Abstract
Objectives:
The primary objective of this study was to examine associations between depression and several measures of health behaviour change across 8 cycles of a population-based, cross-sectional survey of Canadians. The secondary objective of this study was to describe the prevalence of the types of health behaviour changes undergone/sought and types of barriers to change reported, comparing those with and without depression.
Methods:
The sample comprised 65,801 respondents to the Canadian Community Health Survey between 2007 and 2014. Past-year depression was assessed via structured interview (CIDI-SF). Measures of health behaviour change included recent changes made, desire to make changes, and barriers towards making changes. Analyses involved logistic regression, with estimates across cycles pooled using fixed-effects meta-analyses. Pooled prevalences of types of health behaviour changes undergone/sought and types of barriers to change experienced were reported, and associations with depression were examined.
Results:
Depression was associated with higher odds of reporting a recent health behaviour change (pooled odds ratio [OR] = 1.39; 95% confidence interval [CI], 1.30 to 1.48), desire to make health behaviour changes (pooled OR = 1.61; 95% CI, 1.49 to 1.74), and barriers towards change (pooled OR = 1.54; 95% CI, 1.44 to 1.65). The most common change undergone and sought was increased exercise; the most common barrier reported was a lack of willpower.
Conclusions:
Individuals dealing with depression are more likely to report recent health behaviour changes and the desire to make changes but are also more likely to report barriers towards change.
Keywords: depression, health behaviours, behaviour change
Abstract
Objectifs :
Le principal objectif de cette étude était d’examiner les associations entre la dépression et plusieurs mesures du changement de comportement de santé dans les huit cycles de l’enquête transversale dans la population des Canadiens. L’objectif secondaire de l’étude était de décrire la prévalence des types de changements de comportement de santé vécus/recherchés, et les types d’obstacles au changement déclarés, en comparant ceux-ci avec et sans la dépression.
Méthodes :
L’échantillon comprenait 65 801 répondants de l’Enquête sur la santé dans les collectivités canadiennes entre 2007 et 2014. La dépression de l’année précédente a été évaluée par une entrevue structurée (CIDI-SF). Les mesures du changement de comportement de santé incluaient: changements faits récemment, désir de faire des changements, et obstacles à l’exécution de changements. Les analyses comprenaient la régression logistique, avec des estimations dans les cycles regroupés à l’aide de méta-analyses d’effets fixes. Les prévalences combinées des types de changements de comportement de santé vécus/recherchés, et des types d’obstacles au changement rencontrés ont été déclarées, et les associations à la dépression ont été examinées.
Résultats :
La dépression était associée à des probabilités élevées de déclarer un récent changement de comportement de santé (rapports de cotes regroupés [RC] = 1,39; intervalle de confiance (IC) à 95% 1,30 à 1,48), un désir de faire un changement de comportement de santé (RC regroupés = 1,61; IC à 95% 1,49 à 1,74), et des obstacles au changement (RC regroupés = 1,54; IC à 95% 1,44 à 1,65). Le changement vécu et recherché le plus commun était plus d’exercice; l’obstacle déclaré le plus souvent était le manque de volonté.
Conclusions :
Les personnes aux prises avec la dépression sont plus susceptibles de déclarer de récents changements de comportement de santé et le désir de faire des changements, mais elles sont aussi plus susceptibles de faire état des obstacles au changement.
Depression is highly prevalent and carries significant burden at both the individual and societal levels. Estimates suggest that 12% to 16% of individuals will experience a major depressive episode at some point in their lives1,2; onset is often early in life, and recurrence is common.3 Worldwide, depression is one of the leading causes of years lived with a disability and disability-adjusted life years.4 By 2020, the World Health Organization projects that major depressive disorder will be the second leading cause of disability worldwide.5
An emerging body of evidence demonstrates bidirectional associations between depression and poor health behaviours, including low diet quality, smoking, and reduced physical activity.6–9 Depression is also linked to poor physical health outcomes, ranging from obesity and type II diabetes to cardiovascular disease.10–12 Like depression, the economic and societal burden of poor health behaviours, obesity, and chronic physical illness is significant. Their interplay with depression can ultimately lead to the propagation of poor mental and physical health throughout the life span, and when considered together, the combined burden of experiencing depression and poor physical health can be staggering. Large-scale studies examining lifestyle modification (i.e., positively shifting health behaviours) in at-risk groups have had promising results in reducing the incidence of chronic physical illnesses, including type II diabetes and coronary heart disease.13,14 As a result, health behaviour modification may represent an appealing target of prevention and intervention efforts to reduce the burden of poor health in those experiencing or at risk for depression.
