disorder | n = 19 | n = 16 |
| Conduct Disorder | n = 4 | n = 4 |
| Mean Age (SD) | 15.2 (1.5) | 15.2 (1.7) |
| Female (n, %) | 10 (45.5) | 11 (55.0) |
| Hispanic (n, %) | 4 (18.2) | 3 (15.0) |
| Nonwhite (n, %) | 2 (9) | 5 (25.0) |
| Bipolar I Disorder (n, %) | 12 (54.5) | 15 (75.0) |
| Bipolar II Disorder (n, %) | 10 (45.5) | 5 (25.0) |
% represents percentage of participants in cell divided by n within sub-column
One participant within the FFT-A condition was diagnosed with oppositional defiant disorder and conduct disorder.
Analyses of variance (ANOVA) were used to examine differences across comorbidity groups (anxiety, ADHD, DBDs) and treatment groups (FFT versus EC) in the percentage of time with and without depressive or (hypo)manic symptoms over the 2-year study. Baseline mood symptoms (as measured by percentage of time over the 5 weeks preceding treatment) was used as a covariate in the ANOVAs.
Repeated measures mixed-effect regression models were used to examine main and interactive effects of treatment (FFT-A vs. EC), time, and comorbidity on mean PSR mood ratings and family conflict scores over the 24-month study. Mixed-effects regression models account for within-subject dependent data that results from repeated measures and efficiently handles missing data by using all available observations. Within-subject-level random intercepts were included to account for within-subject correlations induced by repeated measurements. Treatment group and current comorbidity diagnosis (with separate models examined for each comorbidity) were entered as the between-subject factor. Time was treated categorically across the course of the study to allow for different trajectories between groups as well as any higherorder non-linear trends throughout the 24-month period. Treatment site and baseline (hypo)manic and depressive symptoms were covaried in each model. When observing significant effects, we conducted post-hoc least square comparisons to determine the locus of effects.
Medication use was examined to determine if comorbidity groups differed in their use of medication classes (i.e., mood stabilizers, antidepressants, antipsychotics, and ADHD medications [e.g., stimulants, adrenergic reuptake inhibitors]) at the baseline and 12-month study time-points. Medication use for each class was coded dichotomously, and groups were compared on frequency of each class of medication using chi-square tests. If any of the comorbidity groups differed in their proportion of medication use, the corresponding repeated-measures mixed model for that comorbidity was re-computed for each outcome to determine whether medication use affected the relationships between comorbid disorders and outcome, or the interactions between comorbidity, treatment, and outcome.
3. Results
3.1. Sample Composition
In total, 145 adolescents participated in the study (n = 72 in FFT and n = 73 in EC), with an average age of 15.6 years (SD = 1.4). Across treatments, 77 (53.1%) adolescents had bipolar I disorder and 68 (46.9%) had bipolar II disorder. All participants entered the study with at least subthreshold mood symptoms: 37 (25.5%) entered in a depressed episode, 72 (49.7%) in a hypo(manic) episode, and 36 (24.8%) in a mixed or a subthreshold mixed episode. The two treatment groups did not differ on demographic variables (age, sex, race, ethnicity, SES), baseline mood symptoms, proportion of bipolar-type diagnosis, or rates of comorbid diagnoses. For comorbid disorders, a total of 57 adolescents (39.3%) had a current anxiety disorder, 48 (33.1%) had a current ADHD, and 42 (29.2%) had DBDs. Additionally, 3 (2.1%) adolescents had an eating disorder. Comorbidities were independent of each other with one exception: adolescents with ADHD were less likely to have a DBD diagnosis than those without ADHD (Wald χ2(1)=18.04, p<.001, odds ratio=0.20). Table 1 shows demographics and symptom characteristics of the participants.
3.2. Percentage of Time with Mood Symptoms
Over the 24-month study, adolescents with a comorbid anxiety diagnosis spent a significantly greater percentage of time with subthreshold or full threshold depressive symptoms compared to adolescents without comorbid anxiety (47.8% (SD = 27.5) versus 34.3% (SD = 26.8); F(1,117)=6.00, p=0.02); the two groups did not differ in percentage time with (hypo)manic symptoms. Adolescents with comorbid ADHD spent a significantly greater percentage of time with (hypo)manic symptoms compared to those without comorbid ADHD over the 24-months (31.8% (SD = 26.2) versus 19.4% (SD = 20.0); F(1,117)=8.15, p=0.01); the two groups did not differ in percentage time with depressive symptoms. Adolescents with comorbid DBDs did not differ in percentage of time with depressive or (hypo)manic symptoms compared to those without DBDs. Results remained the same when removing participants with CD (n = 8) and examining ODD only (n = 19) in the DBD analyses. There were no interactions between comorbidities and treatment condition in predicting percentage time with mood symptoms.
