Abstract
Objective
To provide an understanding of the incidence of anaplastic thyroid cancer within the United States.
Methods
Patients in the Surveillance, Epidemiology, and End Results (SEER) database were included from 1973 to 2014 based on a diagnosis of anaplastic thyroid cancer using ICD O-3 codes. Patients were categorized into cohorts based on their year of diagnosis.
Results
1527 patients were diagnosed with anaplastic thyroid cancer within the SEER 18 registries. The age-adjusted incidence rate was 0.2 per 1,000,000 people (95% CI: 0.0–0.5) in 1973 and was 1.2 per 1,000,000 people (95% CI: 0.8–1.6) in 2014 (average annual percent change: 3.0% [95% CI: 2.2%–3.7%]). Patients tended to be of older age (mean age: 70.5 [range 15.0–102.0]), of female sex (62.8%), and Caucasian (81.1%). Finally, survival over time remained the same, as median disease specific survival months was 4.00 (95% CI: 2.26–5.74) from 1995 to 1999 and 4.00 (95% CI: 3.26–4.74) from 2010 to 2014.
Conclusions
The incidence rate of anaplastic thyroid cancer has increased from 1973 to 2014. Interestingly, median survival in months did not greatly change overtime. Based on this increasing incidence, physicians must act appropriately to identify patients with anaplastic thyroid cancer as it possesses a high morbidity and mortality.
Level of evidence
4.
Keywords: Anaplastic thyroid cancer, Thyroid cancer, Head and neck, Head and neck endocrine surgery, Head and neck oncology
Introduction
Thyroid cancer has steadily increased in incidence over the past several decades. In 2000, the overall incidence of thyroid cancer was roughly 8.0 per 100,000 individuals.1 In 2015, the overall incidence of thyroid cancer was 15.04 per 100,000 individuals according to the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) database.2 Although overall thyroid cancer incidence is increasing, this increase is mostly due to a greater frequency of papillary thyroid cancer. Currently, it is unclear whether the incidence of anaplastic thyroid cancer is increasing or decreasing. Studies in the past have examined the incidence of different thyroid cancers over time. For example, Dijkstra et al3 noted that anaplastic thyroid cancer had not increased in incidence over time when examining patient data from an Irish population. Additionally, Pathak et al4 noted in a database study of patients in the Manitoba Cancer Registry that the incidence of anaplastic thyroid cancer was low in each decade and declined by over 40% from the 1991–2000 decade to the 2001–2010 decade. However, these studies are small institution/regional studies outside of the United States. Little data remains on the trends in incidence of anaplastic thyroid cancer within the United States. Further evaluation of the incidence of anaplastic thyroid cancer cases within the United States will provide physicians with an up to date review of the incidence rate of this disease.
Materials and methods
Data was obtained using the National Cancer Institute's SEER database. Patients from the SEER database were included from 1973 to 2014. The SEER 18 Registry Research Data (released April 2017, based on the November 2016 submission) was utilized. Age-adjusted incidence rates were calculated using the “Incidence-SEER 9 Registry Research Data” (released April 2017, based on the November 2016 submission) from 1973 to 2014. This study was exempted from review by the Office of Research Integrity of the Medical University of South Carolina. Patients were included based on a diagnosis of anaplastic thyroid cancer using the ICD O-3 codes of C73.9: thyroid primary site and 8021/3: Carcinoma, anaplastic, NOS. Patients were grouped into cohorts according to their year of diagnosis.
All data analyses were performed with SPSS 24.0 (IBM Corporation, Armonk, NY), SigmaPlot 12.5 (Systat Software, San Jose, CA), and MedCalc software 16.8 (MedCalc Software bvba, Ostend, Belgium). All continuous variables were tested for normal distribution as determined by the Kolmogorov–Smirnov test.
Categorical variables were summarized by frequency, percentage, and/or range. Continuous variables were summarized by mean (SD) or median (interquartile range) where appropriate. Comparisons of categorical variables were performed using a Chi-Square test. For continuous variables, comparisons among groups were made with a One-Way ANOVA or Kruskal–Wallis test where appropriate. Survival was calculated using the Kaplan–Meier estimate expressed as 5-year disease-specific survival (DSS) rates and median DSS months (95% confidence intervals). Survival rates were compared using the Log-Rank test. The average annual percentage change (AAPC) in incidence for anaplastic thyroid cancer cases in this study from 1973 to 2014 was calculated using the Joinpoint Trend Analysis Software (version 4.5).5 A P value of <0.05 was considered to indicate a statistically significant difference for all statistical tests.
