Abstract
The alteration of water balance and related disorders has emerged as being strictly linked to the state of activation of the vasopressin–aquaporin-2 (vasopressin–AQP2) pathway. The lack of responsiveness of the kidney to the vasopressin action impairs its ability to concentrate the urine, resulting in polyuria, polydipsia, and risk of severe dehydration for patients. Conversely, non-osmotic release of vasopressin is associated with an increase in water permeability in the renal collecting duct, producing water retention and increasing the circulatory blood volume. This review highlights some of the new insights and recent advances in therapeutic intervention targeting the dysfunctions in the vasopressin–AQP2 pathway causing diseases characterized by water balance disorders such as congenital nephrogenic diabetes insipidus, syndrome of inappropriate antidiuretic hormone secretion, nephrogenic syndrome of inappropriate antidiuresis, and autosomal dominant polycystic kidney disease. The recent clinical data suggest that targeting the vasopressin–AQP2 axis can provide therapeutic benefits in patients with water balance disorders.
Keywords: Vasopressin, AQP2, NDI, SIADH, NSIAD, ADPKD
Introduction
The maintenance of water balance is essential for all physiological processes and is critically dependent on water intake via thirst and water output in the kidney under the control of the antidiuretic hormone vasopressin. An increase in plasma osmolality, sensed by osmoreceptors situated in the brain, represents the most important input to cause thirst and stimulation of vasopressin release. Vasopressin is secreted into the circulation by the posterior pituitary gland in response to an increase in serum osmolality or a decrease in blood volume. In the kidney, vasopressin binds to the type 2 vasopressin receptor (V2R) and increases osmotic water transport through the regulation of the aquaporin-2 (AQP2) water channel localized in the kidney connecting tubules and collecting ducts 1, 2. V2R is a G-protein-coupled receptor (GPCR) localized at the basolateral plasma membrane of the principal cells of the kidney collecting duct. A recent transcriptome study of 14 microdissected nephron segments of rat kidney demonstrated the V2R mRNA expression from the medullary thick ascending limb to the inner medullary collecting duct 3. Upon binding of vasopressin to V2R, a G s protein is activated, leading to stimulation of adenylyl cyclases, increase in intracellular cAMP, and activation of protein kinase A (PKA). The cAMP/PKA signal transduction cascade results in multiple phosphorylating events in the C-terminus of the water channel AQP2 regulating its trafficking and the water luminal permeability 2, 4– 6. Vasopressin also triggers increases in intracellular calcium required for AQP2 trafficking 7, 8.
Most of the effect of vasopressin is thought to be related to PKA-mediated phosphorylation currently explored by large-scale phosphoproteomics to identify regulated proteins’ downstream PKA activation 9. On the other hand, several proteins participating in the control of cAMP-dependent AQP2 trafficking, including SNAREs, annexin-2, hsc70, A-kinase anchoring proteins (AKAPs), and small GTPases of the Rho family proteins controlling cytoskeletal dynamics, have been identified 10– 18. In addition to phosphorylation, AQP2 undergoes different regulated post-translational modifications, such as ubiquitination and glutathionylation, which are likely to be fundamental for controlling AQP2 cellular localization, stability, and function 19– 23.
Besides short-term regulation of AQP2 trafficking, vasopressin regulates the total amount of the water channel within the cell and alters the protein half-life of AQP2 24– 29. Alterations in AQP2 abundance as well as defects in vasopressin signaling in the renal collecting duct can seriously compromise renal function and the maintenance of water balance in the body.
This review highlights some of the new insights and recent advances in targeting the vasopressin–AQP2 pathway in some relevant diseases associated with water balance disorders, such as congenital nephrogenic diabetes insipidus (NDI), idiopathic syndrome of inappropriate antidiuretic hormone secretion (SIADH), nephrogenic syndrome of inappropriate antidiuresis (NSIAD), and autosomal dominant polycystic kidney disease (ADPKD).
Vasopressin–AQP2 pathway in water balance disorders
Plasma copeptin as a surrogate marker of vasopressin secretion in renal disorders
Significant progress in studying the role of vasopressin in renal disorders came from the identification of copeptin, a stable surrogate marker of vasopressin secretion that is relatively easily measured 30– 33. Copeptin is a peptide corresponding to the COOH-terminal portion of pro-vasopressin and is co-secreted in equimolar amounts with vasopressin, representing a good biomarker for vasopressin 34. Indeed, it has been reported that plasma concentrations of copeptin correlate strongly in several clinical conditions 32, 33, 35, 36. In a large cross-sectional study, plasma copeptin and microalbuminuria positively correlated 37, and this correlation was also found to persist with a 16-year follow-up 38. The increase in urinary albumin excretion is likely to reflect not only glomerular damage but also systemic endothelial dysfunction and is consistent with the hypothesis that vasopressin induces urinary albumin excretion as previously reported in rats and humans 39, 40. Conversely, suppressing vasopressin by administering a V2R antagonist or by simply increasing water intake might be beneficial for renal function and diabetes 39, 41.
As shown previously, vasopressin levels are also increased in diabetic nephropathy characterized by dysregulation of water balance displaying water depletion as a consequence of osmotic diuresis due to glycosuria 42, probably to limit water loss. Of interest, in patients with type 2 diabetes, plasma copeptin was found to be associated with a faster decline in glomerular filtration rate (GFR) in two distinct studies 43, 44.
The role of vasopressin is particularly central in the pathogenesis of another severe disease, ADPKD, characterized by the expansion of renal cysts eventually leading to loss of renal function. Association of urinary copeptin with the severity of ADPKD was also recently demonstrated 44, suggesting that copeptin can represent a novel marker to predict renal prognosis in ADPKD. Copeptin levels are negatively associated with GFR, kidney size, and number of renal cysts 33, 45, 46. While ADPKD is the most advanced disease for the therapeutic use of vasopressin receptor blockade, this strategy is also currently being explored in chronic kidney diseases (CKDs).
In summary, the vasopressin–AQP2 system has a critical role in various stages of CKD 47– 49 and in several kidney diseases 46, making this pathway very promising from a therapeutic perspective. Indeed, high water intake (particularly plain water) has been proven to be beneficial in preventing CKD progression in several studies (reviewed in 46), based on the expected suppression of vasopressin release that can be easily monitored by plasma copeptin measurements. On the other hand, the association between total fluid intake (excluding water intake) and change in kidney function requires additional prospective studies, since other data do not support the hypothesis that total fluid consumption (excluding water intake) protects against CKD 50; therefore, additional study with prospective evaluation of kidney function is required.
Targeting defective vasopressin–AQP2 pathway in nephrogenic diabetes insipidus
NDI is a disease characterized by the kidney’s inability to concentrate urine despite elevated concentrations of vasopressin. The congenital form of NDI can be due to mutation of either the vasopressin receptor or AQP2 and is associated with marked polyuria, polydipsia, and electrolyte imbalance with a constant risk of severe dehydration for patients 51, 52. Most of the forms of NDI are due to non-functional V2R (X-linked NDI) 53. X-linked NDI accounts for 90% of cases of congenital NDI and occurs with a frequency of 4 to 8 per 1 million male live births. Autosomal NDI accounts for about 10% of the remaining cases 54.