Understanding efforts to modify poor health behaviours can provide important information for the development of initiatives targeted at improving the health of those with depression. Population-level examinations into health behaviour changes are common in those with poor physical health, particularly in those experiencing obesity. Research by Gregory and colleagues,15 for example, suggested that over half of obese individuals reported active efforts to lose weight, with the odds of reporting efforts to lose weight higher in women than in men. However, studies examining health behaviour change in those dealing with depression are often restricted to those experiencing physical comorbidities.16,17 There is a dearth of research describing population-level associations between depression and health behaviour change independent of physical health status.
In the current study, we examined the associations between depression and several measures of health behaviour change across 8 cycles of a population-based, cross-sectional survey of Canadians. In particular, we examined associations between depression and (1) undertaking a recent health behaviour change, (2) reporting the desire to make health behaviour changes, and (3) reporting barriers to health behaviour change. Secondarily, we also described the prevalence of the types of health behaviour changes undergone, the types of health behaviour changes sought, and the types of barriers to change reported, comparing those with and without depression.
Methods
Participants
Data for this study came from the Canadian Community Health Survey (CCHS),18 a repeated cross-sectional survey conducted by Statistics Canada on participants 12 years and older to collect information on health status, access to and use of health services, and determinants of health. Individuals were excluded from data collection if they lived on aboriginal reserves or certain remote areas, were full-time employees of the Canadian Armed Forces, or were members of institutionalized populations (approximately 3% of the Canadian population). The survey includes core content, asked to respondents in all regions, and optional content, asked to respondents in certain regions. Data across 8 annual cycles was examined using 4 data sets comprising the 2007-2008, 2009-2010, 2011-2012, and 2013-2014 annual cycles of the CCHS. Because the depression and health behaviour change modules were optional content, samples were restricted to the provinces and territories with participant data on all study variables. Eligible participants for the current study included those 18 years and older with complete data on study variables. The 2007-2008 sample included respondents from Nova Scotia, New Brunswick, Quebec, Alberta, Yukon Territories, and Nunavut (n = 34,010). The 2009-2010 sample included respondents from Prince Edward Island and British Columbia (n = 11,653). The 2011-2012 sample included respondents from Prince Edward Island, Newfoundland and Labrador, and Nova Scotia (n = 8217). Finally, the 2013-2014 sample included respondents from Prince Edward Island, Nova Scotia, Manitoba, and the Northwest Territories (n = 11,921), yielding a total sample of 65,801 participants from 2007 to 2014. No ethics approval was required for this study; data used are legally accessible to the public and protected by Canadian law.
Measures
Depression was defined as having experienced a major depressive episode in the past 12 months, assessed using the World Health Organization’s Composite International Diagnostic Interview–Short Form (CIDI-SF).19 Sensitivity and specificity of CIDI-SF scales compared to CIDI diagnoses are 89.6% and 93.9%, respectively.19 The CIDI-SF yields scores that give predicted probabilities of depression, whereby those with predicted probabilities of 90% or greater (a score of 5 or greater on a scale of 0 to 8) were categorized as having experienced a major depressive episode in the past 12 months. This corresponds with meeting DSM-IV criteria for a major depressive disorder.20
Three measures of health behaviour change were used. First, eligible respondents were asked to answer the question, “In the past 12 months, did you do anything to improve your health?” Those who answered “yes” were categorized as having made a recent health behaviour change. Second, eligible respondents were asked to answer the question, “Do you think there is anything you should do to improve your physical health?” Those who answered “yes” were categorized as having the desire to make a health behaviour change. Finally, if respondents answered positively to having the desire to make a health behaviour change, they were then asked, “Is there anything stopping you from making this improvement?” Those who answered “yes” were categorized as reporting barriers to making a health behaviour change.
Respondents who reported a recent health behaviour change or the desire to make a health behaviour change were asked to specify the single most important change they had made or desired to make. Options included increasing exercise, lost/lose weight, change/changed eating habits, reduce or stop smoking, reduce alcohol consumption, reduce stress, obtain/obtained medical treatment, took/take vitamins, or “other.” Respondents who reported barriers to improving their health were asked to specify 1 or more barriers from a list of options. Options included a lack of willpower, family responsibilities, work schedule, addiction to drugs or alcohol, physical condition, disability, stress, cost, unavailability, transportation problems, poor weather, and/or other. This information was used to describe the prevalence of reported health behaviour changes made, health behaviour changes desired, and barriers to health behaviour change by type across samples.
Potential confounding factors known or theorized to influence depression and health behaviours were reported descriptively for the study sample and among individuals categorized as depressed and adjusted for in subsequent analyses. These included age, gender, ethnicity (white or visible minority), marital status, annual household income, educational attainment, continuous body mass index (BMI), and presence of a chronic physical illness. Presence of a chronic physical illness included respondents who answered “yes” to having 1 or more of the following: high blood pressure, diabetes, heart disease, back problems, asthma, arthritis, bowel disorders, migraine headaches, complications from stroke, or cancer.
