Abstract
Background
Although there is extensive evidence for the efficacy of online eating disorder (ED) prevention programs in clinical trials, these programs have rarely been adopted beyond the trial phase and offered to a wider audience. As risk factors for eating disorders are partly associated with overweight and overweight in turn is correlated to disordered eating, this study will offer a combined eating disorder prevention program which also promotes a balanced lifestyle to normal weight and overweight individuals alike. The efficacy of the program has been proven in previous trials. The study aims to evaluate the dissemination of a combined eating disorder prevention and health promotion program (everyBody) to women of all age groups and varying levels of ED risk status in the general population.
Methods
A dissemination trial will be conducted in German-speaking countries, including 4160 women from the general population. Participants will be screened to exclude participants who are likely to have an ED. Eligible participants will be allocated to one of five program arms based on their BMI and respective ED symptoms. The guided program consists of 4 to 12 weeks of weekly sessions offering CBT-based exercises, psychoeducational material, self-monitoring, and group discussions. Outcomes will be assessed according to the RE-AIM model, including measures of effectiveness, reach, adoption, implementation, and maintenance of the program.
Discussion/conclusions
This trial aims to disseminate a combined ED prevention and health promotion program in the general population, offering universal, selective and indicated prevention in one program. To our knowledge, it is the first trial to systematically evaluate dissemination efforts based on the RE-AIM model. This trial will be conducted as part of the EU-funded ICare (Integrating Technology into Mental Health Care Delivery in Europe) project.
Keywords: Eating disorders, Prevention, Internet-based intervention, Disseminationi
Highlights
-
•
The trial offers tailored health promotion, universal, selective, and indicated eating disorder prevention in one program.
-
•
The study aims to disseminate a combined eating disorder prevention and health promotion program in the general population.
-
•
Dissemination efforts will be systematically evaluated based on the RE-AIM model.
1. Introduction
A growing number of people struggle with body image issues and/or poor eating and exercise habits. While symptoms of disordered eating and body dissatisfaction primarily affect young women, health problems related to poor eating and exercise habits impair women and men of all ages (Aschenbrenner et al., 2004; Delinsky and Wilson, 2008; Hay et al., 2008; Leon et al., 1997; Shisslak et al., 1995).
Interventions to improve body image and eating and exercise habits and to prevent the onset of eating disorders should aim at reducing modifiable risk factors and, if possible, enhancing/augmenting protective factors. Dieting and body dissatisfaction have been found to be the most potent shared risk factors for full syndrome eating disorders, disordered eating, extreme weight control behaviors and overweight (Goldschmidt et al., 2016; Jacobi et al., 2004; Jacobi et al., in press; Neumark-Sztainer et al., 2007). In turn, overweight and obesity are associated with eating disturbances (Hilbert et al., 2012) and an increased prevalence of bulimia nervosa (BN) and binge eating disorder (BED) (Kessler et al., 2013a). Although the age of onset for eating disorders in women peaks at adolescence and young adulthood (Hudson et al., 2007), negative body image and disordered eating are prevalent in older women as well (Hilbert et al., 2012; Slevec and Tiggemann, 2011). In addition to facilitating disordered eating and eating disorders, dieting has been found to have negative impacts on mental and physical health (e.g. Bacon and Aphramor, 2011; Gallant et al., 2013; McFarlane et al., 1999; Tomiyama et al., 2010) and has proven to be ineffective for long term weight loss and even leading to weight gain (Neumark-Sztainer et al., 2012; Pietilainen et al., 2012; Stice et al., 1999).
A considerable number of interventions for eating disorder prevention have been proven to reduce risk factors and enhance protective factors (Le et al., 2017; Watson et al., 2016). Compared with face-to-face interventions, the potential advantages of internet-based intervention include low cost (Andersson et al., 2014), a wide availability, easier standardization and maintenance over time, flexible tailoring of interventions based on the needs of recipients, and anonymity of recipients (Bauer and Moessner, 2013). A number of reviews and meta-analyses on Internet-based programs have shown that these programs decrease eating disorder related symptoms and risk factors. In a meta-analysis focusing on universal, selective and indicated prevention separately, Watson et al. (2016) noted modest effects for universal prevention but more promising results for selective and indicated prevention. In accordance with these findings, Le et al. (2017) also found small to moderate effect sizes for universal and selective prevention. Opposed to Watson et al.'s conclusion, Le et al. (2017) initially did not find evidence for the effectiveness of indicated prevention. After a reclassification of studies, which increased the number of studies classified as indicated prevention trials, Le et al. (2017) reported significant effects of indicated prevention programs on e.g., eating disorder pathology, dieting, and shape and weight concerns. Finally, Melioli et al. (2016) reported small to moderate effect sizes of Internet-based selective prevention programs for a number of established risk factors and eating disorder symptoms such as the internalization of the thin ideal, shape and weight concerns, body dissatisfaction, bingeing and purging behaviors, and dietary restriction.