NDI can also be acquired and is a frequent side effect of lithium therapy 55 or other drugs 56– 60. Hypokalemia or hypercalcemia with associated hypercalciuria also cause acquired NDI 28, 61– 68.
The year 2013 was the 100th anniversary of vasopressin treatment for central diabetes insipidus due to vasopressin hormone deficiency 69. Despite extensive research in the field, a real cure for NDI is still missing and treatment is rather symptomatic with a continuous supply of water and drugs such as ibuprofen and indomethacin in combination with hydrochlorothiazide, which however only partially (by 25% to 50%) reduce the abundant polyuria 51, 68, 70.
The therapeutic approaches under investigation regard the rescue of mutated V2R or AQP2, in case of defective trafficking of these proteins, or bypassing the V2R signaling, in case of inactive V2Rs, finalized to increasing the cell surface expression of AQP2 51, 71– 73.
In patients with NDI due to V2R mutations or as a consequence of lithium therapy, AQP2 is in fact theoretically functioning, suggesting the possibility of increasing its apical membrane abundance independently from vasopressin or cAMP. Some studies suggest that this may be possible. Sildenafil, a phosphodiesterase inhibitor causing an increase in cyclic guanosine monophosphate, reduced polyuria in rats with lithium-induced NDI 74. Moreover, a child affected by X-linked NDI treated with sildenafil had a beneficial effect in decreasing urine volume and increased urine osmolality 75.
Another approach to bypass defective V2R was altering the cholesterol content of the apical membrane to increase AQP2 accumulation. To this end, different statins have been used. Statins are a family of 3-hydroxy-3-methylglutaryl-CoA reductase inhibitors commonly used to inhibit cholesterol biosynthesis. Besides this, in vitro studies showed that statins reduced endocytosis possibly by inhibiting isoprenylation of Rho GTPase, which leads to actin cytoskeletal reorganization during protein trafficking 76. Of note, in renal cells and in vivo, statins have been shown to promote AQP2 localization to the apical membrane 77, 78, a process known to require apical depolymerization of the actin network and Rho inhibition 11, 12.
Interestingly, a combination of two statins—fluvastatin and secretin—drastically reduced urine output by nearly 90% and doubled urine osmolality in mouse models of NDI in a mouse model 79. Statin treatment was also found to be beneficial in NDI patients with inactivating mutation of the V2R 78 and in patients under lithium therapy 80. Besides the effect in reducing urinary output in patients with NDI, the efficacy of the treatment with statins in increasing apical expression of AQP2 has been monitored by measuring the urinary excretion of AQP2 (u-AQP2), which was found to be increased in a time- and dose-dependent manner 81.
The most recent approach for treating congenital X-linked NDI is based on treatment with metformin, a drug used for the treatment of diabetes which is able to activate the adenosine monophosphate kinase (AMPK) 82, 83. In the renal inner medullary collecting duct, AMPK phosphorylates AQP2 and urea transporter UT-A1, resulting in water and urea reabsorption 83, and improves renal concentrating ability in X-linked NDI mice 82. Therefore, AMPK activation with metformin might represent an alternative therapeutic approach to treat X-linked NDI. More recently, it was shown that inhibition of AKAPs binding to PKA increases PKA activity and activates AQP2 channels in cortical collecting duct cells 84. In line with this finding, in vivo experiments revealed that the compound 3,3′-diamino-4,4′-dihydroxydiphenylmethane (FMP-API-1) induced AQP2 phosphorylation, trafficking, and water reabsorption to the same extent as vasopressin in the context of V2R inhibition. This study points to AKAP-PKA disruptors as a potential novel category of therapeutic drugs for congenital NDI 84.
Targeting selected GPCRs with agonists to increase cAMP has also been considered an option to treat NDI. Among the GPCRs expressed in the inner medulla collecting duct, activation of the calcitonin receptor caused an increase in cAMP and accumulation of AQP2 in the plasma membrane in LLCKP1 cells 85 and reduced urinary output in vasopressin-deficient Brattleboro rats 79. Other GPCRs whose activation was found to be associated with increased AQP2 expression are the angiotensin II AT1 receptor 86 and secretin receptor 79, 87. However, it has to be underlined that in vivo testing of this approach targeting GPCRs revealed that the effect is transient and this is probably due to desensitization of the receptors 79, 85. In parallel, four other GPCRs, the protein-coupled E-prostanoid receptors EP1–EP4, have been considered for their ability to increase cAMP and AQP2 in MDCK cells 88. Selective silencing of EP4 in mice resulted in reduced renal concentrating ability 89. Interestingly, in renal collecting duct cell models, EP4 activation increased AQP2 trafficking independently from cAMP elevation 73, 90, although the mechanisms responsible for EP4-induced stimulation of AQP2 trafficking are not yet clarified.
The calcium signaling pathway in the vasopressin response has also been considered a major target in the treatment of NDI. Specifically, activators of calcium signaling in collecting duct principal cells may represent a therapeutic strategy in NDI. In a recent seminal study, Uchida et al. demonstrated that activation of the calcium signal transducer Wnt5a, through a calcium/calmodulin/calcineurin signaling pathway, induced phosphorylation, trafficking, and mRNA expression of AQP2 in mpkCCDCl4 cells 91. Of note, in isolated cortical collecting ducts from a V2R-inhibited NDI mouse model, Wnt5a increased osmotic water permeability and urine osmolality, activating a different pathway of the vasopressin-induced cAMP elevation, involving a functional role of calcineurin/arachidonic acid known to induce vasopressin-like effects in mpkCCD cells. These new data point to calcineurin activators as possible drugs for the treatment of congenital NDI.
Vasopressin–AQP2 pathway in syndrome of inappropriate antidiuretic hormone secretion and nephrogenic syndrome of inappropriate antidiuresis
SIADH may be considered an opposite disease with respect to NDI. Patients with SIADH have high levels of vasopressin even in the presence of low serum osmolality, leading to dilutional hyponatremia secondary to elevated renal water reabsorption 92, 93.
Hyponatremia is defined as a serum Na level below 135 mmol/L and is associated with an increase in mortality in hospitalized patients 94. In SIADH, high levels of vasopressin are present even when plasma osmolality reaches values that normally suppress vasopressin release and the resulting hyponatremia can be ascribed to a non-osmotic release of vasopressin 95. Nevertheless, a phenomenon called “vasopressin escape” allows the kidney to excrete free water through reduced expression of the gene encoding AQP2, thus increasing water excretion 96, 97. Interestingly, a recent study uncovered some signaling mechanisms that defend against hyponatremia in SIADH 21. A SIADH-like condition is frequently related to aging 93. SIADH has several major etiologies, including central nervous system and pulmonary disorders, tumors, and drugs, the last of which is related mainly to psychopharmacological treatment. An interesting observation is that treatment with antipsychotics is associated with elevated activity of calcineurin and enhanced vasopressin release, which may contribute to activation of AQP2 trafficking causing drug-induced SIADH. Moreover, cyclophosphamide, an anti-cancer drug, activates V2R and induces AQP2 expression in rat kidney despite the absence of vasopressin stimulation 98. This finding suggested the possibility of drug-induced NSIAD. The syndrome of inappropriate antidiuresis has been suggested as an alternative to SIADH, since a subgroup of patients with features of SIADH does not have high plasma vasopressin levels 99. Therefore, dilutional hyponatremia may result from either excessive AVP release or constitutive activation of V2R.
