Abstract
Background:
Futile or potentially inappropriate care (futile/PIC) has been suggested as a factor contributing to clinician well-being; however, little is known about this association.
Objective:
To determine whether futile/PIC provision is associated with measures of clinician well-being.
Design:
Cross-sectional, self-administered, online questionnaire.
Setting:
Two New York City Hospitals.
Participants:
Attending physicians, residents, nurses, and physician assistants in the fields of internal medicine, surgery, neurology, or intensive care.
Exposure(s):
Provision of perceived futile/PIC.
Measurements:
Main outcomes included (1) clinician burnout, measured using the Physician Worklife Study screen; (2) clinician depression, measured using the Patient Health Questionnaire; and (3) intention to quit, measured using questions assessing thoughts of quitting and how seriously it is being considered.
Results:
Of 1784 clinicians who received surveys, 349 participated. Across all clinicians, 91% reported that they either had or had possibly provided futile/PIC to a patient. Overall, 43.4% of clinicians screened positive for burnout syndrome, 7.8% screened positive for depression, and 35.5% reported thoughts of leaving their job as a result of futile/PIC. The amount of perceived futile/PIC provided was associated with burnout (odds ratio [OR] 3.8 [16–30 patients vs 1–2 patients]; 95% confidence interval [CI]: 1.1–12.8) and having thoughts of quitting (OR, 7.4 [16–30 patients vs 1–2 patients]; 95% CI:2.0–27), independent of depression, position, department, and the number of dying patients cared for.
Conclusions:
A large majority of clinicians report providing futile/PIC, and such care is associated with measures of clinician well-being, including burnout and intention to quit.
Keywords: end-of-life care, clinician well-being, burnout, medical futility
Introduction
One in 5 Americans will receive intensive care at or near the end of life (EOL).1 Although such care saves lives, it also has the potential to prolong the dying process and increase suffering of patients and families.2 In many cases, the care provided at the EOL is not consistent with patients’ values or goals.1,3 Describing and defining care that is discordant with a given patient’s goals of care or values, commonly referred to as futile care, has proven controversial.4 The most broadly accepted definition, proposed by 5 major critical care societies, defines futile care as that which cannot accomplish the effect sought by the patient and “potentially inappropriate” as that which has at least some chance of accomplishing the desired effect.5
Although there has been limited research on futile or potentially inappropriate care (futile/PIC), the few studies conducted suggest that futile/PIC is a common occurrence. For example, in a survey of clinicians in California intensive care units (ICUs), 38% of respondents were able to identify patients receiving inappropriate care on the day they completed the survey.6 Another study that prospectively looked at care provided in the ICU found that treatment was futile, or probably futile, 20% of the time.7 Futile/PIC has been associated with significant financial costs,7 decreased quality of patient care,8 and clinician moral distress.9,10 Burnout, one of the most damaging consequences of clinician moral distress,11 has also been proposed as an outcome of providing futile/PIC12; however, no studies from the United States have demonstrated this association. Evidence for associations between burnout and futile/PIC is only supported by indirect associations and studies from international contexts.13,14
Burnout syndrome is associated with emotionally intense work demands and results in exhaustion, cynicism, and decreased work effectiveness.15,16 Among health-care providers in the United States, the prevalence of burnout syndrome appears to have been increasing over the last decade,17,18 with one third of nurses and over half of physicians reporting symptoms of burnout.18–20 Burnout syndrome among health-care providers has emerged as an important area of study because it has been linked to quality-of-care outcomes including self-reported medical errors, increased patient mortality, clinician depression, and substantial financial costs to the health-care system.12,15,21–25
In this study, we sought to better understand the prevalence of futile/PIC provision and its association with prespecified primary measures of clinician well-being including burnout, depression, and thoughts of quitting.