A number of trials included in these meta-analyses focused on StudentBodies, an Internet-based eating disorder prevention program based on the principles of cognitive-behavioral therapy (CBT). It has been proven to be efficient in a large number of clinical trials spanning from universal to indicated prevention (e.g. Jacobi et al., 2007; Jacobi et al., 2012; Taylor et al., 2006; Taylor et al., 2016). Loucas et al. (2014) report reductions in eating disorder psychopathology, weight concerns and drive for thinness. In a meta-analysis, Beintner et al. (2012) found small to moderate effect sizes for drive for thinness, weight and shape concerns, eating concerns, and restrained eating. While Watson et al. (2016) found larger effects for selective interventions compared to universal interventions, Beintner et al. (2012) concluded that both universal and selective interventions can be equally effective. Summarizing the findings on online eating disorder prevention programs in general and on StudentBodies in particular, there is sufficient evidence for the effectiveness of these programs. Definitions and selection criteria for classifying studies as universal, selective and indicated prevention differ widely across trials and reviews (Beintner et al., 2012). For example, Le et al. (2017) considered female gender as an indicator of risk and therefore a selection criterion for selective prevention, whereas Beintner et al. (2012) included female samples in the universal prevention category. As Beintner et al. (2012) noted, the varying criteria between reviews and proportions of at-risk participants may account for the differences in the findings.
Most previous prevention trials primarily included school and college students or comparatively young samples in general (e.g. Le et al., 2017; Melioli et al., 2016; Stice et al., 2007). Hence, research is still needed on prevention in other populations and age groups, e.g., middle aged and older women, as well as for interventions targeting shared risk factors for eating disorders and overweight as part of the same intervention (Le et al., 2017). An advantage of this approach is the avoidance of possible stigmatization of participation in an eating disorder prevention program or a program specifically directed at people with overweight and obesity. Furthermore, despite the existing evidence for the effectiveness of prevention programs for eating disorders, these programs are generally not translated into practice, and access to these programs is often only possible as part of research studies with limited funding (Bauer and Moessner, 2013). Common barriers include limited human resources and inadequate infrastructure (Bauer and Moessner, 2013). Consequently, the processes of implementing prevention programs into practice have hardly been examined in detail.
Online prevention programs have–compared with other preventive approaches–the potential for widespread dissemination at low cost, along with additional advantages described above. However, an online platform through which both screening and tailored interventions are provided for individuals at various levels of risk and/or reporting isolated eating disorder symptoms has not yet been deployed in a community setting. Research has shown that tailoring intervention content can enhance change in behavioral outcomes of the interventions by increasing user satisfaction and adherence (Krebs et al., 2010; Ryan and Lauver, 2002).
The current study aims to provide and evaluate the effectiveness, reach, adoption, implementation, and maintenance of a comprehensive Internet-based prevention program for eating disorders and related behaviors according to the RE-AIM model (Kessler et al., 2013b) The program is designed for adult women of all age groups and offers universal, selective and indicated prevention based on risk status of participants. This trial is conducted as part of the EU-funded ICare (Integrating Technology into Mental Health Care Delivery in Europe) project.
2. Materials and methods
2.1. Objectives and hypotheses
The aim of this study is to evaluate the reach, effectiveness, adoption, implementation and maintenance of a combined online screening and tailored, evidence-based prevention program to promote healthy eating and exercise behaviors, reduce body dissatisfaction, dietary restraint and low-level ED symptoms, and support healthy weight maintenance/management. All programs have an established evidence base from randomized controlled trials (RCTs; e.g. Beintner et al., 2012; Jacobi et al., 2007; Jacobi et al., 2012; Jones et al., 2014).
2.2. Participants
We will include women over 18 who are interested in participating in an online program to improve their body image, exercise and eating behaviors, and have access to the internet and give their informed consent (online). We will exclude men as well as women who report currently being in psychological treatment for eating disorders or having been in treatment at any time during the previous 6 month. Additionally, current eating disorder symptoms will be assessed using an online eating disorder screening. We will exclude women who are likely to have anorexia nervosa (AN), bulimia nervosa (BN), or binge eating disorder (BED) based on the screening results. Participants with full-syndrome eating disorders will be referred to treatment.
Recruitment will take place in Germany, Austria and Switzerland via newspaper and magazine articles, promotion and offering of programs through several health insurances as well as targeted steps for subpopulations likely to experience body dissatisfaction (younger people, gym members, people seeking information on weight loss on the internet). Participants will also be recruited via shared communication strategies employed for the whole consortium, including the ICare website and Facebook account.