3.3. Severity of Mood Symptoms
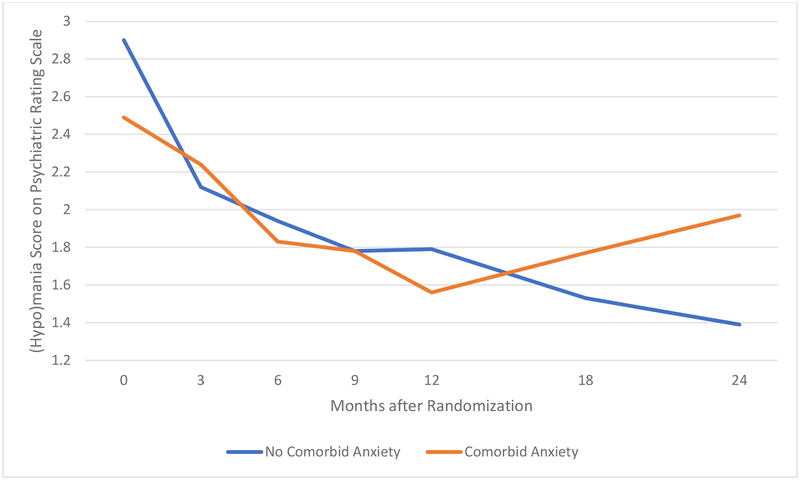
(Hypo)manic symptoms improved over the course of the 24-months in the full sample (F(6,501)=21.97, p<0.001). Comorbid anxiety disorder was not independently related to the severity of (hypo)manic symptoms over 24-months; however, there was a significant two-way interaction between anxiety diagnosis and time (F(6,503)=3.38, p=0.003). This interaction indicated that bipolar youth with and without anxiety disorders showed no differences throughout the active treatment phase (i.e., the first 9 months of the study) other than at baseline, when the comorbid anxiety group had significantly lower (hypo)manic symptoms (F(1,409)=5.83 p=0.02). The two groups then diverged during the post-treatment phase (months 9–24), with the comorbid anxiety group showing significantly higher (hypo)manic symptoms by the end of the study (F(1,558)=6.51, p=0.01; see Figure 1).
Figure 1.
Effect of Comorbid Anxiety by Time on (Hypo)manic Symptomsa
aWeekly Psychiatric Status Rating Scale (hypo)mania scores were obtained from the Adolescent Longitudinal Interval Follow-up Evaluation (ALIFE) and averaged across time intervals. Means are adjusted for pre-randomization (hypo)mania and depression scores and for study site.
Regarding depressive symptoms, depression improved in the full sample over the 24month study (F(6,515)=14.75 p<0.001). However, comorbid anxiety did not relate to the severity of depressive symptoms over time. There were no interactions between comorbid anxiety, time, or psychosocial treatment on the severity of (hypo)manic or depressive symptoms.
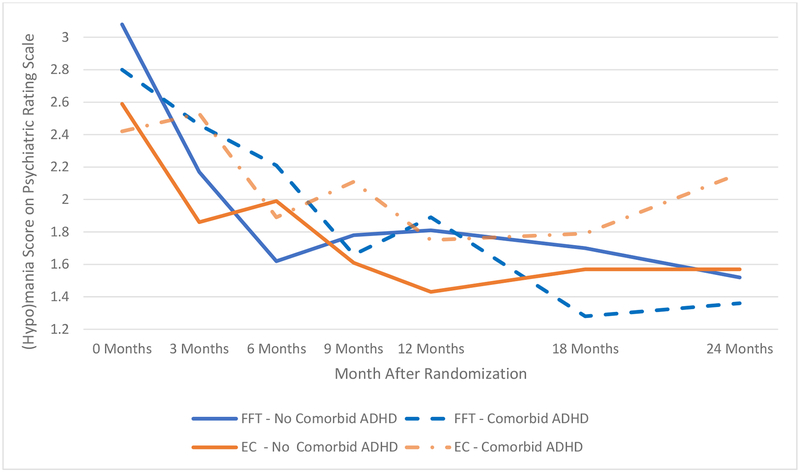
The main effect of comorbid ADHD did not relate to the severity of (hypo)manic symptoms over the course of the study; however, ADHD significantly interacted with time in predicting (hypo)manic symptoms (F(6,500)=2.22, p=0.04). The individuals with comorbid ADHD were initially slower to improve in (hypo)manic symptoms, having more severe (hypo)manic symptoms at the 3-month assessment compared to individuals without ADHD (F(1,463)=6.23, p=0.01). There was no two-way interaction between psychosocial treatment and comorbid ADHD; however, there was a marginally significant three-way interaction between comorbid ADHD, treatment, and time (F(6,500=2.02, p=0.06). The interaction indicated that there were no significant differences between treatment groups in the active treatment phase, but during the post-treatment phase, the patients with ADHD diverged based on their treatment condition (Figure 2). The patients with comorbid ADHD who received FFT-A showed an 18% decrease in (hypo)manic symptoms from the 9 – 24 months assessments. In contrast, patients with comorbid ADHD who received EC had a 2% increase in (hypo)manic symptoms over the same interval, a significant difference between treatment groups (F(1,570)=4.53, p=0.03; Figure 2). Comorbid ADHD did not relate to depressive symptoms over time, nor did it interact with time or treatment on depressive symptoms.
Figure 2.
Effect of Comorbid ADHD by Treatment and Time and (Hypo)manic Symptomsa
aWeekly Psychiatric Status Rating Scale (hypo)mania scores were obtained from the Adolescent Longitudinal Interval Follow-up Evaluation (ALIFE) and averaged across time intervals. Means are adjusted for pre-randomization (hypo)mania and depression scores and for study site.
Comorbid DBDs did not relate to (hypo)manic symptoms. Adolescents with comorbid DBDs had greater depressive symptoms over time than those without (F(1,127)=4.16, p=0.04). Comorbid DBDs did not interact with time or psychosocial treatment on mood symptoms. Results were unchanged when removing participants with CD from the mixed model involving DBD comorbidity.