Methods
Study Design
This study involved a cross-sectional, self-administered, online questionnaire sent to registered nurses (RN), physician assistants, nurse practitioners, attending physicians, and physician trainees (residents, interns, and fellows) conducted at the NewYork-Presbyterian Hospital (NYPH)/Weill Cornell Medicine (WCM) and NewYork-Presbyterian/Queens (NYPQ), from June to July 2017. NewYork-Presbyterian Hospital/WCM and NYPQ are large, urban academic medical centers in New York City, New York; NYPH/WCM is a referral center; and NYPQ is a community-based hospital. Inclusion criteria included clinical staff (1) who worked in the fields of internal medicine, surgery, neurology, or intensive care, (2) who were involved in the care of at least 5 hospital inpatients in the previous 6 months, and (3) who were employed at least part time for the last 6 months.
Study staff collaborated with departmental leaders to identify eligible clinical providers and held information sessions with potential participants to inform them of the study and its aims. In collaboration with the institutional review boards at NYPH/WCM and NYPQ, which both approved this study, significant efforts were made to protect participants due to the potentially sensitive nature of this study. This included securely collecting and managing responses in an anonymous REDcap database,26 collecting minimal demographic information and combining responses from both hospitals. Clinicians were presented with potential risks of participating at the outset of the survey, and consent was implied if they continued the survey.
Measures
Futile care.
To measure the prevalence of clinician-perceived futile/PIC, we asked clinicians whether in the last 6 months, they had provided care they considered to be futile or potentially inappropriate (1 = no; 2 = possibly; 3 = yes) and for how many patients had provided such care (6-point ordered categorical variable). For analysis, the provision of futile/PIC in the last 6 months was recoded into a binary variable (0 = no; 1 = yes and possibly).
To understand the intensity of distress providers experience, we asked “If you have provided futile/PIC; how much distress did you experience?” (10-point scale; 1 = no distress, 10 = extreme distress).
Burnout.
To measure burnout, we used a single-item question initially developed for the physician work–life study,27 which has been validated by demonstrating statistically significant associations with the Maslach Burnout Inventory and found to be predictive of the emotional exhaustion subscale, which is the core component of burnout.28–30 Scores ≥3 were used as the burnout screening cutoff.27
Depression.
To measure depression, we used the 2 item Patient Health Questionnaire-2 (PHQ-2),31 which consists of the first 2 questions of the PHQ-9 and is a well-validated and commonly used measure. Scores ≥3 were used as the depression screening cutoff.31
Intention to quit.
To measure the intention to leave ones’ position, we used 2 items similar to existing, validated measures.32 These included (1) “As a result of providing futile/PIC, have you had thoughts of leaving your current position?” (1 = no, 2 = somewhat, 3 = yes) and (2) “If you are considering leaving your position due to pressures around provision of futile/PIC, how seriously are you considering it?” (10-point scale; 1 = not very seriously, 10 = very seriously). For analysis, intention to yes and quit was recoded to a binary variable (0 = no; 1 = somewhat).
Statistical Analysis
Summary statistics were calculated to describe basic trends, and significance testing of associations between outcome and predictor variables was done with χ2 and Fisher exact tests, as appropriate. The distributions of binary variables are described using Clopper-Pearson binomial 95% confidence limits, and tests of normality were performed using Shapiro-Wilk tests. Bivariable and multivariable logistic regression models were used to identify predictors of burnout and having thoughts of quitting. Statistical inferences were based on 2-sided tests with P < .05 considered statistically significant. Statistical analyses were conducted using STATA statistical software version 15.1 (STATAcorp; College Station, Texas).
Results
Respondent Characteristics
The survey was sent to 1784 clinicians, and 349 responded for a response rate of 19.6%. Sixteen respondents did not meet inclusion criteria and were dropped from analysis. Registered nurses comprised the largest group of respondents, and most respondents were from either a medical or an intensive care service (Table 1). The majority of providers (51.6%) cared for between 6 and 30 dying patients in the preceding 6 months, with 15.6% caring for over 31 dying patients (Table 1).
Table 1.