2.3. Study design
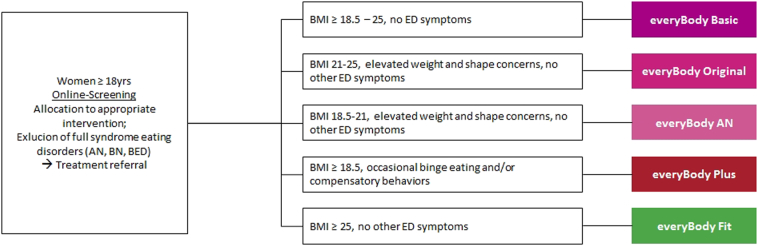
The study design is a nonrandomized, parallel-group interventional design. Following an online screening, participants will be allocated to the appropriate intervention (see Fig. 1). Women will be allocated to programs based on their BMI, the presence of subthreshold (<1/week) binge eating/purging, and the presence of elevated weight and shape concerns defined as a score larger than 42 on the weight and shape concerns scale (Grund, 2003). Table 1 provides an overview of the suite of interventions.
Fig. 1.
Allocation to study arm based on BMI and ED symptoms.
Table 1.
Summary of program characteristics.
| Program | Duration | Guidance level | Aims |
|---|---|---|---|
| everyBody Basic | 4 weeks | No guidance | Promoting healthy eating and exercise habits |
| everyBody Original | 8 weeks | Moderated group chat | Improving body image, promoting healthy eating and exercise habits, improving self-esteem |
| everyBody Plus | 8 weeks | Moderated group chat and weekly personal feedback | Improving body image, establishing healthy eating and exercise habits, improving self-esteem, reducing occasional binge eating and/or purging |
| everyBody AN | 10 weeks | Moderated group chat and weekly personal feedback | Improving body image, establishing healthy eating and exercise habits, improving self-esteem, reducing dietary restraint |
| everyBody Fit | 12 weeks | Moderated group chat | Healthy weight regulation, promoting healthy eating and exercise habits, improving self-esteem |
Each participant will be assessed prior to the intervention (screening, T0; baseline, T1), at mid- intervention (Tmid), at post-intervention (T2), at 6-month follow-up (T3) and at 12-month follow-up (T4). All assessments will be administered online. Participants will have to provide an e-mail address as contact information and give online informed consent to the usage of their data and being contacted for follow-up assessments.
This trial is registered at http://www.isrctn.org, number ISRCTN13716228. It has been approved by the ethics committee of TU Dresden (EK 83032016). The trial will be conducted in compliance with the protocol, the Declaration of Helsinki and good clinical practice. All relevant EU legislation and international texts on privacy will be observed and respected.
2.4. Intervention
We will deploy a combined online screening and suite of tailored evidence-based prevention programs (everyBody), which are further developments of StudentBodies. The suite of prevention programs comprises five programs, targeting different risk factors presumed to lead to or maintain eating pathology and different stages of risk for eating disorders and/or overweight and obesity. The programs aim at improving cognitive, affective and behavioral outcomes.
The cognitive-behavioral programs consist of four to twelve consecutive weekly sessions provided on an online platform. They include reading assignments, self-monitoring, a personal journal and behavioral exercises. Topics covered are healthy eating and exercise patterns, intuitive eating, self-esteem, dealing with “forbidden foods” and binge eating/purging, improving body image, coping with stress and negative emotions. The interventions are Internet-based and therefore site-independent and will be delivered from one site only. Program access for participants is possible wherever Internet access is provided.
Four programs (see Table 1) are supplemented by a moderated asynchronous group discussion to exchange experiences and thoughts with other participants. Participants in two programs will receive additional individualized weekly feedback based on their self-monitoring and journal entries. Trained clinical psychologists supervised by the study principal investigator (IB) will provide the personal feedback and moderate the online discussion board.
2.5. Assessment and data management
All assessment will be administered within the online platform. We will monitor data completeness, timeliness and internal validity. Personal data will be protected at all data processing steps according to current legislation. Appropriate technical and organizational measures are implemented to protect participant data. Personal data will be pseudonymized and any data transfer will be encrypted. After the end of the trial, data will be anonymized for further analysis. Only aggregated data will be presented in any publication of the study. Table 2 summarizes all measures used for assessments.
Table 2.
Measures and time points of assessment.
| Measure | Screening | Baseline | Mid intervention | Post intervention | FU 6 month | FU 12 month | |
|---|---|---|---|---|---|---|---|
| WCS | Weight and shape concerns | x | x | x | x | x | x |
| BMI | Assessment of underweight/overweight | x | x | x | x | x | |
| ED core symptoms | Binge eating, compensatory behavior | x | x | x | x | x | x |
| EDE-Q Restraint Scale | Restrained eating behaviors | x | |||||
| sociodemographic variables | E.g. age, occupation, education, recruitment path | x | |||||
| RSE | Self-esteem | x | x | x | x | x | |
| AQOL-8D | Quality of life | x | x | x | x | x | |
| PHQ-9 | Symptoms of depression | x | x | x | x | x | |
| GAD-7 | Symptoms of anxiety | x | x | x | x | x | |
| AUDIT-C | Alcohol consumption | x | x | x | x | x | |
| fruit and vegetable intake | Assessment of intervention effects on this measure | x | x | x | x | x | |
| IES | Intuitive eating | x | x | x | x | x | |
| CEQ (adapted for online interventions) | Expectations regarding intervention | x | x | ||||
| CD-RISC-10 | Resilience | x | |||||
| SSRQ | Self-regulation | x | |||||
| BFI-10 | Personality traits | x | |||||
| WAI-SR (adapted) | Working alliance | x | |||||
| CSRI | Health economic evaluation | x | x | x | x |
FU follow up, WCS Weight Concerns Scale, BMI Body Mass Index, EDE-Q Eating Disorder Examination-Questionnaire, RSE Rosenberg Self-Esteem Scale, AQOL-8D Assessment of Quality of Life-8D, PHQ-9 Patient Health Questionnaire 9, GAD-7 Generalized Anxiety Disorder 7, AUDIT-C Alcohol Use Disorders Identification Test-Consumption, IES Intuitive Eating Scale, CEQ Credibility/Expectancy Questionnaire, CD-RISC-10 Connor-Davidson Resilience Scale-10, SSRQ Short Self-Regulation Questionnaire, BFI-10 Big Five Inventory-10, WAI-SR Adapted Working Alliance Inventory – Short Revised, CSRI Client Service Receipt Interview.
2.6. Outcomes
2.6.1. Measures of effectiveness
Outcomes regarding eating disorder symptoms include the reduction of weight and shape concerns, assessed with the Weight Concerns Scale (WCS; Grund, 2003), the reduction of core ED symptoms (number of binge eating episodes in the last four weeks, number of compensatory behaviors in the last 4 weeks), and eating disorder psychopathology measured with the Eating Disorder Examination Questionnaire (EDE-Q; Fairburn and Beglin, 1994; Hilbert and Tuschen-Caffier, 2006). We will assess eating habits regarding intuitive eating with the Intuitive Eating Scale (IES; Herbert et al., 2013; Tylka, 2006) as well as fruit and vegetable consumption as a proxy for balanced eating habits. The primary outcome is the effectiveness of the intervention measured by the reduction WCS-scores at post-intervention compared with baseline. Secondary outcomes regarding ED pathology will be the reduction of WCS-scores at follow-up compared with baseline and the reduction of core ED symptoms at post intervention and follow-up compared with baseline in participants who had these symptoms at baseline. Besides ED pathology and measures of eating behavior, further secondary outcomes will be the increase in self-esteem, measured with the Rosenberg Self Esteem-Scale (Rosenberg, 1965), at post intervention and follow-up compared with baseline and the increase in quality of life, assessed with the Assessment of Quality of Life-8D (AQOL-8D; Richardson et al., 2011) at post intervention and follow-up compared with baseline.
2.6.2. RE-AIM measures
We will apply the RE-AIM model (Glasgow and Linnan, 2008; Kessler et al., 2013b) to guide evaluation of the program implementation, which addresses the dimensions reach, effectiveness, adoption, implementation, and maintenance. The reach of the programs will be evaluated by assessing demographic and ED specific variables of the participants and relating these to the overall population addressed by different recruitment strategies. Effectiveness will be evaluated by primary and secondary outcomes as described above. The adoption of the program will be assessed by analyzing which of the approached stakeholders (e.g., health insurances, gyms, universities, GPs) will promote the program and support recruitment. Communications with the approached stakeholders will be analyzed qualitatively to understand adoption. The implementation of the program will be assessed by analyzing how stakeholders promote the program and relating this to recruitment success. Measures included will be access paths, cost per recruit for different recruitment strategies, and participants' adherence to the program. Finally, the maintenance on the participant level will be assessed by including a 6-month follow-up assessment of primary and secondary effectiveness outcomes. Maintenance on a setting level will be assessed by analyzing stakeholder attempts to deliver the intervention at their own expense after recruitment for the study is completed.
2.6.3. Moderators and mediators
We will assess potential moderators and mediators to outcome and adherence. Symptoms of depression and anxiety will be assessed with the Patient Health Questionnaire 9 (Löwe et al., 2002) and Generalized Anxiety Disorder 7 (Spitzer et al., 2006), respectively. Alcohol consumption will be assessed with the Alcohol Use Disorders Identification Test – Consumption (Bush et al., 1998; Wurst et al., 2013). Further, participants' expectations regarding the intervention will be assessed with an adapted version of the Credibility/Expectancy Questionnaire (Devilly and Borkovec, 2000). At baseline, we will also assess participants' intentions to use the program. Resilience, i.e. the ability to cope with stress will be assessed with the Connor–Davidson Resilience Scale-10 (Campbell-Sills and Stein, 2007). Traits like self-regulation and personality traits as potential moderators will be measured with the Short Self-Regulation Questionnaire (Carey et al., 2004) and the Big Five Inventory-10 (Rammstedt and John, 2007), respectively. The working alliance of participants, i.e. how participants rate the usefulness of the intervention will be assessed with the Working Alliance Inventory - Short Revised (Hatcher and Gillaspy, 2006) which has been adapted for online prevention programs. Adherence to the intervention (e.g., the number of completed sessions, use of the discussion groups, diary entries) will be tracked automatically by the intervention platform. Moderator and mediator analyses will be conducted across all trials of the ICare research consortium and will be discussed in a separate paper. For economic evaluations the Client Service Receipt Interview (Beecham and Knapp, 2001) has been adapted to this trial and will be described in a separate paper as well.