3.4. Family Functioning
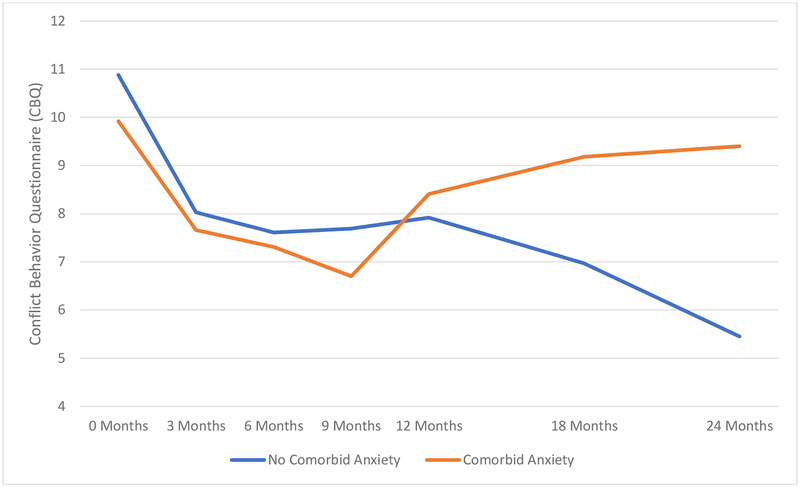
Across the full sample, there was an overall decrease in levels of parent and adolescentreported conflict over the study (F(6,383)=7.83, p<0.001). There was a significant interaction between comorbid anxiety and time in predicting family functioning scores (F(6,383)=3.66, p=0.001). The comorbid anxiety and no comorbid anxiety groups showed no differences throughout the active treatment phase. However, the two groups diverged during the posttreatment period such that by the end of the study, the group with comorbid anxiety disorder had higher conflict scores (F(1,407)=9.24, p=0.003; See Figure 3). There was no interaction between comorbid anxiety and treatment on family conflict scores.
Figure 3.
Effect of Comorbid Anxiety by Time on Family Conflictb
bConflict Behavior Questionnaire (CBQ) scores were obtained via self-report from patient and primary caregiver at each time interval and averaged to create an average family conflict score. Means are adjusted for pre-randomization (hypo)mania and depression scores and for study site.
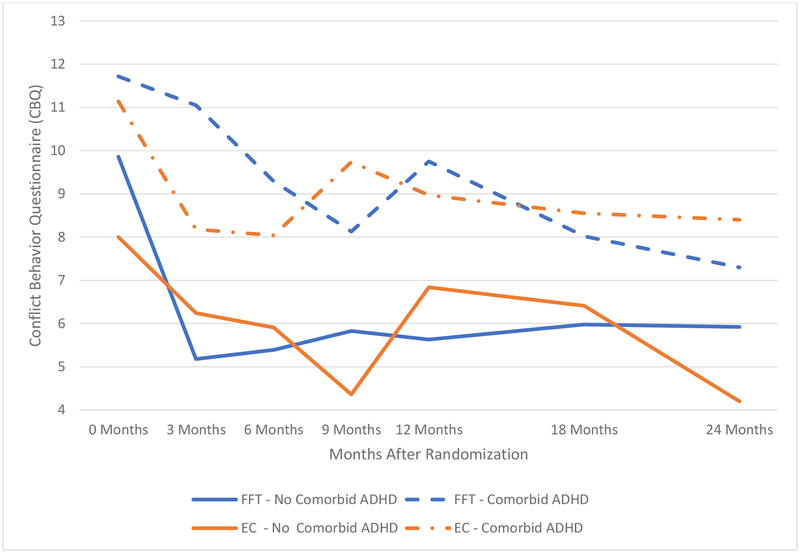
Comorbid ADHD was predictive of greater family conflict throughout the study (F(1,122)=14.02, p<0.001). There were no two-way interactions between comorbid ADHD and treatment or time on family conflict scores. However, there was a three-way interaction between comorbid ADHD, treatment, and time on family conflict scores (F(6,382)=2.29, p=0.04). This interaction indicated that the ADHD groups in both treatment conditions reported greater family conflict than the non-ADHD groups during the first year of the study. However, in the second study year, only the patients with comorbid ADHD who received EC reported higher family conflict scores than EC-treated patients without ADHD (F(1,390)=6.04, p=0.01). The ADHD group in FFT-A showed reductions in conflict that converged with the non-ADHD group in FFT-A group by the end of the study (see Figure 4).
Figure 4.
Effect of Comorbid ADHD by Treatment and Time on Family Conflictb
bConflict Behavior Questionnaire (CBQ) scores were obtained via self-report from patient and primary caregiver at each time interval and averaged to create an average family conflict score. Means are adjusted for pre-randomization (hypo)manic and depression scores and for study site.
Comorbid DBDs were predictive of higher family conflict throughout the study (F(1,128)=15.93, p<0.001). There were no interactions between comorbid DBDs, time or psychosocial treatment on family conflict. When removing participants with CD from the DBD model, comorbid ODD remained predictive of higher family conflict; however, it interacted with time (F(6,385)=2.22, p=0.04). The interaction indicated that participants with comorbid ODD had greater family conflict for most of the active treatment phase (i.e., baseline and 3 and 9 months) as well as the 12-month follow-up compared to participants without ODD, but it reduced and became indistinguishable from participants without ODD by the end of the posttreatment phase.