Respondent Characteristics.
| N | Percentagea | |
|---|---|---|
| Position | ||
| Attending | 67 | 20.1 |
| Registered nurse | 135 | 40.5 |
| NP/PA | 52 | 15.6 |
| Intern/resident/fellow | 72 | 21.6 |
| Department | ||
| Intensive care/critical care | 119 | 35.7 |
| Medical service | 133 | 39.9 |
| Surgical service | 29 | 8.7 |
| Neurological service | 19 | 5.7 |
| Medical surgical unit | 16 | 4.8 |
| Number of dying patients cared for in last 6 months | ||
| 0 | 12 | 3.6 |
| 1–5 | 96 | 28.8 |
| 6–30 | 172 | 51.6 |
| 31–51 | 30 | 9.0 |
| 51–74 | 12 | 3.6 |
| 75+ | 10 | 3.0 |
| Provision of futile or potentially inappropriate care to dying patients in the last 6 months | ||
| Yes | 252 | 75.7 |
| No | 29 | 8.7 |
| Possibly | 52 | 15.6 |
| If yes or possibly above, number of patients provided such care | ||
| 1–2 | 83 | 27.4 |
| 3–5 | 95 | 31.4 |
| 6–15 | 91 | 30.0 |
| 16–30 | 26 | 8.6 |
| 31+ | 8 | 2.7 |
| Number of patients for which the provision of futile or potentially inappropriate care was observed | ||
| 0 | 21 | 6.3 |
| 1–2 | 82 | 24.3 |
| 3–5 | 73 | 21.9 |
| 6–15 | 87 | 26.1 |
| 16–30 | 44 | 13.2 |
| 31+ | 26 | 7.8 |
| Total | 333 | - |
Abbreviations: NP, nurse practitioners; PA, physician assistants.
Percentages calculated included missing values. Seven respondents declined to enter position, 17 declined to enter department, 1 declined to enter number of dying patients cared for, 1 declined to enter quantity of futile/PIC provided, and 1 declined to enter quantity of futile/PIC observed.
Prevalence of Futile or Potentially Inappropriate Care
Across all clinicians, 91.4% reported that they either had, or had possibly, provided futile/PIC to dying patients in the preceding 6 months, with 41.3% reporting that they had provided futile/PIC for at least 6 patients (Table 1).
Adjusting for department, physician trainees were significantly more likely than attending physicians to report providing futile/PIC (odds ratio [OR] 8.1; 95% confidence interval [CI]:1.6–40.8; P = .01). Clinicians working in intensive/critical care departments reported providing futile/PIC the most frequently (95%) and were adjusting for position; they were more likely to report providing such care than those working in surgical (OR, 7.0; CI: 1.3–37.6; P = .02) or neurological services (OR, 14.1; CI: 3.0–66; P = .001).
Burnout, Depression, and Desire to Quit
The distress clinicians reported as a result of futile/PIC (measured on a 10-point scale) was normally distributed (Shapiro-Wilk, P = .43) around a mean of 5.7 (standard deviation of 2.3), and there were no significant differences by department or position. The total proportion of clinicians who screened positive for depression was 7.8%, and there were no significant differences across position or department.
Overall, 35.1% of providers reported that they had thoughts of leaving their job as a result of futile/PIC, and this was highest among RNs (47.3%; Table 2). Further, of RNs who reported thoughts of leaving their job, 68.9% rated the seriousness of these thoughts as a 5 or greater on a 10-point scale. In multivariable analysis, the odds of having thoughts of leaving ones’ job significantly increased with the amount of futile/PIC clinicians reported providing. Compared to clinicians who reported providing futile/PIC for 1 to 2 patients, those who provided such care for 3 to 5 patients were 3.5 times more likely to have thoughts of quitting (CI: 1.6–7.8; P =.002), and those who reported providing futile/PIC for 16 to 30 patients were 7.4 times more likely to have thoughts of quitting (CI: 2.0–27; P = .003; Table 3).
Table 2.