Statistical Analyses
Analytic samples represented between 92.04% and 95.49% of eligible participants. Statistical analyses included complete cases with data on all study variables. Demographic characteristics of the included samples were presented both pooled and separately, with reporting done using frequencies or means. Differences between depressed and nondepressed groups were examined using chi-square tests of independence for categorical variables or 2-sample t tests for continuous variables. Differences in demographic characteristics between those included and excluded for analysis were also described. Logistic regression was used to estimate unadjusted and adjusted associations between depression and reporting a recent health behaviour change, the desire to make health behaviour changes, and barriers to making health behaviour changes for each 2-year set of data, with potential interactions for age and sex investigated by adding an interaction term with each variable and depression. Associations were reported using odds ratios (ORs) and 95% confidence intervals (CIs). Prevalence of types of health behaviour changes undergone, types of health behaviour changes desired, and types of barriers to change were calculated for each 2-year set of data; associations with depression were reported for the 2007-2008 sample and summarized in tables.
Pooling of estimates for each measure of health behaviour change, as well as for prevalences of health behaviour changes and barriers to change, was done with fixed-effects meta-analyses using the inverse-variance method, where study weights were calculated using the inverse of the variance of the effect estimate to minimize imprecision of pooled estimates.21 Fixed-effects models were used because of minimal clinical and methodological heterogeneity across samples.22 A sensitivity analysis was performed by removing respondents who had reported receipt of medical treatment as a recent health behaviour change (approximately 5.42% of eligible respondents depending on analytic sample), to account for potential reporting of mental health treatment by participants with depression as a physical health behaviour change. All analyses were weighted to represent the Canadian population. This was done using relative weights, calculated by dividing provided sampling weights by the average sampling weight of each analytic sample.23 Study analyses were performed in 2018 using SAS version 9.4 (SAS Institute, Cary, NC) and Review Manager version 5.3 (The Nordic Cochrane Centre, Copenhagen).24
Results
Pooled characteristics of the 2007-2014 CCHS cycles are summarized in Table 1. Of 65,801 total respondents, 4752 were categorized as depressed (7.22%). Most respondents with depression were younger than 45 years, were white, and had completed postsecondary education. A higher proportion of depressed respondents was female, was single, and had a chronic physical illness compared to the total sample. Demographic characteristics across cycles were relatively similar (Suppl. Tables S1 to S4); compared to the 2007-2008 sample, differences included a higher proportion of minorities in the 2009-2010 sample (see Suppl. Table S2) and a higher mean BMI in the 2011-2012 and 2013-2014 samples (Suppl. Tables S3 and S4, respectively). Factors associated with missing data on depression and/or health behaviour change included age, ethnicity, marital status, income, education, and presence of a chronic physical illness (see Suppl. Table S5).
Table 1.
Pooled Sample Characteristics of the 2007-2014 Canadian Community Health Survey.
| Variable | Total Sample (n = 65,801) | Depressed (n = 4752) |
|---|---|---|
| Age (y) | ||
| 18-19 | 2.45 (2.33 to 2.57) | 3.70 (3.17 to 4.24) |
| 20-24 | 8.09 (7.88 to 8.30) | 10.04 (9.19 to 10.89) |
| 25-29 | 6.66 (6.47 to 6.86) | 12.49 (11.55 to 13.42) |
| 30-34 | 8.54 (8.33 to 8.76) | 8.91 (8.10 to 9.72) |
| 35-39 | 8.56 (8.34 to 8.77) | 9.32 (8.50 to 10.15) |
| 40-44 | 9.63 (9.40 to 9.85) | 9.51 (8.69 to 10.34) |