The use of antagonists of the vasopressin receptors (vaptans) represents the most direct treatment for hyponatremia in SIADH. In this respect, over the last 10 years, significant advances in the treatment of SIADH have been made 100.
Among vaptans, conivaptan represents the first vasopressin receptor blocker approved by the US Food and Drug Administration 93. Conivaptan is given intravenously and acts on both V1 and V2 vasopressin receptors, resulting in solute-free water diuresis (aquaresis). Tolvaptan instead is orally active and is a selective antagonist of the V2R. It has been shown to be effective and safe for up to 3 years 101. Both conivaptan and tolvaptan are approved for the treatment of hypervolemic hyponatremia in patients with heart failure or cirrhosis and of euvolemic hyponatremia in patients with SIADH. We recently demonstrated that tolvaptan prevents AQP2 trafficking and function in collecting duct principal cells and reduces AQP2 excretion in two patients with SIADH paralleled by normalization of plasma sodium concentration, clearly demonstrating the central role of AQP2 blockade in the aquaretic effect of tolvaptan 102. An alternative approach with broad potential clinical application is the identification of small-molecule inhibitors of aquaporins 103; however, so far, progress in the field has been disappointing.
As discussed, SIADH is characterized by hypersecretion of vasopressin. However, 10% to 20% of patients with inappropriate antidiuresis display low or undetectable vasopressin circulating levels. This condition was found to be associated with gain-of-function mutations of the V2R, first discovered in 2005 104, and the associated disease was defined as NSIAD to distinguish it from SIADH. NSIAD is a very rare disease representing the mirror image of NDI; 21 cases have been reported to date and the majority of them come from five families. In the first two cases of NSIAD, the mutations of the V2R were found at residue R137.
In the first two cases of NSIAD, the mutations of the V2R gene ( AVPR2) result in changes in codon 137 from arginine to cysteine or leucine (R137C and R137L). Of note, whereas substitution of R137 to cysteine or leucine results in NSIAD, conversion of R137 to histidine (R137H) is a well-known loss-of-function mutation associated with NDI, leading to water loss and inability to concentrate urine 105. Thus, mutations of the same amino acid of the V2R, R137, can have opposite clinical outcomes. Other constitutively activating mutations causing NSIAD—namely F229V 106, I130N 107, and L312S 108—have been subsequently identified. Theoretically, NSIAD should be treated with a V2R inverse agonist; however, tolvaptan and satavaptan had no efficacy in patients carrying mutations of R137 109. In contrast, both drugs have an effect on F229V, I130N mutants, and L312S in vitro, suggesting that they could be effective in patients carrying these mutations 106– 108.
Targeting the vasopressin–AQP2 pathway in autosomal dominant polycystic kidney disease
ADPKD is an inherited disorder with an estimated frequency of 1 in 400 to 1,000 live births 110 and is characterized by the progressive growth of renal cysts causing disruption of renal architectures and eventually leading to end-stage renal disease. Despite high baseline vasopressin levels, patients frequently present defective urinary concentration, and this is probably due to a peripheral resistance to vasopressin 111, 112. Interestingly, the blockade of V2R using tolvaptan in patients with rapidly progressing ADPKD has been proven to slow cyst growth, supporting the involvement of the V2R pathway in ADPKD 113, 114.
The hereditary form of ADPKD is due to mutations in PKD1 or PKD2 genes, encoding for polycystin 1 (PC1) and polycystin 2 (PC2), respectively. PC1 is localized to the primary cilium and in cell–cell contacts, suggesting a role as an adhesion protein 115. PC2, instead, is a non-selective cation channel permeable to calcium, expressed in the endoplasmic reticulum and in primary cilium, where it forms a complex with PC1 and has a role in intracellular Ca 2+ homeostasis. At the cellular level, mutations in PKD1 or PKD2 are associated with a reduction in intracellular calcium, increase in cAMP, and constitutive activation of PKA, making the collecting duct principal cells under constant tonic effect of vasopressin. The disruption in calcium and cAMP signaling cascades activates pathways causing cell proliferation, increased fluid secretion, and interstitial inflammation 116, 117. Our recent in vitro study demonstrated that in human conditionally immortalized proximal tubular epithelial cells silenced for PKD1 (ciPTEC-PC1KD) or generated from a patient with ADPKD1 (ciPTEC-PC1Pt), selective activation of the calcium-sensing receptor increases cytosolic calcium, reduces intracellular cAMP and mTOR activity 118, and rescues defective ATP mitochondrial production 119, reversing the principal ADPKD dysregulations.
Currently, there is no cure for the disease; it is clinically manageable only through the control of its many complications, and the existing therapeutic approaches are rather supportive. Nevertheless, as mentioned, some drugs targeting the vasopressin–AQP2 pathway have been found to slow the progression of ADPKD in animal models and clinical trials 120. Tolvaptan has been tested on ADPKD patients with higher total kidney volume and was found to delay the progression of ADPKD, supporting the link between V2R signaling and ADPKD development 113, 121. Tolvaptan has been approved to delay the progression of ADPKD in Japan, Canada, and the European Union, and very recently the US Food and Drug Administration also approved tolvaptan as the first drug treatment to slow kidney function decline in adults at risk of rapidly progressing ADPKD.
Conclusions and perspectives
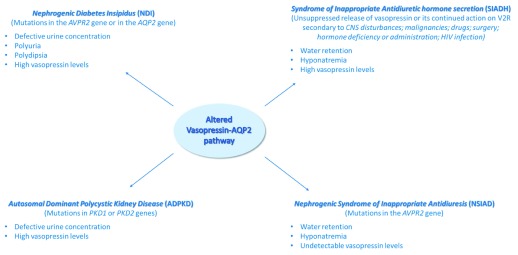
Over the past decade, interest in the vasopressin–AQP2 pathway has been renewed, mainly because of the availability of vaptans, the orally active vasopressin receptor antagonists, and of the use of copeptin as a surrogate marker of vasopressin. The dysregulation of the vasopressin–AQP2 system is clearly and tightly associated with specific diseases such as NDI, SIADH, NSIAD, and ADPKD, briefly discussed in this review ( Figure 1).
Figure 1. Targeting the vasopressin–AQP2 pathway in water balance disorders.
Alterations of the vasopressin–AQP2 axis, causes of the disease, and principal effects observed in selected water balance disorders. AQP2, aquaporin-2; CNS, central nervous system; V2R, type 2 vasopressin receptor.
With regard to NDI, many target molecules for the treatment of congenital NDI have been proposed; however, no specific pharmacological drugs have yet reached clinical application. In the development of drugs for the treatment of congenital NDI, it is important to identify/design drugs that directly activate AQP2 without toxic effects and to pay attention to preserving the medullary osmotic gradient, representing the driving force for water reabsorption. In this scenario, the screening for calcineurin activators like Wnt5a is a potentially promising therapeutic strategy to develop novel drugs for the treatment of heritable NDI.