Measures of Wellness Including Depression, Burnout, Thoughts of Leaving Ones Job, and Perceptions of Futile/PIC by Position, Department, and the Amount of Perceived Futile/PIC Provided.
| Provided Futile/PIC | Screened Positive for Depression | Screened Positive for Burnout | Reported Thoughts of Leaving Job | |||||
|---|---|---|---|---|---|---|---|---|
| N (%) | Pa | N (%) | Pa | N (%) | Pa | N (%) | Pa | |
| Quantity of futile/PIC care provided | ||||||||
| 1–2 | 4 (4.9) | .53 | 20 (24.1) | <.001 | 15 (18.1) | <.001 | ||
| 3–5 | 9 (10.0) | 43 (46.2) | 41 (44.1) | |||||
| 6–15 | 9 (10.0) | 51 (57.3) | 37 (41.1) | |||||
| 16–30 | 2 (7.7) | 15 (57.7) | 15 (57.7) | |||||
| 31+ | 1 (14.3) | 7 (87.5) | 7 (87.5) | |||||
| Position | ||||||||
| Attending physician | 57 (85.1) | .09 | 3 (4.8) | .46 | 17 (25.4) | <.003 | 14 (20.9) | <.001 |
| Registered nurse | 126 (93.3) | 12 (9.4) | 64 (48.8) | 62 (47.3) | ||||
| NP/PA | 46 (88.5) | 2 (3.9) | 20 (39.2) | 24 (46.1) | ||||
| Physician trainee | 69 (95.8) | 7 (9.9) | 38 (53.5) | 14 (19.7) | ||||
| Department | ||||||||
| Intensive/critical care | 114(95.8) | .01 | 9 (7.8) | .88 | 56 (47.5) | .61 | 55 (47.0) | .003 |
| Medical service | 123 (92.5) | 10(7.6) | 52 (39.7) | 38 (29.0) | ||||
| Surgical service | 25 (86.2) | 1 (4.0) | 13 (48.1) | 5(17.9) | ||||
| Neurological service | 14(73.7) | 2 (10.5) | 9 (47.4) | 5 (26.3) | ||||
| Totalb | 298 (91) | 25(8) | 142 (43) | 115 (35) | ||||
Abbreviations: NP, nurse practitioners; PA, physician assistants; PIC, potentially inappropriate care.
significance testing performed with χ2 or Fisher Exact, as appropriate.
Six participants chose to not respond to the burnout measure, 12 chose to not respond to the depression measure and 5 chose to not respond to the “thoughts of quitting” measure.
Table 3.
Bivariable and Multivariable Models Describing the Association Between Provider Burnout and Thoughts of Quitting With Predictor Variables.
| Associations With Burnout | Associations With Thoughts of Quitting | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bivariable Models (Unadjusted Estimates) |
Multivariable Model (Adjusted Estimates) |
Bivariable Models (Unadjusted Estimates) |
Multivariable Model (Adjusted Estimates) |
|||||||||
| Odds Ratio |
P Value |
Odds Ratio |
P Value |
Odds Ratio |
P Value |
Odds Ratio |
P Value |
|||||
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||
| Quantity of futile/PIC care provided | ||||||||||||
| 1–2 | REF | REF | REF | REF | ||||||||
| 3–5 | 2.7 | 1.4–5.2 | .003 | 2.6 | 1.2–5.4 | .011 | 3.6 | 1.8–7.1 | <.001 | 3.5 | 1.6–7.8 | .002 |
| 6–15 | 4.2 | 2.2–8.1 | <.001 | 3.8 | 1.6–8.9 | .002 | 3.2 | 1.6–6.4 | .001 | 3.4 | 1.4–8.3 | .008 |
| 16–30 | 4.3 | 1.7–10.9 | .002 | 3.8 | 1.1–12.8 | .031 | 6.2 | 2.4–16.1 | <.001 | 7.4 | 2.0–27 | .003 |
| 31+ | 22.0 | 2.6–190 | .005 | 10.7 | 0.83–137 | .069 | 31.7 | 3.6–277 | .002 | 41.3 | 2.9–596 | .006 |
