Abstract
Objective
To systematically review outcomes for cautery-assisted palatal stiffening operation (CAPSO) as a treatment for adult obstructive sleep apnea (OSA).
Methods
Five databases (including PubMed/MEDLINE) were searched through July 12, 2017.
Results
Eight studies (307 patients) met criteria. Overall, CAPSO alone (80 patients) improved AHI from a mean ± standard deviation (M ± SD) of (16.8 ± 11.9) to (9.9 ± 10.9) events/h (41.1% decrease). Mixed CAPSO with/without tonsillectomy (92 patients) improved AHI from a M ± SD of (24.8 ± 12.6) to (10.6 ± 9.5) events/h (61.7% decrease). CAPSO with expansion pharyngoplasty (EP), (78 patients) improved AHI from a M ± SD of (26.3 ± 17.7) to (12.6 ± 5.8) events/h (52.1% decrease). CAPSO alone (90 patients) improved lowest oxygen saturation (LSAT) by 5.4 points. Mixed CAPSO with/without tonsillectomy (77 patients) improved LSAT by 10.6 points, and CAPSO with EP (78 patients) improved LSAT by 5.2 points. Sleepiness improved (182 patients) from an Epworth Sleepiness Scale score of 11.8 to 5.1, P < 0.001. Snoring reduced (120 patients) from 7.9 to 2.5 on visual analog scales (0–10 scale), P < 0.001.
Conclusions
Apnea-hypopnea index has improved by 41.0% for CAPSO alone, 61.7% for CAPSO with tonsillectomy and 52.1% for CAPSO with expansion pharyngoplasty. Additionally, lowest oxygen saturation, sleepiness and snoring have also improved after CAPSO.
Keywords: Surgery, Sleep apnea syndromes, Systematic review, Meta-analysis
Introduction
Obstructive sleep apnea (OSA) is a disorder that is caused by complete or partial obstructions of the upper airway, often at multiple levels (retropalatal, retrolingual, or nasal cavity). OSA is defined by the presence of at least 5 obstructive respiratory events (apneas, hypopneas, or respiratory effort related arousals) per hour of sleep and usually results in reduced blood oxygen saturation that subsequently causes increased sympathetic activity, hypertension, and daytime somnolence. Up to 4% of adults are believed to have OSA with additional symptoms, most commonly middle aged males, though up to 20% of American adults are believed to have at least mild OSA if formally studied in a sleep lab by polysomnography.1, 2, 3 If left untreated, OSA has been associated with a wide range of comorbidities to include cardiovascular disorders, neurocognitive dysfunction, and mortality.4, 5
Cautery-assisted palatal stiffening operation (CAPSO) is a simple, single-stage procedure for the treatment of both snoring and OSA. It was first introduced formally by Mair and was subsequently modified by Pang.6, 7, 8 The operation can be performed under local anesthetic or with general anesthesia. CAPSO consists of denuding a portion of the anterior aspect of the soft palate with a blended cautery and then cauterizing the denuded tissue to further stiffen it for hemostasis and healing by secondary intention, with or without primary closure of the mucosa.9 CAPSO has been performed with and without tonsillectomy and recently in conjunction with expansion pharyngoplasty. The goal of CAPSO and other palatal surgical procedures is to enlarge the retropalatal space by providing scar tissue which stiffens the soft palate and produces fibrosis and produces anterior displacement of the soft palate.
CAPSO has been suggested as a viable alternative to other, more invasive surgical modalities for the treatment of OSA such as uvulopalatopharyngoplasty (UPPP), laser-assisted uvuloplasty (LAUP), and radiofrequency ablation (RFA) due to the significant complications associated with these interventions as well as the requirement for general anesthesia, expensive equipment, and multiple-stage operations. CAPSO has been reported to be less painful than many other procedures.10 CAPSO has been shown to be an effective procedure for the prevention of snoring,11, 12, 13 and has been used to treat OSA.
Therefore, the objective of this study is to systematically review all international publications reporting polysomnography data for CAPSO as treatment for adult patients with OSA, followed by a meta-analysis of the data obtained, particularly apnea-hypopnea index (AHI) and lowest oxygen saturation (LSAT). In order to fully evaluate the effect of CAPSO, a meta-analysis evaluating CAPSO with and without tonsillectomy and/or in conjunction with expansion pharyngoplasty is necessary, and the outcomes should be compared between these groups. Therefore, the study inclusion criteria were as follows using the PICOS acronym: (1) Patients: any adult patient (≥18 years old) with OSA; (2) Intervention: CAPSO; (3) Comparison: polysomnography data pre-surgical and post-surgical; (4) Outcomes: AHI, LSAT, Epworth sleepiness scale (ESS), visual analog scale (VAS), respiratory disturbance index (RDI); (5) Study design: any study design from case reports through randomized controlled-trials.