Results
From 1973 to 2014, 1527 patients were diagnosed with anaplastic thyroid cancer within the SEER 18 registries. Of the 1527 patients, 959 were female and 568 were male. Caucasian race was noted in 1238 cases (81.1%). Additionally, there were 162 cases involving patients of Asian or Pacific Islander race. Furthermore, African American race was noted in 114 cases. Finally, a large majority of the patients were diagnosed with anaplastic thyroid cancer at or above the age of 50 with a mean age of 70.5 (Range 15.0–102.0).
Incidence
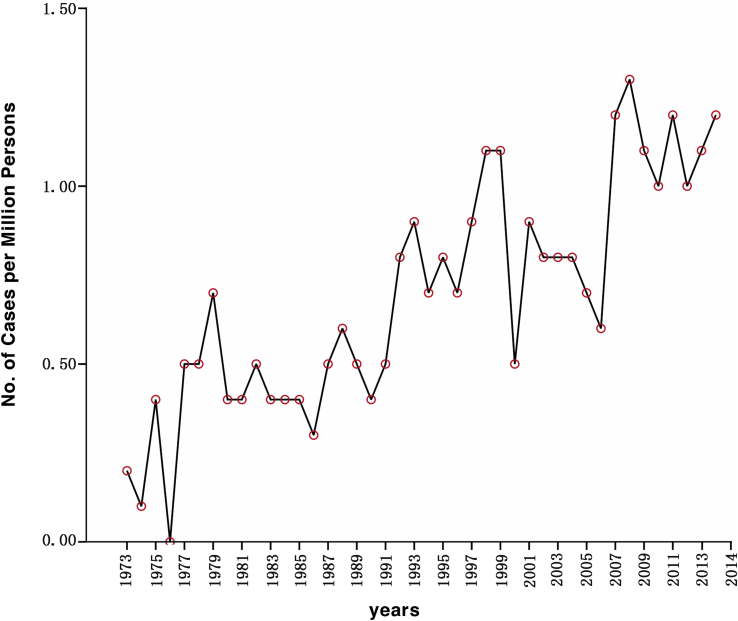
The number of cases in each year of diagnosis category was charted over time as shown in Table 1. Fig. 1 shows the age-adjusted incidence rate per 1,000,000 people (based on 2000 US Standard Population data) of anaplastic thyroid cancer in the United States. The age-adjusted incidence rate of anaplastic thyroid cancer in 1973 was 0.2 per 1,000,000 (95% CI: 0.0–0.5) people. In comparison, the age-adjusted incidence rate in 2014 was 1.2 per 1,000,000 people (95% CI: 0.8–1.6) (Fig. 1). The average annual percentage change for anaplastic thyroid cancer cases from 1973 to 2014 in this study was 3.0% (95% CI: 2.2%–3.7%).
Table 1.
Patient demographics of anaplastic thyroid cancer patients.