3.6. Medication Use
As reported in Miklowitz et al. (2014), the number of pharmacotherapy visits during the study (overall mean=11.6, SD=6.9) did not differ between the FFT-A and EC groups. Additionally, the two groups did not differ in the mean number of medications prescribed at baseline (FFT-A, mean=2.0, SD=1.0; EC, mean=1.6, SD=0.9) or at the 12-month or 24-month assessment points.
There were no differences in the frequency of prescriptions for different medication classes in the anxiety vs. non-anxiety or in the DBDs vs. non-DBDs group contrasts. Results were unchanged when removing CD from the analyses that examined participants with DBDs. Not surprisingly, adolescents with ADHD were more likely to be taking ADHD medications (e.g., mixed amphetamine salts) compared to adolescents without ADHD at the baseline (χ2(1)=12.73, p=.001) and 12-month time-points (χ2(1)=11.48, p=.002). Medication use, when covaried in the models examining the course of comorbid ADHD, did not relate to symptom outcomes or family conflict scores, nor did it change the outcomes of the significant effects presented above. However, the marginally significant effect of the three-way interaction between comorbid ADHD, treatment condition and time on (hypo)manic symptoms was weakened (F(6,537)=1.72, p=0.11) when including ADHD medication usage as a covariate even though ADHD medications did not in themselves predict (hypo)manic symptoms (F(1,113)=0.58, p=0.81).
4. Discussion
This study examined the predictive and moderating effects of comorbid axis I disorders in a randomized trial of family interventions for adolescents with bipolar I and II disorders. We found that bipolar youth with comorbid anxiety and ADHD (but not DBDs) spent more weeks with subthreshold or threshold mood symptoms over the two-year study. Comorbid anxiety was related to more weeks with depressive symptoms, while comorbid ADHD was related to more weeks with (hypo)manic symptoms. These findings are consistent with previous work that implicates anxiety as an antecedent of later depressive symptoms in the offspring of parents with bipolar disorder (Duffy et al., 2010) as well as a correlate of greater concurrent depressive symptoms (Cummings and Fristad, 2012). It is also consistent with the observation of longer courses of manic or mixed episodes in bipolar I patients with ADHD compared to those without (e.g., DelBello et al., 2007; Sivakumar et al., 2013).
If anxiety and ADHD precede the onset of mood symptoms and predict longer courses of depressive and (hypo)manic symptoms, respectively, then these comorbid conditions may be indicative of the “predominant pole” of the youth’s bipolar illness (Rosa et al., 2008). Thus, comorbid anxiety disorders may predict a predominantly depressive course of bipolar illness whereas comorbid ADHD may predict a predominantly (hypo)manic course over the lifetime. Identifying predominant polarity within bipolar patients has important treatment implications, such as the likelihood that patients will respond to antipsychotic medications (e.g., Colom et al., 2006; Popovic et al., 2012).
In the sample as a whole, there were reductions in the severity of (hypo)manic symptoms and family conflict over the two-year study. Nonetheless, comorbid ADHD predicted slower improvements in (hypo)manic symptoms during the active treatment phase and greater family conflict over the entire study. These results suggest that bipolar youth with versus without comorbid ADHD may require different treatment approaches. For example, bipolar youth with comorbid ADHD may require more intensive treatment efforts at the outset of treatment, possibly as a result of impairment in executive functioning, verbal memory deficits and/or other neurocognitive deficits (Narvaez et al., 2014; Rucklidge, 2006). The more intensive treatment efforts for these youth may involve more repetition of FFT-A communication and problemsolving skills or cognitive rehabilitation strategies elated to organization and planning (Maric et al., 2018; Safren et al., 2005).
Contrary to expectations, comorbid conditions played little role in moderating the effects of FFT on mood symptoms or family conflict. However, comorbid ADHD interacted with treatment condition in its relationship on family conflict and marginally on (hypo)manic symptom severity. Despite slower improvement in family conflict and (hypo)manic symptoms across ADHD groups overall, adolescents with ADHD in FFT-A had improvements during the post-treatment phase such that their level of family conflict and (hypo)manic symptoms became indistinguishable from the non-ADHD groups. On the other hand, adolescents with ADHD in EC had greater family conflict and more severe (hypo)manic symptoms at the end of the study. Of note, these results were unrelated to medications used to treat ADHD.
Considering the wide range of psychiatric presentations and comorbidities in BSDs, a staging model of treatment has been proposed in which treatment is based on the stage (i.e., severity, refractory and/or comorbid presentation) of illness (Berk et al., 2007; Kapczinski et al., 2009). Based on previous research, patients without significant mood symptoms or comorbid conditions benefit from a family psychoeducation-only treatment (Berk et al., 2011; Reinares et al., 2010). The results of this study suggest that comorbid ADHD in the context of bipolar disorder increases the stage of severity, which may necessitate more time-intensive adaptations of FFT-A or other skill-based treatments. We do not know whether other focused treatment protocols, such as cognitive behavioral therapy (CBT), interpersonal and social rhythm therapy or group psychoeducation would accomplish the same objectives, an important direction for research.