Methods
Protocol
The Tripler Army Medical Center approved this study via the protocol TAMC 16N14.
Study eligibility criteria
Studies were included without any limitations placed on year of publication, country, or language. For purposes of study eligibility, inclusion criteria are: (1) Adult patients with sleep disordered breathing; (2) Outcomes for sleep study information, snoring and/or sleepiness; (3) Anterior palatoplasty or palatal stiffening operation or CAPSO or modified CAPSO with or without tonsillectomy/expansion pharyngoplasty (plication of palatopharyngeus). Studies were excluded if other surgical procedures were performed at the same time, such as: (1) Laser-assisted uvuloplasty or laser-assisted UPPP; (2) UPPP; (3) Lateral pharyngoplasty; (4) Pillar implants; (5) Z-palatoplasty or z-palatopharyngoplasty; (6) Sclerosing agents for palatal stiffening; (7) Radiofrequency ablation of the soft palate; (8) Transpalatal advancement pharyngoplasty.
Information sources
The five databases searched during this study included Google Scholar, PubMed/MEDLINE, The Cochrane Library, Scopus, and Embase. Searches were conducted between the dates of December 5, 2016 and July 12, 2017. Each database was individually searched from its initiation.
Search strategy
The search strategies were tailored to each specific database, the search used in PubMed/MEDLINE included: ((“Cautery-assisted palatal stiffening operation”) OR (“palatoplast*” OR “uvuloplast*” OR “palatal stiffening”) OR (“cauter*” and “anterior palatoplast*”)).
Study selection and data collection
Three authors (C.L., M.C. and R.A.) independently searched the international literature for relevant studies to include in this review. Titles and abstracts were first reviewed and studies with potentially applicable material were then downloaded in full text form. Once downloaded, each manuscript was independently reviewed by at least two co-authors to ensure inclusion criteria were met. Data was then extracted from each article and documented in a table according to year published. The data extrapolated from each study included total number of subjects, ages, body mess indexsBMIs, and all pre- and post-operative data measured (AHIs, LSATs, ESSs, VASs, etc.). If a study did not report all the data necessary for inclusion in the meta-analysis, or if there was an unresolvable discrepancy in the data, then the authors were contacted using the information provided in the manuscript. The methods section for each manuscript was reviewed in detail to ensure that there were different patient populations within each manuscript and if there was a possibility of overlapping timeframes or patients, then the plan was to contact the authors at least twice for more information.
Data items
If multiple follow-up polysomnography measurements were provided by a study, then the most recent data was used as long as no additional surgeries had been performed.
Summary measures
Summary measures included the weighted mean differences (MD) and the standardized mean differences (SMD). The associated 95% confidence intervals (95%CI) were also calculated based on the data. The magnitudes of effect for SMD were assigned using Cohen's guidelines as small = 0.2, medium = 0.5, and large = 0.8.14
Heterogeneity and risk of bias
For the meta-analysis, Review Manager Software (REVMAN) version 5.3 (Copenhagen: The Nordic Cochrane Centre: The Cochrane Collaboration, 2014) was used for data analysis. REVMAN was used to calculate the Cochrane Q statistic (Q statistic), and based on previously published studies a value ≤ 0.10 was deemed statistically significant.15 Another measure of heterogeneity (inconsistency) was calculated by REVMAN as well (I2 statistic), and values were defined as follows: 25% (low), 50% (moderate) and 75% (high) levels of inconsistency.16 We used the recommendations given by the Cochrane Collaboration and evaluate the REVMAN funnel plots using visual inspection for the risk of bias if 10 or more studies reported outcomes for a specific variable.
Sensitivity analysis
After performing the meta-analysis and calculating the Q statistic and I2 statistic, if there was heterogeneity, then a sensitivity analysis was performed in order to identify which study or studies were responsible.