Conversely, for the management of opposite diseases such as SIADH, characterized by hyperactivation of the vasopressin–AQP2 pathway, as discussed in this review, the use of vaptans to block vasopressin receptors represents the main avenue for the direct treatment of hyponatremia. Although among vaptans tolvaptan is well tolerated, the design of new V2R blockers reducing the reported side effects should be encouraged. Moreover, co-targeting V2R and other GPCRs known to increase intracellular calcium might be a successful approach for ADPKD treatments.
Novel AQP-targeting therapies through modulation of microRNA (miRNA) function have recently been suggested (reviewed in 122). The possibility of using miRNA alone or in combination with other drugs to modulate the vasopressin–AQP2 pathway specifically provides new hints for AQP-based therapeutics 27, 123. In this respect, the recent identification of miR-132 as a first miRNA target which blocks vasopressin gene expression has opened new avenues for drug development 124.
Abbreviations
ADPKD, autosomal dominant polycystic kidney disease; AKAP, A-kinase anchoring protein; AMPK, adenosine monophosphate kinase; AQP2, aquaporin-2; CKD, chronic kidney disease; GFR, glomerular filtration rate; GPCR, G-protein-coupled receptor; miRNA, microRNA; NDI, nephrogenic diabetes insipidus; NSIAD, nephrogenic syndrome of inappropriate antidiuresis; PKA, protein kinase A; SIADH, syndrome of inappropriate antidiuretic hormone secretion; V2R, type 2 vasopressin receptor
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Tae-Hwan Kwon, Department of Biochemistry and Cell Biology, Kyungpook National University, Taegu, South Korea
Kenichi Ishibashi, Department of Pathophysiology, Meiji Pharmaceutical University, Tokyo, Japan
Enno Klussmann, Max Delbrück Center for Molecular Medicine Berlin (MDC), Berlin, Germany
Funding Statement
This study was supported in part by Telethon funding (grant number GGP13227) and by ASI (Italian Space Agency, grant number 2013-091-R.0). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; referees: 3 approved]
References
- 1. Knepper MA, Kwon TH, Nielsen S: Molecular physiology of water balance. N Engl J Med. 2015;372(14):1349–58. 10.1056/NEJMra1404726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jung HJ, Kwon TH: Molecular mechanisms regulating aquaporin-2 in kidney collecting duct. Am J Physiol Renal Physiol. 2016;311(6):F1318–F1328. 10.1152/ajprenal.00485.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 3. Lee JW, Chou CL, Knepper MA: Deep Sequencing in Microdissected Renal Tubules Identifies Nephron Segment-Specific Transcriptomes. J Am Soc Nephrol. 2015;26(11):2669–77. 10.1681/ASN.2014111067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nedvetsky PI, Tamma G, Beulshausen S, et al. : Regulation of aquaporin-2 trafficking. Handb Exp Pharmacol. 2009; (190):133–57. 10.1007/978-3-540-79885-9_6 [DOI] [PubMed] [Google Scholar]
- 5. Rojek A, Füchtbauer EM, Kwon TH, et al. : Severe urinary concentrating defect in renal collecting duct-selective AQP2 conditional-knockout mice. Proc Natl Acad Sci U S A. 2006;103(15):6037–42. 10.1073/pnas.0511324103 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 6. Valenti G, Procino G, Tamma G, et al. : Minireview: aquaporin 2 trafficking. Endocrinology. 2005;146(12):5063–70. 10.1210/en.2005-0868 [DOI] [PubMed] [Google Scholar]
- 7. Chou CL, Yip KP, Michea L, et al. : Regulation of aquaporin-2 trafficking by vasopressin in the renal collecting duct. Roles of ryanodine-sensitive Ca 2+ stores and calmodulin. J Biol Chem. 2000;275(47):36839–46. 10.1074/jbc.M005552200 [DOI] [PubMed] [Google Scholar]
- 8. Balasubramanian L, Sham JS, Yip KP: Calcium signaling in vasopressin-induced aquaporin-2 trafficking. Pflugers Arch. 2008;456(4):747–54. 10.1007/s00424-007-0371-7 [DOI] [PubMed] [Google Scholar]
- 9. Hoffert JD, Pisitkun T, Knepper MA: Phosphoproteomics of vasopressin signaling in the kidney. Expert Rev Proteomics. 2011;8(2):157–63. 10.1586/epr.11.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Isobe K, Jung HJ, Yang CR, et al. : Systems-level identification of PKA-dependent signaling in epithelial cells. Proc Natl Acad Sci U S A. 2017;114(42):E8875–E8884. 10.1073/pnas.1709123114 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 11. Klussmann E, Tamma G, Lorenz D, et al. : An inhibitory role of Rho in the vasopressin-mediated translocation of aquaporin-2 into cell membranes of renal principal cells. J Biol Chem. 2001;276(23):20451–7. 10.1074/jbc.M010270200 [DOI] [PubMed] [Google Scholar]
- 12. Tamma G, Klussmann E, Maric K, et al. : Rho inhibits cAMP-induced translocation of aquaporin-2 into the apical membrane of renal cells. Am J Physiol Renal Physiol. 2001;281(6):F1092–101. 10.1152/ajprenal.0091.2001 [DOI] [PubMed] [Google Scholar]
- 13. Procino G, Barbieri C, Tamma G, et al. : AQP2 exocytosis in the renal collecting duct -- involvement of SNARE isoforms and the regulatory role of Munc18b. J Cell Sci. 2008;121(Pt 12):2097–106. 10.1242/jcs.022210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tamma G, Procino G, Mola MG, et al. : Functional involvement of Annexin-2 in cAMP induced AQP2 trafficking. Pflugers Arch. 2008;456(4):729–36. 10.1007/s00424-008-0453-1 [DOI] [PubMed] [Google Scholar]
- 15. Park EJ, Lim JS, Jung HJ, et al. : The role of 70-kDa heat shock protein in dDAVP-induced AQP2 trafficking in kidney collecting duct cells. Am J Physiol Renal Physiol. 2013;304(7):F958–71. 10.1152/ajprenal.00469.2012 [DOI] [PubMed] [Google Scholar]
- 16. Lu HA, Sun TX, Matsuzaki T, et al. : Heat shock protein 70 interacts with aquaporin-2 and regulates its trafficking. J Biol Chem. 2007;282(39):28721–32. 10.1074/jbc.M611101200 [DOI] [PubMed] [Google Scholar]
- 17. Schrade K, Tröger J, Eldahshan A, et al. : An AKAP-Lbc-RhoA interaction inhibitor promotes the translocation of aquaporin-2 to the plasma membrane of renal collecting duct principal cells. PLoS One. 2018;13(1):e0191423. 10.1371/journal.pone.0191423 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 18. Henn V, Edemir B, Stefan E, et al. : Identification of a novel A-kinase anchoring protein 18 isoform and evidence for its role in the vasopressin-induced aquaporin-2 shuttle in renal principal cells. J Biol Chem. 2004;279(25):26654–65. 10.1074/jbc.M312835200 [DOI] [PubMed] [Google Scholar]