Conversely to comorbid ADHD, bipolar youth with comorbid anxiety had similar declines in (hypo)manic symptoms and family conflict throughout the active treatment phase compared to bipolar youth without anxiety. Previous work has also found that the presence of comorbid anxiety does not change the results that can be achieved with family therapy in youth with mood disorders (Cummings and Fristad, 2012). Individuals with anxiety may be particularly amenable to skills-based approaches, as perfectionist and social desirability tendencies common to anxiety contribute to treatment adherence (Cummings et al., 2014). However, in this study comorbid anxiety was predictive of a poorer course of (hypo)manic symptoms and family conflict in the post-treatment phase compared to youth without anxiety. Other prospective (up to 4 years) and retrospective studies have found that comorbid anxiety in bipolar youth is associated with longer and a greater number of affective episodes (Ratheesh et al., 2011; Sala et al., 2010; Sala et al., 2014). The link between anxiety and mood symptoms may result from shared cognitive, emotional and behavioral processes (Barlow, 2004; Brown and Barlow, 2009), as well as the influences of family conflict on both sets of disorders (Schleider and Weisz, 2017).
Comorbid anxiety disorders in bipolar youth were associated with a better response to FFT, CBT, and interpersonal and social rhythm therapy (IPSRT) when compared to a brief educational control (Deckersbach et al., 2014). IPSRT attempts to improve the social routines and reduce stressful life events, which are implicated in the onset of mood episodes (Frank, 2007; Malkoff-Schwartz et al., 2000). Previous work has also found that targeting cognitive distortions through CBT (Brent et al., 1998) and behavioral avoidance through exposure and response prevention (Peris et al., 2015) are efficacious in managing anxiety. Although they have not been examined in bipolar youth, FFT and other family treatments may be enhanced for these populations by creating modules for learning cognitive or behavioral skills (e.g., emotion regulation, extrafamilial social skills) in addition to communication and problem-solving.
Surprisingly, of the three clusters of comorbid disorders we examined, only DBDs were related to severity of depressive symptoms over the 2-year study. DBDs, overall, were also associated with increased family conflict throughout most of the study. Previous research suggests poor emotion regulation and communication skills form a vulnerability to mood difficulties in youth with DBDs (Cavanagh et al., 2017). While FFT-A does include communication training, emotion regulation is not encompassed within the family therapies of this study. Parental depression is also a significant risk factor in the development of DBDs and predicts persistence of disruptive behavioral problems (Burke et al., 2004; Campbell et al., 1996). Considering the high heritability of mood disorders (Lichtenstein et al., 2009; McGuffin et al., 2003), it is possible that parental psychiatric difficulties has a greater effect on depressive symptoms and family discord for bipolar youth with (versus without) DBDs.
There is a paucity of empirically-based treatments for depression in the context of DBDs (Burke et al., 2004). Some evidence suggests efficacy for multifamily psychoeducational psychotherapy for youth with mood disorders and disruptive behaviors (Boylan et al., 2013). Parent management training is another evidence-based treatment for youth with DBDs (Eyberg et al., 2008; Kazdin, 2018), One model (Sanders et al., 2000) included modules on mood management, although outcomes related to mood disorders were not reported. In terms of pharmacological treatments, there appears to be mixed treatment responses in this population. Naturalistic treatments and open-label trials have found poorer treatment response to valproate and lithium in bipolar youth with DBDs (e.g., Masi et al., 2008; Masi et al., 2010). However, a randomized controlled trial found significant improvements in manic symptoms in response to risperidone in this population (West et al., 2011).
We acknowledge several limitations of this study. We did not randomize participants to treatment conditions stratified on comorbid diagnoses, which would have increased our confidence in three-way interactions involving treatment, comorbid disorders, and time. We also did not measure the severity of comorbid diagnoses or assess whether patients still met criteria for a comorbid disorder during the 2-year follow-up. Considering the overlap between mood symptoms and ADHD (e.g., ADHD symptoms; Carlson and Klein, 2014; Duffy et al., 2018), we were careful to assess whether (hypo)manic or depressive symptoms were distinguishable from the adolescent’s baseline state, so as not to as well as not “double-count” the same symptoms (e.g., distractibility, pressured speech) for multiple disorders. Nonetheless, mood symptoms may have been superimposed onto comorbid diagnoses that fluctuated in severity over time. An additional limitation is that study psychiatrists prescribed medications to participants based on best clinical judgement. Thus, participants within a comorbidity group did not necessarily receive the same medications (and some did not receive medications at all). We cannot assume our results would have remained the same if participants within a comorbidity group received a standardized medication and dosage. Finally, the two treatment conditions (FFT-A and EC) were not matched in frequency of sessions, so we cannot determine whether effects by treatment are a result of time spent in clinical care as opposed to the content of that additional care.
In summary, comorbid anxiety and ADHD were associated with a greater time with and more severe mood symptoms among adolescents with bipolar I and II disorder. Effects of treatment condition did not vary with whether patients had comorbid anxiety disorders or DBDs; however, treatment conditions did have differential effects on patients with comorbid ADHD. Future research should investigate the underlying mechanisms (e.g., greater emotional dysregulation, cognitive impairment) that lead to poorer courses of symptoms and family functioning in bipolar youth with comorbid conditions. Additionally, it will be important to determine which adjunctive skills-based psychosocial treatments for bipolar youth with comorbid conditions. In will also be critical to evaluate in what order patients should receive care and whether levels of treatment intensity can be matched to patterns of comorbidity and symptom severity at treatment initiation.