Results
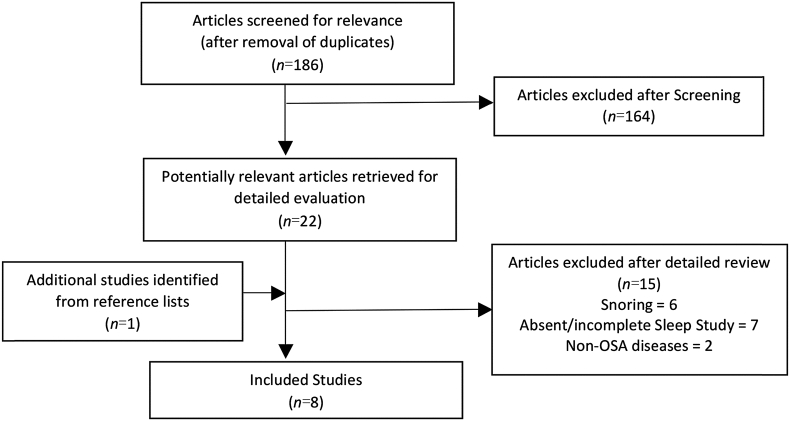
The search strategy generated 186 studies, of which 23 were found to discuss cautery techniques or encompass potentially relevant data, and were subsequently downloaded in their full versions. From this collection, studies were further excluded if they lacked objective pre- and post-operative polysomnography data or were designed to treat snoring alone or some other non-OSA disease. Overall, 8 articles met inclusion and exclusion criteria.7, 8, 17, 18, 19, 20, 21, 22 Fig. 1 demonstrates the exclusions at each stage of the process.
Figure 1.
Flow diagram demonstrating literature search, study inclusion and exclusion.
The QUADAS-2 Tool23 was used to evaluate the quality of each study and Table 1 provides the results. For the three studies by Pang et al,7, 8, 18 the 2007 study was a prospective case series evaluating snoring/sleep sub-specialty clinics over an 18-month period, the 2009 study was a non-randomized prospective multicenter (Singapore, Malaysia, USA) trial evaluating 77 consecutive patients, and the 2016 study was a non-randomized prospective dual-center (Singapore and Italy) evaluating 73 consecutive patients.
Table 1.
Quality criteria of included studies according to QUADAS-2 assessment tool.
| Study | Risk of bias |
Applicability concerns |
|||||
|---|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard | |
| Bayir 201617 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Pang 201618 | Low risk | Low risk | Low risk | High risk | Low risk | Low risk | Low risk |
| Selcuk 201719 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Marzetti 201320 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ugur 201421 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Pang 20097 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Pang 20078 | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Wassmuth 200022 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
AHI
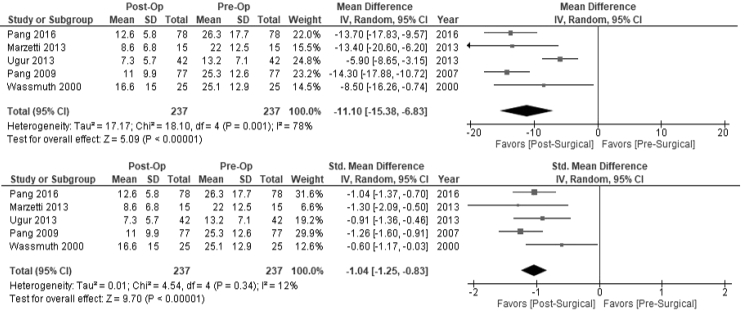
Meta-analysis of the five studies with AHI data demonstrated a reduced AHI (237 patients) from a preoperative mean ± standard deviation (M ± SD) of (21.56 ± 14.90) to (11.31 ± 8.98) events/h (47.54% decrease). A sub-analysis using random effects modeling was performed on the five studies with AHI data (237 patients), and there was an AHI MD of −11.10 events/h [95%CI -15.38, −6.38], overall effect (Z) = 5.09, P < 0.001, Q statistic P = 0.001 (heterogeneity present), I2 = 78% (high inconsistency). The sensitivity analysis demonstrated that after removal of the study Ugur et al21(2014), MD revealed no heterogeneity (Q statistic P = 0.62) or inconsistency (I2 = 0), see Fig. 2.
Figure 2.
Mean Difference in AHI Pre- and Post-CAPSO, with 95%CI (Top); Standardized Mean Difference in AHI pre- and post-CAPSO, with 95%CI (Bottom). AHI: apnea-hypopnea index; CAPSO: cautery-assisted palatal stiffening operation.
The AHI SMD was −1.04 [95%CI -1.25, −0.83] (large magnitude of effect), overall effect Z = 5.49, P < 0.001, Q statistic P = 0.34 (no heterogeneity present), I2 = 12% (low inconsistency) presented in Table 2. Sensitivity Analysis demonstrated that the inconsistency dropped to 0% if Pang et al7(2009) and/or Wassmuth et al22(2000) were removed (Fig. 2).