| 45-49 | 9.96 (9.74 to 10.19) | 11.26 (10.37 to 12.16) |
| 50-54 | 10.26 (10.02 to 10.49) | 10.18 (9.26 to 11.10) |
| 55-59 | 9.40 (9.18 to 9.62) | 9.20 (8.38 to 10.01) |
| 60-64 | 7.43 (7.23 to 7.63) | 5.09 (4.47 to 5.71) |
| 65-69 | 5.74 (5.57 to 5.92) | 2.86 (2.39 to 3.33) |
| 70-74 | 4.25 (4.10 to 4.41) | 1.69 (1.32 to 2.05) |
| 75-79 | 3.03 (2.90 to 3.17) | 0.99 (0.71 to 1.27) |
| 80+ | 2.74 (2.60 to 2.88) | 0.82 (0.54 to 1.10) |
| Sex | ||
| Male | 50.62 (50.24 to 51.00) | 37.99 (36.61 to 39.36) |
| Female | 49.29 (48.90 to 49.68) | 62.01 (60.63 to 63.38) |
| Ethnicity | ||
| White | 87.65 (87.41 to 87.89) | 87.11 (86.17 to 88.06) |
| Visible minority | 12.52 (12.27 to 12.77) | 12.90 (11.95 to 13.85) |
| Marital status | ||
| Married/common-law | 64.49 (64.13 to 64.85) | 47.06 (45.65 to 48.47) |
| Widowed/separated/divorced | 13.26 (13.00 to 13.52) | 19.19 (18.08 to 20.31) |
| Single | 22.22 (21.90 to 22.54) | 33.58 (32.25 to 34.92) |
| Income ($) | ||
| <20,000 | 9.03 (8.81 to 9.25) | 15.78 (14.75 to 16.82) |
| 20,000-39,999 | 19.23 (18.93 to 19.53) | 22.49 (21.31 to 23.67) |
| 40,000-59,999 | 18.63 (18.33 to 18.92) | 18.26 (17.16 to 19.35) |
| 60,000-79,999 | 16.31 (16.03 to 16.59) | 15.76 (14.72 to 16.79) |
| ≥80,000 | 36.68 (36.31 to 37.04) | 27.33 (26.07 to 28.59) |
| Education | ||
| < Secondary | 14.58 (14.31 to 14.85) | 14.45 (13.46 to 15.44) |
| Secondary | 15.87 (15.59 to 16.15) | 16.67 (15.62 to 17.72) |
| Some postsecondary | 7.02 (6.82 to 7.21) | 7.91 (7.15 to 8.67) |
| Postsecondary | 61.29 (60.92 to 61.66) | 59.76 (58.37 to 61.15) |
| Presence of chronic physical illness | 36.23 (35.86 to 36.59) | 47.56 (46.15 to 48.96) |
| Body mass index, mean (SD), kg/m2 | 26.18 (5.02) | 26.59 (6.19) |
Values are presented as frequency (95% confidence interval) unless otherwise indicated.
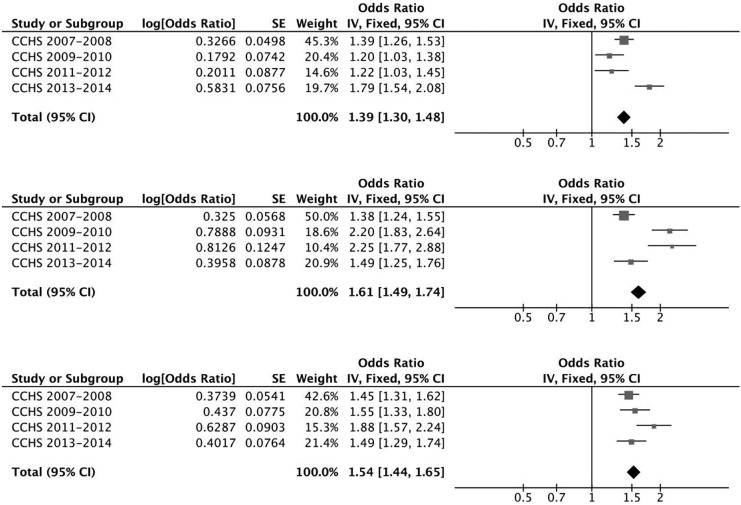
Depression was associated with higher odds of reporting a recent health behaviour change, the desire to make health behaviour changes, and barriers to health behaviour change in all study years examined in unadjusted and adjusted models (see Suppl. Table S6). Across cycles, depression was associated with 39% higher odds of reporting a recent health behaviour change (pooled OR = 1.39; 95% CI, 1.30 to 1.48), 61% higher odds of reporting the desire to make health behaviour changes (pooled OR = 1.61; 95% CI, 1.49 to 1.74), and 54% higher odds of reporting barriers to health behaviour change (pooled OR = 1.54; 95% CI, 1.44 to 1.65; see Figure 1). Interactions between depression and age, as well as depression and sex, were not statistically significant (Ps > .05) across measures of health behaviour change. A sensitivity analysis removing respondents who reported receipt of medical treatment as their most important health behaviour change attenuated pooled estimates for reporting a recent health behaviour change (pooled OR = 1.23; 95% CI, 1.15 to 1.33) but did not meaningfully affect odds of reporting the desire to make health behaviour changes (pooled OR = 1.68; 95% CI, 1.53 to 1.84) or reporting barriers to health behaviour change (pooled OR = 1.64; 95% CI, 1.51 to 1.77).
Figure 1.
For respondents without and with depression, the most important health behaviour change reported in the past 12 months across all cycles was increased exercise, followed by a change in eating habits, lost weight, receipt of medical treatment, reduced/quit smoking, and “other” changes (see Table 2). Few respondents reported having reduced alcohol, reduced stress, or taken vitamins as their most important change (<5% in both groups). In the 2007-2008 sample, compared to respondents without depression, respondents with depression were more likely to report reduced/cessation of smoking, reduced stress, and receipt of medical treatment and less likely to report having exercised or changed their eating habits as their most important health behaviour change in the past 12 months (Ps < .05; see Suppl. Table S7). Results were consistent in remaining cycles.