Highlights.
Comorbid disorders were examined as moderators of treatment response to family therapy in bipolar youth over a 2-year period.
Comorbid anxiety was associated with more time with depressive symptoms as well as more severe (hypo)manic symptoms and family conflict.
Comorbid ADHD was associated with more time with (hypo)manic symptoms as well as more severe (hypo)manic symptoms and family conflict.
Bipolar youth with ADHD fared better in FFT-A relative to EC.
Comorbid DBDs were associated with more severe depressive symptoms and family conflict.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders (DSM-5®) Am. Psychiatr. Pub. [Google Scholar]
- Arnold LE, Demeter C, Mount K, Frazier TW, Youngstrom EA, Fristad M, Birmaher B, Findling RL, Horwitz SM, Kowatch R, 2011. Pediatric bipolar spectrum disorder and ADHD: comparison and comorbidity in the LAMS clinical sample. Bipolar Disord 13, 509–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N, 2003. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents Mary Ann Liebert, Inc. [DOI] [PubMed] [Google Scholar]
- Barlow DH, 2004. Psychological treatments. Am. Psychologist 59, 869. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Gartner J, Hagen B, 2000. Comorbid depression and heart rate variability as predictors of aggressive and hyperactive symptom responsiveness during inpatient treatment of conduct-disordered, ADHD boys. Aggressive Beh.: Of. J. Intern. Soc. Res. Aggres 26, 425–441. [Google Scholar]
- Beauchaine TP, Webster-Stratton C, Reid MJ, 2005. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: a latent growth curve analysis. J. Consult. Clin. Psychol 73, 371. [DOI] [PubMed] [Google Scholar]
- Berk M, Brnabic A, Dodd S, Kelin K, Tohen M, Malhi GS, Berk L, Conus P, McGorry PD, 2011. Does stage of illness impact treatment response in bipolar disorder? Empirical treatment data and their implication for the staging model and early intervention. Bipolar Disor 13, 87–98. [DOI] [PubMed] [Google Scholar]
- Berk M, Hallam KT, McGorry PD, 2007. The potential utility of a staging model as a course specifier: a bipolar disorder perspective. J. Affect. Disord 100, 279–281. [DOI] [PubMed] [Google Scholar]
- Boylan K, MacPherson HA, Fristad MA, 2013. Examination of disruptive behavior outcomes and moderation in a randomized psychotherapy trial for mood disorders. J. Am. Acad. Child Adoles. Psychiatry 52, 699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D, 1998. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. J. Am. Acad. Child Adolesc. Psychiatry 37, 906–914. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH, 2009. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychol. Assessment 21, 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Birmaher B, 2004. Oppositional defiant disorder and conduct disorder: a review of the past 10 years, part II. Focus 41, 1275–1576. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Pierce EW, Moore G, Marakovitz S, Newby K, 1996. Boys’ externalizing problems at elementary school age: Pathways from early behavior problems, maternal control, and family stress. Dev. Psychopathol 8, 701–719. [Google Scholar]
- Carlson GA, Klein DN, 2014. How to understand divergent views on bipolar disorder in youth. Annu. Rev. Clin. Psychol 10, 529–551. [DOI] [PubMed] [Google Scholar]
- Cavanagh M, Quinn D, Duncan D, Graham T, Balbuena L, 2017. Oppositional defiant disorder is better conceptualized as a disorder of emotional regulation. J. Atten. Disord 21, 381–389. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M, 1985. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Arch. Gen. Psychiatry 42, 696–702. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Daban C, Pacchiarotti I, Sanchez-Moreno J, 2006. Clinical and therapeutic implications of predominant polarity in bipolar disorder. J. Affect. Disord 93, 13–17. [DOI] [PubMed] [Google Scholar]
- Consoli A, Bouzamondo A, Guilé J-M, Lechat P, Cohen D, 2007. Comorbidity with ADHD decreases response to pharmacotherapy in children and adolescents with acute mania: evidence from a metaanalysis. Can. J. Psychiatry 52, 323–328. [DOI] [PubMed] [Google Scholar]
- Cummings CM, Caporino NE, Kendall PC, 2014. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol. Bull 140, 816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings CM, Fristad MA, 2012. Anxiety in children with mood disorders: a treatment help or hindrance? J. Abnorm. Child Psychol 40, 339–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckersbach T, Peters AT, Sylvia L, Urdahl A, Magalhães PV, Otto MW, Frank E, Miklowitz DJ, Berk M, Kinrys G, 2014. Do comorbid anxiety disorders moderate the effects of psychotherapy for bipolar disorder? Results from STEP-BD. Am. J. Psychiatry 171, 178–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM, 2007. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am. J. Psychiatry 164, 582–590. [DOI] [PubMed] [Google Scholar]
- Duffy A, Alda M, Hajek T, Sherry SB, Grof P, 2010. Early stages in the development of bipolar disorder. J. Affect. Disord 121, 127–135. [DOI] [PubMed] [Google Scholar]