Table 2.
Polysomnographic data pre- and Post-CAPSO surgery.
| Study Authors Year | Surg | N | Age | BMI(kg/m2) | Pre-Op AHI/RDI (events/h | Post-Op AHI/RDI (events/h | AHI/RDI percent Change (%) | Pre-Op LSAT | Post-Op LSAT(%) |
|---|---|---|---|---|---|---|---|---|---|
| Bayir 201617 | M | 35 | 43.86 ± 7.18 | 29.19 ± 3.66 | 11.93 ± 7.71a | 10.20 ± 8.53a | −14.5a | 86.1 ± 3.89 | 87.8 ± 2.85 |
| Pang 201618 | CE | 78 | 46.8 (25–67) | 25.5 (20.3–31.2) | 26.3 ± 17.7 | 12.6 ± 5.8 | −52.1 | 83.8 ± 8.2 | 89.0 ± 3.6 |
| Selcuk 201719 | C | 22 | 48.22 ± 9.23 | 25.85 ± 2.57 | 14.50 ± 9.99 | – | – | – | – |
| Marzetti 201320 | M | 15 | 48.3 ± 10.2 | 26.5 ± 2.4 | 22 ± 12.5 | 8.6 ± 6.8 | −61.0 | – | – |
| Ugur 201421 | C | 42 | 39.2 ± 7.6 | 28.5 (24.8–31.6) | 13.2 ± 7.1 | 7.3 ± 5.7 | −44.7 | 75.8 ± 20.0 | 84.7 ± 5.8 |
| Pang 20097 | M | 77 | 39.3 (21–51) | 24.9 (20.7–26.8) | 25.3 ± 12.6 | 11.0 ± 9.9 | −56.5 | 81.4 ± 19.2 | 92.0 ± 16.9 |
| Pang 20078 | C | 13 | 24–47 | 28.4 (21.6–31.2) | 12.3 | 5.2 | −57.7 | 88.30 | 92.50 |
| Wassmuth 200022 | C | 25 | 22–69 | 28.6 ± 3.0 | 25.1 ± 12.9 | 16.6 ± 15.0 | −33.9 | – | – |
| Total | 307 | 43.3 ± 9.3 | 26.63 ± 3.65 | 21.56 ± 14.90 | 11.31 ± 8.98 | −47.54 | 82.24 ± 15.13 | 89.22 ± 10.59 |
Oxygen Desaturation Index; AHI: Apnea/hypopnea Index; CAPSO: Cautery-Assisted Palatal Stiffening Operation; RDI: Respiratory Disturbance Index; LSAT: Lowest oxygen saturation. N: Number; Surg: Surgery Type (C: CAPSO alone, CE: CAPSO with expansion pharyngoplasty and M: mixed CAPSO alone or with tonsillectomy or expansion pharyngoplasty).
CAPSO alone
A sub-analysis for patients who underwent CAPSO alone without any other intervention demonstrated that the patients had a reduction in their AHI (80 patients) from a M ± SD of (16.8 ± 11.9) to (9.9 ± 10.9) events/h (41.1% decrease).
Mixed CAPSO with/without tonsillectomy
A sub-analysis for patients who underwent CAPSO with tonsillectomy demonstrated that the patients had a reduction in their AHI (92 patients) from a M ± SD of (24.8 ± 12.6) to (10.6 ± 9.5) events/h (61.7% decrease).
CAPSO with expansion pharyngoplasty
The outcomes for patients who underwent CAPSO with expansion pharyngoplasty demonstrated that the patients had a reduction in their AHI (78 patients) from a M ± SD of (26.3 ± 17.7) to (12.6 ± 5.8) events/h (52.1% decrease).
Oxygen desaturation index (ODI)
The ODI was reported by Bayir et al17 (2016). Overall, the ODI decreased from a M ± SD of (11.93 ± 7.71) to (10.20 ± 8.53) events/h (a 14.5% reduction). In 20 patients, the ODI improved overall, from a M ± SD of (11.76 ± 9.04) to (6.77 ± 5.36) events/h (a 42.4% reduction). However, in 15 unsuccessful patients, the ODI worsened overall, from a M ± SD of (12.17 ± 5.77) to (14.78 ± 9.92) events/h (a 21.4% increase).
