Abstract
Background: There is no general consensus regarding the best and most accurate method for assessing the size of implant required for achieving the best symmetry in oncoplastic reconstruction. Materials and Methods: Breast weight, volume and size of implant were recorded prospectively on patients undergoing immediate reconstruction over a 3-year period. Cases with specimen size greater than 2,000 g were excluded. The primary endpoint was size of implant used in relation to specimen weight and volume. Secondary endpoints were the influence of age and histology on specimen weight, volume and breast density. Results: A total of 278 mastectomies were performed. Correlation of implant size with volume was marginally stronger than that with weight (r=81%, p<0.001 vs. r=78.9%, p<0.001 respectively). Women aged 50 years and above had lower breast weight for the same breast volume than women under 50 years. The difference was merely 4%, but was statistically significant (p=0.001). Histology had no statistically significant influence on breast density. Conclusion: Specimen weight and volume were found to be closely correlated. Weight can be measured more accurately and easily with reproducible readings compared to volume.
Keywords: Mastectomy, breast, breast density, body weight
Reconstruction surgery is increasingly offered to women undergoing mastectomy. Implant reconstruction with acellular dermal matrix has gained popularity in recent years compared to pedicle and free flap reconstructions (1). There is no general consensus as to what the best and most accurate method of assessing the size of implant to be used in order to achieve desirable result in terms of symmetry. Some surgeons use the volume of mastectomy specimen to determine the implant size, whilst others use specimen weight (2). There are very few published reviews on this topic.
This study examined the relation of mastectomy specimen weight and volume with implant size in order to better inform intra-operative decision-making regarding implant selection.
Materials and Methods
Data were collected prospectively on patients who underwent mastectomy at the London Breast Institute. Breast weight, volume measurement and size of implant were recorded if immediate reconstruction was chosen. Patients were under the care of two senior oncoplastic breast surgeons from January 