Abstract
Background/Aim: Postresective mandibular reconstruction is common in cases of oral and mandibular tumors. However, complications such as plate fracture and/or plate exposure can occur. The purpose of this study was to analyze complications and survival of reconstructive plates used to correct mandibular defects caused by oral cancer. Patients and Methods: Clinical and radiological data from 34 patients were analyzed. Only discontinuous mandibular defect cases were included in this study. All cases were classified using the Hashikawa’s CAT and Eichner’s classification methods. Then, we determined whether these classifications and clinical treatment methods were significantly related to complications. Results: Complications after mandibular reconstruction occurred in 10 of 34 patients, specifically, two plate fractures, one screw fracture, and seven plate exposures occurred. The plate fractures occurred 5 and 6 months after operation, and the screw fracture occurred 39 months after operation. Using the Hashikawa’s CAT classification, the two cases of plate fracture were one of AT type and the other of T type, and the screw fracture was AT type. Using Eichner’s classification, all three cases of plate and screw fractures were B2 type. Conclusion: We suggest that plate and screw fractures were caused by the type of mandibular defect and bite force.
Keywords: Reconstruction plate, mandibular defect
Large mandibular defects resulting from oral cancer, trauma, or osteoradionecrosis are common findings in the oral and maxillofacial area (1,2).
One purpose of the reconstruction of the mandible is the recovery of functions including occlusion, speech, breathing, feeding, and swallowing, and another is recovery of appearance (3-5). The choice of reconstructive options for an extensive defect remains controversial. The versatility of a double flap transfer for composite oromandibular defects has been reported by several authors (6-8). Meanwhile, some surgeons have concerns about the disadvantages of double flap transfer, including increased technical difficulty and surgical invasion (9,10). Thus, they choose a simpler procedure with a mandibular reconstruction plate and soft tissue coverage. Moreover, when donor bone cannot be harvested or the patient’s prognosis is poor, bone reconstruction may not be possible. In such cases, reconstruction plates can be used (11).
Since the early 1980s, the standard treatment for a mandibular discontinuity defect has been the use of a rigid reconstruction plate with concurrent or subsequent osseous reconstruction (12,13). Recently, the effectiveness of osteosynthesis has improved with the use of titanium reconstruction plates, which provide better biocompatibility, and locking screws for biochemical improvement (12). However, postoperative plate-related complications, including plate exposure, plate fracture, and infection still occur occasionally. These complications require the removal of the reconstruction material. Therefore, we examined the survival of cases utilizing reconstruction plates and aimed to evaluate the factors associated with postoperative complications.
Patients and Methods
We performed a retrospective analysis of 34 cases of mandibular reconstruction with reconstruction plates after segmental mandibulectomy from 1992 to 2011 at Nagasaki University Hospital in Japan. The patients underwent a surgical operation and reconstruction plates were used to correct the mandibular discontinuity defect. The surgical procedures were performed while the patients were under general anesthesia. Clinical data on the area of the mandibular defect, the number of screws in the palate, and occlusal pattern were evaluated. The complications associated with the reconstruction plates of the mandible were also determined. Furthermore, comparison of the cases with and without complications were analyzed according to gender, age, occlusal pattern, location of defect, and the number of screws.
The defects of mandibles were analyzed using Hashikawa’s CAT classification (14) and occlusal patterns were analyzed using Eichner’s index. In the CAT classification system, “C” refers to defects in the condylar head of the mandible, “A” refers to defects in the mandibular angle, and “T” refers to defects in the mental tubercle. In Eichner’s classification system (15), patients are classified into one of six groups based on the presence or absence of occlusal contacts in the premolar and molar region.
Results
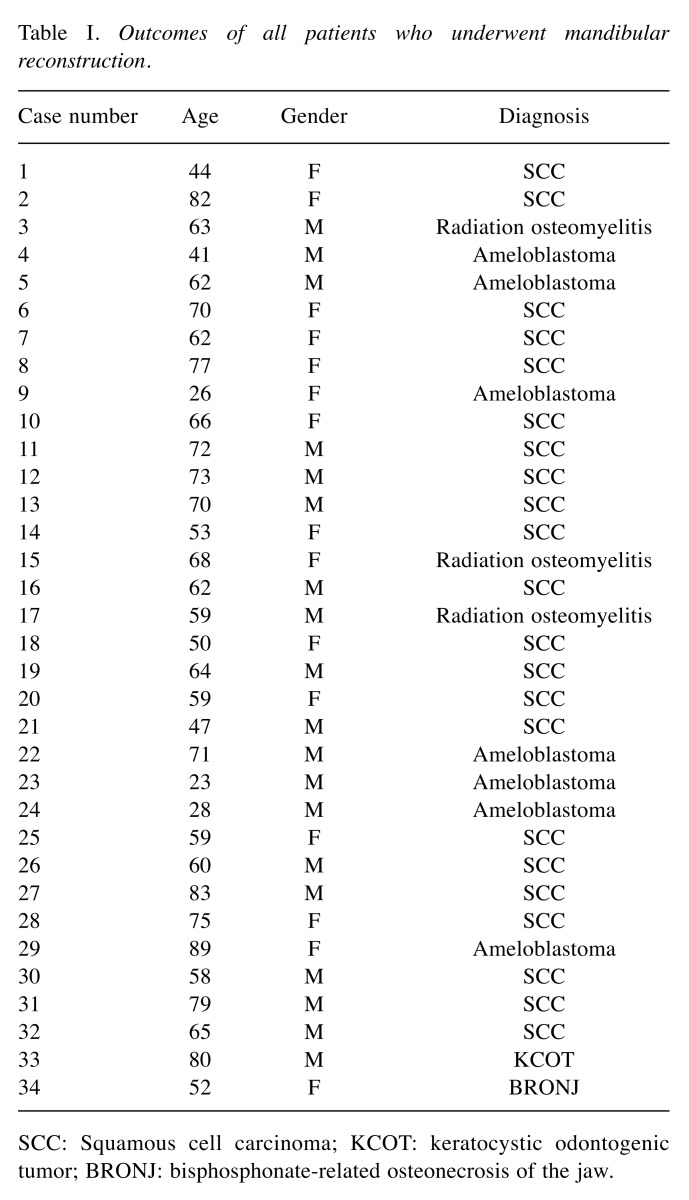
The patients were 19 men and 15 women aged 23 to 89 years (median age, 60 years). They had different diagnoses, including malignant tumor (n=22), benign tumor (n=8), osteoradionecrosis (n=3), and bisphosphonate-related osteonecrosis of the jaw (BRONJ) (n=1) (Table I). Titanium reconstruction plates were used in all cases. The mean number of screws in the palate was eight (range=7-9 screws). In four patients, two types of soft tissue flap (DP flap and PMMC flap) were used, whereas a simple closure was used in the remaining patients.
Table I. Outcomes of all patients who underwent mandibular reconstruction.
SCC: Squamous cell carcinoma; KCOT: keratocystic odontogenic tumor; BRONJ: bisphosphonate-related osteonecrosis of the jaw.
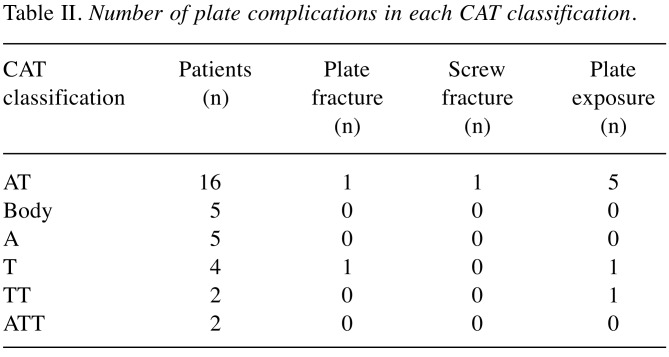
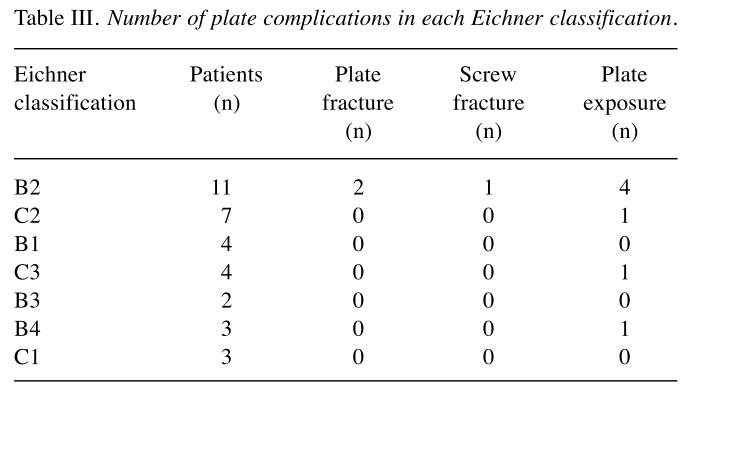
The distributions of cases according to the CAT and Eichner’s classification methods are shown in Tables Ⅱ and Ⅲ, respectively. Among all patients, AT type was the most frequently observed CAT classification, and B2 type was the most frequently observed Eichner’s classification.
Complications. Postoperative plate-related complications occurred in 10 patients (two plate fractures, one screw fracture, and seven plate exposures), who then underwent plate removal. The plate-related complication occurred from 1 to 39 months after operation (mean 7.2 months).
These patients included four men and six women, and their mean age was 60 years (range=44-79 years).
There were no significant differences between the patients with and without complications in terms of gender and age.
Plate exposure. The cases of plate exposure included one case of intraoral exposure and six cases of extraoral exposure. The case of intraoral exposure was diagnosed as BRONJ. The exposure was observed from 1 to 9 months after operation.
The types of soft tissue flap included DP flap (n=2) and PMMC (n=2), and in the two cases where a DP flap was used, plate exposure occurred.
Using the CAT classification, five cases were AT type, one case was T type, and one case was TT type. Using Eichner’s classification, the seven cases of plate exposure comprised four cases of B2 type and one case each of B4, C2, and C3 type.
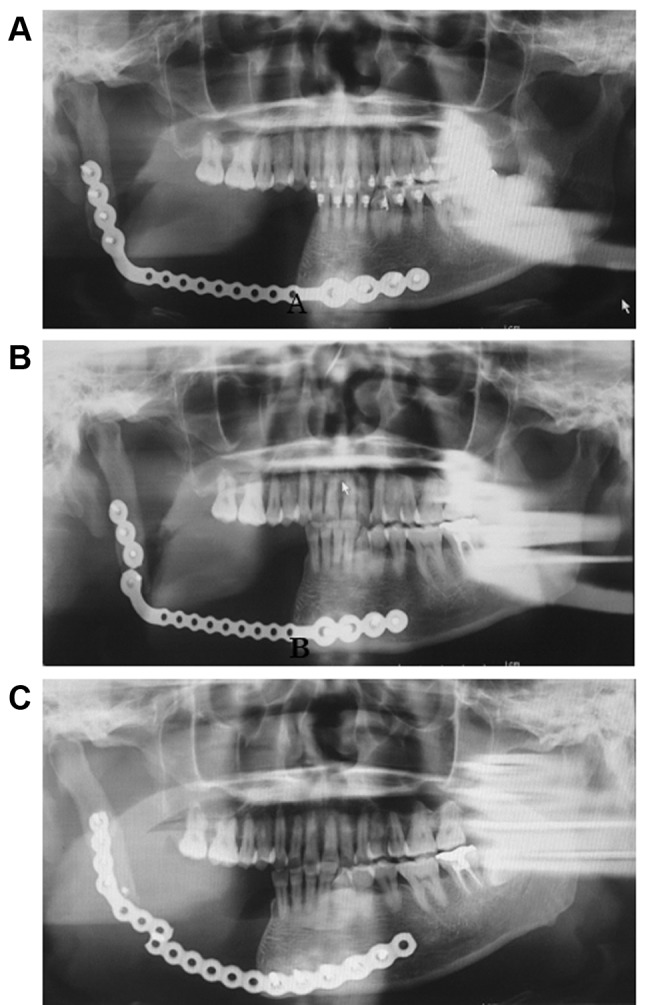
Plate-related fracture. Two cases of plate fracture and one case of screw facture were observed. The plate fractures occurred 5 and 6 months after operation (Figure 1), and the screw fracture occurred 39 months after operation. Using the CAT classification, the two cases of plate fracture were of AT type and T type, and the case with screw fracture was AT type. Using Eichner’s classification, all three cases of plate and screw fractures were B2 type.
Figure 1. Panoramic radiography. The segmental dissection of the mandible and reconstruction of the defect by the plate (malignant tumor, case No.30). A: 1 week after operation B: 5 months after operation. C: 6 months after re-operation.
Discussion
The success rate of mandibular reconstruction has increased as a result of advances in plate design and materials (16-18). However, plate-related complications still develop frequently and can sometimes cause serious problems for patients (12). In our series, complications of the reconstruction plate comprised plate exposure, plate fracture, and screw fracture.
There are numerous factors contributing to plate exposure (19), including; persistence of dead space below the plate, thin soft tissue over the plate surface, imbalance between soft tissue on the plate surface and the form of the plate, extent of mandibular resection, dead space due to displacement between the plate and the surrounding tissue, effects of radiation therapy, necrosis of soft tissue surrounding a plate, and allergy to metal. In our series, plate exposures occurred in two cases where a DP flap was used and in two cases where a PMMC flap was used. Furthermore, all cases of plate exposure were in thin patients with little fatty tissue on the skin over the mandible. The DP flaps consisted of thin soft tissue and it was difficult to diminish the dead space between the soft tissue and the reconstruction plate. Hence, we suggest that for soft tissue used with the reconstruction plate is preferable to use a voluminous flap, and the surgical technique needs to diminish the dead space between the reconstruction plate and the soft tissue.
In our case series, there were two cases of plate fracture and one case of screw fracture. There are some possible causes of complications of mandibular reconstructions, including, bite force, excessive intraoperative bending of the reconstruction plate, the type of mandibular defect, and infections.
Concerning mechanical stresses, Shibahara et al. (11) have reported that plate fractures due to mechanical stress occurred in eight of 110 patients who underwent reconstruction after resection of the mandibular angle. Furthermore, Boyd et al. (20) have shown that bite force affected both the mechanical stress on reconstruction plates and the success rate of reconstructive surgery. Sakakibara et al. (11) reported that mandibular angle defects and B2+B3+B4 occlusions are significantly related to plate fractures, and suggested that these fractures may be due to bite force or mechanical limitations of reconstruction plates. In our present study, using the CAT classification, the cases of plate fracture were one of AT type and the other of T type, and the case of screw fracture was AT type. Using Eichner’s classification, all three cases of plate and screw fractures were B2 type. We also suggested in the present study that bite force and the type of mandibular defect were the causes of plate fracture.
In conclusion, the usage of reconstruction plates for the mandibular defects needs to consider the mechanical stress on the plate, and the surgical technique for both the plate and soft tissue is important.
Conflicts of Interest
The Authors have stated explicitly that there are no conflicts of interests in connection with this article.
Table 2. Number of plate complications in each CAT classification.
Table 3. Number of plate complications in each Eichner classification.
References
- 1.Wu CH, Lin YS, Liu YS, Lin CL. Biomechanical evaluation of a novel hybrid reconstruction plate for mandible segmental defects; A finite element analysis and fatigue testing. J Cranio Maxillofac Surg. 2017;45:1671–1680. doi: 10.1016/j.jcms.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 2.Zhao L, Shang H, Chen X, Liu Y. Biomechanical analysis of a curvilinear distractor device for correcting mandibular symphysial defects. J Oral Maxillofac Surg. 2014;72:1158–1167. doi: 10.1016/j.joms.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Okoturo E, Ogunbanjo O, Akinleye A. Quality of life of patients with segmental mandibular resection and immediate reconstruction with plates. J Oral Maxillofac Surg. 2011;69:2253–2259. doi: 10.1016/j.joms.2010.10.043. [DOI] [PubMed] [Google Scholar]
- 4.Hassan SJ, Weymuller EA. Assessment of quality of life in head and neck cancer. Head Neck. 1993;15:485–496. doi: 10.1002/hed.2880150603. [DOI] [PubMed] [Google Scholar]
- 5.Young CW, Pogel MA, Schmidt BI. Quality of life in patients undergoing segmental mandibular resection and staged reconstruction with nonvasculized bone graft. J Oral Maxillofac Surg. 2007;65:706–712. doi: 10.1016/j.joms.2006.05.064. [DOI] [PubMed] [Google Scholar]
- 6.Miyamoto S, Sakuraba M, Nagamatsu S, Kamizono K, Hayashi R. Comparison of reconstruction plate and double flap for reconstruction of an extensive mandibular defect. Microsurgery. 2012;32:452–457. doi: 10.1002/micr.21976. [DOI] [PubMed] [Google Scholar]
- 7.Hanasono MM, Weinstock YE, Yu P. Reconstruction of extensive head and neck defects with multiple simultaneous free flaps. Plast Reconstr Surg. 2008;122:1739–1746. doi: 10.1097/PRS.0b013e31818a9afa. [DOI] [PubMed] [Google Scholar]
- 8.Nakatsuka T, Harii K, Yamada A, Ueda K, Ebihara S. Dual free flap transfer using forearm flap for mandibular reconstruction. Head Neck. 1992;14:452–458. doi: 10.1002/hed.2880140605. [DOI] [PubMed] [Google Scholar]
- 9.Davidson J, Boyd B, Gullane P, Rostein L, Freeman J, Manktelow R, Rosen I. A comparison of the results following oromandibular reconstruction using a radial forearm flap with either radial bone or a reconstruction plate. Plast Reconstr Surg. 1991;88:201–208. doi: 10.1097/00006534-199108000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Irish JC, Gullane PJ, Glbert RW, Brown DH, Birt BD, Boyd JB. Primary mandibular reconstruction with the titanium hollow screw reconstruction plate: evaluation of 51 cases. Plast Reconstr Surg. 1995;96:93–99. doi: 10.1097/00006534-199507000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Sakakibara A, Hashikawa K, Yokoo S, Sakakibara S, Komori T, Tahara S. Risk factors and surgical refinements of postresective mandibular reconstruction: a retrospective study. Plast Surg Int. 2014;2014:893746–893746. doi: 10.1155/2014/893746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seol GJ, Jeon EG, Lee JS, Choi SY, Kim JW, Kwon TG, Paeng JY. Reconstruction plates used in the surgery for mandibular discontinuity defect. J Korean Assoc Oral Maxillofac Surg. 2014;40:266–271. doi: 10.5125/jkaoms.2014.40.6.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peacock ZS, Afshar S, Lukas SJ, Kaban LB. Customized repair of fractured mandibular reconstruction plates. J Oral Maxillofac Surg. 2012;70:563–573. doi: 10.1016/j.joms.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Hashikawa K, Yokoo S, Tahara S. Novel classification system for oncological mandibular defect: CAT classification. Jpn J Head Neck Cancer. 2008;34:412–418. [Google Scholar]
- 15.Eichner K. A group classification of missing teeth for prostho-dontics. Deutsche Zahnarztliche Zeitschrift. 1955;10:1831–1834. [Google Scholar]
- 16.Rendenbach C, Sellenschloh K, Gerbig L, Morlock MM, Beck-Broichsitter B, Smeets R, Heiland M, Huber G. CAD-CAM plates versus conventional fixation plates for primary mandibular reconstruction: a biomechanical in vitro analysis. J Cranio Maxillofac Surg. 2017;45:1878–1883. doi: 10.1016/j.jcms.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 17.Herford AS, Ellis E. Use of a locking reconstruction bone plate/screw system for mandibular surgery. J Oral Maxillofac Surg. 1998;56:1261–1265. doi: 10.1016/s0278-2391(98)90605-x. [DOI] [PubMed] [Google Scholar]
- 18.Schoning H, Emshoff R. Primary temporary AO plate reconstruction of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:667–672. doi: 10.1016/s1079-2104(98)90201-3. [DOI] [PubMed] [Google Scholar]
- 19.Onoda S, Kimata Y, Yamada K, Sugiyama N, Onoda T, Eguchi M, Mizukawa N. Prevention points for plate exposure in the mandibular reconstruction. J Cranio Maxillofac Surg. 2012;40:310–314. doi: 10.1016/j.jcms.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 20.Boyd JB. Use of reconstruction plates in conjunction with soft-tissue free flaps for oromandibular reconstruction. Clin Plast Surg. 1994;21:69–77. [PubMed] [Google Scholar]