Lowest oxygen saturation
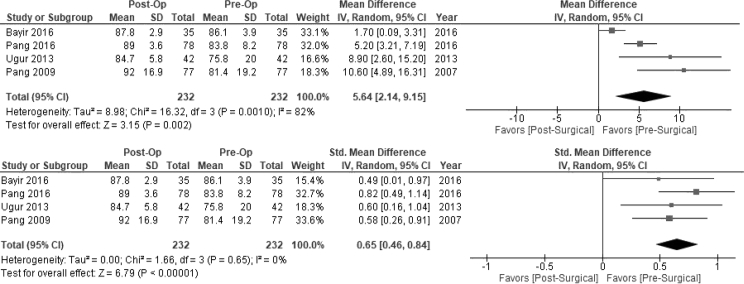
The LSAT (232 patients) increased from a preoperative M ± SD of 82.24% ± 15.13%–89.22% ± 10.59% (Table 2). A sub-analysis using random effects modeling was performed on the four studies with LSAT data (232 patients), and there was an LSAT MD of 5.64% (95%CI 2.14, 9.15), overall effect (Z) = 3.15, P = 0.002, Q statistic P = 0.001 (heterogeneity present), I2 = 82% (high inconsistency). Sensitivity analysis demonstrated that after removal of the study Bayir et al17(2016) and Pang et al18(2016), MD revealed no heterogeneity (Q statistic P = 0.70) or inconsistency (I2 = 0), see Fig. 3.
Figure 3.
Mean Difference in LSAT Pre- and Post-CAPSO, with 95%CI (Top); Standardized Mean Difference in LSAT pre- and post-CAPSO, with 95%CI (Bottom). Abbreviations: LSAT = lowest oxygen saturation; CAPSO = cautery-assisted palatal stiffening operation.
The LSAT SMD was 0.65 (95%CI 0.46, 0.84, moderate magnitude of effect), overall effect Z = 6.79, P < 0.001, Q statistic P = 0.65 (no heterogeneity present), I2 = 0 (no inconsistency) (Fig. 3).
CAPSO alone
A sub-analysis for patients who underwent CAPSO alone without any other intervention demonstrated that the patients had an increase in the LSAT (90 patients) from a M ± SD of (81.6 ± 15.9) to (87.0 ± 6.4) events/h (5.4 oxygen saturation point increase).
Mixed CAPSO with/without tonsillectomy
A sub-analysis for patients who underwent CAPSO with tonsillectomy demonstrated that the patients had an increase in the LSAT (77 patients) from a M ± SD of (81.4 ± 19.2) to (92.0 ± 16.9) events/h (10.6 oxygen saturation point increase).
CAPSO with expansion pharyngoplasty
The outcomes for patients who underwent CAPSO with expansion pharyngoplasty demonstrated that the patients had an increase in the LSAT (78 patients) from a M ± SD of (83.8 ± 8.2) to (89.0 ± 3.6) events/h (5.2 oxygen saturation point increase).
Sleepiness
A total of 272 patients had sleepiness data and of these 182 provided M ± SDs. The combined pre-operative M ± SD for ESS was 11.8 ± 4.1 and the combined post-operative M ± SD for ESS was 5.1 ± 4.0, P < 0.001 (95%CI 5.87, 7.54).
Arousals
Only Ugur et al21 offered any discussion of arousals as objectively measured by a PSG. They reported the total number of spontaneous arousals in 1 h as the arousal index (ARI) with preoperative M ± SD of 15.7 ± 7.7 and postoperative M ± SD of 11.7 ± 6.4 for a statistically significant P-value of 0.023.
Complications
Our review of the literature revealed four main complications to consider in palatal procedures: (1) pain, (2) bleeding, (3) velopharyngeal insufficiency (VPI) and (4) globus sensation/inability to clear phlegm.
Postoperative pain was the most common complaint and frequently measured using a VAS ranging from 0 (no problem) to 10 (excruciating pain with extreme difficulty speaking/swallowing). The VAS were completed multiple times throughout the first 2 weeks postoperatively and revealed a maximum amount of pain between postoperative days 2–5. Pang 2007 et al8 (reported a mean pain score of 8.6 (range 7.3–9.1) with a maximum on day 2 and improving to a mean of 2.2 (range 1.8–3.6) by day 14. Ugur et al21 reported a mean pain score of 6 for the first 3 postoperative days which decreased to a mean of 1 by day 14. Marzetti et al20 reported a mean pain score of 5.1 during the first 3 days and an average duration of 7.1 days.