Table 2.
Pooled Prevalence Estimates of Most Important Changes Made in Previous Year by Depressive Status (2007-2014).
| Variable | Prevalence (95% Confidence Interval) | |
|---|---|---|
| Depresseda | Nondepressedb | |
| Exercised | 39.42 (37.77 to 41.07) | 52.40 (51.88 to 52.92) |
| Lost weight | 11.84 (10.75 to 12.92) | 10.53 (10.21 to 10.86) |
| Changed eating habits | 14.35 (13.16 to 15.53) | 17.07 (16.68 to 17.47) |
| Reduced/quit smoking | 8.17 (7.24 to 9.10) | 5.95 (5.70 to 6.21) |
| Reduced alcohol | 1.28 (0.90 to 1.66) | 0.90 (0.80 to 1.00) |
| Reduced stress | 3.46 (2.84 to 4.08) | 1.44 (1.32 to 1.56) |
| Received medical treatment | 11.64 (10.55 to 12.72) | 5.42 (5.18 to 5.66) |
| Took vitamins | 0.72 (0.43 to 1.00) | 1.20 (1.08 to 1.31) |
| Other | 6.35 (5.52 to 7.17) | 4.30 (4.09 to 4.51) |
All estimates are weighted to the Canadian population.
a n = 4752.
b n = 61,049.
Similar to recent changes made, for respondents without and with depression, the most important health behaviour change desired across cycles was increased exercise (see Table 3). Several respondents in both groups reported wanting to reduce or quit smoking. Prevalence estimates of remaining changes desired were similar to recent changes reported for change in eating habits and reducing alcohol. Few reported wanting to reduce stress (<5% in both groups), seek medical treatment (<3% in both groups), or take vitamins (<1% in both groups). In the 2007-2008 sample, compared to respondents without depression, respondents with depression were more likely to report wanting to reduce or quit smoking, reduce stress, or seek medical treatment and were less likely to report wanting to exercise or change their eating habits (Ps < .05; see Suppl. Table S8). Results were consistent in remaining cycles.
Table 3.
Pooled Prevalence Estimates of Most Important Changes Needed to Improve Physical Health by Depressive Status (2007-2014).
| Variable | Prevalence (95% Confidence Interval) | |
|---|---|---|
| Depresseda | Nondepressedb | |
| Increase exercise | 43.03 (41.48 to 44.59) | 51.39 (50.91 to 51.86) |
| Lose weight | 9.04 (8.14 to 9.94) | 9.68 (9.40 to 9.96) |
| Change eating habits | 14.08 (12.99 to 15.18) | 17.90 (17.54 to 18.26) |
| Reduce/quit smoking | 20.16 (18.90 to 21.42) | 12.44 (12.13 to 12.75) |
| Reduce alcohol | 0.69 (0.43 to 0.95) | 0.79 (0.71 to 0.88) |
| Reduce stress | 3.18 (2.63 to 3.73) | 2.50 (2.35 to 2.65) |
| Receive medical treatment | 2.34 (1.87 to 2.81) | 1.16 (1.06 to 1.26) |
| Take vitamins | 0.09 (0.00 to 0.20) | 0.23 (0.18 to 0.27) |
| Other | 5.15 (4.46 to 5.85) | 3.26 (3.10 to 3.43) |
All estimates are weighted to the Canadian population.
a n = 4724.
b n = 60,669.
The most common barrier to making health behaviour changes reported across cycles was a lack of willpower for respondents in both groups, followed by work schedules, “other” barriers, family responsibilities, disability, and stress (see Table 4). Few respondents endorsed experiencing remaining barriers. In the 2007-2008 sample, compared to respondents without depression, respondents with depression were more likely to report barriers including work schedules, stress, financial constraints, and disability and less likely to report family responsibilities (Ps < .05; see Suppl. Table S9). Results were consistent in remaining cycles.
Table 4.