- Duffy A, Malhi GS, Carlson GA, 2018. The challenge of psychiatric diagnosis: Looking beyond the symptoms to the company that they keep. Bipolar Disord 20, 410–413. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR, 2008. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J. Clin. Child & Adolesc. Psychol 37, 215–237. [DOI] [PubMed] [Google Scholar]
- Frank E, 2007. Interpersonal and social rhythm therapy: a means of improving depression and preventing relapse in bipolar disorder. J. Clin. Psychol 63, 463–473. [DOI] [PubMed] [Google Scholar]
- Frías Á, Palma C, Farriols N, 2015. Comorbidity in pediatric bipolar disorder: prevalence, clinical impact, etiology and treatment. J. Affect. Disord 174, 378–389. [DOI] [PubMed] [Google Scholar]
- Fristad MA, Verducci JS, Walters K, Young ME, 2009. Impact of multifamily psychoeducational psychotherapy in treating children aged 8 to 12 years with mood disorders. Arch. Gen. Psychiatry 66, 1013–1021. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Fersch-Podrat R, Axelson DA, Gilbert A, Hlastala SA, Birmaher B, Frank E, 2014. Early intervention for adolescents at high risk for the development of bipolar disorder: Pilot study of Interpersonal and Social Rhythm Therapy (IPSRT). Psychother 51, 180. [DOI] [PubMed] [Google Scholar]
- Joshi G, Wozniak J, Petty C, Vivas F, Yorks D, Biederman J, Geller D, 2010. Clinical characteristics of comorbid obsessive-compulsive disorder and bipolar disorder in children and adolescents. Bipolar Disord 12, 185–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapczinski F, Dias VV, Kauer-Sant’Anna M, Frey BN, Grassi-Oliveira R, Colom F, Berk M, 2009. Clinical implications of a staging model for bipolar disorders. Expert Rev. f Neurother 9, 957–966. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N, 1997. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child & Adolesc. Psychiatry 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, 2018. Implementation and evaluation of treatments for children and adolescents with conduct problems: findings, challenges, and future directions. Psychother. Res 28, 3–17. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC, 1987. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch. Gen. Psychiatry 44, 540–548. [DOI] [PubMed] [Google Scholar]
- Lichtenstein P, Yip BH, Björk C, Pawitan Y, Cannon TD, Sullivan PF, Hultman CM, 2009. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet 373, 234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malkoff-Schwartz S, Frank E, Anderson B, Hlastala S, Luther J, Sherrill J, Houck P, Kupfer D, 2000. Social rhythm disruption and stressful life events in the onset of bipolar and unipolar episodes. Psychol. Med 30, 1005–1016. [DOI] [PubMed] [Google Scholar]
- Maric M, van Steensel FJ, Bögels SM, 2018. Parental involvement in CBT for anxietydisordered youth revisited: family CBT outperforms child CBT in the long term for children with comorbid ADHD symptoms. J. Atten. Disord 22, 506–514. [DOI] [PubMed] [Google Scholar]
- Masi G, Milone A, Manfredi A, Pari C, Paziente A, Millepiedi S, 2008. Comorbidity of conduct disorder and bipolar disorder in clinically referred children and adolescents. J. Child Adolesc. Psychopharm 18, 271–279. [DOI] [PubMed] [Google Scholar]
- Masi G, Mucci M, Pfanner C, Berloffa S, Magazù A, Perugi G, 2012. Developmental pathways for different subtypes of early-onset bipolarity in youths. J. Clin. Psychiatry 73, 1335–1341. [DOI] [PubMed] [Google Scholar]
- Masi G, Perugi G, Millepiedi S, Mucci M, Pfanner C, Berloffa S, Pari C, Gagliano A, D’Amico F, Akiskal HS, 2010. Pharmacological response in juvenile bipolar disorder subtypes: a naturalistic retrospective examination. Psychiatry Res 177, 192–198. [DOI] [PubMed] [Google Scholar]
- McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A, 2003. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch. Gen. Psychiatry 60, 497–502. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC, 2007. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch. General Psychiatry 64, 543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J. p., Burstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M, 2011a. Service utilization for lifetime mental disorders in US adolescents: results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 50, 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Jin R, He J-P, Kessler RC, Lee S, Sampson NA, Viana MC, Andrade LH, Hu C, Karam EG, 2011b. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch. Gen. Psychiatry 68, 241–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, 2010. Bipolar disorder: A family-focused treatment approach Guilford Press. [Google Scholar]