| Characteristic | Total | 1973–1974 | 1975–1979 | 1980–1984 | 1985–1989 | 1990–1994 | 1995–1999 | 2000–2004 | 2005–2009 | 2010–2014 | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases (%) | 1527 (100) | 4 (0.3) | 37 (2.4) | 41 (2.7) | 46 (3.0) | 93 (6.1) | 154 (10.1) | 290 (19.0) | 391 (25.6) | 471 (30.8) | |
| Mean Age (Range) | 70.5 (15.0–102.0) | 66.0 (58.0–74.0) | 68.0 (15.0–94.0) | 71.3 (44.0–98.0) | 75.1 (50.0–96.0) | 72.0 (34.0–95.0) | 71.4 (30.0–95.0) | 69.2 (30.0–97.0) | 70.3 (26.0–98.0) | 70.7 (26.0–102.0) | 0.16 |
| Sex No. (%) | 0.27 | ||||||||||
| Female | 959 (62.8) | 2 (50.0) | 31 (83.8) | 25 (61.0) | 32 (69.6) | 58 (62.4) | 100 (64.9) | 173 (59.7) | 247 (63.2) | 291 (61.8) | |
| Male | 568 (37.2) | 2 (50.0) | 6 (16.2) | 16 (39.0) | 14 (30.4) | 35 (37.6) | 54 (35.1) | 117 (40.3) | 144 (36.8) | 180 (38.2) | |
| Race No. (%) | 0.73 | ||||||||||
| Unknown | 4 (0.3) | 0 | 0 | 0 | 0 | 1 (1.1) | 0 | 0 | 2 (0.5) | 1 (0.2) | |
| AI/AN | 9 (0.6) | 0 | 0 | 0 | 0 | 1 (1.1) | 1 (0.6) | 2 (0.7) | 2 (0.5) | 3 (0.6) | |
| Asian | 162 (10.6) | 1 (25.0) | 3 (8.1) | 3 (7.3) | 0 | 10 (10.8) | 20 (13.0) | 22 (7.6) | 45 (11.5) | 58 (12.3) | |
| Caucasian | 114 (7.5) | 0 | 1 (2.7) | 0 | 2 (4.3) | 6 (6.5) | 12 (7.8) | 27 (9.3) | 28 (7.2) | 38 (8.1) | |
| African American | 1238 (81.1) | 3 (75.0) | 33 (89.2) | 38 (92.7) | 44 (95.7) | 75 (80.6) | 121 (78.6) | 239 (82.4) | 314 (80.3) | 371 (78.8) |
AI/AN: American Indian/Alaskan Natives, Asian: Asian and Pacific Islanders, P < 0.05 = significant.
Fig. 1.
Age-adjusted incidence rate per million persons (2000 US standard population) of anaplastic thyroid cases based on year of diagnosis.
Type of surgical procedure
Table 2 describes the type of surgical procedures performed for patients diagnosed with anaplastic thyroid cancer in this study. 725 (47.5%) patients did not have any surgery noted during their cancer course, 94 (6.2%) underwent subtotal (ST) or near total (NT) thyroidectomy, and 300 (19.6%) patients underwent total thyroidectomy (TT). The percent of ST/NT thyroidectomies remained stable from 1995 to 1999 to 2010–2014: 5.8% and 6.6% respectively. The percent of TT remained stable from 1995 to 1999 to 2010–2014: 22.7% and 22.3% respectively. The percent of patients receiving no surgical management increased from 1995 to 1999, where it was 37.6% to 2000–2004, where it was 55.5% (P < 0.001) (Table 2).
Table 2.
Surgical management of anaplastic thyroid cancer patients [No. (%)].
| Surgery Type | Total | 1973–1974 | 1975–1979 | 1980–1984 | 1985–1989 | 1990–1994 | 1995–1999 | 2000–2004 | 2005–2009 | 2010–2014 | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| None | 725 (47.5) | 0 | 1 (2.7) | 2 (4.9) | 9 (19.6) | 35 (37.6) | 58 (37.6) | 161 (55.5) | 202 (51.7) | 257 (54.6) | <0.001 |
| Lobectomy and/or isthmectomy | 141 (9.2) | 0 | 0 | 0 | 3 (6.5) | 6 (6.5) | 20 (13.0) | 28 (9.7) | 42 (10.7) | 42 (8.9) | |
| ST/NT | 94 (6.2) | 0 | 0 | 0 | 3 (6.5) | 9 (9.7) | 9 (5.8) | 19 (6.6) | 23 (5.9) | 31 (6.6) | |
| TT | 300 (19.6) | 0 | 0 | 0 | 2 (4.3) | 17 (18.3) | 35 (22.7) | 52 (17.9) | 89 (22.8) | 105 (22.3) | |
| Thyroidectomy NOS | 14 (0.9) | 0 | 0 | 0 | 1 (2.2) | 1 (1.1) | 4 (2.6) | 3 (1.0) | 1 (0.3) | 4 (0.8) | |
| Othera | 253 (16.6) | 4 (100.0) | 36 (97.3) | 39 (95.1) | 28 (60.9) | 25 (27.0) | 28 (18.1) | 27 (9.3) | 34 (8.6) | 32 (6.7) |
ST/NT: Subtotal/Near Total Thyroidectomy, TT: Total Thyroidectomy, NOS: Not Otherwise Specified, P < 0.05 = significant.
Other includes: Surgery NOS, Unknown Surgery Status, and Incisional/Aspiration Biopsy or Local Excision.
Survival
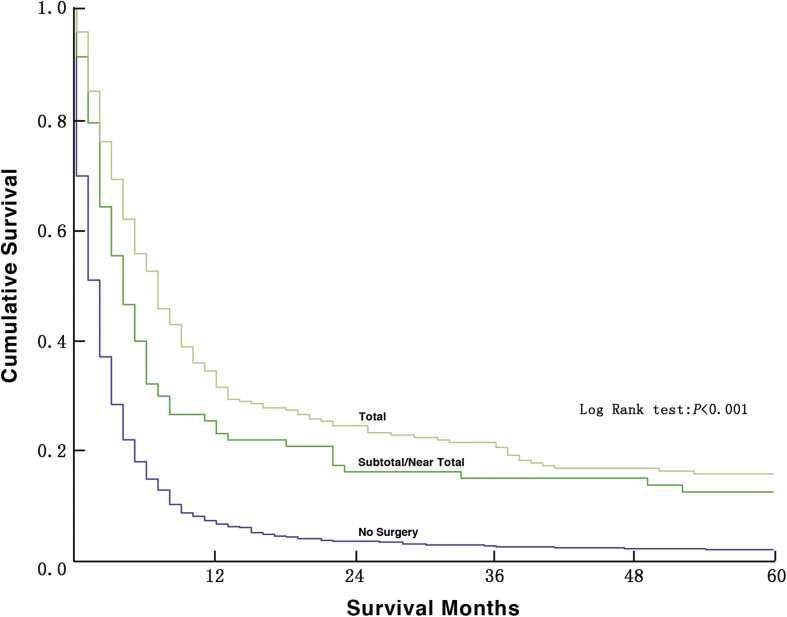
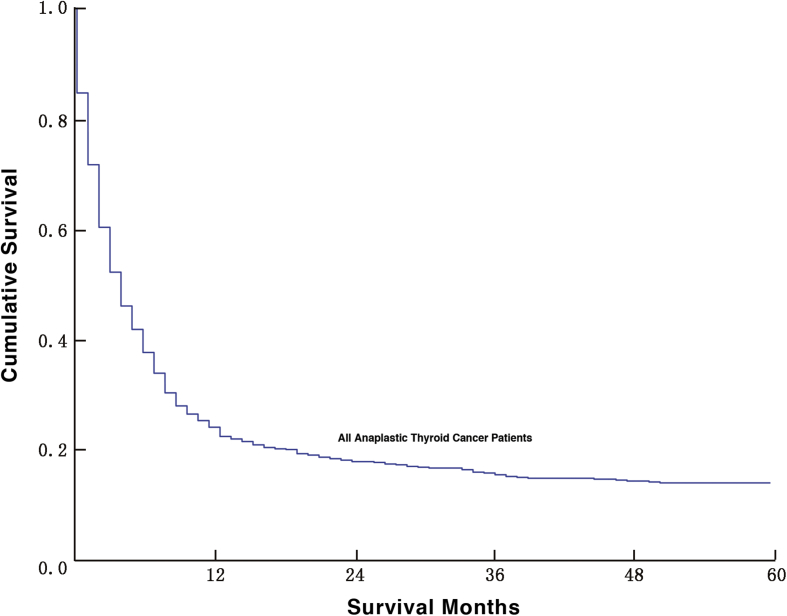
As shown in Table 3, the median months of DSS for patients diagnosed from 1995 to 1999 was 4.00 (95% CI: 2.26–5.74). The median months of DSS was 4.00 (95% CI: 3.26–4.74) for patients diagnosed between 2010 and 2014 (Table 3). For patients who received no surgical management, the median months of DSS was 2.00 (95% CI: 1.65–2.35) compared to 6.00 (95% CI: 3.91–8.09) for ST/NT patients and 10.00 (95% CI: 7.70–12.30) for TT patients (P < 0.001). Fig. 2 compares the survival rates of patients who received no surgery, ST/NT, or TT. Finally, Fig. 3 demonstrates the DSS rate of all patients in this study diagnosed with anaplastic thyroid cancer regardless of the year of diagnosis.
Table 3.
Survival of anaplastic thyroid cancer patients.
| Characteristic | Total | 1973–1974 | 1975–1979 | 1980–1984 | 1985–1989 | 1990–1994 | 1995–1999 | 2000–2004 | 2005–2009 | 2010–2014 |
|---|---|---|---|---|---|---|---|---|---|---|
| Disease-Specific Deaths No. (%)a | 1052 (100) | 2 (50.00) | 31 (83.78) | 33 (80.49) | 38 (82.61) | 76 (81.72) | 110 (71.43) | 213 (73.45) | 255 (65.22) | 294 (62.42) |
| Median DSS Months (95% CI) | 4.00 (3.57–4.44) | 13.00 (0.0–29.97) | 3.00 (2.34–3.66) | 5.00 (4.02–5.98) | 2.00 (1.11–2.89) | 2.00 (0.96–3.04) | 4.00 (2.26–5.74) | 3.00 (2.16–3.84) | 5.00 (3.73–6.28) | 4.00 (3.26–4.74) |
DSS: Disease-Specific Survival, 95% CI: Confidence Interval.
Death percentage based on total number of cases in each cohort.
Fig. 2.
5-year disease-specific survival of patients who received no surgery, a subtotal/near total thyroidectomy, or a total thyroidectomy.
Fig. 3.
5-year disease-specific survival of all anaplastic thyroid cancer patients.
Discussion
Anaplastic thyroid cancer continues to increase in incidence based on the results of this study. This result aligns with the documented increase in total number of thyroid cancer cases within the United States.6 The continued increase in the number of cases found in this study could be explained by the fact that the SEER database is continuously expanding,7 and the population in the United States in increasing. Furthermore, the increase in the number of anaplastic thyroid cancer cases could be due to improved diagnostic guidelines for healthcare providers. In 2012, the American Thyroid Association released comprehensive guidelines for patients diagnosed with anaplastic thyroid cancer.8 Corresponding with the increased number of anaplastic thyroid cases seen over time, the age-adjusted incidence rate per 1,000,000 people (based on 2000 US Standard Population data) of anaplastic thyroid cancer in the United States demonstrated an increasing trend from 1973 to 2014 (average annual percentage change: 3.0% [95% CI: 2.2%–3.7%]) (Fig. 1). While the age-adjusted incidence rates may be increasing, the rate of anaplastic thyroid cancer still remains very low within the United States.
Female individuals continue to experience higher rates of anaplastic thyroid cancer compared to male patients. In each decade examined, the number of female cases was higher than the number of male cases within this study. Davies and Welch9 noted in 2014 a similar higher incidence rate amongst female patients as they noted a 4-times-greater absolute increase in total thyroid cancer cases amongst women as compared to men. However, interestingly, 37.2% of the cases noted in this study were identified in male patients. This number demonstrates that anaplastic thyroid cancer may not be as selective toward the female sex as compared to other thyroid cancer types. No significant changes in racial demographics were appreciated in this study. Patients of Caucasian race continue to experience the highest percentage of anaplastic thyroid cases with roughly 80% of the total cases noted in the SEER registry. Similarly, a meta-analysis by Ma et al10 noted an increased risk of thyroid cancer in Caucasian individuals. Furthermore, in this study, anaplastic thyroid cancer appears to be most commonly diagnosed in the older population based on the mean age at diagnosis. This result aligns with a prospective cohort study by Kwong et al11 which noted older patients had a higher risk of anaplastic thyroid cancer as compared to younger individuals.
Regarding surgical management, 25.8% of patients in this study underwent a ST, NT, or TT. The percentages of both ST/NT thyroidectomies and TT remained stable over time. Per the 2015 National Comprehensive Cancer Network (NCCN) guidelines, patients with resectable disease should undergo a total thyroidectomy.12 Additionally, the percentage of patients who did not receive any surgical care increased from the 1995–1999 cohort (37.6%) to the 2000–2004 cohort (55.5%). Thereafter, in each subsequent cohort, greater than 50% of anaplastic thyroid cancer patients did not receive any surgical management. Our findings concur with current literature as most anaplastic thyroid cancers present as unresectable or metastatic cancers and thus surgical intervention may not be warranted.12, 13
Anaplastic thyroid cancer has been known to be an aggressive type of thyroid cancer with a low survival rate.14 A retrospective study by Nachalon et al13 noted a median survival of 6 months (95% CI: 2.1–9.8) of 26 patients with anaplastic thyroid cancer from 2008 to 2013. In this study, the median months of DSS was 4.00 (95% CI: 3.26–4.74) for patients diagnosed from 2010 to 2014. Of note, median months of DSS and DSS rates for patients who underwent a TT were greater than those who underwent a ST/NT thyroidectomy or those who did not receive any surgical management. The increase in survival for TT patients is likely due to the presence of resectable disease.12 Conversely, patients who did not receive any surgical management likely presented with more advanced disease.13 These results along with the DSS curve of all patients in this study shown in Fig. 3 demonstrate the consistent low number of survival months for patients diagnosed with anaplastic thyroid cancer regardless of surgical management.
Although several results have been discussed, there are limitations that are to be noted within this study. First, the increasing anaplastic thyroid cancer incidence rate noted in this study could be attributed to advancements in diagnostic modalities. However, information regarding the use of diagnostic modalities is not available within the SEER database and thus this variable could not be examined. Additionally, although multimodality treatment regimens are often used for patients with anaplastic thyroid cancer,12 information regarding radiation and chemotherapy is categorized in the SEER database as “yes” and “none/unknown”.15 Given this categorization, radiation and chemotherapy data were not evaluated as potential changes in treatment regimens were likely to be affected by patients with an unknown status. Finally, to review age-adjusted incidence rates spanning from 1973 to 2014, the “Incidence-SEER 9 Registry Research Data” was used. Despite these limitations, the SEER database was selected for use in this study as it is a national database that provides a large volume of data even on rare cancers such as anaplastic thyroid cancer. In relation to this study, a single or multi-institutional study may not provide a reasonable number of anaplastic thyroid cancer cases for data analysis. To our knowledge, McIver et al16 2001 50-year cohort of 134 patients and Mohebati et al17 2014 study of 83 patients were two of the largest institutional studies related to anaplastic thyroid cancer in the United States. This study provides data on 1527 cases of anaplastic thyroid cancer and will provide a large-population analysis of cases within the United States. The SEER database also provides the ability to examine patient demographics, cancer staging, and treatment trends. Data obtained from databases such as the SEER registry minimizes regional factors that may alter overall cancer prevalence or characteristics at a national level.
Conclusion
Our study shows that the incidence rate of anaplastic thyroid cancer is increasing in the United States. However, the overall incidence of anaplastic thyroid cancer still remains low. Most patients continue to not undergo surgical management. While the increase in thyroid cancer is well documented, the specific cause for the increase in thyroid cancer remains to be determined. Studies have hypothesized the increased incidence of thyroid cancer can be attributed to increased access to healthcare and screening modalities.18, 19 This hypothesis most likely relates to patients diagnosed with papillary thyroid cancer, as patients with anaplastic thyroid cancer present late in their disease course and thus a true rise in the incidence of this cancer may be occurring. Further studies must be performed to evaluate the specific risk and causative factors for anaplastic thyroid cancer. Regardless of the cause, anaplastic thyroid cancer continues to increase in incidence. Physicians must act appropriately to identify patients with this disease as it possesses a high morbidity and mortality.
Conflict of interest
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Edited by Jing Li
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Davies L., Morris L.G., Haymart M. American Association of Clinical Endocrinologists and American College of Endocrinology disease state clinical review: the increasing incidence of thyroid cancer. Endocr Pract. 2015;21:686–696. doi: 10.4158/EP14466.DSCR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howlader N.N.A., Krapcho M., Miller D. 2017. SEER Cancer Statistics Review, 1975-2014.https://seer.cancer.gov/csr/1975_2014/ [Google Scholar]
- 3.Dijkstra B., Prichard R.S., Lee A. Changing patterns of thyroid carcinoma. Ir J Med Sci. 2007;176:87–90. doi: 10.1007/s11845-007-0041-y. http://www.ncbi.nlm.nih.gov/pubmed/17486294 [DOI] [PubMed] [Google Scholar]
- 4.Pathak K.A., Leslie W.D., Klonisch T.C., Nason R.W. The changing face of thyroid cancer in a population-based cohort. Cancer Med. 2013;2:537–544. doi: 10.1002/cam4.103. http://www.ncbi.nlm.nih.gov/pubmed/24156026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joinpoint Trend Analysis Software. 2017. https://surveillance.cancer.gov/joinpoint/ [Google Scholar]
- 6.Magreni A., Bann D.V., Schubart J.R., Goldenberg D. The effects of race and ethnicity on thyroid cancer incidence. JAMA Otolaryngol Head Neck Surg. 2015;141:319–323. doi: 10.1001/jamaoto.2014.3740. http://www.ncbi.nlm.nih.gov/pubmed/25654447 [DOI] [PubMed] [Google Scholar]
- 7.Scosyrev E., Messing J., Noyes K., Veazie P., Messing E. Surveillance Epidemiology and End Results (SEER) program and population-based research in urologic oncology: an overview. Urol Oncol. 2012;30:126–132. doi: 10.1016/j.urolonc.2009.11.005. http://www.ncbi.nlm.nih.gov/pubmed/20363162 [DOI] [PubMed] [Google Scholar]
- 8.Smallridge R.C., Ain K.B., Asa S.L. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2012;22:1104–1139. doi: 10.1089/thy.2012.0302. http://www.ncbi.nlm.nih.gov/pubmed/23130564 [DOI] [PubMed] [Google Scholar]
- 9.Davies L., Welch H.G. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014;140:317–322. doi: 10.1001/jamaoto.2014.1. http://www.ncbi.nlm.nih.gov/pubmed/24557566 [DOI] [PubMed] [Google Scholar]
- 10.Ma J., Huang M., Wang L., Ye W., Tong Y., Wang H. Obesity and risk of thyroid cancer: evidence from a meta-analysis of 21 observational studies. Med Sci Monit. 2015;21:283–291. doi: 10.12659/MSM.892035. http://www.ncbi.nlm.nih.gov/pubmed/25612155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwong N., Medici M., Angell T.E. The influence of patient age on thyroid nodule formation, multinodularity, and thyroid cancer risk. J Clin Endocrinol Metab. 2015;100:4434–4440. doi: 10.1210/jc.2015-3100. http://www.ncbi.nlm.nih.gov/pubmed/26465395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haddad R.I., Lydiatt W.M., Ball D.W. Anaplastic thyroid carcinoma, Version 2.2015. J Natl Compr Cancer Netw. 2015;13:1140–1150. doi: 10.6004/jnccn.2015.0139. http://www.ncbi.nlm.nih.gov/pubmed/26358798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nachalon Y., Stern-Shavit S., Bachar G., Shvero J., Limon D., Popovtzer A. Aggressive palliation and survival in anaplastic thyroid carcinoma. JAMA Otolaryngol Head Neck Surg. 2015;141:1128–1132. doi: 10.1001/jamaoto.2015.2332. http://www.ncbi.nlm.nih.gov/pubmed/26512447 [DOI] [PubMed] [Google Scholar]
- 14.Ranganath R., Shah M.A., Shah A.R. Anaplastic thyroid cancer. Curr Opin Endocrinol Diabetes Obes. 2015;22(5):387–391. doi: 10.1097/MED.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 15.Dictionary of SEER Stat Variables November 2016 Submission. 2017. https://seer.cancer.gov/data/seerstat/nov2016/seerstat-variable-dictionary-nov2016.pdf (released April 2017) [Google Scholar]
- 16.McIver B., Hay I.D., Giuffrida D.F. Anaplastic thyroid carcinoma: a 50-year experience at a single institution. Surgery. 2001;130:1028–1034. doi: 10.1067/msy.2001.118266. http://www.ncbi.nlm.nih.gov/pubmed/11742333 [DOI] [PubMed] [Google Scholar]
- 17.Mohebati A., Dilorenzo M., Palmer F. Anaplastic thyroid carcinoma: a 25-year single-institution experience. Ann Surg Oncol. 2014;21:1665–1670. doi: 10.1245/s10434-014-3545-5. http://www.ncbi.nlm.nih.gov/pubmed/24554064 [DOI] [PubMed] [Google Scholar]
- 18.Udelsman R., Zhang Y. The epidemic of thyroid cancer in the United States: the role of endocrinologists and ultrasounds. Thyroid. 2014;24:472–479. doi: 10.1089/thy.2013.0257. http://www.ncbi.nlm.nih.gov/pubmed/23937391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morris L.G., Sikora A.G., Tosteson T.D., Davies L. The increasing incidence of thyroid cancer: the influence of access to care. Thyroid. 2013;23:885–891. doi: 10.1089/thy.2013.0045. http://www.ncbi.nlm.nih.gov/pubmed/23517343 [DOI] [PMC free article] [PubMed] [Google Scholar]