- 19. Trimpert C, Wesche D, de Groot T, et al. : NDFIP allows NEDD4/NEDD4L-induced AQP2 ubiquitination and degradation. PLoS One. 2017;12(9):e0183774. 10.1371/journal.pone.0183774 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 20. Moeller HB, Olesen ET, Fenton RA: Regulation of the water channel aquaporin-2 by posttranslational modification. Am J Physiol Renal Physiol. 2011;300(5):F1062–73. 10.1152/ajprenal.00721.2010 [DOI] [PubMed] [Google Scholar]
- 21. Lee JW, Alsady M, Chou CL, et al. : Single-tubule RNA-Seq uncovers signaling mechanisms that defend against hyponatremia in SIADH. Kidney Int. 2018;93(1):128–46. 10.1016/j.kint.2017.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 22. Medvar B, Raghuram V, Pisitkun T, et al. : Comprehensive database of human E3 ubiquitin ligases: application to aquaporin-2 regulation. Physiol Genomics. 2016;48(7):502–12. 10.1152/physiolgenomics.00031.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 23. Tamma G, Ranieri M, Di Mise A, et al. : Glutathionylation of the aquaporin-2 water channel: a novel post-translational modification modulated by the oxidative stress. J Biol Chem. 2014;289(40):27807–13. 10.1074/jbc.M114.586024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sandoval PC, Claxton JS, Lee JW, et al. : Systems-level analysis reveals selective regulation of Aqp2 gene expression by vasopressin. Sci Rep. 2016;6:34863. 10.1038/srep34863 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 25. Sandoval PC, Slentz DH, Pisitkun T, et al. : Proteome-wide measurement of protein half-lives and translation rates in vasopressin-sensitive collecting duct cells. J Am Soc Nephrol. 2013;24(11):1793–805. 10.1681/ASN.2013030279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nedvetsky PI, Tabor V, Tamma G, et al. : Reciprocal regulation of aquaporin-2 abundance and degradation by protein kinase A and p38-MAP kinase. J Am Soc Nephrol. 2010;21(10):1645–56. 10.1681/ASN.2009111190 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 27. Ranieri M, Zahedi K, Tamma G, et al. : CaSR signaling down-regulates AQP2 expression via a novel microRNA pathway in pendrin and NaCl cotransporter knockout mice. FASEB J. 2018;32(4):2148–59. 10.1096/fj.201700412RR [DOI] [PubMed] [Google Scholar]
- 28. Centrone M, Ranieri M, Di Mise A, et al. : AQP2 Abundance is Regulated by the E3-Ligase CHIP Via HSP70. Cell Physiol Biochem. 2017;44(2):515–31. 10.1159/000485088 [DOI] [PubMed] [Google Scholar]
- 29. Wu Q, Moeller HB, Stevens DA, et al. : CHIP Regulates Aquaporin-2 Quality Control and Body Water Homeostasis. J Am Soc Nephrol. 2018;29(3):936–48. 10.1681/ASN.2017050526 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 30. Morgenthaler NG, Struck J, Alonso C, et al. : Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem. 2006;52(1):112–9. 10.1373/clinchem.2005.060038 [DOI] [PubMed] [Google Scholar]
- 31. Morgenthaler NG, Struck J, Jochberger S, et al. : Copeptin: clinical use of a new biomarker. Trends Endocrinol Metab. 2008;19(2):43–9. 10.1016/j.tem.2007.11.001 [DOI] [PubMed] [Google Scholar]
- 32. Szinnai G, Morgenthaler NG, Berneis K, et al. : Changes in plasma copeptin, the c-terminal portion of arginine vasopressin during water deprivation and excess in healthy subjects. J Clin Endocrinol Metab. 2007;92(10):3973–8. 10.1210/jc.2007-0232 [DOI] [PubMed] [Google Scholar]
- 33. Roussel R, Fezeu L, Marre M, et al. : Comparison between copeptin and vasopressin in a population from the community and in people with chronic kidney disease. J Clin Endocrinol Metab. 2014;99(12):4656–63. 10.1210/jc.2014-2295 [DOI] [PubMed] [Google Scholar]
- 34. de Bree FM, Burbach JP: Structure-function relationships of the vasopressin prohormone domains. Cell Mol Neurobiol. 1998;18(2):173–91. 10.1023/A:1022564803093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Balanescu S, Kopp P, Gaskill MB, et al. : Correlation of plasma copeptin and vasopressin concentrations in hypo-, iso-, and hyperosmolar States. J Clin Endocrinol Metab. 2011;96(4):1046–52. 10.1210/jc.2010-2499 [DOI] [PubMed] [Google Scholar]
- 36. Nakajima A, Lu Y, Kawano H, et al. : Association of arginine vasopressin surrogate marker urinary copeptin with severity of autosomal dominant polycystic kidney disease (ADPKD). Clin Exp Nephrol. 2015;19(6):1199–205. 10.1007/s10157-015-1101-7 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 37. Meijer E, Bakker SJ, Halbesma N, et al. : Copeptin, a surrogate marker of vasopressin, is associated with microalbuminuria in a large population cohort. Kidney Int. 2010;77(1):29–36. 10.1038/ki.2009.397 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 38. Enhörning S, Bankir L, Bouby N, et al. : Copeptin, a marker of vasopressin, in abdominal obesity, diabetes and microalbuminuria: The prospective Malmö Diet and Cancer Study cardiovascular cohort. Int J Obes (Lond). 2013;37(4):598–603. 10.1038/ijo.2012.88 [DOI] [PubMed] [Google Scholar]
- 39. Bardoux P, Bichet DG, Martin H, et al. : Vasopressin increases urinary albumin excretion in rats and humans: Involvement of V2 receptors and the renin-angiotensin system. Nephrol Dial Transplant. 2003;18(3):497–506. 10.1093/ndt/18.3.497 [DOI] [PubMed] [Google Scholar]
- 40. Fernandes S, Bruneval P, Hagege A, et al. : Chronic V2 vasopressin receptor stimulation increases basal blood pressure and exacerbates deoxycorticosterone acetate-salt hypertension. Endocrinology. 2002;143(7):2759–66. 10.1210/endo.143.7.8918 [DOI] [PubMed] [Google Scholar]
- 41. Sugiura T, Yamauchi A, Kitamura H, et al. : High water intake ameliorates tubulointerstitial injury in rats with subtotal nephrectomy: Possible role of TGF-beta. Kidney Int. 1999;55(5):1800–10. 10.1046/j.1523-1755.1999.00443.x [DOI] [PubMed] [Google Scholar]
- 42. Bankir L, Bardoux P, Ahloulay M: Vasopressin and diabetes mellitus. Nephron. 2001;87(1):8–18. 10.1159/000045879 [DOI] [PubMed] [Google Scholar]
- 43. Boertien WE, Riphagen IJ, Drion I, et al. : Copeptin, a surrogate marker for arginine vasopressin, is associated with declining glomerular filtration in patients with diabetes mellitus (ZODIAC-33). Diabetologia. 2013;56(8):1680–8. 10.1007/s00125-013-2922-0 [DOI] [PubMed] [Google Scholar]
- 44. Pikkemaat M, Melander O, Bengtsson Boström K: Association between copeptin and declining glomerular filtration rate in people with newly diagnosed diabetes. The Skaraborg Diabetes Register. J Diabetes Complicat. 2015;29(8):1062–5. 10.1016/j.jdiacomp.2015.07.006 [DOI] [PubMed] [Google Scholar]