Pooled Prevalence Estimates of Types of Barriers to Change by Depressive Status (2007-2014).
| Variable | Prevalence (95% Confidence Interval) | |
|---|---|---|
| Depresseda | Nondepressedb | |
| Lack willpower | 31.38 (29.53 to 33.24) | 33.21 (32.58 to 33.85) |
| Family responsibilities | 9.90 (8.70 to 11.09) | 14.55 (14.07 to 15.02) |
| Work schedule | 16.19 (14.72 to 17.66) | 25.13 (24.55 to 25.72) |
| Addiction | 2.83 (2.17 to 3.50) | 0.83 (0.71 to 0.96) |
| Physical condition | 7.54 (6.49 to 8.59) | 3.32 (3.07 to 3.56) |
| Disabled | 10.17 (8.96 to 11.37) | 5.06 (4.77 to 5.35) |
| Stressed | 10.28 (9.06 to 11.49) | 3.88 (3.61 to 4.14) |
| Financial constraints | 9.61 (8.45 to 10.78) | 4.75 (4.47 to 5.03) |
| Not available in area | 1.10 (0.68 to 1.51) | 0.91 (0.79 to 1.04) |
| Transportation problems | 0.75 (0.41 to 1.10) | 0.31 (0.23 to 0.38) |
| Weather problems | 1.74 (1.22 to 2.26) | 1.91 (1.73 to 2.09) |
| Other | 15.27 (13.84 to 16.70) | 17.35 (16.84 to 17.86) |
All estimates are weighted to the Canadian population.
a n = 3727.
b n = 40,402.
Discussion
This study of more than 65,000 Canadians found that respondents with depression were more likely to report a recent health behaviour change, the desire to make health behaviour changes, and barriers to health behaviour change. Respondents with and without depression most commonly endorsed an increase in exercise as the most important health behaviour change they had made or were seeking to make. The most common barrier to change endorsed in both groups was a lack of willpower. Respondents with depression were more likely to cite health behaviour changes including smoking cessation and stress reduction, as well as barriers including financial constraints and disability, relative to nondepressed respondents. To our knowledge, this study is the first to examine the broad associations between depression and health behaviour change in a general population sample. Our results are consistent with studies examining health behaviour change in groups experiencing comorbid depression and poor physical health16,17,25 and provide data to support the associations between depression and health behaviour change independent of physical health status.
From a public health perspective, it is promising that a significant proportion of respondents experiencing depression reported both recent efforts to improve their physical health (69.46%, 2007-2008) and the desire to make changes to improve their physical health (75.98%, 2007-2008). As relations between depression and several poor health behaviours (e.g., diet, low physical activity) are bidirectional, it can be theorized that modifying poor health behaviours can influence not only long-term physical health but also long-term mental health. Standard treatment of depression typically comprises the use of pharmacotherapy, psychological therapies, or a combination of both. However, the examination of lifestyle modification, particularly through diet and exercise, as a standalone or adjunct treatment for depression has received increased attention in recent years.26,27 For example, a recent randomized controlled trial demonstrated significant improvement in depressive symptoms for subjects enrolled in a diet support group compared to subjects enrolled in a social support group.27 Furthermore, meta-analyses have demonstrated moderate effect sizes favouring exercise over standard treatment or control for depression.26 Our findings, which suggest that many of those dealing with depression report efforts and/or interest in making health behaviour changes, are promising, particularly as examinations into the feasibility and effectiveness of lifestyle modification as an avenue for treating depression continue to emerge. Addressing health behaviours commonly cited by participants with depression in the current study, including exercise, smoking, and diet, may be the most meaningful targets of intervention.
Several studies also suggest that among those who seek standard treatment for depression, those who report barriers to receipt of treatment or to treatment adherence have poorer prognostic outcomes than those who do not.28–31 By comparison, examinations of barriers to lifestyle modification among those experiencing depression are scarce. In the current study, those with depression who wanted to make changes to improve their physical health were more likely to report barriers that prevented them from making these changes. Those with depression who seek or who are referred to treatments involving lifestyle modification may encounter difficulties during treatment due to perceived barriers. Those with low mastery (i.e., those who feel like the circumstances of their life are outside their control) or low self-efficacy (i.e., lower belief in one’s ability to accomplish a task) may particularly perceive barriers to health behaviour change as factors that are beyond their control, negatively influencing their ability to comply with treatment. These factors have in turn been linked to depression recurrence and poor health behaviours.32,33
Consideration of barriers to successful health behaviour change is important when designing and administering effective interventions. The barriers to change identified in the current study are of particular interest, including a lack of willpower, which was the most commonly cited barrier in both groups, and financial constraints, disability, and stress, which were more commonly cited in participants with depression than those without. For example, the inclusion of a motivational interviewing component may be of relevance. Motivational interviewing in the context of obesity treatments (i.e., involving diet and physical activity changes) has demonstrated improved short-and long-term treatment adherence,34,35 with positive findings extending to different delivery methods (e.g., in-person, telephone), different age groups, and racially diverse and lower-income samples.35,36 Furthermore, the addition of a mindfulness meditation component to treatment can serve to reduce stress,37 a factor that was identified as an important health behaviour change and as a barrier to change in the current study. Addressing barriers to change in those with depression can have positive impacts on treatment adherence and long-term maintenance of treatment gains, which can ultimately protect against depression recurrence and poor physical health outcomes.
The current study has several limitations to consider. Data used for this study were cross-sectional and do not allow for ascertainment of temporality or causality of relations between depression and health behaviour change. It is possible that depression may have occurred after a recent health behaviour change. In addition, because a change in appetite or weight, including significant weight loss, is one of the criteria used for diagnosis of a major depressive episode,38 it is possible that respondents who lost weight due to depression may have endorsed a health behaviour change for this reason. Depression and health behaviour change variables were derived from self-report items and thus may be subject to reporting bias. For example, some respondents may have overendorsed health behaviour change; if this varied by depression status, this may bias our findings in either direction. Furthermore, self-reported health behaviour change may not be indicative of successful health behaviour change. Reported health behaviour changes may have been short-lived, and/or degree of change may be too small to meaningfully affect one’s physical health status. Respondents were also limited to selecting one type of health behaviour change, although it is possible that multiple health behaviour changes were either desired by or completed by respondents. Finally, although the complex survey design of the CCHS is intended to generate findings representative of the Canadian population, the inclusion of repeated provinces across cycles (e.g., Prince Edward Island, Nova Scotia) may lead to clustering effects.
The current study also has strengths. First, we used a population-based survey with a large sample size and high response rate, which allowed for the examination of associations between depression and health behaviour change in a representative sample with adjustment for several confounders. Second, we were able to examine associations between depression and health behaviour change using 8 years of data, demonstrating consistency over time. Third, we were able to provide data on health behaviour change in individuals dealing with depression without restriction to those with comorbid physical conditions, which is particularly valuable as research examining associations between depression and health behaviours, as well as the feasibility of lifestyle-based interventions for depression, continues to grow.
Conclusion
In the current study, we observed significant associations between depression and measures of health behaviour change, where those with depression were more likely to report a recent health behaviour change, the desire to make health behaviour changes, and barriers to change. To our knowledge, this is the first study to demonstrate these associations in a general population sample. These findings can have important implications for public health via highlighting the feasibility of lifestyle modification as a potential treatment of depression, as well as promoting advocacy of adopting healthy behaviours as a means to prevent adverse physical and mental health outcomes. Future studies may seek to examine prospective associations between depression and health behaviour change, as well as further ascertain whether reported changes are maintained over time.
Supplemental Material
Supplemental_Tables for Associations between Depression and Health Behaviour Change: Findings from 8 Cycles of the Canadian Community Health Survey by Zahra M. Clayborne, and Ian Colman in The Canadian Journal of Psychiatry
Acknowledgments
Data used for this study were collected by Statistics Canada, but the analyses, results, and interpretation of the findings are the responsibility of the study authors and do not reflect the views of Statistics Canada.
Data Access
The data used for this study come from Statistics Canada public use microdata files available via the Data Liberation Initiative. The Data Liberation Initiative allows free access to these files for faculty and students at participating postsecondary educational institutions in Canada.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Zahra Clayborne is supported by a Master’s Award from the Canadian Institutes of Health Research. Dr. Ian Colman is supported by the Canada Research Chairs Program. The sources of funding had no role in study design; the collection, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
ORCID iD: Ian Colman, PhD  http://orcid.org/0000-0001-5924-0277
http://orcid.org/0000-0001-5924-0277
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Patten SB, Jian LW, Williams JVA, et al. Descriptive epidemiology of major depression in Canada. Can J Psychiatry. 2006;51(2):84–90. [DOI] [PubMed] [Google Scholar]
- 2. Kessler R, Petukhova M, Sampson NA, et al. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2007;21(3):169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fombonne E, Wostear G, Cooper V, et al. The Maudsley long-term follow-up of child and adolescent depression: suicidality, criminality and social dysfunction in adulthood. Br J Psychiatry. 2001;179:218–223. [DOI] [PubMed] [Google Scholar]
- 4. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Murray CJ, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Geneva (Switzerland): World Health Organization; 1996. [Google Scholar]
- 6. Jerstad SJ, Boutelle KN, Ness KK, et al. Prospective reciprocal relations between physical activity and depression in female adolescents. J Consult Clin Psychol. 2010;78(2):268–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jacka FN, Pasco JA, Mykletun A, et al. Association of Western and traditional diets with depression and anxiety in women. Am J Psychiatry. 2010;167(3):305–311. [DOI] [PubMed] [Google Scholar]
- 8. McMartin SE, Jacka FN, Colman I. The association between fruit and vegetable consumption and mental health disorders: evidence from five waves of a national survey of Canadians. Prev Med. 2013;56(3-4):225–230. [DOI] [PubMed] [Google Scholar]
- 9. Choi WS, Patten CA, Gillin JC, et al. Cigarette smoking predicts development of depressive symptoms among U.S. adolescents. Ann Behav Med. 1997;19(1):42–50. [DOI] [PubMed] [Google Scholar]
- 10. Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease. Arch Gen Psychiatry. 1998;55(7):580–592. [DOI] [PubMed] [Google Scholar]
- 11. Mezuk B, Eaton WW, Albrecht S, et al. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31(12):2383–2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. [DOI] [PubMed] [Google Scholar]
- 13. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hu FB, Stampfer MJ, Manson JE, et al. Trends in the incidence of coronary heart disease and changes in diet and lifestyle in women. N Engl J Med. 2000;343(8):530–537. [DOI] [PubMed] [Google Scholar]
- 15. Gregory CO, Blanck HM, Gillespie C, et al. Perceived health risk of excess body weight among overweight and obese men and women: differences by sex. Prev Med. 2008;47(1):46–52. [DOI] [PubMed] [Google Scholar]
- 16. Lin EHB, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–2160. [DOI] [PubMed] [Google Scholar]
- 17. Appelhans BM, Whited MC, Schneider KL, et al. Depression severity, diet quality, and physical activity in women with obesity and depression. J Acad Nutr Diet. 2012;112(5):693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Statistics Canada. Surveys and statistical programs—Canadian Community Health Survey—Mental Health (CCHS). Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5015. Accessed April 9, 2017.