2014 to December 2016. The exclusion criteria included patients with mastectomy specimen weighing more than 2,000 g. The volume of breast tissue was measured by volume displacement method. The weight of breast tissue was measured on a scale in grams.
The primary endpoint studied was size of implant used in relation to mastectomy specimen weight and volume. Secondary endpoints were the influence of age on specimen weight and volume relation; the influence of the presence of invasive cancer, ductal carcinoma in situ (DCIS) on weight and volume relation, and breast weight to volume ratio (BWV, i.e. breast tissue density).
These variables were analysed using regression, two-sample t-test, Pearson’s correlation test, and Wald test as appropriate.
Results
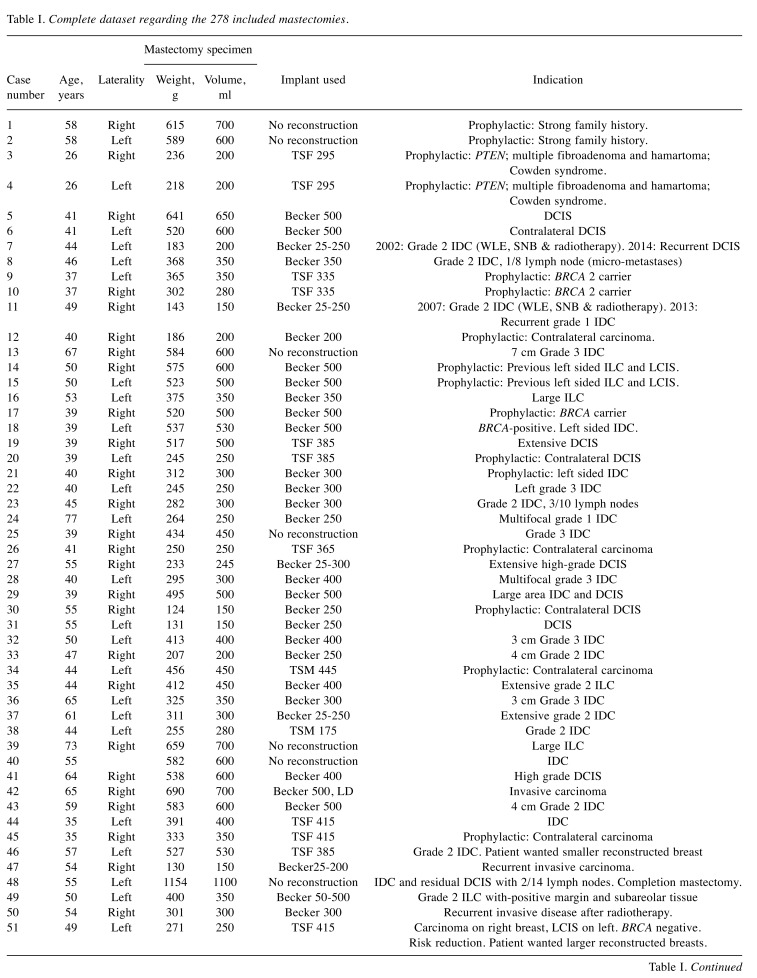
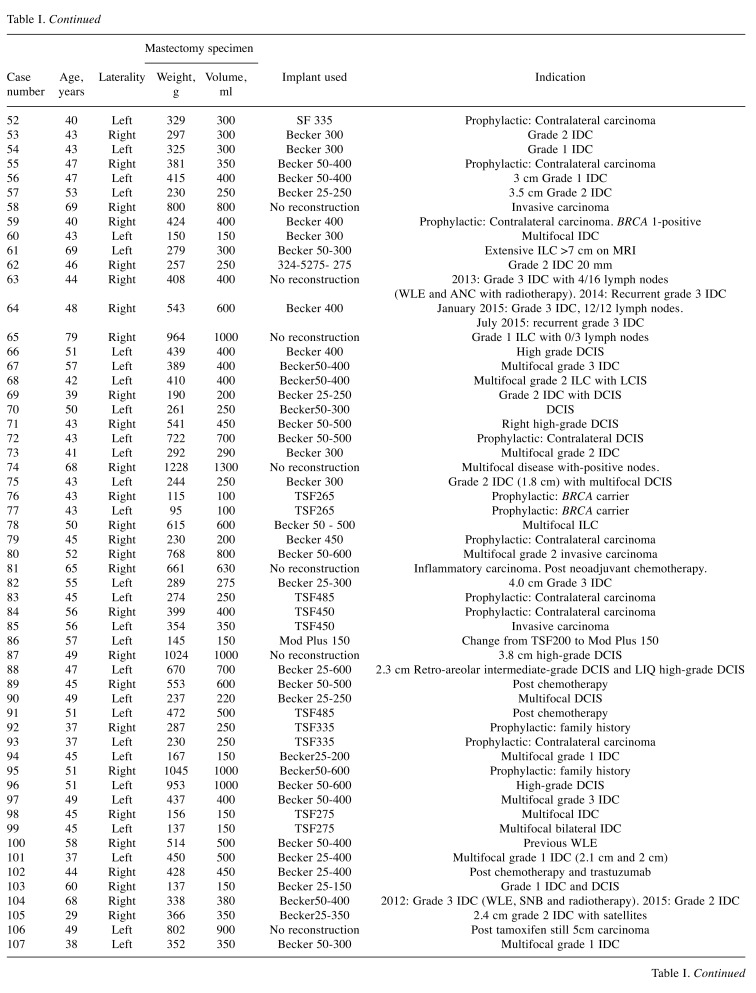
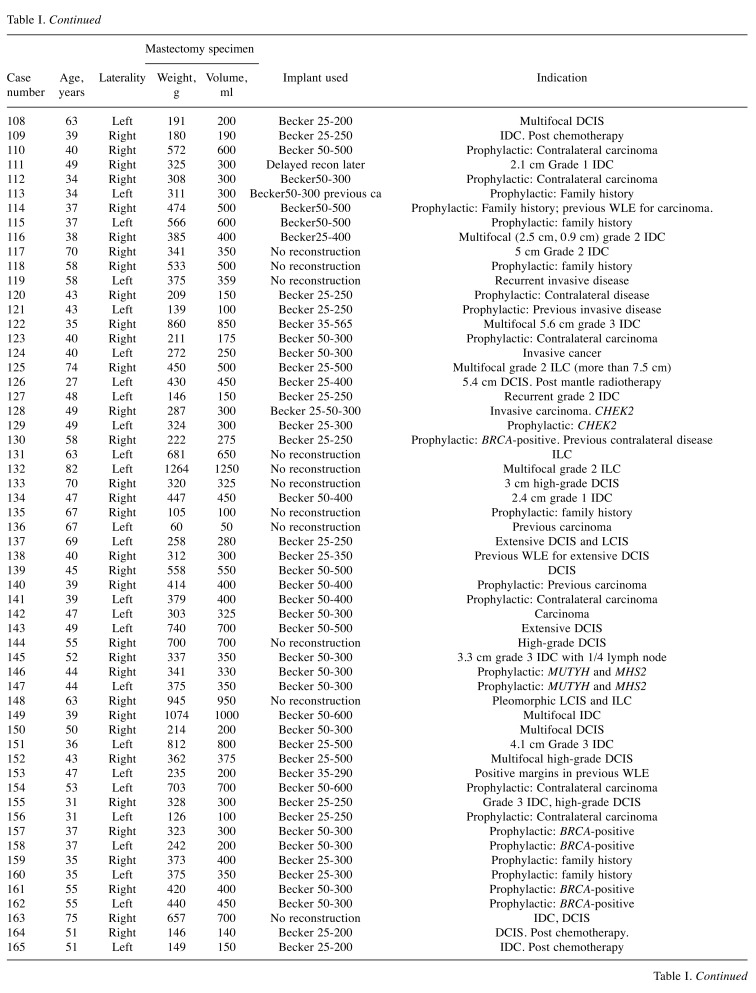
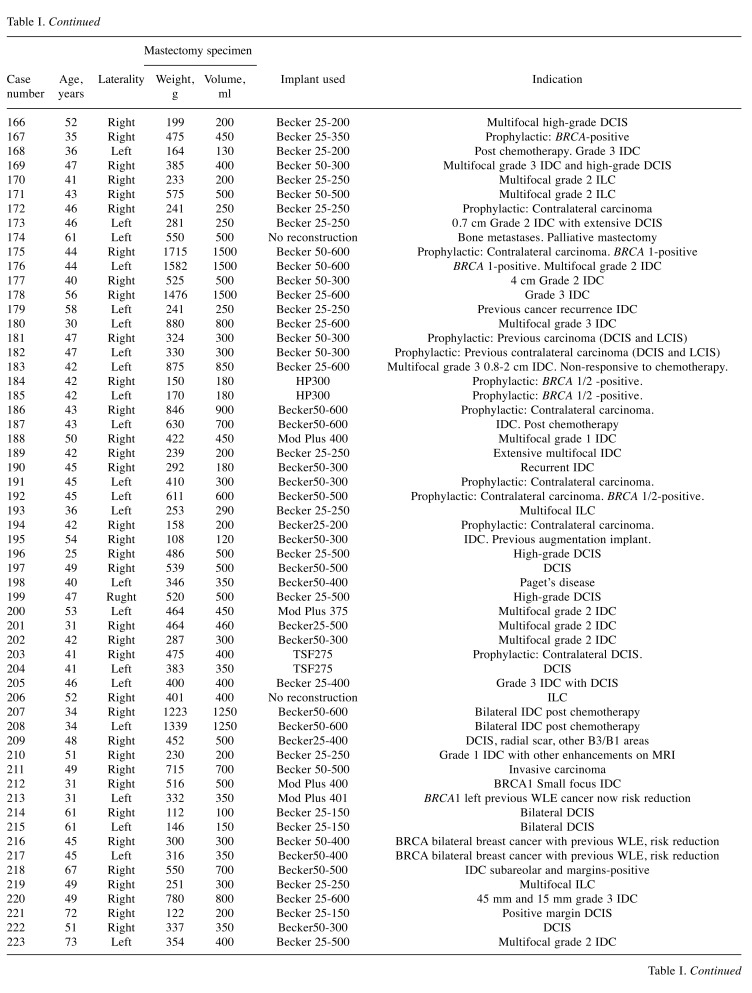
A total of 278 operations were performed on 221 women, of whom 53 had bilateral mastectomies (N=278). The mean age of women was 48 years (range=24-90 years). There were 150 right and 128 left breast specimens. The complete dataset is presented in Table I.