- 45. Ponte B, Pruijm M, Ackermann D, et al. : Copeptin is associated with kidney length, renal function, and prevalence of simple cysts in a population-based study. J Am Soc Nephrol. 2015;26(6):1415–25. 10.1681/ASN.2014030260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Clark WF, Devuyst O, Roussel R: The vasopressin system: New insights for patients with kidney diseases: Epidemiological evidence and therapeutic perspectives. J Intern Med. 2017;282(4):310–21. 10.1111/joim.12654 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 47. Clark WF, Sontrop JM, Huang SH, et al. : Hydration and Chronic Kidney Disease Progression: A Critical Review of the Evidence. Am J Nephrol. 2016;43(4):281–92. 10.1159/000445959 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 48. Kwon TH, Frøkiaer J, Knepper MA, et al. : Reduced AQP1, -2, and -3 levels in kidneys of rats with CRF induced by surgical reduction in renal mass. Am J Physiol. 1998;275(5 Pt 2):F724–41. 10.1152/ajprenal.1998.275.5.F724 [DOI] [PubMed] [Google Scholar]
- 49. Teitelbaum I, McGuinness S: Vasopressin resistance in chronic renal failure. Evidence for the role of decreased V2 receptor mRNA. J Clin Invest. 1995;96(1):378–85. 10.1172/JCI118044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Palmer SC, Wong G, Iff S, et al. : Fluid intake and all-cause mortality, cardiovascular mortality and kidney function: A population-based longitudinal cohort study. Nephrol Dial Transplant. 2014;29(7):1377–84. 10.1093/ndt/gft507 [DOI] [PubMed] [Google Scholar]
- 51. Sands JM, Klein JD: Physiological insights into novel therapies for nephrogenic diabetes insipidus. Am J Physiol Renal Physiol. 2016;311(6):F1149–F1152. 10.1152/ajprenal.00418.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 52. Sands JM, Bichet DG, American College of Physicians, et al.: Nephrogenic diabetes insipidus. Ann Intern Med. 2006;144(3):186–94. 10.7326/0003-4819-144-3-200602070-00007 [DOI] [PubMed] [Google Scholar]
- 53. Bichet DG, Bockenhauer D: Genetic forms of nephrogenic diabetes insipidus (NDI): Vasopressin receptor defect (X-linked) and aquaporin defect (autosomal recessive and dominant). Best Pract Res Clin Endocrinol Metab. 2016;30(2):263–76. 10.1016/j.beem.2016.02.010 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 54. Di Iorgi N, Napoli F, Allegri AE, et al. : Diabetes insipidus--diagnosis and management. Horm Res Paediatr. 2012;77(2):69–84. 10.1159/000336333 [DOI] [PubMed] [Google Scholar]
- 55. Bedford JJ, Weggery S, Ellis G, et al. : Lithium-induced nephrogenic diabetes insipidus: Renal effects of amiloride. Clin J Am Soc Nephrol. 2008;3(5):1324–31. 10.2215/CJN.01640408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. CASTELL DO, SPARKS HA: NEPHROGENIC DIABETES INSIPIDUS DUE TO DEMETHYLCHLORTETRACYCLINE HYDROCHLORIDE. JAMA. 1965;193:237–9. 10.1001/jama.1965.03090030059024 [DOI] [PubMed] [Google Scholar]
- 57. Metzger NL, Varney Gill KL: Nephrogenic diabetes insipidus induced by two amphotericin B liposomal formulations. Pharmacotherapy. 2009;29(5):613–20. 10.1592/phco.29.5.613 [DOI] [PubMed] [Google Scholar]
- 58. Roth H, Becker KL, Shalhoub RJ, et al. : Nephrotoxicity of demethylchlortetracycline hydrochloride. A prospective study. Arch Intern Med. 1967;120(4):433–5. 10.1001/archinte.1967.04410010047006 [DOI] [PubMed] [Google Scholar]
- 59. Singer I, Rotenberg D: Demeclocycline-induced nephrogenic diabetes insipidus. In-vivo and in-vitro studies. Ann Intern Med. 1973;79(5):679–83. 10.7326/0003-4819-79-5-679 [DOI] [PubMed] [Google Scholar]
- 60. Torin DE: Nephrogenic diabetes insipidus induced by demethylchlortetracycline (Declomycin). Calif Med. 1967;107(5):420–2. [PMC free article] [PubMed] [Google Scholar]
- 61. Marples D, Frøkiaer J, Dørup J, et al. : Hypokalemia-induced downregulation of aquaporin-2 water channel expression in rat kidney medulla and cortex. J Clin Invest. 1996;97(8):1960–8. 10.1172/JCI118628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wang W, Li C, Kwon TH, et al. : AQP3, p-AQP2, and AQP2 expression is reduced in polyuric rats with hypercalcemia: prevention by cAMP-PDE inhibitors. Am J Physiol Renal Physiol. 2002;283(6):F1313–25. 10.1152/ajprenal.00040.2002 [DOI] [PubMed] [Google Scholar]
- 63. Sands JM, Flores FX, Kato A, et al. : Vasopressin-elicited water and urea permeabilities are altered in IMCD in hypercalcemic rats. Am J Physiol. 1998;274(5 Pt 2):F978–85. 10.1152/ajprenal.1998.274.5.F978 [DOI] [PubMed] [Google Scholar]
- 64. Bustamante M, Hasler U, Leroy V, et al. : Calcium-sensing receptor attenuates AVP-induced aquaporin-2 expression via a calmodulin-dependent mechanism. J Am Soc Nephrol. 2008;19(1):109–16. 10.1681/ASN.2007010092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Procino G, Mastrofrancesco L, Tamma G, et al. : Calcium-sensing receptor and aquaporin 2 interplay in hypercalciuria-associated renal concentrating defect in humans. An in vivo and in vitro study. PLoS One. 2012;7(3):e33145. 10.1371/journal.pone.0033145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Ranieri M, Tamma G, Di Mise A, et al. : Negative feedback from CaSR signaling to aquaporin-2 sensitizes vasopressin to extracellular Ca 2+. J Cell Sci. 2015;128(13):2350–60. 10.1242/jcs.168096 [DOI] [PubMed] [Google Scholar]
- 67. Tamma G, Di Mise A, Ranieri M, et al. : A decrease in aquaporin 2 excretion is associated with bed rest induced high calciuria. J Transl Med. 2014;12:133. 10.1186/1479-5876-12-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Procino G, Carmosino M, Tamma G, et al. : Extracellular calcium antagonizes forskolin-induced aquaporin 2 trafficking in collecting duct cells. Kidney Int. 2004;66(6):2245–55. 10.1111/j.1523-1755.2004.66036.x [DOI] [PubMed] [Google Scholar]
- 69. Qureshi S, Galiveeti S, Bichet DG, et al. : Diabetes insipidus: celebrating a century of vasopressin therapy. Endocrinology. 2014;155(12):4605–21. 10.1210/en.2014-1385 [DOI] [PubMed] [Google Scholar]
- 70. Monnens L, Jonkman A, Thomas C: Response to indomethacin and hydrochlorothiazide in nephrogenic diabetes insipidus. Clin Sci (Lond). 1984;66(6):709–15. [DOI] [PubMed] [Google Scholar]