2.7. Statistical methods
For the analysis of the data we will follow international guidelines, such as ICH E9 Statistical Guidelines for Clinical Trials (ICH E9 Expert Working Group, 1999). The primary statistical analysis will be described in a statistical analysis plan (SAP). Before data analysis a blinded review will be performed to decide on a suitable multiple imputation strategy and select potential covariables for the secondary analysis of the trial. The overall analysis strategy is structured into four phases: (i) data description, (ii) analysis of the primary hypothesis including sensitivity analyses, (iii) secondary analyses and (iv) further exploratory analyses.
The study collective will be characterized by descriptive statistical methods such as relative and absolute frequencies, mean, median, standard deviation, and inter-quartile-range (IQR) and appropriate graphics such as histograms, boxplots, and bar charts. Mean and median will reported together with 95%-confidence interval estimated. Assumptions for the appropriate statistical tests will be checked for normality by histograms, skewness, and Kolmogorov-Smirnov test, sphericity will be assessed through Mauchly test, (or any of the epsilon corrections in case it cannot be assumed), and the assumption of equality of variance-covariance matrices through Box test and Levene test.
The primary outcome in each program will be analyzed using a two-sided Wilcoxon test for paired data using the Intention-to-treat principle. Sensitivity analyses on the primary analysis will be performed using the per-protocol (PP) collective. Additional sensitivity analysis will be performed on the imputed dataset and by the application of a generalized linear mixed model. Additional safety tests will be defined in the study protocol and the statistical analysis plan. The results of the primary and secondary analyses will be presented by appropriate effect estimates and 95% confidence intervals.
Secondary analyses will be performed using multilevel mixed effect models. Separate models will be calculated for each primary and secondary outcome variable per each intervention group as well as across groups. Depending on the distribution of data in the various outcomes we will choose linear models (for normally distributed data) or negative binomial models (for left-skewed data). Each model includes assessment time as a predictor. Further predictors will be entered as necessary, e.g. baseline characteristics of participants, or variables associated with dropout. We will consistently use the nominal significance level of 0.05 (two-tailed).
The statistical analysis of the primary and secondary outcomes will be described in a statistical analysis plan that will be signed by the study committee and the responsible statistician.
2.8. Sample size calculation
To estimate the necessary sample size for the trial we aim to test the null-hypothesis that the weight and shape concerns (WSC) at post intervention will be equal to the weight and shape concerns at baseline.
For each program i the hypothesis formulates as:
Effects of each program will be assessed in independently. We will apply a two-sided Wilcoxon test for paired data since normality of the primary outcome variable cannot be assumed a priori. Using a significance level of alpha = 5% a total analyzable sample of N = 208 per program would be sufficient to detect even small intervention effects with a power of 80% (Wilcoxon test for paired data, two sided, Cohen's d = 0.20, alpha = 5%, power = 0.8). In a feasibility pilot study on the intervention suite, using the criteria specified above 47% of participants were allocated to everyBody Basic, 11% to everyBody Original, 10% to everyBody Plus, 12% to everyBody AN, and 20% to everyBody Fit. Hence, to achieve 208 analyzable cases in everyBody Plus, the program the smallest proportion of participants will be allocated to, 2080 women have to enroll in the program and complete post-intervention assessments. Assuming a dropout rate of 50%, a total of 4160 women will have to enroll.
Sample size calculations were performed using the G*Power software (Version 3.1.9).
3. Discussion and conclusion
This paper provides the study protocol for a dissemination trial of an eating disorder prevention and health promotion program. Eating disorder symptoms and overweight share several risk factors (e.g. dieting and body dissatisfaction) which can be addressed jointly in a comprehensive prevention program. Additionally, targeting multiple health problems in one program is preferable for dissemination purposes (Stice et al., 2007). So far there is little research exploring the effectiveness of such a program targeting participants of a wide age range and different stages of risk for developing an eating disorder or nutrition-related illnesses. This trial aims to contribute knowledge to this field. The impact of combined prevention for eating disorders and nutrition-related illnesses on public health will be investigated as well.
One of the strengths of this trial is the comprehensive approach to prevention, providing a program spanning from universal to indicated prevention and addressing all adult women regardless of age. Further, as prospective participants are screened for DSM-5 eating disorders and referred to treatment, if necessary, we are able to provide support even for those who cannot participate. A challenge will be avoiding and managing attrition. Based on experiences in a pilot study for this trial the estimated dropout for this study amounts to 50%. This was taken into account in the sample size calculation, but drop-out rates can reach even higher numbers and vary widely in internet-based programs (Eysenbach, 2005). To prevent dropout and maintain adherence we will send various reminders within the program platform. Participants will not be randomized into groups nor will there be control groups, both prohibiting group comparisons. As the various program versions used in this trial have been previously shown to be effective in RCTs, we will not conduct an RCT but focus on dissemination of the prevention program instead. The unique value of this trial will be the opportunity to translate research findings (i.e., a comprehensive, yet individual prevention program) into practice. The RE-AIM model will guide the exploration of external funding sources and feasible dissemination paths.
Trial status
The first participants were enrolled in the study in November 2016. Follow-up assessments for all participants are expected to be completed by May 2019.
Competing interests
The authors declare that they have no competing interests.
Funding
This project has received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No 634757.
Author contributions
IB and CJ designed the study in the first place. DG and BT contributed significantly to the study design. BN wrote the first draft of the manuscript. BN, IB, DG & CJ revised the manuscript and did the final draft. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank all journalists, organizations, health insurance companies, among the many others who help with recruitment for their support. The study will be part of the doctoral thesis of BN.
Contributor Information
Barbara Nacke, Email: barbara.nacke@tu-dresden.de.
Ina Beintner, Email: ina.beintner@tu-dresden.de.
Dennis Görlich, Email: dennis.goerlich@ukmuenster.de.
Bianka Vollert, Email: bianka.vollert@tu-dresden.de.
Juliane Schmidt-Hantke, Email: juliane.schmidt-hantke@tu-dresden.de.
Kristian Hütter, Email: kristian.huetter@tu-dresden.de.
C. Barr Taylor, Email: btaylor@stanford.edu.
Corinna Jacobi, Email: corinna.jacobi@tu-dresden.de.
References
- Andersson G., Cuijpers P., Carlbring P., Riper H., Hedman E. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiat. 2014;13(3):288–295. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschenbrenner K., Aschenbrenner F., Kirchmann H., Strauss B. Störungen des Essverhaltens bei gymnasiasten und studenten. Psychother. Psychosom. Med. Psychol. 2004;54(6):259–263. doi: 10.1055/s-2003-814925. [DOI] [PubMed] [Google Scholar]
- Bacon L., Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr. J. 2011;10:9. doi: 10.1186/1475-2891-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer S., Moessner M. Harnessing the power of technology for the treatment and prevention of eating disorders. Int. J. Eat. Disord. 2013;46:508–515. doi: 10.1002/eat.22109. [DOI] [PubMed] [Google Scholar]
- Beecham J., Knapp M. Costing psychiatric interventions. In: Thornicroft G., editor. Measuring Mental Health Needs. 2 ed. Royal College of Psychiatrists; London: 2001. pp. 200–224. [Google Scholar]
- Beintner I., Jacobi C., Taylor C.B. Effects of an internet-based prevention programme for eating disorders in the USA and Germany--a meta-analytic review. Eur. Eat. Disord. Rev. 2012;20(1):1–8. doi: 10.1002/erv.1130. [DOI] [PubMed] [Google Scholar]
- Bush K., Kivlahan D.R., McDonell M.B., Fihn S.D., Bradley K.A. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch. Intern. Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L., Stein M.B. Psychometric analysis and refinement of the Connor-Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J. Trauma. Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Carey K.B., Neal D.J., Collins S.E. A psychometric analysis of the self-regulation questionnaire. Addict. Behav. 2004;29(2):253–260. doi: 10.1016/j.addbeh.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Delinsky S.S., Wilson G.T. Weight gain, dietary restraint, and disordered eating in the freshman year of college. Eat. Behav. 2008;9(1):82–90. doi: 10.1016/j.eatbeh.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Devilly G.J., Borkovec T.D. Psychometric properties of the credibility/expectancy questionnaire. J. Behav. Ther. Exp. Psychiatry. 2000;31(2):73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. J. Med. Internet Res. 2005;7(1) doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C.G., Beglin S.J. Assessment of eating disorders: interview or self-report questionnaire? Int. J. Eat. Disord. 1994;16:363–370. [PubMed] [Google Scholar]
- Gallant A.R., Perusse-Lachance E., Provencher V., Begin C., Drapeau V. Characteristics of individuals who report present and past weight loss behaviours: results from a Canadian university community. Eat. Weight Disord. 2013;18(4):395–401. doi: 10.1007/s40519-013-0057-4. [DOI] [PubMed] [Google Scholar]
- Glasgow R.E., Linnan L.A. Evaluation of theory-based interventions. In: Glanz K., Rimer B.K., Viswanath K., editors. Health behavior and health education: Theory, research, and practice. 2008. pp. 487–508. [Google Scholar]
- Goldschmidt A.B., Wall M., Choo T.-H.J., Becker C., Neumark-Sztainer D. Shared risk factors for mood-, eating-, and weight-related health outcomes. Health Psychol. 2016;35(3):245. doi: 10.1037/hea0000283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grund K. 2003. Validierung der Weight Concerns Scale zur Erfassung von Essstörungen. (Diploma Thesis Dissertation/Thesis, Unpublished), Universität Trier, Trier. [Google Scholar]
- Hatcher R.L., Gillaspy J.A. Development and validation of a revised short version of the working alliance inventory. Psychother. Res. 2006;16(1):12–25. [Google Scholar]
- Hay P.J., Mond J., Buttner P., Darby A. Eating disorder behaviors are increasing: findings from two sequential community surveys in South Australia. PLoS One. 2008;3(2) doi: 10.1371/journal.pone.0001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert B.M., Blechert J., Hautzinger M., Matthias E., Herbert C. Intuitive eating is associated with interoceptive sensitivity. effects on body mass index. Appetite. 2013;70:22–30. doi: 10.1016/j.appet.2013.06.082. [DOI] [PubMed] [Google Scholar]
- Hilbert A., de Zwaan M., Braehler E. How frequent are eating disturbances in the population? Norms of the eating disorder examination-questionnaire. PLoS One. 2012;7(1) doi: 10.1371/journal.pone.0029125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A., Tuschen-Caffier B. Verlag für Psychotherapie; Münster: 2006. Eating Disorder Examination-Questionnaire: Deutschsprachige Übersetzung. [Google Scholar]
- Hudson J.I., Hiripi E., Pope H.G., Jr., Kessler R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICH E9 Expert Working Group Statistical principles for clinical trials: ICH harmonized tripartite guideline. Stat. Med. 1999;18(15):1903–1942. [PubMed] [Google Scholar]
- Jacobi C., Hayward C., de Zwaan M., Kraemer H.C., Agras W.S. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol. Bull. 2004;130(1):19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Jacobi C., Hütter K., Fittig E. Psychosocial risk factors for eating disorders. In: Agras S., editor. The Oxford Handbook of Eating Disorders. Oxford University Press; New York: 2018. in press. [Google Scholar]
- Jacobi C., Morris L., Beckers C., Bronisch-Holtze J., Winter J., Winzelberg A.J., Taylor C.B. Maintenance of internet-based prevention: a randomized controlled trial. Int. J. Eat. Disord. 2007;40(2):114–119. doi: 10.1002/eat.20344. [DOI] [PubMed] [Google Scholar]
- Jacobi C., Volker U., Trockel M., Taylor C. Effects of an internet-based intervention for subthreshold eating disorders: a randomized controlled trial. Behav. Res. Ther. 2012;50(2):93–99. doi: 10.1016/j.brat.2011.09.013. [DOI] [PubMed] [Google Scholar]
- Jones M., Lynch K.T., Kass A.E., Burrows A., Williams J., Wilfley D.E., Taylor C.B. Healthy weight regulation and eating disorder prevention in high school students: a universal and targeted web-based intervention. J. Med. Internet Res. 2014;16(2) doi: 10.2196/jmir.2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P.A., Chiu W.T., Deitz A.C., Hudson J.I., Shahly V.…Xavier M. The prevalence and correlates of binge eating disorder in the World Health Organization world mental health surveys. Biol. Psychiatry. 2013;73(9):904–914. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.S., Purcell E.P., Glasgow R.E., Klesges L.M., Benkeser R.M., Peek C.J. What does it mean to "employ" the RE-AIM model? Eval. Health Prof. 2013;36(1):44–66. doi: 10.1177/0163278712446066. [DOI] [PubMed] [Google Scholar]
- Krebs P., Prochaska J.O., Rossi J.S. A meta-analysis of computer-tailored interventions for health behavior change. Prev. Med. 2010;51(3–4):214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le L.K.-D., Barendregt J.J., Hay P., Mihalopoulos C. Prevention of eating disorders: a systematic review and meta-analysis. Clin. Psychol. Rev. 2017;53:46–58. doi: 10.1016/j.cpr.2017.02.001. [DOI] [PubMed] [Google Scholar]