While bleeding and VPI are certainly more serious complications, they rarely if ever occurred in the studies examined. Ugur et al21 reported 4 patients (9.5%) with nasal regurgitation of liquids on swallowing during the first postoperative week, but this symptom resolved by 6 weeks. They did not observe any postoperative bleeding or long-term VPI. They did find that 16 patients (38%) had globus sensation and inability to clear phlegm 2 years after the operation. Wassmuth et al22 had no return visits for bleeding, dehydration, or subjective symptoms of VPI (temporary or long-term) elicited on direct patient questioning. Both Pang et al7(2009) and Marzetti et al20 also reported no complications to include velopharyngeal incompetence, oronasal fistula, or primary or secondary hemorrhage.
Visual analog scale for snoring
A total of 210 patients had snoring data and of these 120 provided M ± SDs. The combined pre-operative M ± SD for VAS was 7.9 ± 5.1 and the combined post-operative M ± SD for VAS was 2.5 ± 4.6, P < 0.001 (95%CI 4.17–6.64).
Risk of bias
None of the variables had at least 10 studies reporting outcomes; therefore, funnel plots and risk of bias was not performed.
Discussion
There are three main findings in this systematic review and meta-analysis. First, this study shows that CAPSO has improved respiratory parameters in OSA patients. The compiled results of eight separate studies using respiratory parameters during polysomnography have demonstrated the improvement. The systematic review provided a total of 307 patients with data available for meta-analysis. Overall, CAPSO reduced the AHI M ± SD by approximately 50% from a pre to post-operative value of (21.6 ± 14.9) to (11.3 ± 9.0) events/h. The AHI standardized mean difference provides us with information as to how large the magnitude of effect was and at a value of −1.04 [95%CI -1.25, −0.83], this is a large magnitude of effect. A 50% reduction is clinically significant given that patients can undergo an isolated CAPSO in the clinic, using local anesthetic. Studies by Selcuk et al,19 Ugur et al,21 Pang et al7, 8, 18 and Wassmuth et al22 provide outcomes for 102 patients who underwent CAPSO alone. When the CAPSO procedures were performed alone (without tonsillectomy or expansion pharyngoplasty) the AHI still improved by 41% from 21.6 to 11.3 events/h which is taking a patient on average from moderate OSA down to mild OSA. There was a significant improvement in the AHI when tonsillectomy was added (61.7% reduction in AHI). There are only a few surgical interventions that can be performed in clinic and can have a significant reduction in the AHI.
Second, the lowest oxygen saturation improved from a preoperative value of 82% to a post-operative value of 89% (a 7% increase). An improvement of 7% in the lowest oxygen saturation is significant and improves the post-operative value to nearly 90%. When using random effects modelling, the LSAT mean difference was 5.64% [95%CI 2.14, 9.15], demonstrating a significant improvement. Given that patients with OSA have a drop of their oxygen saturations during an apnea or hypopnea, the fact that they decreased on average to only 89% instead of 82% demonstrates that the patients likely spent less time having the obstruction and/or it is possible that the airway was partially more open (after the CAPSO) secondary to the scar tissue from the CAPSO displacing the palate anteriorly.
Third, there was significant heterogeneity present when outcomes for AHI and lowest oxygen saturations were evaluated. For the AHI, the mean difference had high heterogeneity (Q statistic P = 0.001, and high inconsistency I2 = 78%, were eliminated when the study by Ugur et al was removed during the sensitivity analysis. For the standardized mean difference, the removal of Wassmuth et al22 and Pang et al7(2009) eliminated inconsistency which was low to begin with (I2 = 12%). The Ugur et al21 and Wassmuth et al22 state that they did not perform a tonsillectomy as part of the procedure, therefore, the patients did not have as much improvement in the AHI. There was significant heterogeneity in the lowest oxygen saturation mean difference with Q statistic P = 0.001 (heterogeneity present), I2 = 82% (high inconsistency) and the sensitivity analysis showed that Bayir et al17 and Pang et al18(2016) were the sources. For Bayir et al17 there was minimal change in the LSAT, from 86.1% to 87.8% and it is possible that the higher BMI was a reason given that the average was 29.2 kg/m2. In the Pang et al18(2016) study, the patients had a 5.2 point improvement in the LSAT (from 83.8% to 89.0%), which is less than the rest of the studies which had about 8 point improvement in the LSAT.
Lastly, a significant finding from this study is that when the outcomes are compared to the LAUP meta-analysis, there was an overall reduction of 41% in the AHI for patients undergoing CAPSO alone which is more of an improvement than the 32% reduction in AHI that was calculated in the LAUP meta-analysis.24 In the LAUP meta-analysis, the authors recommended that LAUP be performed with caution or not at all given that nearly 44% of the patients undergoing LAUP had a worsening of their AHI.24 In this meta-analysis, there were 6 of 115 (or 5% of patients who underwent CAPSO alone ended up having a worsening of their AHI), specifically: (1) Pang et al8 (2007) reported that none of the 13 patients had worsening of their AHI (without tonsillectomy), (2) Pang et al7(2009) reported that none of the 77 patients had a worsening of their AHI after CAPSO with tonsillectomy and (3) Wassmuth et al22(2000) reported that 6 of 25 (24%) patients had a worsening of their AHI after CAPSO alone. The AHI has improved by 41.0% for CAPSO alone, 61.7% for CAPSO with tonsillectomy and 52.1% for CAPSO with expansion pharyngoplasty; therefore, adding the tonsillectomy when appropriate can help improve the sleep apnea outcomes. When the ODI is evaluated (Bayir et al17), there was success in 20 patients from (11.76 ± 9.04) to (6.77 ± 5.36) events/h (a 42.4% reduction); but in 15 patients, the ODI worsened overall, from (12.17 ± 5.77) to (14.78 ± 9.92) events/h (a 21.4% increase). Therefore, it is possible that there are a select group of patients whose respiratory parameters during sleep worsen, but at this time it is difficult to determine which patients may improve and which ones may worsen given that the significant majority of studies have not provided the individual patient data.
As Wassmuth et al22 assert, the lack of substantial complications accompanying with CAPSO stands in stark contrast to the multiple morbidities associated with comparable procedures such as UPPP which include hemorrhage, severe pain, VPI, and nasopharyngeal stenosis. While postoperative pain appears to be the only noteworthy morbidity associated with CAPSO, it is a one-time occurrence as opposed to the repeated pain experienced in multi-step procedures offered in comparable interventions such as UPPP and LAUP. Furthermore, these more invasive procedures tend to be associated with a higher degree of pain for a longer duration of time. Ugur et al21 found an average VAS pain score of 7.5 for UPPP. For the uvulopalatal flap procedure, Marzetti et al20 reported a mean VAS pain score of 6.8 with an average duration of 10.8 days. Pang et al7(2009) found that the patients who underwent a concurrent tonsillectomy experienced a higher intensity of pain, suggesting that the pain was more likely attributable to tonsillectomy than anterior palatoplasty.
Limitations
There are limitations to this study. First, there are few publications reporting outcomes for CAPSO (primarily case reports and small case series). However, this shortcoming is understandable given that CAPSO is a targeted and patient-specific surgery requiring individual evaluation that presents challenges when attempting a randomized trial. Because fewer than 10 studies reported any given variable, we did not perform a risk of bias (Begg's and Egger's, funnel plot visual assessment); however, it is known that both medical and surgical literature can be biased against negative or equivalent findings, it is possible that studies demonstrating worsening of or no difference in OSA may have either been rejected from publication or were simply not submitted.
Conclusions
AHI has improved by 41% for CAPSO alone, 61.7% for CAPSO with tonsillectomy and 52.1% for CAPSO with expansion pharyngoplasty. Additionally, lowest oxygen saturation, sleepiness and snoring have also improved after CAPSO.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest between this research and any of the authors herein listed.
Disclaimer
The views expressed in this abstract/manuscript are those of the author(s) and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the US Government.
Acknowledgement
We would like to thank our Uniformed Services University of the Health Sciences librarian Rhonda J. Allard, MLIS, for assisting in the searching of manuscripts.
Edited by Jie Gao
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Azagra-Calero E., Espinar-Escalona E., Barrera-Mora J.M., Llamas-Carreras J.M., Solano-Reina E. Obstructive sleep apnea syndrome (OSAS). Review of the literature. Med Oral Patol Oral Cir Bucal. 2012;17:e925–e929. doi: 10.4317/medoral.17706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young T., Palta M., Dempsey J., Skatrud J., Weber S., Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 3.Shamsuzzaman A.S., Gersh B.J., Somers V.K. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA. 2003;290:1906–1914. doi: 10.1001/jama.290.14.1906. [DOI] [PubMed] [Google Scholar]
- 4.Yeboah J., Redline S., Johnson C. Association between sleep apnea, snoring, incident cardiovascular events and all-cause mortality in an adult population. MESA Atheroscler. 2011;219:963–968. doi: 10.1016/j.atherosclerosis.2011.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Young T., Finn L., Peppard P.E. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 6.Mair E.A., Day R.H. Cautery-assisted palatal stiffening operation. Otolaryngol Head Neck Surg. 2000;122:547–556. doi: 10.1067/mhn.2000.106475. [DOI] [PubMed] [Google Scholar]
- 7.Pang K.P., Tan R., Puraviappan P., Terris D.J. Anterior palatoplasty for the treatment of OSA: three-year results. Otolaryngol Head Neck Surg. 2009;141:253–256. doi: 10.1016/j.otohns.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 8.Pang K.P., Terris D.J. Modified cautery-assisted palatal stiffening operation: new method for treating snoring and mild obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;136:823–826. doi: 10.1016/j.otohns.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 9.Yaremchuk K. Palatal procedures for obstructive sleep apnea. Otolaryngol Clin North Am. 2016;49:1383–1397. doi: 10.1016/j.otc.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 10.Akcam T., Arslan H.H., Deniz S. Comparison of early postoperative pain among surgical techniques for obstructive sleep apnea. Eur Arch Otorhinolaryngol. 2012;269:2433–2440. doi: 10.1007/s00405-012-2078-4. [DOI] [PubMed] [Google Scholar]
- 11.Rashid M., Ahmed Z., Manzoor T. Modified palatal stiffening procedure for snoring. J Coll Physicians Surg Pak. 2011;21:330–333. [PubMed] [Google Scholar]
- 12.Cincik H., Cekin E., Cetin B., Gungor A., Poyrazoglu E. Comparison of uvulopalatopharyngoplasty, laser-assisted uvulopalatoplasty and cautery-assisted uvulopalatoplasty in the treatment of primary snoring. ORL J Otorhinolaryngol Relat Spec. 2006;68:149–155. doi: 10.1159/000091313. [DOI] [PubMed] [Google Scholar]
- 13.Clarke R.W., Yardley M.P., Davies C.M., Panarese A., Clegg R.T., Parker A.J. Palatoplasty for snoring: a randomized controlled trial of three surgical methods. Otolaryngol Head Neck Surg. 1998;119:288–292. doi: 10.1016/S0194-5998(98)70064-6. [DOI] [PubMed] [Google Scholar]
- 14.Cohen J. L. Erlbaum Associates; Hillsdale, N.J.: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 15.Lau J., Ioannidis J.P., Schmid C.H. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127:820–826. doi: 10.7326/0003-4819-127-9-199711010-00008. [DOI] [PubMed] [Google Scholar]
- 16.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bayır Ö., Acar M., Yüksel E. The effects of anterior palatoplasty on floppy eyelid syndrome patients with obstructive sleep apnea. Laryngoscope. 2016;126:2171–2175. doi: 10.1002/lary.25905. [DOI] [PubMed] [Google Scholar]
- 18.Pang K.P., Piccin O., Pang E.B., Pang K.A., Chan Y.H., Rotenberg B.W. Combined expansion pharyngoplasty and anterior palatoplasty for the treatment of OSA. Indian J Otolaryngol Head Neck Surg. 2016;68:528–533. doi: 10.1007/s12070-016-1020-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selcuk A., Ozer T., Esen E. Evaluation of effects of anterior palatoplasty operation on upper airway parameters in computed tomography in patients with pure snoring and obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2017;274:2183–2188. doi: 10.1007/s00405-016-4448-9. [DOI] [PubMed] [Google Scholar]
- 20.Marzetti A., Tedaldi M., Passali F.M. Preliminary findings from our experience in anterior palatoplasty for the treatment of obstructive sleep apnea. Clin Exp Otorhinolaryngol. 2013;6:18–22. doi: 10.3342/ceo.2013.6.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ugur K.S., Ark N., Kurtaran H., Kizilbulut G., Yuksel A., Gunduz M. Anterior palatoplasty for selected mild and moderate obstructive sleep apnea: preliminary results. Eur Arch Otorhinolaryngol. 2014;271:1777–1783. doi: 10.1007/s00405-013-2701-z. [DOI] [PubMed] [Google Scholar]
- 22.Wassmuth Z., Mair E., Loube D., Leonard D. Cautery-assisted palatal stiffening operation for the treatment of obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 2000;123:55–60. doi: 10.1067/mhn.2000.105184. [DOI] [PubMed] [Google Scholar]
- 23.Whiting P.F., Rutjes A.W., Westwood M.E. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 24.Camacho M., Nesbitt N.B., Lambert E. Laser-assisted uvulopalatoplasty for obstructive sleep apnea: a systematic review and meta-analysis. Sleep. 2017;40(3) doi: 10.1093/sleep/zsx004. [DOI] [PubMed] [Google Scholar]