- 71. Milano S, Carmosino M, Gerbino A, et al. : Hereditary Nephrogenic Diabetes Insipidus: Pathophysiology and Possible Treatment. An Update. Int J Mol Sci. 2017;18 (11): pii: E2385. 10.3390/ijms18112385 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 72. Bockenhauer D, Bichet DG: Nephrogenic diabetes insipidus. Curr Opin Pediatr. 2017;29(2):199–205. 10.1097/MOP.0000000000000473 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 73. Ando F, Uchida S: Activation of AQP2 water channels without vasopressin: therapeutic strategies for congenital nephrogenic diabetes insipidus. Clin Exp Nephrol. 2018;22(3):501–7. 10.1007/s10157-018-1544-8 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 74. Sanches TR, Volpini RA, Massola Shimizu MH, et al. : Sildenafil reduces polyuria in rats with lithium-induced NDI. Am J Physiol Renal Physiol. 2012;302(1):F216–25. 10.1152/ajprenal.00439.2010 [DOI] [PubMed] [Google Scholar]
- 75. Assadi F, Sharbaf FG: Sildenafil for the Treatment of Congenital Nephrogenic Diabetes Insipidus. Am J Nephrol. 2015;42(1):65–9. 10.1159/000439065 [DOI] [PubMed] [Google Scholar]
- 76. Sidaway JE, Davidson RG, McTaggart F, et al. : Inhibitors of 3-hydroxy-3-methylglutaryl-CoA reductase reduce receptor-mediated endocytosis in opossum kidney cells. J Am Soc Nephrol. 2004;15(9):2258–65. 10.1097/01.ASN.0000138236.82706.EE [DOI] [PubMed] [Google Scholar]
- 77. Procino G, Barbieri C, Carmosino M, et al. : Fluvastatin modulates renal water reabsorption in vivo through increased AQP2 availability at the apical plasma membrane of collecting duct cells. Pflugers Arch. 2011;462(5):753–66. 10.1007/s00424-011-1007-5 [DOI] [PubMed] [Google Scholar]
- 78. Li W, Zhang Y, Bouley R, et al. : Simvastatin enhances aquaporin-2 surface expression and urinary concentration in vasopressin-deficient Brattleboro rats through modulation of Rho GTPase. Am J Physiol Renal Physiol. 2011;301(2):F309–18. 10.1152/ajprenal.00001.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Procino G, Milano S, Carmosino M, et al. : Combination of secretin and fluvastatin ameliorates the polyuria associated with X-linked nephrogenic diabetes insipidus in mice. Kidney Int. 2014;86(1):127–38. 10.1038/ki.2014.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Elie D, Segal M, Low NC, et al. : Statins in the prevention of lithium-associated diabetes insipidus: preliminary findings. Kidney Int. 2015;87(4):862. 10.1038/ki.2014.409 [DOI] [PubMed] [Google Scholar]
- 81. Procino G: Fluvastatin Increases AQP2 Urine Excretion in a Dyslipidemic Patient with Nephrogenic Diabetes Insipidus: An In Vivo and In Vitro Study. J Diabetes Metab. 2014;5:408 10.4172/2155-6156.1000408 [DOI] [Google Scholar]
- 82. Efe O, Klein JD, LaRocque LM, et al. : Metformin improves urine concentration in rodents with nephrogenic diabetes insipidus. JCI Insight. 2016;1(11): pii: e88409. 10.1172/jci.insight.88409 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 83. Klein JD, Wang Y, Blount MA, et al. : Metformin, an AMPK activator, stimulates the phosphorylation of aquaporin 2 and urea transporter A1 in inner medullary collecting ducts. Am J Physiol Renal Physiol. 2016;310(10):F1008–12. 10.1152/ajprenal.00102.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 84. Ando F, Mori S, Yui N, et al. : AKAPs-PKA disruptors increase AQP2 activity independently of vasopressin in a model of nephrogenic diabetes insipidus. Nat Commun. 2018;9(1):1411. 10.1038/s41467-018-03771-2 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 85. Bouley R, Lu HA, Nunes P, et al. : Calcitonin has a vasopressin-like effect on aquaporin-2 trafficking and urinary concentration. J Am Soc Nephrol. 2011;22(1):59–72. 10.1681/ASN.2009121267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Kwon TH, Nielsen J, Knepper MA, et al. : Angiotensin II AT 1 receptor blockade decreases vasopressin-induced water reabsorption and AQP2 levels in NaCl-restricted rats. Am J Physiol Renal Physiol. 2005;288(4):F673–84. 10.1152/ajprenal.00304.2004 [DOI] [PubMed] [Google Scholar]
- 87. Li C, Wang W, Rivard CJ, et al. : Molecular mechanisms of angiotensin II stimulation on aquaporin-2 expression and trafficking. Am J Physiol Renal Physiol. 2011;300(5):F1255–61. 10.1152/ajprenal.00469.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Olesen ET, Rützler MR, Moeller HB, et al. : Vasopressin-independent targeting of aquaporin-2 by selective E-prostanoid receptor agonists alleviates nephrogenic diabetes insipidus. Proc Natl Acad Sci U S A. 2011;108(31):12949–54. 10.1073/pnas.1104691108 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 89. Gao M, Cao R, Du S, et al. : Disruption of prostaglandin E2 receptor EP4 impairs urinary concentration via decreasing aquaporin 2 in renal collecting ducts. Proc Natl Acad Sci U S A. 2015;112(27):8397–402. 10.1073/pnas.1509565112 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 90. Olesen ET, Moeller HB, Assentoft M, et al. : The vasopressin type 2 receptor and prostaglandin receptors EP2 and EP4 can increase aquaporin-2 plasma membrane targeting through a cAMP-independent pathway. Am J Physiol Renal Physiol. 2016;311(5):F935–F944. 10.1152/ajprenal.00559.2015 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 91. Ando F, Sohara E, Morimoto T, et al. : Wnt5a induces renal AQP2 expression by activating calcineurin signalling pathway. Nat Commun. 2016;7:13636. 10.1038/ncomms13636 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 92. Hannon MJ, Thompson CJ: The syndrome of inappropriate antidiuretic hormone: prevalence, causes and consequences. Eur J Endocrinol. 2010;162 Suppl 1:S5–12. 10.1530/EJE-09-1063 [DOI] [PubMed] [Google Scholar]
- 93. Schrier RW, Sharma S, Shchekochikhin D: Hyponatraemia: more than just a marker of disease severity? Nat Rev Nephrol. 2013;9(1):37–50. 10.1038/nrneph.2012.246 [DOI] [PubMed] [Google Scholar]
- 94. Gheorghiade M, Abraham WT, Albert NM, et al. : Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J. 2007;28(8):980–8. 10.1093/eurheartj/ehl542 [DOI] [PubMed] [Google Scholar]
- 95. Anderson RJ, Chung HM, Kluge R, et al. : Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med. 1985;102(2):164–8. 10.7326/0003-4819-102-2-164 [DOI] [PubMed] [Google Scholar]
- 96. Ecelbarger CA, Nielsen S, Olson BR, et al. : Role of renal aquaporins in escape from vasopressin-induced antidiuresis in rat. J Clin Invest. 1997;99(8):1852–63. 10.1172/JCI119352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Ecelbarger CA, Chou CL, Lee AJ, et al. : Escape from vasopressin-induced antidiuresis: role of vasopressin resistance of the collecting duct. Am J Physiol. 1998;274(6 Pt 2):F1161–6. 10.1152/ajprenal.1998.274.6.F1161 [DOI] [PubMed] [Google Scholar]