- Leon G.R., Keel P.K., Klump K.L., Fulkerson J.A. The future of risk factor research in understanding the etiology of eating disorders. Psychopharmacol. Bull. 1997;33:405–411. [PubMed] [Google Scholar]
- Loucas C.E., Fairburn C.G., Whittington C., Pennant M.E., Stockton S., Kendall T. E-therapy in the treatment and prevention of eating disorders: a systematic review and meta-analysis. Behav. Res. Ther. 2014;63:122–131. doi: 10.1016/j.brat.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Spitzer R., Zipfel S., Herzog W. Pfizer; Karlsruhe: 2002. Gesundheitsfragebogen für Patienten (PHQ D). Komplettversion und Kurzform. Testmappe mit Manual, Fragebögen, Schablonen. [Google Scholar]
- McFarlane T., Polivy J., McCabe R.E. Help, not harm: psychological foundation for a nondieting approach toward health. J. Soc. Issues. 1999;55(2):261–276. [Google Scholar]
- Melioli T., Bauer S., Franko D.L., Moessner M., Ozer F., Chabrol H., Rodgers R.F. Reducing eating disorder symptoms and risk factors using the internet: a meta-analytic review. Int. J. Eat. Disord. 2016;49(1):19–31. doi: 10.1002/eat.22477. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D., Wall M., Story M., Standish A.R. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. J. Adolesc. Health. 2012;50(1):80–86. doi: 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D.R., Wall M.M., Haines J.I., Story M.T., Sherwood N.E., van den Berg P.A. Shared risk and protective factors for overweight and disordered eating in adolescents. Am. J. Prev. Med. 2007;33(5):359–369. doi: 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- Pietilainen K.H., Saarni S.E., Kaprio J., Rissanen A. Does dieting make you fat? A twin study. Int. J. Obes. 2012;36(3):456–464. doi: 10.1038/ijo.2011.160. [DOI] [PubMed] [Google Scholar]
- Rammstedt B., John O.P. Measuring personality in one minute or less: a 10-item short version of the big five inventory in English and German. J. Res. Pers. 2007;41(1):203–212. [Google Scholar]
- Richardson J.R.J., Elsworth G., Iezzi A., Khan M.A., Mihalopoulos C., Schweitzer I., Herrman H. Monash University, Business and Economics, Centre for Health Economics; 2011. Increasing the Sensitivity of the AQoL Inventory for the Evaluation of Interventions Affecting Mental Health. [Google Scholar]
- Rosenberg M. Princeton University Press; Princeton: 1965. Society and the Adolescent Self-Image. [Google Scholar]
- Ryan P., Lauver D.R. The efficacy of tailored interventions. J. Nurs. Scholarsh. 2002;34(4):331–337. doi: 10.1111/j.1547-5069.2002.00331.x. [DOI] [PubMed] [Google Scholar]
- Shisslak C.M., Crago M., Estes L.S. The spectrum of eating disturbances. Int. J. Eat. Disord. 1995;18:209–219. doi: 10.1002/1098-108x(199511)18:3<209::aid-eat2260180303>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Slevec J.H., Tiggemann M. Predictors of body dissatisfaction and disordered eating in middle-aged women. Clin. Psychol. Rev. 2011;31(4):515–524. doi: 10.1016/j.cpr.2010.12.002. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stice E., Cameron R.P., Killen J.D., Hayward C., Taylor C.B. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J. Consult. Clin. Psychol. 1999;67(6):967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- Stice E., Shaw H., Marti C.N. A meta-analytic review of eating disorder prevention programs: encouraging findings. Annu. Rev. Clin. Psychol. 2007;3:207–231. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- Taylor C.B., Bryson S., Luce K.H., Cunning D., Celio Doyle A., Abascal L.B.…Wilfley D.E. Prevention of eating disorders in at-risk college-age women. Arch. Gen. Psychiatry. 2006;63(8):881. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor C.B., Kass A.E., Trockel M., Cunning D., Weisman H., Bailey J., Wilfley D.E. Reducing eating disorder onset in a very high risk sample with significant comorbid depression: a randomized controlled trial. J. Consult. Clin. Psychol. 2016;84(5):402–414. doi: 10.1037/ccp0000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama A.J., Mann T., Vinas D., Hunger J.M., Dejager J., Taylor S.E. Low calorie dieting increases cortisol. Psychosom. Med. 2010;72(4):357–364. doi: 10.1097/PSY.0b013e3181d9523c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylka T.L. Development and psychometric evaluation of a measure of intuitive eating. J. Couns. Psychol. 2006;53(2):226–240. [Google Scholar]
- Watson H.J., Joyce T., French E., Willan V., Kane R.T., Tanner-Smith E.E., Egan S.J. Prevention of eating disorders: a systematic review of randomized, controlled trials. Int. J. Eat. Disord. 2016;49(9):833–862. doi: 10.1002/eat.22577. [DOI] [PubMed] [Google Scholar]
- Wurst F.M., Rumpf H.-J., Skipper G.E., Allen J.P., Kunz I., Beschoner P., Thon N. Estimating the prevalence of drinking problems among physicians. Gen. Hosp. Psychiatry. 2013;35(5):561–564. doi: 10.1016/j.genhosppsych.2013.04.018. [DOI] [PubMed] [Google Scholar]