| Position | ||||||||||||
| Attending physician | REF | REF | REF | REF | ||||||||
| Registered nurse | 2.8 | 1.5–5.4 | .002 | 2.0 | 0.69–5.7 | .20 | 3.4 | 1.7–6.7 | <.001 | 2.4 | 0.83–7.2 | .11 |
| NP/PA | 1.9 | 0.86–4.2 | .11 | 1.7 | 0.65–4.4 | .28 | 3.2 | 1.4–7.2 | .004 | 3.4 | 1.3–8.8 | .01 |
| Physician trainee | 3.4 | 1.7–7.0 | .001 | 2.3 | 0.95–5.6 | .07 | 0.93 | 0.41–2.1 | .86 | 0.64 | 0.24–1.7 | .37 |
| Department | ||||||||||||
| Intensive/critical care | REF | REF | REF | REF | ||||||||
| Medical service | 0.73 | 0.44–1.2 | .22 | 0.70 | 0.28–1.7 | .43 | 0.46 | 0.27–0.78 | .004 | 0.81 | 0.32–2.0 | .65 |
| Surgical service | 1.0 | 0.45–2.4 | .95 | 1.4 | 0.37–5.0 | .64 | 0.25 | 0.09–0.69 | .008 | 0.76 | 0.17–3.4 | .72 |
| Neurological service | 1.0 | 0.38–2.6 | .511 | 1.1 | 0.31–4.2 | .84 | 0.40 | 0.14–1.2 | .10 | 0.85 | 0.22–3.3 | .82 |
| Depression | 11.4 | 3.34–39.0 | <.001 | 9.5 | 2.7–34.1 | .001 | 4.5 | 1.9–10.8 | .001 | 5.1 | 1.8–13.9 | .002 |
| Quantity of dying patients cared for | 1.5 | 1.2–2.0 | .001 | 1.2 | 0.78–1.8 | .43 | 1.3 | 1.1–1.7 | .02 | 0.91 | 0.58–1.4 | .67 |
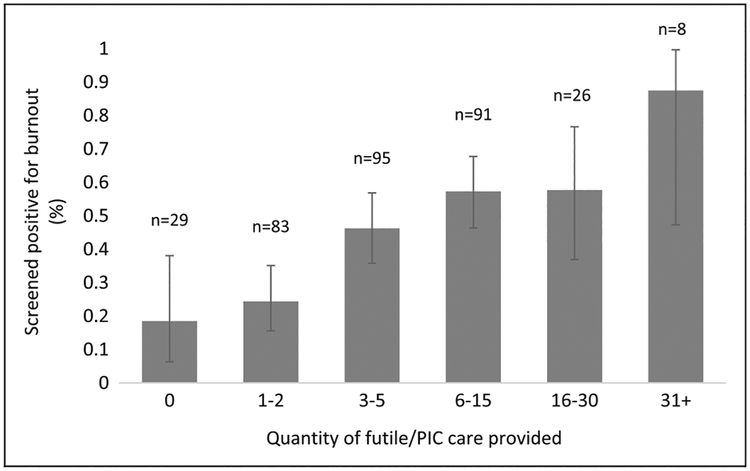
Overall, 43.4% of providers screened positive for burnout syndrome (Table 2). Across all clinicians, the proportion who screen positive for burnout increases along with the reported number of futile/PIC cases provided, ranging from 19% (CI:6.3%−38.1%) among those reporting no cases of futile/PIC to 88% (CI: 47.3%−99.7%) among those providing such care for over 31 patients (Figure 1). In multivariable analysis, the amount of futile/PIC clinicians reported providing was associated with burnout, independent of position, department, depression, and the number of dying patients cared for. Compared to clinicians who reported providing futile/PIC for 1 to 2 patients, those who provided such care for 3 to 5 patients were 2.6 times (CI: 1.2–5.4; P = .01) more likely to have burn out, and those who provided such care for 16 to 30 patients were 3.8 times (CI: 1.1–12.8; P = .031) more likely to have burn out (Table 3).
Figure 1.
Proportion of providers who screen positive for burnout over the amount of futile or potentially inappropriate care clinicians reported providing in the last 6 months. Uncertainty defined using Clopper-Pearson binomial 95% confidence limits.
Discussion
In this study, we found that a large majority of clinicians (91.4%) reported either providing or possibly providing futile/PIC. In addition, we found that the amount of such care provided is significantly associated with clinician burnout and with having thoughts of leaving one’s job, independent of other factors including position, department, depression, and the number of dying patients for whom they cared. To the best of our knowledge, this is the first study to show the association of futile/PIC with provider burnout in a US context.
The proportion of clinicians in this study who reported providing futile/PIC is consistent with what has been reported elsewhere. We found that 89.7% of clinicians reported providing futile/PIC, and this was highest among physician trainees (95.3%). These results are similar to a Canadian study of intensive care providers who found that 95% of nurses and 87% of physicians believed that futile care had been provided in their ICUs within the last year.33 Other studies have also found that physician trainees report significant distress associated with issues surrounding futile/PIC, and in 1 study, 70% reported providing care against their conscience at the EOL.10,34 These morally distressing experiences during the most formative years of training can lead to diminished professional identity and demoralization.11
In this study, the proportion of clinicians who screened positive for burnout was also similar to what has been reported elsewhere. We found that 43.4% of all providers screened positive for burnout. When controlling for position, department, and the number of dying patients cared for, only depression and provision of perceived futile/PIC were associated with burnout. One large study of US physicians found that 54% were experiencing professional burnout, and some studies have suggested that this number may be as high as 71%.12,18 Several studies have found that providers in intensive/critical care are more likely to experience burnout.12 While intensive/critical care was associated with greater burnout in bivariable analysis, this effect was not seen in multivariable analysis, suggesting that high rates of burnout in ICUs may at least in part be explained by the greater provision of futile/PIC in ICUs.
Burnout syndrome among health-care providers has been associated with a multitude of negative outcomes for clinicians, patients, and even hospital systems.12 In recognition of this, there has been a growing literature aimed at identifying the causes of burnout and proposing solutions. Although a 2016 review by the official critical care societies collaborative identified PIC as a major cause of burnout,12 there have been few interventions that focus on futile/PIC. Most burnout interventions have focused on individual factors, such as mindfulness exercises, or organizational factors, such as decreasing workload.35,36 The results of our study suggest that interventions focused on reducing rates, and perceptions of futile/PIC may be an important means of reducing burnout and clinician turnover.
Evidence continues to build that clinician well-being, the fourth component of the “quadruple aim” to improve health-care quality, is critical to the health of both patients and health-care systems.37 A recently published charter on clinician well-being states that effective patient care requires the well-being of all members of the health-care team. The charter concludes that health-care organizations need to not only identify factors associated with well-being but also leverage these factors to help design effective interventions.37 Although futile/PIC is often suggested as a cause of burnout and decreased well-being,12 it is seldom mentioned as an opportunity for interventions aimed at decreasing burnout. Most academic discussions on improving the organizational factors that affect well-being focus on factors that detract from satisfying, supportive, and caring relationships with patients such as burdensome electronic health records, increased administrative burdens, and workload.16,38 Futile/PIC is an understudied barrier to satisfying and caring relationships with patients, and our results suggest that clinician well-being interventions should include those aimed at decreasing perceptions of futile/PIC.
There are several limitations to this study that may affect interpretation of our results. First, because the study was performed in hospitals in New York City, it may not be generalizable to additional contexts. To make our results more generalizable, we selected 2 hospitals that operate in very different contexts with demographically different populations: one, a tertiary referral center in Manhattan, and the other, a community hospital in Queens, one of the most ethnically diverse counties in the United States. We believe that this will make our results applicable to a larger proportion of hospitals in the United States.
Another limitation of this study was the low response rate, which introduces the risk of nonresponse bias. We have several reasons to believe that the population sampled reflects the general population at both hospitals. First, the frequencies of burnout, depression, thoughts of quitting, and provision of perceived futile/PIC observed in our study are similar to those that have been published elsewhere.12,18 Second, the scale of how much distress clinicians perceive from futile/PIC care was normally distributed around a mean similar to what has been published elsewhere,6 suggesting that there was no obvious bias among participants regarding perceptions of futile/PIC. Finally, Web-based surveys of clinicians often have response rates lower than 20%;39 moreover, responding and nonresponding health-care providers have been repeatedly shown to have similar characteristics.40
There are several steps that further research on this subject could take to improve understanding of the role that futile/PIC plays in clinician well-being. First, although a definition of futile/PIC was given to participants, there was likely a variety of interpretations (eg, care that was too aggressive, or care that was not aggressive enough), which may have varying effects on clinician well-being. Similarly, using a dichotomized measure of futile/PIC over a 6-month period, it is difficult to determine the degree to which clinicians found specific instances of care to be either futile or potentially inappropriate or when a specific experience occurred. Events that occurred months prior may have a lower impact on well-being and those that are ongoing may play a larger role, despite their evolving and unresolved nature. Focus group analyses of a subgroup of participants could provide insight into the abovementioned questions as well as expert adjudication of specific instances determined by clinicians to be futile/PIC.
Second, to protect participants, extensive demographic information was not collected, and some groups were aggregated for the analysis (eg, physician trainees), which may introduce bias. Future studies could investigate other variables that may influence clinician perceptions of futile/PIC including clinician sex, years in practice, marital status, and/or religious beliefs. Finally, clinician well-being is a complicated outcome with many contributing factors, and future studies would benefit from a more detailed assessment of the role that these specific factors play in clinician well-being. For example, the quality of a clinicians’ communication skills may work to both decrease experiences with futile/PIC and may also improve clinician well-being.
Conclusion
Futile/PIC has been proposed as an important contributor to burnout syndrome among health-care providers, but this has not been demonstrated among US clinicians. Our results suggest that provision of futile/PIC care is common and causes significant distress among providers. We also show that having thoughts of quitting and burnout are associated with the amount of provider perceived futile/PIC. Future research is needed to address how to protect clinicians from the negative consequences of exposure to providing futile/PIC.
Acknowledgment
The research team acknowledge the valued contributions of Claire E. Holland, MSPH. She was not compensated for her contributions to this project.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a grant to Dr Prigerson from the National Cancer Institute (CA197730). Drs Prigerson and Kozlov were supported by funding from the National Institute on Aging (AG049666) and National Center for Advancing Translational Science grant from the National Institutes of Health (UL1 TR002384). Jason Lambden was supported by the American Federation for Aging Research (Medical Student Training in Aging Research Program).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, et al. ; Robert Wood Johnson Foundation ICU End-Of-Life Peer Group. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32(3):638–643. [DOI] [PubMed] [Google Scholar]
- 2.Montgomery H, Grocott M, Mythen M. Critical care at the end of life: balancing technology with compassion and agreeing when to stop. Br J Anaesth. 2017;119(suppl 1):i85–i89. [DOI] [PubMed] [Google Scholar]
- 3.Khandelwal N, Curtis JR, Freedman VA, et al. How often is endof-life care in the United States inconsistent with patients’ goals of care? J Palliat Med. 2017;20(12):1400–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kasman DL. When is medical treatment futile? J Gen Intern Med. 2004;19(10):1053–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bosslet GT, Pope TM, Rubenfeld GD, et al. An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med. 2015;191(11):1318–1330. [DOI] [PubMed] [Google Scholar]
- 6.Anstey MH, Adams JL, McGlynn EA. Perceptions of the appropriateness of care in California adult intensive care units. Crit Care. 2015;19(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huynh TN, Kleerup EC, Wiley JF, et al. The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med. 2013;173(20):1887–1894. [DOI] [PubMed] [Google Scholar]
- 8.Kompanje EJ, Piers RD, Benoit DD. Causes and consequences of disproportionate care in intensive care medicine. Curr Opin Crit Care. 2013;19(6):630–635. [DOI] [PubMed] [Google Scholar]
- 9.Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med. 2007;35(2):422–429. [DOI] [PubMed] [Google Scholar]
- 10.Dzeng E, Colaianni A, Roland M, et al. Moral distress amongst American physician trainees regarding futile treatments at the end of life: a qualitative study. J Gen Intern Med. 2016;31(1):93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. 2009;20(4):330. [PubMed] [Google Scholar]
- 12.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement—burnout syndrome in critical care health-care professionals: a call for action. Chest. 2016;150(1):17–26. [DOI] [PubMed] [Google Scholar]