- 19. Kessler RC, Andrews G, Mroczek DK, et al. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Meth Psych Res. 1998;7(4):171–185. [Google Scholar]
- 20. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed Washington (DC): American Psychiatric Association; 1994. [Google Scholar]
- 21. Deeks J, Higgins J, Altman D. Analysing data and undertaking meta-analyses In: Higgins JPT, Green S. (eds) Cochrane handbook for systematic reviews of interventions. 4th ed New York, NY: Wiley; 2011:243–296. [Google Scholar]
- 22. Borenstein M, Hedges LV, Higgins JPT, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. [DOI] [PubMed] [Google Scholar]
- 23. Statistics Canada. Canadian community health survey (CCHS): 2007 microdata files user guide. Available from: http://www23.statcan.gc.ca/imdb-bmdi/pub/document/3226_D7_T9_V4-eng.pdf. Accessed February 28, 2018.
- 24. The Nordic Cochrane Centre. Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Cochrane Collaboration; 2014. [Google Scholar]
- 25. Dixon JB, Dixon ME, O’Brien PE. Depression in association with severe obesity: changes with weight loss. Arch Intern Med. 2003;163(17):2058–2065. [DOI] [PubMed] [Google Scholar]
- 26. Mead GE, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database Syst Rev. 2008;(4):CD004366. [DOI] [PubMed] [Google Scholar]
- 27. Jacka FN, O’Neil A, Opie R, et al. A randomised controlled trial of dietary improvement for adults with major depression (the “SMILES” trial). BMC Med. 2017;15(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Olfson M, Marcus SC, Tedeschi M, et al. Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry. 2006;163(1):101–108. [DOI] [PubMed] [Google Scholar]
- 29. Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36(1):60–69. [DOI] [PubMed] [Google Scholar]
- 30. Meredith LS, Stein BD, Paddock SM, et al. Perceived barriers to treatment for adolescent depression. Med Care. 2009;47(6):677–685. [DOI] [PubMed] [Google Scholar]
- 31. Sirey JA, Bruce ML, Alexopoulos GS, et al. Stigma as a barrier to recovery: perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52(12):1615–1620. [DOI] [PubMed] [Google Scholar]
- 32. Colman I, Naicker K, Zeng Y, et al. Predictors of long-term prognosis of depression. CMAJ. 2011;183(17):1969–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Daniel M, Brown A, Dhurrkay JG, et al. Mastery, perceived stress and health-related behaviour in northeast Arnhem Land: a cross-sectional study. Int J Equity Health. 2006;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bean MK, Powell P, Quinoy A, et al. Motivational interviewing targeting diet and physical activity improves adherence to paediatric obesity treatment: results from the MI Values randomized controlled trial. Pediatr Obes. 2015;10(2):118–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Armstrong MJ, Mottershead TA, Ronksley PE, et al. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12(9):62–92. [DOI] [PubMed] [Google Scholar]
- 36. Burke LE, Dunbar-Jacob J, Orchard TJ, et al. Improving adherence to a cholesterol-lowering diet: a behavioral intervention study. Patient Educ Couns. 2005;57(1):134–142. [DOI] [PubMed] [Google Scholar]
- 37. Grossman P, Niemann L, Schmidt S, et al. Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res. 2004;57(1):35–43. [DOI] [PubMed] [Google Scholar]
- 38. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed Arlington (VA): American Psychiatric Association; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental_Tables for Associations between Depression and Health Behaviour Change: Findings from 8 Cycles of the Canadian Community Health Survey by Zahra M. Clayborne, and Ian Colman in The Canadian Journal of Psychiatry