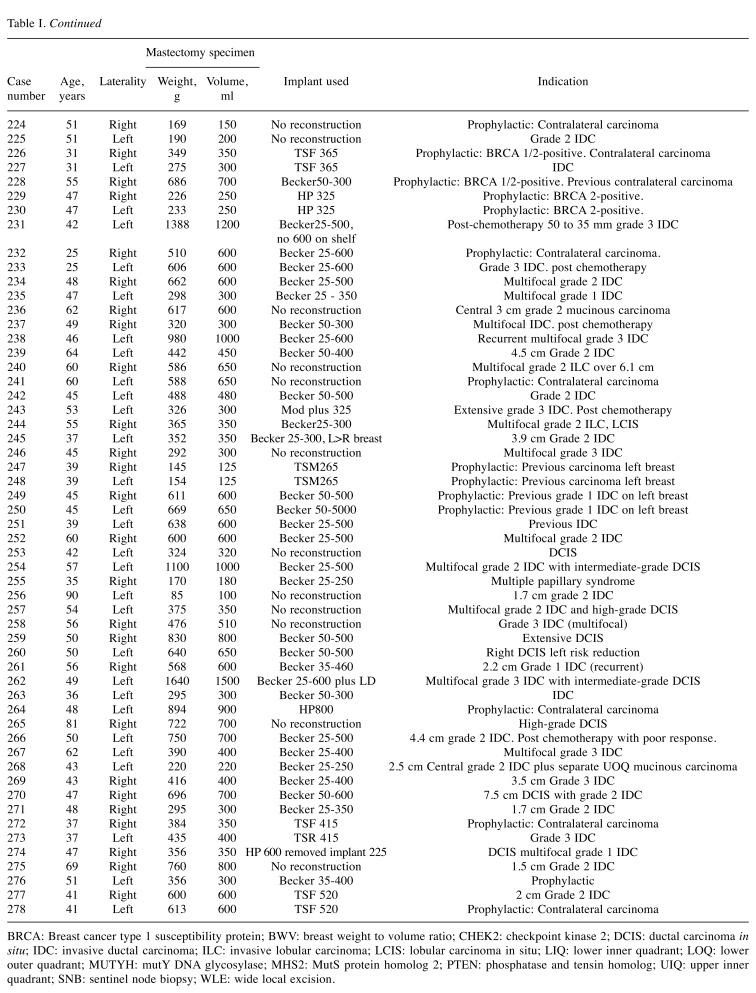
Table I. Complete dataset regarding the 278 included mastectomies.
BRCA: Breast cancer type 1 susceptibility protein; BWV: breast weight to volume ratio; CHEK2: checkpoint kinase 2; DCIS: ductal carcinoma in situ; IDC: invasive ductal carcinoma; ILC: invasive lobular carcinoma; LCIS: lobular carcinoma in situ; LIQ: lower inner quadrant; LOQ: lower outer quadrant; MUTYH: mutY DNA glycosylase; MHS2: MutS protein homolog 2; PTEN: phosphatase and tensin homolog; UIQ: upper inner quadrant; SNB: sentinel node biopsy; WLE: wide local excision.
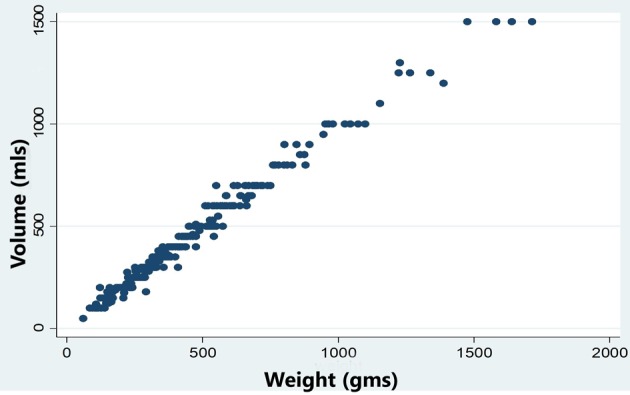
Relation between breast weight and volume. There was strong positive linear relation between breast weight and volume (r=99.07, p<0.001) (Figure 1). The R-squared parameter of the regression suggested that 98.1% of the variation in weight was explained by the variation in volume.
Figure 1. Scatter plot of mastectomy specimen weight vs. volume.
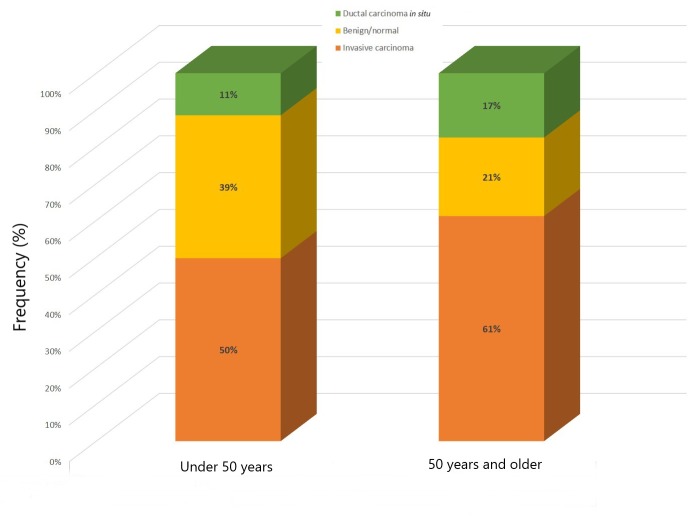
Influence of histology on BWV. The population was stratified into groups based on histology: Invasive carcinoma, DCIS and benign histology (Figure 2). These were compared for differences in BWV. Different tests led to the conclusion that histology had no statistically significant influence on breast density.
Figure 2. Stratification of histology by age group.
Influence of age on breast weight, volume and BWV. Breast weight, volume and BWV were studied in patients above and below the age of 50 using regression analysis and the Student’s t-test.
In this population, no statistically significant correlation was seen for breast weight by age group. However, women at an age of 50 years and above had lower breast weight for the same breast volume than women under 50 years of age. The difference was merely 4%, but was statistically significant (p=0.001).
Analysis of the correlation of age with BWV confirmed this finding. We found that women at an age of 50 years and over had a lower breast weight for the same breast volume than women under 50 years of age (p=0.0001). This was confirmed by regression analysis. R-Squared of the regression suggested that age would account for 5.3% of variation in BWV.
Implant size used in relation to breast weight and volume. Correlation of implant size with volume was marginally stronger than that with weight (r=81%, p<0.001 vs. r=78.9%, p<0.001, respectively).
Discussion
Mastectomy specimen weight and volume are fairly closely correlated. The presence of cancer whether in the form of invasive disease or DCIS did not seem to affect the correlation between weight and volume of the breast tissue. The weight can be measured more accurately easily with repeated readings on a scale, whereas volume measurement is best estimated to the nearest 25-50 cc. However, there are many other factors in deciding the type and size of implant, including whether to use a fixed volume or expandable prosthesis. Patient preference regarding size, and the limits of commercial availability of implants of certain sizes are also crucial considerations.
However, age is an important factor in the relation between weight and volume. A higher age results in lower breast weight for the same volume. On average, specimens from women after 50 years of age, taken arbitrarily as the age of menopause, were found to have about 4% lower weight than those from woman under 50 with the same breast volume. This fits with the general belief that younger breasts have denser glandular breast tissue.
The potential role of breast imaging modalities such ultrasonography, computed tomography and magnetic resonance imaging in predicting breast volume preoperatively has been investigated with variable results (3). Ultrasound has the limitation of reduced objectivity and reproducibility. Computed tomography involves radiation exposure and in the supine position does not reflect breast geometrics accurately. Magnetic resonance imaging assessment of breast volume has demonstrated a significant correlation with actual breast weight, with breast density influencing the correlation (3).
The correlation between the intraoperative breast specimen weight and volume was previously investigated by other authors (4,5). Parmar et al. reported non-significant difference of 6.6% between the weight of intraoperative breast specimens and volume, with the difference being smaller in postmenopausal women most likely due to lower breast density in this group. The study was relatively small (69 specimens) and predominantly included breast reduction specimens (4). Lee and colleagues designed equations to calculate the breast volume on the basis of the breast weight, incorporating adjustment for breast density (5).
The strength of our study arises from using adequate sample size, use of intraoperative mastectomy specimens and presence of malignant pathology, which represents the most common indication for mastectomy. The main limitation is the lack of data regarding breast density, where the fibroglandular-to-adipose ratio might affect the correlation. Furthermore, our methodology does not provide a means of predicting breast volume preoperatively in order to guide reconstructive surgery planning.
We utilized our simple approach in selecting the best implant for breast reconstruction following skin-sparing mastectomy after carrying out an adjustment for the use of SurgiMend™ (Integra Life Sciences, Plainsboro, NJ, USA), a foetal bovine acellular dermal matrix (ADM) with the following dimensions: 16 cm × 8 cm × 0.1 cm. The volume of the ADM after integration was estimated to be 32 cc, assuming an additional thickness of 1.5 mm of granulation tissue. The required implant size was, therefore, calculated as follows:
Volume of implant=mastectomy weight (g) - 32
We previously reported an excellent subjective patient satisfaction and objective independent aesthetic assessment scores (9 out of 10) after oncoplastic breast reconstruction (6,7). We are currently extrapolating our methodology to the evolving technique of pre-pectoral ADM-assisted implant-based immediate breast reconstruction following skin-sparing mastectomy (8).
In conclusion, our study provides evidence that intraoperative measurement of the weight of mastectomy specimens accurately reflects the breast volume and this simple approach can be used to guide implant selection during breast reconstruction.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The data in this manuscript were presented in a poster at the San Antonio Breast Cancer Symposium on Dec-8, 2017.
Conflicts of Interests
The Authors have no conflicts of interest to report pertaining to this study. The Senior Author (KM) provides clinical and academic advisory sevices to Q Medical Technologies.
Acknowledgements
The Authors would like to thank Ivanna Naumets for her help with the statistical analysis.
References
- 1.Sbitany H, Piper M, Lentz R. Prepectoral breast reconstruction: A safe alternative to submuscular prosthetic reconstruction following nipple-sparing mastectomy. Plast Reconstr Surg. 2017;140(3):432–443. doi: 10.1097/PRS.0000000000003627. [DOI] [PubMed] [Google Scholar]
- 2.Baek WY, Byun IH, Kim YS, Lew DH, Jeong J, Roh TS. Patient satisfaction with implant based breast reconstruction associated with implant volume and mastectomy specimen weight ratio. J Breast Cancer. 2017;20(1):98–103. doi: 10.4048/jbc.2017.20.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoo A, Minn KW, Jin US. Magnetic resonance imaging-based volumetric analysis and its relationship to actual breast weight. Arch Plast Surg. 2013;40(3):203–208. doi: 10.5999/aps.2013.40.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parmar C, West M, Pathak S, Nelson J, Martin L. Weight versus volume in breast surgery: An observational study. JRSM Short Rep. 2011;2(11):87. doi: 10.1258/shorts.2011.011070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee JH, Yeo CH, Kim T, Chung KJ, Lee SJ, Kang SH, Choi JE. Conversion from weight to volume of mastectomy specimen: Convenient equations. J Plast Reconstr Aesthet Surg. 2017;70(6):792–794. doi: 10.1016/j.bjps.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Headon H, Kasem A, Manson A, Choy C, Carmichael AR, Mokbel K. Clinical outcome and patient satisfaction with the use of bovine-derived acellular dermal matrix (surgimend) in implant based immediate reconstruction following skin sparing mastectomy: A prospective observational study in a single centre. Surg Oncol. 2016;25(2):104–110. doi: 10.1016/j.suronc.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 7.El Hage Chehade H, Headon H, Wazir U, Carmaichael AR, Choy C, Kasem A, Mokbel K. Nipple-sparing mastectomy using a hemi-periareolar incision with or without minimal medial-lateral extensions; clinical outcome and patient satisfaction: A single centre prospective observational study. Am J Surg. 2017;213(6):1116–1124. doi: 10.1016/j.amjsurg.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 8.Wazir U, Mokbel K. The evolving role of pre-pectoral adm-assisted implant-based immediate breast reconstruction following skin-sparing mastectomy. Am J Surg. 2018;216(3):639–640. doi: 10.1016/j.amjsurg.2018.01.021. [DOI] [PubMed] [Google Scholar]