- 13.Meltzer LS, Huckabay LM. Critical care nurses’ perceptions of futile care and its effect on burnout. Am J Crit Care. 2004;13(3): 202–208. [PubMed] [Google Scholar]
- 14.Schwarzkopf D, Rüddel H, Thomas-Rüddel DO, et al. Perceived nonbeneficial treatment of patients, burnout, and intention to leave the job among ICU nurses and junior and senior physicians. Crit Care Med. 2017;45(3):e265–e273. [DOI] [PubMed] [Google Scholar]
- 15.Shanafelt TD, Dyrbye LN, West CP. Addressing physician burn-out: the way forward. JAMA. 2017;317(9):901–902. [DOI] [PubMed] [Google Scholar]
- 16.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences, and solutions. J Intern Med. 2018;283(6): 516–529. [DOI] [PubMed] [Google Scholar]
- 17.Lemaire JB, Wallace JE. Burnout among doctors. BMJ. 2017;358: j3360. [DOI] [PubMed] [Google Scholar]
- 18.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. [DOI] [PubMed] [Google Scholar]
- 19.Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout among health care professionals: a call to explore and address this under-recognized threat to safe, high-quality care NAM Perspectives. 2017. Discussion Paper, National Academy of Medicine, Washington, DC: https://nam.edu/burnout-among-health-care-professionals-a-call-to-explore-andaddress-this-underrecognized-threat-to-safe-high-quality-care. Accessed March 15, 2018. [Google Scholar]
- 20.McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff (Millwood). 2011;30(2):202–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016; 91(4):422–431. [DOI] [PubMed] [Google Scholar]
- 22.Wurm W, Vogel K, Holl A, et al. Depression-burnout overlap in physicians. Plos One. 2016;11(3):e0149913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12): 1826–1832. [DOI] [PubMed] [Google Scholar]
- 24.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–1721. [DOI] [PubMed] [Google Scholar]
- 25.Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38(5):223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2): 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmoldt R, Freeborn D, Klevit H. Physician burnout: recommendations for HMO managers. HMO Pract. 1994;8(2):58–63. [PubMed] [Google Scholar]
- 28.Waddimba AC, Scribani M, Nieves MA, Krupa N, May JJ, Jenkins P. Validation of single-item screening measures for provider burnout in a rural health care network. Eval Health Prof. 2016; 39(2):215–225. [DOI] [PubMed] [Google Scholar]
- 29.Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75–79. [Google Scholar]
- 30.Brenninkmeijer V, VanYperen N. How to conduct research on burnout: advantages and disadvantages of a unidimensional approach in burnout research. Occup Environ Med. 2003; 60(Suppl 1):i16–i20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. [DOI] [PubMed] [Google Scholar]
- 32.Homburg V, Heijden B, Valkenburg L. Why do nurses change jobs? An empirical study on determinants of specific nurses’ post-exit destinations. J Nurs Manag. 2013;21(6):817–826. [DOI] [PubMed] [Google Scholar]
- 33.Palda VA, Bowman KW, McLean RF, Chapman MG. “Futile” care: do we provide it? Why? A semistructured, Canada-wide survey of intensive care unit doctors and nurses. J Crit Care. 2005;20(3):207–213. [DOI] [PubMed] [Google Scholar]
- 34.Solomon MZ, O’Donnell L, Jennings B, et al. Decisions near the end of life: professional views on life-sustaining treatments. Am J Public Health. 1993;83(1):14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195–205. [DOI] [PubMed] [Google Scholar]
- 36.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. [DOI] [PubMed] [Google Scholar]
- 37.Thomas LR, Ripp JA, West CP. Charter on physician well-being. JAMA. 2018;319(15):1541–1542. [DOI] [PubMed] [Google Scholar]
- 38.Schwenk TL. Physician well-being and the regenerative power of caring. JAMA. 2018;319(15):1543–1544. [DOI] [PubMed] [Google Scholar]
- 39.Dykema J, Jones NR, Piche T, Stevenson J. Surveying clinicians by web: current issues in design and administration. Eval Health Prof. 2013;36(3):352–381. [DOI] [PubMed] [Google Scholar]
- 40.Kellerman SE, Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20(1):61–67. [DOI] [PubMed] [Google Scholar]