- Miklowitz DJ, Axelson DA, Birmaher B, George EL, Taylor DO, Schneck CD, Beresford CA, Dickinson LM, Craighead WE, Brent DA, 2008. Family-focused treatment for adolescents with bipolar disorder: results of a 2-year randomized trial. Arch. Gen. Psychiatry 65, 1053–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Chung B, 2016. Family-focused therapy for bipolar disorder: Reflections on 30 years of research. Fam. Process 55, 483–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Schneck CD, George EL, Taylor DO, Sugar CA, Birmaher B, Kowatch RA, DelBello MP, Axelson DA, 2014. Pharmacotherapy and family-focused treatment for adolescents with bipolar I and II disorders: a 2-year randomized trial. Am. J. Psychiatry 171, 658–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Schneck CD, Singh MK, Taylor DO, George EL, Cosgrove VE, Howe ME, Dickinson LM, Garber J, Chang KD, 2013. Early intervention for symptomatic youth at risk for bipolar disorder: a randomized trial of family-focused therapy. J. Am. Acad. Child Adolesc. Psychiatry 52, 121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narvaez JC, Zeni CP, Coelho RP, Wagner F, Pheula GF, Ketzer CR, Trentini CM, Tramontina S, Rohde LA, 2014. Does comorbid bipolar disorder increase neuropsychological impairment in children and adolescents with ADHD? Rev. Bras. Psiquiatr 36, 53–59. [DOI] [PubMed] [Google Scholar]
- O’Donnell LA, Axelson DA, Kowatch RA, Schneck CD, Sugar CA, Miklowitz DJ, 2017. Enhancing quality of life among adolescents with bipolar disorder: A randomized trial of two psychosocial interventions. J. Affect. Disord 219, 201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Compton SN, Kendall PC, Birmaher B, Sherrill J, March J, Gosch E, Ginsburg G, Rynn M, McCracken JT, 2015. Trajectories of change in youth anxiety during cognitive—behavior therapy. J. Consult. Clin. Psychol 83, 239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis RH, Smoller JW, Fava M, Rosenbaum JF, Nierenberg AA, Sachs GS, 2004. The prevalence and clinical correlates of anger attacks during depressive episodes in bipolar disorder. J. Affect. Disord 79, 291–295. [DOI] [PubMed] [Google Scholar]
- Popovic D, Reinares M, Goikolea JM, Bonnin CM, Gonzalez-Pinto A, Vieta E, 2012. Polarity index of pharmacological agents used for maintenance treatment of bipolar disorder. Eur. Neuropsychopharmacol 22, 339–346. [DOI] [PubMed] [Google Scholar]
- Ratheesh A, Srinath S, Reddy YJ, Girimaji SC, Seshadri SP, Thennarasu K, Hutin Y, 2011. Are anxiety disorders associated with a more severe form of bipolar disorder in adolescents? Indian J. Psychiatry 53, 312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinares M, Colom F, Rosa AR, Bonnín CM, Franco C, Solé B, Kapczinski F, Vieta E, 2010. The impact of staging bipolar disorder on treatment outcome of family psychoeducation. J. Affect. Disorders 123, 81–86. [DOI] [PubMed] [Google Scholar]
- Robin A, Foster S, 1995. The conflict behavior questionnaire Dictionary of Behaviorial Assessment Techniques New York: Pergamon, 148–150. [Google Scholar]
- Rosa AR, Andreazza AC, Kunz M, Gomes F, Santin A, Sanchez-Moreno J, Reinares M, Colom F, Vieta E, Kapczinski F, 2008. Predominant polarity in bipolar disorder: diagnostic implications. J. Affect. Disorders 107, 45–51. [DOI] [PubMed] [Google Scholar]
- Rucklidge JJ, 2006. Impact of ADHD on the neurocognitive functioning of adolescents with bipolar disorder. Biol. Psychiatry 60, 921–928. [DOI] [PubMed] [Google Scholar]
- Safren SA, Otto MW, Sprich S, Winett CL, Wilens TE, Biederman J, 2005. Cognitivebehavioral therapy for ADHD in medication-treated adults with continued symptoms. Behav. Res. Ther 43, 831–842. [DOI] [PubMed] [Google Scholar]
- Sala R, Axelson DA, Castro-Fornieles J, Goldstein TR, Ha W, Liao F, Gill MK, Iyengar S, Strober MA, Goldstein BI, 2010. Comorbid anxiety in children and adolescents with bipolar spectrum disorders: prevalence and clinical correlates. J. Clin. Psychiatry 71, 1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sala R, Strober MA, Axelson DA, Gill MK, Castro-Fornieles J, Goldstein TR, Goldstein BI, Ha W, Liao F, Iyengar S, 2014. Effects of comorbid anxiety disorders on the longitudinal course of pediatric bipolar disorders. J. Am. Acam. Child Adolesc. Psychiatry 53, 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders MR, Markie-Dadds C, Tully LA, Bor W, 2000. The triple P-positive parenting program: a comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. J. Consult. Clin. Psychol 68, 624. [PubMed] [Google Scholar]
- Schleider JL, Weisz JR, 2017. Family process and youth internalizing problems: A triadic model of etiology and intervention. Dev. Psychopathol 29, 273–301. [DOI] [PubMed] [Google Scholar]
- Sivakumar T, Agarwal V, Sitholey P, 2013. Comorbidity of attention-deficit/hyperactivity disorder and bipolar disorder in North Indian clinic children and adolescents. Asian J. Psychiatry 6, 235–242. [DOI] [PubMed] [Google Scholar]
- Vitiello B, Riddle MA, Yenokyan G, Axelson DA, Wagner KD, Joshi P, Walkup JT, Luby J, Birmaher B, Ryan ND, 2012. Treatment moderators and predictors of outcome in the Treatment of Early Age Mania (TEAM) study. J. Am. Acad Child Adolesc. Psychiatry 51, 867–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West AE, Weinstein SM, Celio CI, Henry D, Pavuluri MN, 2011. Co-morbid disruptive behavior disorder and aggression predict functional outcomes and differential response to risperidone versus divalproex in pharmacotherapy for pediatric bipolar disorder. J. Child Adolescent Psychopharm 21, 545–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstrom EA, Arnold LE, Frazier TW, 2010. Bipolar and ADHD comorbidity: both artifact and outgrowth of shared mechanisms. Clin. Psychol.: Science and Practice 17, 350359. [DOI] [PMC free article] [PubMed] [Google Scholar]