- 98. Kim S, Choi HJ, Jo CH, et al. : Cyclophosphamide-induced vasopressin-independent activation of aquaporin-2 in the rat kidney. Am J Physiol Renal Physiol. 2015;309(5):F474–83. 10.1152/ajprenal.00477.2014 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 99. Robertson GL: Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis. Am J Med. 2006;119(7 Suppl 1):S36–42. 10.1016/j.amjmed.2006.05.006 [DOI] [PubMed] [Google Scholar]
- 100. Cuesta M, Thompson CJ: The syndrome of inappropriate antidiuresis (SIAD). Best Pract Res Clin Endocrinol Metab. 2016;30(2):175–87. 10.1016/j.beem.2016.02.009 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 101. Berl T, Quittnat-Pelletier F, Verbalis JG, et al. : Oral tolvaptan is safe and effective in chronic hyponatremia. J Am Soc Nephrol. 2010;21(4):705–12. 10.1681/ASN.2009080857 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 102. Tamma G, Di Mise A, Ranieri M, et al. : The V2 receptor antagonist tolvaptan raises cytosolic calcium and prevents AQP2 trafficking and function: an in vitro and in vivo assessment. J Cell Mol Med. 2017;21(9):1767–80. 10.1111/jcmm.13098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Tradtrantip L, Jin BJ, Yao X, et al. : Aquaporin-Targeted Therapeutics: State-of-the-Field. Adv Exp Med Biol. 2017;969:239–50. 10.1007/978-94-024-1057-0_16 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 104. Feldman BJ, Rosenthal SM, Vargas GA, et al. : Nephrogenic syndrome of inappropriate antidiuresis. N Engl J Med. 2005;352(18):1884–90. 10.1056/NEJMoa042743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Rosenthal W, Seibold A, Antaramian A, et al. : Mutations in the vasopressin V2 receptor gene in families with nephrogenic diabetes insipidus and functional expression of the Q-2 mutant. Cell Mol Biol (Noisy-le-grand). 1994;40(3):429–36. [PubMed] [Google Scholar]
- 106. Carpentier E, Greenbaum LA, Rochdi D, et al. : Identification and characterization of an activating F229V substitution in the V2 vasopressin receptor in an infant with NSIAD. J Am Soc Nephrol. 2012;23(10):1635–40. 10.1681/ASN.2012010077 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 107. Erdélyi LS, Mann WA, Morris-Rosendahl DJ, et al. : Mutation in the V2 vasopressin receptor gene, AVPR2, causes nephrogenic syndrome of inappropriate diuresis. Kidney Int. 2015;88(5):1070–8. 10.1038/ki.2015.181 [DOI] [PubMed] [Google Scholar]
- 108. Tiulpakov A, White CW, Abhayawardana RS, et al. : Mutations of Vasopressin Receptor 2 Including Novel L312S Have Differential Effects on Trafficking. Mol Endocrinol. 2016;30(8):889–904. 10.1210/me.2016-1002 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 109. Decaux G, Vandergheynst F, Bouko Y, et al. : Nephrogenic syndrome of inappropriate antidiuresis in adults: high phenotypic variability in men and women from a large pedigree. J Am Soc Nephrol. 2007;18(2):606–12. 10.1681/ASN.2006090987 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 110. Harris PC, Torres VE: Genetic mechanisms and signaling pathways in autosomal dominant polycystic kidney disease. J Clin Invest. 2014;124(6):2315–24. 10.1172/JCI72272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Zittema D, Boertien WE, van Beek AP, et al. : Vasopressin, copeptin, and renal concentrating capacity in patients with autosomal dominant polycystic kidney disease without renal impairment. Clin J Am Soc Nephrol. 2012;7(6):906–13. 10.2215/CJN.11311111 [DOI] [PubMed] [Google Scholar]
- 112. Gabow PA, Kaehny WD, Johnson AM, et al. : The clinical utility of renal concentrating capacity in polycystic kidney disease. Kidney Int. 1989;35(2):675–80. 10.1038/ki.1989.38 [DOI] [PubMed] [Google Scholar]
- 113. Chebib FT, Perrone RD, Chapman AB, et al. : A Practical Guide for Treatment of Rapidly Progressive ADPKD with Tolvaptan. J Am Soc Nephrol. 2018;29(10):2458–70. 10.1681/ASN.2018060590 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 114. van Gastel MDA, Torres VE: Polycystic Kidney Disease and the Vasopressin Pathway. Ann Nutr Metab. 2017;70 Suppl 1:43–50. 10.1159/000463063 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 115. Ong AC, Harris PC: A polycystin-centric view of cyst formation and disease: the polycystins revisited. Kidney Int. 2015;88(4):699–710. 10.1038/ki.2015.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Chebib FT, Sussman CR, Wang X, et al. : Vasopressin and disruption of calcium signalling in polycystic kidney disease. Nat Rev Nephrol. 2015;11(8):451–64. 10.1038/nrneph.2015.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Torres VE, Chapman AB, Devuyst O, et al. : Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2012;367(25):2407–18. 10.1056/NEJMoa1205511 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 118. Di Mise A, Tamma G, Ranieri M, et al. : Activation of Calcium-Sensing Receptor increases intracellular calcium and decreases cAMP and mTOR in PKD1 deficient cells. Sci Rep. 2018;8(1):5704. 10.1038/s41598-018-23732-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Di Mise A, Ranieri M, Centrone M, et al. : Activation of the Calcium-Sensing Receptor Corrects the Impaired Mitochondrial Energy Status Observed in Renal Polycystin-1 Knockdown Cells Modeling Autosomal Dominant Polycystic Kidney Disease. Front Mol Biosci. 2018;5:77. 10.3389/fmolb.2018.00077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Happé H, Peters DJ: Translational research in ADPKD: lessons from animal models. Nat Rev Nephrol. 2014;10(10):587–601. 10.1038/nrneph.2014.137 [DOI] [PubMed] [Google Scholar]
- 121. Devuyst O, Chapman AB, Gansevoort RT, et al. : Urine Osmolality, Response to Tolvaptan, and Outcome in Autosomal Dominant Polycystic Kidney Disease: Results from the TEMPO 3:4 Trial. J Am Soc Nephrol. 2017;28(5):1592–602. 10.1681/ASN.2016040448 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 122. Gomes A, da Silva IV, Rodrigues CMP, et al. : The Emerging Role of microRNAs in Aquaporin Regulation. Front Chem. 2018;6:238. 10.3389/fchem.2018.00238 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 123. Kim JE, Jung HJ, Lee YJ, et al. : Vasopressin-regulated miRNAs and AQP2-targeting miRNAs in kidney collecting duct cells. Am J Physiol Renal Physiol. 2015;308(7):F749–64. 10.1152/ajprenal.00334.2014 [DOI] [PubMed] [Google Scholar]
- 124. Bijkerk R, Trimpert C, van Solingen C, et al. : MicroRNA-132 controls water homeostasis through regulating MECP2-mediated vasopressin synthesis. Am J Physiol Renal Physiol. 2018;315(4):F1129–F1138. 10.1152/ajprenal.00087.2018 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation