Abstract
Individuals receiving in-center maintenance hemodialysis bear a high burden of both physical and mood symptoms. More than half of patients on hemodialysis report sleep disturbance, muscle cramps, and fatigue. Patients describe symptoms as having a deleterious effect on their quality of life, suggesting that symptom alleviation may meaningfully improve patient-reported outcomes. Moreover, patients on hemodialysis have identified symptom management as a key area for research and innovation, prioritizing symptom alleviation over other health outcomes such as mortality and biochemical indices. Despite the importance of symptoms to patients, there has been little research explicitly geared toward improving patient symptoms, and therefore minimal innovation in symptom management. In general, the physiologic underpinnings of symptoms are poorly understood, hampering the development of targeted therapies. In fact, there have been few drugs or devices approved by the US Food and Drug Administration for the indication of improving any patient-reported outcomes for patients on hemodialysis. Recognizing this gap in innovation, the Kidney Health Initiative, a public–private partnership between the American Society of Nephrology and US Food and Drug Administration, convened a workgroup to first prioritize symptoms for the development of therapeutic interventions, and then identify near-term actionable research goals for the prioritized physical symptoms of insomnia, muscle cramps, and fatigue. This paper summarizes the pathophysiology of the three prioritized symptoms, identifies key knowledge gaps, acknowledges factors that challenge development of new therapies, and offers the nephrology community actionable research goals for insomnia, muscle cramps, and fatigue.
Keywords: chronic dialysis, dialysis, end stage kidney disease, ESRD, hemodialysis, ESKD, kidney disease
Introduction
Individuals receiving in-center maintenance hemodialysis experience exceptionally high rates of morbidity and poor quality of life compared with individuals with other chronic diseases (1,2). A high burden of both physical and mood symptoms is strongly associated with these poor outcomes. More than half of patients on hemodialysis report sleep disturbance, cramping, and fatigue (3). Patients describe symptoms as substantially affecting their quality of life because of interference with social relationships, financial stability, and overall wellbeing (4,5). These data suggest that symptom alleviation may meaningfully improve patient-reported outcomes.
Moreover, patients on hemodialysis have identified symptom management as a key area for research and innovation, prioritizing symptoms over other health outcomes such as mortality and biochemical indices (6,7). Despite the importance of symptoms to patients, there has been little research geared toward improving patient symptoms, and therefore minimal innovation in symptom management over the years. Additionally, payment models focus largely on biochemical rather than patient-centered outcomes, missing an opportunity to incent symptom-focused care delivery. In general, the physiologic underpinnings of symptoms are poorly understood, hampering the development of targeted therapies. In fact, there have been few drugs or devices approved by the US Food and Drug Administration (FDA) for the indication of improving any patient-reported outcomes for patients on hemodialysis. Innovation in symptom management is essential to meet the needs of individuals receiving maintenance hemodialysis.
Kidney Health Initiative Hemodialysis Symptom Project
Overview
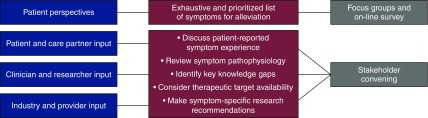
In 2016, the Kidney Health Initiative (KHI), a public–private partnership between the American Society of Nephrology and FDA, assembled an interdisciplinary workgroup to (1) conduct a study to prioritize symptoms to target for therapeutic development among in-center patients on hemodialysis, and (2) convene a stakeholder meeting to identify opportunities for targeted therapeutic development for the prioritized symptoms (Figure 1).
Figure 1.
KHI project overview. In 2016, the KHI assembled an interdisciplinary workgroup to (1) conduct a study to prioritize symptoms to target for innovation among in-center patients on hemodialysis, and (2) convene a diverse stakeholder meeting to identify specific opportunities for targeted therapeutic development for the prioritized symptoms.
Patient Prioritization of Hemodialysis Symptoms
Results of the workgroup’s prioritization study were published in an earlier issue of the Clinical Journal of the American Society of Nephrology (8). The study found that the top prioritized physical symptoms were insomnia, muscle cramps, and fatigue, and the top mood symptoms were anxiety, depression, and frustration. Participants endorsed interest in therapies such as exercise, support groups, and medications. Notably, many participants cited challenges with high pill burdens and expressed preferences for nonpharmacologic treatment options.
Stakeholder Meeting
The KHI workgroup then held a stakeholder meeting with the goals of (1) reviewing the pathophysiology of the prioritized physical symptoms, (2) identifying barriers to the development of new therapies for these symptoms, and (3) determining potential opportunities for new or improved treatment and prevention strategies. The meeting focused on physical symptoms because (1) physical symptoms are more common than mood symptoms, (2) treating physical symptoms may improve mood symptoms (4,8), and (3) at least two randomized, controlled trials (RCTs) for depression, the top mood symptom, have been conducted among patients on hemodialysis in the United States (9,10).
Meeting participants (n=23) included nephrologists, researchers with symptom expertise, clinical pharmacists, dialysis organization representatives, payers, patients, and care partners (Supplemental Table 1). The event consisted of large and small group meetings designed to spur interaction and yield specific, actionable recommendations to inform future research direction (Supplemental Figure 1). In symptom-specific small groups, participants reviewed existing treatment strategies (Table 1), discussed plausible symptom pathophysiology, and identified critical knowledge gaps and challenges (Table 2). Participants then collaboratively developed action plans with three specific, measurable, achievable, results-focused, and time-bound (S.M.A.R.T.) research goals for each symptom (Table 3). In generating and prioritizing research goals, participants weighed the available evidence, as well as the feasibility, acceptability, and immediacy of the candidate interventions.
Table 1.
Current treatment landscape for insomnia, muscle cramps, and fatiguea
| Intervention Type | Insomnia | Muscle Cramps | Fatigue |
|---|---|---|---|
| Behavioral | Cognitive–behavioral therapy | Physical exercise | Cognitive–behavioral therapy |
| Physical exercise | Physical exercise | ||
| Sleep hygiene training | Stress management | ||
| Sleep restriction | Energy conservation | ||
| Relaxation training | |||
| Pharmacologicb | Sedative hypnotics | Vasodilators | Human growth hormone |
| Anxiolytics | Neurologic agents | Anabolic steroids | |
| Antipsychotics | Quinine | Anxiolytics | |
| Antidepressants | Intradialytic saline, hypertonic saline, glucose, and mannitol | Antidepressants | |
| Antihistamines | Oral rehydration salts | Psychostimulants | |
| Melatonin | Erythropoietics | ||
| Iron | |||
| Dietary supplements | L-carnitine, potassium, magnesium, vitamins E and C, creatinine | L-carnitine, vitamins B-12 and D, essential fatty acids | |
| Dialysis-related | Home dialysis | Home dialysis | Home dialysis |
| Frequent hemodialysis | Frequent hemodialysis | Frequent hemodialysis | |
| Shift, schedule | Fluid removal rate | Shift, schedule | |
| Dialysate temperature | Treatment time | Fluid removal rate | |
| Ultrafiltration profiling | Treatment time | ||
| Sodium profiling | Extracellular hypervolemia | ||
| Dialysate composition | |||
| Dialysate temperature | |||
| Comorbid condition treatment | Restless leg syndrome | Liver disease | Depression |
| Obstructive sleep apnea | Neurologic disease | Anxiety | |
| Depression | Thyroid dysfunction | Sleep disorders | |
| Anxiety | Thyroid dysfunction | ||
| Parathyroid disease | |||
| Numerous other conditions | |||
| Other | Transplantation | Transplantation | Transplantation |
| Circadian rhythm resynchronization | Tonic water | Acupressure | |
| Light therapy | Pickle juice | Hypnosis | |
| Acupressure | Yellow mustard | ||
| Hypnosis | White sugar | ||
| Chicken broth | |||
| Salt water |
Listed therapies are representative and are not exhaustive of all potential symptom-alleviating therapies.
Includes short- and long-term drugs, prescription and over-the-counter drugs, compounds, and hormones.
Table 2.
Knowledge gaps, barriers, and potential solutions by symptom
| Symptom | Knowledge Gaps | Barriers | Potential Solutionsa |
|---|---|---|---|
| Insomniab | Limited understanding of pathophysiology (i.e., sleep-wake cycle disruption with dialysis schedule, napping during dialysis, restless leg syndrome, extracellular hypervolemia, sleep apnea, uremic toxins) | Challenges in implementing CBT in dialysis settings | CBT adapted for dialysis settings |
| Unknown if pathophysiology of insomnia differs by dialysis modality | Insomnia medications identified as high-risk by payers | Pharmacological treatments (e.g., sleep aids) | |
| Limited knowledge of effect of insomnia on patient-reported and clinical outcomes | Low adherence to CPAP machines | Improvement in CPAP technology | |
| Lack of PK/PD modeling studies of insomnia drugs among patients with ESKD | Stimulation to help patients stay awake during dialysis | ||
| Muscle crampsc | Limited understanding of pathophysiology (i.e., electrolyte imbalance, muscle fatigue, fluid shifts, hypotension, neurologic). | Limited data to drive treatment selection | Intradialytic exercise |
| No single, universally accepted definition of cramping | Patient reservations about reporting cramps to clinic personnel (personal pride, fear of being labeled as “difficult”) | Spicy substances (e.g., pickle juice, mustard) | |
| Limited knowledge of effect of cramping on patient-reported and clinical outcomes | Lack of objective approaches to dry-weight estimation | Ultrafiltration rate reduction | |
| Pharmacologic treatments (e.g., gabapentin, quinine) | |||
| Technological advances in dry-weight estimation | |||
| Fatigued | Limited understanding of pathophysiology (i.e., role of sleep disorders, mental health, anemia, ultrafiltration, uremia, comorbid medical conditions, treatment shift, modality) | Payer-driven dialysis scheduling, limited flexibility | Pharmacologic treatments (e.g., ESAs, psychostimulants) |
| Lack of standardized approach to medical work-up of fatigue | Fatigue often multifactorial and may be without clear, modifiable root cause in some individuals | Physical exercise | |
| Limited evidence on medication use for fatigue among patients with ESKD | Unclear ownership of medical work-up of fatigue (cost and provider barriers to acceptability) | CBT | |
| Lack of objective approaches to dry-weight estimation | Standardized approach to medical work-up |
CBT, cognitive–behavioral therapy; CPAP, continuous positive airway pressure; PK/PD, pharmacokinetic/pharmacodynamic; ESAs, erythropoiesis-stimulating agents.
The overarching recommendations of payment reform, dialysis care delivery system modifications, and standardized symptom data collection as avenues by which to improve symptom management were common to all three symptoms and are excluded from the table.
Insomnia small group (n=12) included patients (n=2), care partner (n=1), nephrologists (n=3), researcher content expert (n=2), clinical pharmacist (n=1), payer representative (n=1), industry representative (n=1), and dialysis organization representative (n=1).
Muscle cramps small group (n=9) included patients (n=2), nephrologists (n=5), clinical pharmacist (n=1), and dialysis organization representative (n=1).
Fatigue group (n=23) included insomnia (n=12) and muscle cramps (n=9) participants and government representatives (n=2).
Table 3.
Symptom-specific strategic action plans for top-prioritized research goals
| Goals | Actions | Potential Challengesa | Solutions | Timeframe, yr |
|---|---|---|---|---|
| Insomnia | ||||
| Test CBT and explore integration of exercise with CBT | Conduct clinical trial | CBT adaptation to dialysis setting | Expert, interdisciplinary clinical team | 4–5 |
| Provider buy-in | Provider outreach to facilitate implementation and promote sustainability | |||
| Exercising in dialysis clinic | Patient outreach, local champions | |||
| Exercising at home | ||||
| Test effectiveness of site-specific insomnia protocols including online CBT and CBT adapted for dialysis | Perform provider outreach | Health literacy of patients | Simple, accessible protocols that incorporate patient input | 3–5 |
| Develop algorithms | Internet access, tablet availability | Patient outreach, local champions | ||
| Develop infrastructure for treatment delivery | Patient adherence | Dialysis organization outreach | ||
| Test online CBT for hemodialysis | Dialysis personnel and provider buy-in | Tablet manufacturer outreach | ||
| Test safety and efficacy of at least one drug for insomnia in patients on dialysis | Select drug | Business risk to pharmaceutical companies | Pharmaceutical industry-independent funding | 2–3 |
| Conduct clinical trial | Contraindications to drugs | Industry outreach | ||
| Unknown patient preferences | Patient outreach, local champions | |||
| Muscle cramps | ||||
| Measure frequency, duration and severity of cramps to characterize problem | Investigate measures from other clinical settings | Lack of existing data | Potential KHI proposal | 1 |
| Develop and pilot test an assessment tool for cramping | Language, cultural differences | Include non-English-speaking patients and patients from different cultural backgrounds | ||
| Test acceptability of available, low-risk interventions (e.g., pickle juice, mustard) | Conduct pilot tests | Unknown patient preferences | Patient outreach, local champions | 3 |
| Dialysis personnel buy-in | Dialysis organization outreach | |||
| Lack of experience with agent | Industry partnership | |||
| Test effectiveness of treatments | Select most promising interventions from pilot testing for pragmatic clinical trial | Lack of existing data | Patient outreach, local champions | 5–7 |
| Conduct smaller clinical trials that incorporate physiologic measures | Dialysis personnel buy-in | Dialysis organization outreach | ||
| Fatigue | ||||
| Develop a standardized checklist for medical workup | Develop checklist | Need for balancing completeness and feasibility | Engage multidisciplinary partners | 1 |
| High number of potential conditions for screening | Modify evidence-based algorithms from other disciplines | |||
| Cost of work-up | Dialysis organization outreach | |||
| Potential for duplicative testing | ||||
| Ownership of findings and subsequent management | ||||
| Test efficacy of standard of care versus exercise versus exercise plus CBT | Identify exercise approach | Implementation | Align with existing social work and CBT programs at partnered dialysis organizations | 3–4 |
| Develop protocol with patient engagement (consider patient preferences and acceptance) | Sustainability | Early involvement of stakeholders to facilitate implementation and promote sustainability | ||
| Conduct clinical trial | Facility workflows | Expert, interdisciplinary clinical team | ||
| Legal | ||||
| Explore psychostimulants and assess associated patient preferences and risk tolerance | Develop protocol for PK/PD modeling study | Lack of existing data | Pharmaceutical industry-independent funding | 1 |
| Develop protocol for study assessing patient risk–benefit, tolerance, and preferences | Potential harm | Industry outreach | ||
| Contraindications to drugs | Patient preference and risk tolerance assessment | |||
| Lack of interest from pharmaceutical companies | ||||
| Negative effect on sleep | ||||
CBT, cognitive–behavioral therapy; KHI, Kidney Health Initiative, PK/PD, pharmacokinetic/pharmacodynamic.
Funding and recruitment challenges were common to all three symptoms and are excluded from the table.
Key Targets for Improving Management of All Symptoms
Meeting participants identified three overarching recommendations for spurring innovation in symptom therapeutics that transcended symptom type. First, participants recognized dialysis care delivery system aspects, such as communication, care team support, and clinic environment, as relevant to symptom management. Data from patients with advanced cancer have shown a link between symptom reporting and better patient-reported and health outcomes (11). However, data suggest that patients on dialysis may under-report their symptoms to care teams (4). To improve symptom management, clinicians must routinely address symptoms with their patients. Developing standardized care processes that foster patient–care team communication and facilitate symptom-related discussions, such as clinician rounding tools, may enhance communication. Patient support groups and mentoring programs are also potential strategies for improving symptom management and coping.
Second, participants recognized a role for payment reform, suggesting incorporation of symptom management into the definition of “quality” dialysis care. Existing quality measures focus largely on biochemical indices rather than patient-prioritized symptoms (7). Despite a lack of evidence-based interventions for many symptoms, focusing clinical interactions on symptoms may produce better outcomes (11). Payment incentives for documentation of such symptom-based interactions would promote more individualized, patient-centered rounding. The Centers for Medicare and Medicaid Services, an integral partner in payment reform efforts, convened an ESKD Patient-Reported Outcomes Technical Expert Panel in May 2017, marking an important step in efforts to align payment incentives with patient-prioritized outcomes (12).
Third, participants recommended development of standardized approaches to symptom data collection, recognizing inadequate data as a barrier to innovation. In clinical practice, the mostly commonly used symptom assessment tool is the Kidney Disease Quality of Life symptom subscale, a scale that captures degree of bother of 12 physical symptoms over the past 4 weeks. However, clinics typically administer the Kidney Disease Quality of Life annually, limiting its utility in week-to-week management decisions. Although symptom-specific patient-reported outcome measures (PROMs) such as the Insomnia Severity Index and Functional Assessment of Chronic Illness Therapy, Fatigue exist, they are used in research settings only. Efforts to develop a short, valid, dialysis-specific PROM for fatigue are underway (13). There is no existing PROM for muscle cramps among patients on dialysis. Such limitations in symptom data lead to knowledge gaps about the association of symptoms with potentially modifiable aspects of hemodialysis treatment (e.g., modality, schedule, and dialysate composition). Moreover, development of symptom-specific PROMs would facilitate testing symptom responsiveness to intervention in future research.
Symptom-Specific Gaps, Potential Solutions, and Research Goals
Insomnia
Existing data indicate that 40%–85% of patients on hemodialysis experience significant sleep disturbance (3,14,15). In a study of over 1600 patients on dialysis, 50% had trouble falling sleep, 50% woke up at night, and 49% had early morning awakening; over half reported one or more of these sleep-related symptoms all or most of the time (15). Moreover, insomnia is associated with worse quality of life and higher mortality among patients on hemodialysis (16,17).
Pathophysiology.
Although there are numerous approaches to insomnia management, few have dialysis population-specific evidence supporting them, and key knowledge gaps about the pathophysiology of insomnia in ESKD remain. Existing data reveal alterations in circadian rhythm and sleep structure, and attenuation of nocturnal melatonin surge among individuals with kidney failure, mechanisms that offer potential therapeutic targets (18,19). However, other factors also affect sleep and may influence the efficacy of insomnia therapies. Examples include medical conditions (obstructive sleep apnea, restless leg syndrome, mental health disorders, and pain), sequelae of ESKD (extracellular hypervolemia, uremic toxin accumulation, and inflammation), dialysis prescription aspects (modality, shift, and frequency), and sleep hygiene (napping) (17). Research aimed at elucidating the individual roles of factors unique to ESKD in insomnia would inform therapeutic development. Furthermore, it is important to differentiate among sleep disorders in both research and clinical practice, recognizing that different sleep-related disturbances (e.g., insomnia, sleepiness, and poor sleep quality) require different therapeutic approaches.
Therapeutic Strategies.
Patients have expressed interest in nonpharmacologic strategies for symptom management (8), rendering cognitive–behavioral therapy (CBT) an attractive insomnia treatment for patients on hemodialysis. CBT is the first-line therapy for insomnia in the general population. This therapy rests on several core principles, including the principle that psychologic problems stem, in part, from unhelpful ways of thinking or patterns of unhelpful behavior. CBT focuses on solutions, encouraging patients to challenge faulty thinking and change destructive patterns of behavior (20). It has been shown to improve sleep latency, efficiency, and quality in nondialysis populations (21,22). Challenges to administering CBT to patients on dialysis include lack of trained therapists, low patient adherence, and cost of scaling to large populations. Delivery of CBT by telehealth platforms, both in the dialysis unit and at home, may be one way to overcome these challenges. Potential limitations to this strategy, such as low patient computer literacy and limited internet access and mobile device availability, should be considered when developing CBT programs.
Medication management may be needed in some patients. However, there are critical knowledge gaps about insomnia drug safety and efficacy that stem from a dearth of pharmacokinetic/pharmacodynamic (PK/PD) modeling studies among patients on dialysis. Such knowledge gaps may also have implications for drug costs. For example, existing observational data associate benzodiazepine- and nonbenzodiazepine-receptor agonist use with higher risk of death among patients on hemodialysis (23,24). Without PK/PD modeling studies to guide safety assessment, payers may label such drugs as high risk, creating barriers to access. Unfortunately, clinical trials of drugs with lower-risk side effect profiles, such as melatonin, demonstrate that sleep improvement is not sustained (25). More dialysis-specific studies of insomnia agents, particularly drugs that promote restorative sleep, not just sleep induction, should be conducted. Moreover, research aimed at understanding patient preferences and approaches to risk–benefit decision-making for drugs that may improve insomnia and quality of life but potentially increase death risk or other adverse outcomes is needed.
Research Goals.
Participants prioritized three actionable, near-term insomnia research recommendations. First, participants identified CBT as the most important strategy to investigate. Specifically, they recommended performing an RCT to test CBT efficacy (with and without exercise) in treating insomnia among individuals on hemodialysis. Given the challenges associated with adapting CBT and sustainable exercise programs to the dialysis setting, engagement with expert, interdisciplinary teams with complementary dialysis and psychology expertise will be needed to develop such interventions. Second, the group recommended testing the effectiveness of site-specific insomnia protocols for telehealth, online and in-person CBT, in the dialysis setting. Such research is an essential foundational step for dissemination of CBT to the broader dialysis community. Provider outreach and development of clinic and organization infrastructure to support pilot tests of online CBT will be needed. Third, the group recommended testing the safety and efficacy of at least one insomnia drug in patients on dialysis via an RCT. Potential challenges to this goal include business risk to pharmaceutical companies, safety issues, and patient preferences for nonpharmacologic approaches. Industry and patient outreach, and safety studies will be important to overcoming these challenges.
Recently, there has been tangible progress toward achieving these research goals. A phase 3, randomized, open-label trial comparing the efficacy of telehealth CBT versus trazodone versus medication placebo for the treatment of chronic insomnia among patients on hemodialysis is underway (Clinicaltrial.gov identifier NCT03534284).
Muscle Cramps
The estimated prevalence of hemodialysis-related muscle cramps is 33%–78% (26). Muscle cramps can be excruciatingly painful and are a source of significant distress, interfering with sleep, activities of daily living, and quality of life (4). Moreover, muscle cramps associate with early dialysis termination and consequent underdialysis and adverse health outcomes (26).
Pathophysiology.
Critical knowledge gaps about muscle cramp pathophysiology inhibit the development of targeted interventions. Hemodialysis-related fluid and electrolyte shifts are often cited as the primary causes of cramps. However, data suggest roles for other factors including muscle fatigue, neurologic dysfunction, impaired oxygen delivery, and electrolyte, vitamin, and other dietary deficiencies, among others (26,27). In the exercise physiology literature, the muscle fatigue hypothesis suggests that muscle fatigue induces muscle contraction by inhibiting the neural mechanisms that typically block contraction (27). Predisposing factors to such fatigue-induced cramping include older age, poor conditioning, and metabolic disturbances—common conditions among patients on dialysis (27).
Therapeutic Strategies.
Although overly rapid fluid removal during dialysis can lead to cramps, oversimplification and attribution of all cramps to fluid shifts may lead to missed therapeutic opportunities. Research exploring alternative physiologic explanations is needed. Given the tendency of patients on dialysis to fatigue faster than those not on dialysis (28), emphasis on the muscle fatigue hypothesis is warranted (27). Exercise-based interventions may be effective for muscle fatigue-induced cramping. Home remedies for cramping, such as pickle juice and yellow mustard, also offer insight into the physiologic underpinnings of cramping in the setting of exercise. Exercise physiology data suggest that pungent tastes, like vinegar and ginger, can stimulate an oropharyngeal neural reflex that inhibits hyperactive α-motor neurons, leading to muscle relaxation and cramp relief (29,30). Such low-cost and seemingly low-risk interventions that are already in use by some patients, are ripe for safety testing and pragmatic trials.
In addition to significant gaps in knowledge about cramp pathophysiology, there is no accepted definition of, or PROM for, muscle cramps. Without standardized data capture, we lack the capacity to accurately (1) assess and compare muscle cramp prevalence, severity, and frequency; (2) study the effect of cramps on patient-reported and clinical outcomes; and (3) measure cramp response to intervention. Cramps can take many forms and simply asking patients a single question annually about cramps as part of a health-related quality of life survey is inadequate. There are also potential reporting barriers specific to muscle cramps. In a prior qualitative study, patients noted that personal pride and societal pressure sometimes affected their decisions to withhold the reporting of symptoms from their care teams (4); this was reinforced by patient comments during the stakeholder meeting.
Research Goals.
Such knowledge gaps and reporting barriers led participants to recommend developing a muscle cramp PROM to facilitate characterization of population burden as its first actionable, near-term research goal. Given the potential challenges in capturing cramps across culturally divergent populations, inclusion of individuals from diverse backgrounds in measure development is essential. Second, participants recommended testing patient acceptability of available, low-risk interventions such as pickle juice and mustard to inform intervention selection for a future trial. Actionable steps in this regard include patient and dialysis organization engagement and exploration of potential funding opportunities. Third, the group recommended conducting a pragmatic clinical trial to test the effectiveness of the most promising treatment identified in acceptability testing. Additionally, given the gaps in pathophysiology knowledge, smaller trials incorporating physiologic measures to advance mechanistic knowledge will be important in efforts to uncover new therapeutic approaches.
Offering optimism for future advances, efforts to develop a PROM for dialysis-related muscle cramps are underway, as evidenced by the endorsement of a related project proposal by the KHI (31).
Fatigue
Fatigue is perhaps the most common symptom experienced by patients on hemodialysis, with prevalence estimates ranging 60%–97% (7). A recent international consensus effort prioritized fatigue as one of the most important outcomes for hemodialysis clinical trials (7). Fatigue is associated with a higher risk of mortality and depression and lower quality of life among individuals on dialysis (32).
Pathophysiology and Therapeutic Strategies.
The multifactorial nature of fatigue and dearth of targeted treatments for fatigue in any population present challenges to innovation in fatigue therapeutics for the dialysis population. Contributors to fatigue include comorbid medical conditions (mood disorders, thyroid and parathyroid dysfunction, sleep disorders, and others), muscle fatigue, inflammation, nutritional status, medication side effects, and dialysis-related factors such as toxin accumulation, volume status, and potentially, modality, schedule, treatment time, and fluid removal practices (33). Data supporting causal associations between these factors and fatigue are weak, but do point to therapeutic development opportunities. Inflammatory cytokines such as IL-6 and TNF-α are potential targets because they are elevated in ESKD and associate with lower functional status and higher mortality among patients on dialysis (34,35). Dialysis treatment modifications, and particularly fluid removal practices, offer actionable targets, but data supporting their effects are mixed (36,37), and patient acceptance of treatment time extension is not clear (38). Additional bench and translational research aimed at elucidating fatigue pathophysiology may point to opportunities for targeted drug development.
Challenges associated with determining the drivers of patient-specific fatigue affect development of targeted interventions. Most patients on dialysis have numerous potential fatigue contributors given their high burden of comorbid conditions and prescribed medications, and there is not an accepted approach to the medical work-up of fatigue. More standardized approaches to fatigue work-up may help identify candidate targets for intervention. However, work-up cost and unclear ownership of results could challenge implementing such an approach in the dialysis setting.
Research Goals.
Participants prioritized three actionable, near-term fatigue research goals. First, participants recommended developing a standardized checklist for medical work-up of fatigue to help clinicians identify patient-specific fatigue contributors. To overcome challenges associated with the need to balance completeness, feasibility, cost, duplicative testing, and ownership of results, engagement of multidisciplinary partners (e.g., geriatricians and oncologists), and review of fatigue algorithms in nondialysis populations will be necessary. Second, the group recommended performing a RCT to test the efficacy of standard of care versus exercise versus exercise and CBT in treating fatigue among patients on hemodialysis. The group recognized challenges with scaling exercise programs, noting barriers related to implementation, sustainability, and facility workflows. Aligning CBT and exercise interventions with existing social work programs and engaging expert, interdisciplinary teams throughout the research process will help overcome these challenges. Third, the group recommended exploring psychostimulants as a potential therapy and called for physiologically based PK/PD modeling studies and studies assessing patient risk–benefit, tolerance, and preferences. Early engagement with industry will be essential to realizing these pharmacologic, study-related goals.
As with insomnia and cramping, there is reason for optimism. An RCT testing the effectiveness of collaborative care (a multidisciplinary management plan with individualized pharmacologic and/or behavioral therapy interventions) on fatigue among patients on hemodialysis is underway (Clinicaltrials.gov identifier NCT03440853).
Charting a Path Forward to Improve the Hemodialysis Symptom Experience
Innovative research designed to improve symptom management among individuals receiving hemodialysis has the potential to meaningfully affect patients’ lives. KidneyX, a public–private accelerator, is one exciting new path for such innovation (39). Tables 3 and 4 display overarching recommendations for fostering innovation in symptom management. Initial focus on patient-prioritized symptoms, such as insomnia, muscle cramps, and fatigue, will ensure that research is responsive to the most pressing patient needs. Investigation of CBT with and without exercise as management strategies and execution of drug PK/PD modeling studies are research areas that offer opportunity for meaningful developments across all three prioritized symptoms. Additionally, drawing upon known and yet-to-be-discovered symptom pathophysiology from non-nephrology disciplines will create opportunities to develop more targeted therapies. Once therapies are identified, partnerships with patients, dialysis provider organizations, medical providers, and industry will be essential for designing and implementing clinical trials testing the effect of interventions on symptom management.
Table 4.
Overarching recommendations for fostering innovation in symptom management
| No. | Recommendation |
|---|---|
| 1. | Develop definitions for individual symptoms accounting for culturally divergent patient experiences. |
| 2. | Develop validated and standardized measures for individual symptoms to accurately assess burden. |
| 3. | Conduct research to better understand the biologic basis for these symptoms in patients on dialysis. |
| 4. | Conduct clinical trials of promising treatments including drugs, devices, and behavioral therapy. |
| 5. | Test modifying dialysis care delivery to support and seamlessly integrate evidence-based treatments. |
| 6. | Demonstrate the effect of symptoms on patient-reported and clinical outcomes. |
| 7. | Advocate for payment reform that incentivizes improved treatment and management of symptoms. |
| 8. | Perform focused prioritization and gap assessments among patients on peritoneal dialysis and patients on home-based hemodialysis. |
Disclosures
J.E.F. has received speaking honoraria from American Renal Associates, Fresenius Medical Care, North America, American Society of Nephrology, National Kidney Foundation, and multiple universities in the past 2 years. J.E.F. has received research funding for studies unrelated to this project from the Renal Research Institute, a subsidiary of Fresenius Medical Care, North America in the past 2 years. A.B.P. has current funding from the US Food and Drug Administration and the Renal Research Institute. A.B.P. has served as a consultant for Pfizer Inc., AMAG Pharmaceuticals, Rockwell Medical, and Baxter. E.M.A.-R. has received funding from Astra Zeneca and Bayer Pharmaceuticals. W.L.S.P. has received speaking honoraria from the American Society of Nephrology, National Kidney Foundation, and the American Nephrology Nurses Association, and has received research funding in the past 2 years for studies unrelated to this project from the College of Pharmacy at University of Minnesota.
Supplementary Material
Acknowledgments
We thank all of the attendees for their contributions to the meeting discussions. This work was supported by the Kidney Health Initiative (KHI), a public–private partnership between the American Society of Nephrology, the US Food and Drug Administration, and >75 member organizations and companies to enhance patient safety and foster innovation in kidney disease.
KHI funds were used to defray costs incurred during the conduct of the project, including project management support, which was expertly provided by American Society of Nephrology staff members Melissa West and Rick Kempinksi. There was no honorarium or other financial support provided to KHI workgroup members. J.E.F. is supported by National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health grant K23 DK109401. M.B.R. received support from grant KL2 TR000421 from the National Center for Advancing Translational Sciences, and from the extramural grant program of Satellite Healthcare, a not-for-profit renal care provider.
Because R.M. is the Editor-in-Chief of the Clinical Journal of the American Society of Nephrology, he was not involved in the peer review process for this manuscript. Another editor oversaw the peer review and decision-making process for this manuscript. Ian de Boer, a Deputy Editor of the Clinical Journal of the American Society of Nephrology, is at the same institution as some of the authors, including the Editor-in-Chief, and therefore was also not involved in the peer review process for this manuscript.
The views and opinions expressed in this publication are those of the authors and do not necessarily reflect the official policies of any KHI member organization, the US Department of Veterans Affairs, or the US Department of Health and Human Services, nor does any mention of trade names, commercial practices, or organization imply endorsement by the US Government. The authors of this paper had final review authority and are fully responsible for its content. KHI makes every effort to avoid actual, potential, or perceived conflicts of interest that may arise as a result of industry relationships or personal interests among the members of the workgroup. More information on KHI, the workgroup, and the conflict of interest policy can be found at www.kidneyhealthinitiative.org. The content of this article does not reflect the views or opinions of the American Society of Nephrology (ASN) or the Clinical Journal of the American Society of Nephrology (CJASN). Responsibility for the information and views expressed therein lies entirely with the author(s).
See Supplemental Table 1 for meeting participants.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.07670618/-/DCSupplemental.
References
- 1.Merkus MP, Jager KJ, Dekker FW, de Haan RJ, Boeschoten EW, Krediet RT: Physical symptoms and quality of life in patients on chronic dialysis: Results of The Netherlands Cooperative Study on Adequacy of Dialysis (NECOSAD). Nephrol Dial Transplant 14: 1163–1170, 1999 [DOI] [PubMed] [Google Scholar]
- 2.Valderrábano F, Jofre R, López-Gómez JM: Quality of life in end-stage renal disease patients. Am J Kidney Dis 38: 443–464, 2001 [DOI] [PubMed] [Google Scholar]
- 3.Abdel-Kader K, Unruh ML, Weisbord SD: Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol 4: 1057–1064, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flythe JE, Dorough A, Narendra JH, Forfang D, Hartwell L, Abdel-Rahman E: Perspectives on symptom experiences and symptom reporting among individuals on hemodialysis. Nephrol Dial Transplant 33: 1842–1852, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox KJ, Parshall MB, Hernandez SHA, Parvez SZ, Unruh ML: Symptoms among patients receiving in-center hemodialysis: A qualitative study. Hemodial Int 21: 524–533, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manns B, Hemmelgarn B, Lillie E, Dip SC, Cyr A, Gladish M, Large C, Silverman H, Toth B, Wolfs W, Laupacis A: Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol 9: 1813–1821, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evangelidis N, Tong A, Manns B, Hemmelgarn B, Wheeler DC, Tugwell P, Crowe S, Harris T, Van Biesen W, Winkelmayer WC, Sautenet B, O’Donoghue D, Tam-Tham H, Youssouf S, Mandayam S, Ju A, Hawley C, Pollock C, Harris DC, Johnson DW, Rifkin DE, Tentori F, Agar J, Polkinghorne KR, Gallagher M, Kerr PG, McDonald SP, Howard K, Howell M, Craig JC; Standardized Outcomes in Nephrology–Hemodialysis (SONG-HD) Initiative: Developing a set of core outcomes for trials in hemodialysis: An international delphi survey. Am J Kidney Dis 70: 464–475, 2017 [DOI] [PubMed] [Google Scholar]
- 8.Flythe JE, Hilliard T, Castillo G, Ikeler K, Orazi J, Abdel-Rahman E, Pai AB, Rivara MB, St Peter WL, Weisbord SD, Wilkie C, Mehrotra R: Symptom prioritization among adults receiving in-center hemodialysis: A mixed methods study. Clin J Am Soc Nephrol 13: 735–745, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cukor D, Ver Halen N, Asher DR, Coplan JD, Weedon J, Wyka KE, Saggi SJ, Kimmel PL: Psychosocial intervention improves depression, quality of life, and fluid adherence in hemodialysis. J Am Soc Nephrol 25: 196–206, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hedayati SS, Daniel DM, Cohen S, Comstock B, Cukor D, Diaz-Linhart Y, Dember LM, Dubovsky A, Greene T, Grote N, Heagerty P, Katon W, Kimmel PL, Kutner N, Linke L, Quinn D, Rue T, Trivedi MH, Unruh M, Weisbord S, Young BA, Mehrotra R: Rationale and design of A Trial of Sertraline vs. Cognitive Behavioral Therapy for End-stage Renal Disease Patients with Depression (ASCEND). Contemp Clin Trials 47: 1–11, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, Rogak L, Bennett AV, Dueck AC, Atkinson TM, Chou JF, Dulko D, Sit L, Barz A, Novotny P, Fruscione M, Sloan JA, Schrag D: Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol 34: 557–565, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Medicare and Medicaid Services: End-Stage Renal Disease Patient-Reported Outcomes Technical Expert Panel Final Report, 2017. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/TEP-Current-Panels.html. Accessed May 28, 2018
- 13.Ju A, Unruh M, Davison S, Dapueto J, Dew MA, Fluck R, Germain M, Jassal SV, Obrador G, O’Donoghue D, Josephson MA, Craig JC, Viecelli A, O’Lone E, Hanson CS, Manns B, Sautenet B, Howell M, Reddy B, Wilkie C, Rutherford C, Tong A; SONG-HD Fatigue Workshop Collaborators: Establishing a core outcome measure for fatigue in patients on hemodialysis: A Standardized Outcomes in Nephrology-Hemodialysis (SONG-HD) consensus workshop report. Am J Kidney Dis 72: 104–112, 2018 [DOI] [PubMed] [Google Scholar]
- 14.Weisbord SD, Fried LF, Arnold RM, Fine MJ, Levenson DJ, Peterson RA, Switzer GE: Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol 16: 2487–2494, 2005 [DOI] [PubMed] [Google Scholar]
- 15.Anand S, Johansen KL, Grimes B, Kaysen GA, Dalrymple LS, Kutner NG, Chertow GM: Physical activity and self-reported symptoms of insomnia, restless legs syndrome, and depression: The comprehensive dialysis study. Hemodial Int 17: 50–58, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehrotra R, Chiu YW, Kalantar-Zadeh K, Bargman J, Vonesh E: Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch Intern Med 171: 110–118, 2011 [DOI] [PubMed] [Google Scholar]
- 17.Lindner AV, Novak M, Bohra M, Mucsi I: Insomnia in patients with chronic kidney disease. Semin Nephrol 35: 359–372, 2015 [DOI] [PubMed] [Google Scholar]
- 18.Koch BC, Nagtegaal JE, Kerkhof GA, ter Wee PM: Circadian sleep-wake rhythm disturbances in end-stage renal disease. Nat Rev Nephrol 5: 407–416, 2009 [DOI] [PubMed] [Google Scholar]
- 19.Koch BC, Nagtegaal JE, Hagen EC, Wee PM, Kerkhof GA: Different melatonin rhythms and sleep-wake rhythms in patients on peritoneal dialysis, daytime hemodialysis and nocturnal hemodialysis. Sleep Med 11: 242–246, 2010 [DOI] [PubMed] [Google Scholar]
- 20.American Psychological Association: What Is Cognitive Behavioral Therapy? 2018. Available at: http://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral.aspx. Accessed September 4, 2018
- 21.Jernelöv S, Lekander M, Blom K, Rydh S, Ljótsson B, Axelsson J, Kaldo V: Efficacy of a behavioral self-help treatment with or without therapist guidance for co-morbid and primary insomnia--a randomized controlled trial. BMC Psychiatry 12: 5, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vincent N, Lewycky S: Logging on for better sleep: RCT of the effectiveness of online treatment for insomnia. Sleep 32: 807–815, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elder SJ, Pisoni RL, Akizawa T, Fissell R, Andreucci VE, Fukuhara S, Kurokawa K, Rayner HC, Furniss AL, Port FK, Saran R: Sleep quality predicts quality of life and mortality risk in haemodialysis patients: Results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 23: 998–1004, 2008 [DOI] [PubMed] [Google Scholar]
- 24.Winkelmayer WC, Mehta J, Wang PS: Benzodiazepine use and mortality of incident dialysis patients in the United States. Kidney Int 72: 1388–1393, 2007 [DOI] [PubMed] [Google Scholar]
- 25.Russcher M, Koch BC, Nagtegaal JE, van Ittersum FJ, Pasker-de Jong PC, Hagen EC, van Dorp WT, Gabreëls B, Wildbergh TX, van der Westerlaken MM, Gaillard CA, Ter Wee PM: Long-term effects of melatonin on quality of life and sleep in haemodialysis patients (Melody study): A randomized controlled trial. Br J Clin Pharmacol 76: 668–679, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moledina DG, Perry Wilson F: Pharmacologic treatment of common symptoms in dialysis patients: A narrative review. Semin Dial 28: 377–383, 2015 [DOI] [PubMed] [Google Scholar]
- 27.Bergeron M: Muscle cramps during exercise: Is it fatigue or electrolyte deficit? Curr Sports Med Rep 7: S50–S55, 2008 [Google Scholar]
- 28.Hellberg M, Höglund P, Svensson P, Abdulahi H, Clyne N: Decline in measured glomerular filtration rate is associated with a decrease in endurance, strength, balance and fine motor skills. Nephrology (Carlton) 22: 513–519, 2017 [DOI] [PubMed] [Google Scholar]
- 29.Miller KC: Rethinking the cause of exercise-associated muscle cramping: Moving beyond dehydration and electrolyte losses. Curr Sports Med Rep 14: 353–354, 2015 [DOI] [PubMed] [Google Scholar]
- 30.Schwellnus MP: Cause of exercise associated muscle cramps (EAMC)--altered neuromuscular control, dehydration or electrolyte depletion? Br J Sports Med 43: 401–408, 2009 [DOI] [PubMed] [Google Scholar]
- 31.Kidney Health Initiative: Sixth Annual KHI Stakeholders Meeting, 2018. Available at: https://www.asn-online.org/khi/meetings.aspx. Accessed May 29, 2018
- 32.Bossola M, Di Stasio E, Antocicco M, Panico L, Pepe G, Tazza L: Fatigue is associated with increased risk of mortality in patients on chronic hemodialysis. Nephron 130: 113–118, 2015 [DOI] [PubMed] [Google Scholar]
- 33.Jhamb M, Weisbord SD, Steel JL, Unruh M: Fatigue in patients receiving maintenance dialysis: A review of definitions, measures, and contributing factors. Am J Kidney Dis 52: 353–365, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Balakrishnan VS, Guo D, Rao M, Jaber BL, Tighiouart H, Freeman RL, Huang C, King AJ, Pereira BJ; HEMO Study Group: Cytokine gene polymorphisms in hemodialysis patients: Association with comorbidity, functionality, and serum albumin. Kidney Int 65: 1449–1460, 2004 [DOI] [PubMed] [Google Scholar]
- 35.Kimmel PL, Phillips TM, Simmens SJ, Peterson RA, Weihs KL, Alleyne S, Cruz I, Yanovski JA, Veis JH: Immunologic function and survival in hemodialysis patients. Kidney Int 54: 236–244, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bossola M, Marzetti E, Di Stasio E, Monteburini T, Cenerelli S, Mazzoli K, Parodi E, Sirolli V, Santarelli S, Ippoliti F, Nebiolo PE, Bonomini M, Melatti R, Vulpio C: Prevalence and associated variables of post-dialysis fatigue: Results of a prospective multicentre study. Nephrology (Carlton) 23: 552–558, 2018 [DOI] [PubMed] [Google Scholar]
- 37.Hussein WF, Arramreddy R, Sun SJ, Reiterman M, Schiller B: Higher ultrafiltration rate is associated with longer dialysis recovery time in patients undergoing conventional hemodialysis. Am J Nephrol 46: 3–10, 2017 [DOI] [PubMed] [Google Scholar]
- 38.Flythe JE, Mangione TW, Brunelli SM, Curhan GC: Patient-stated preferences regarding volume-related risk mitigation strategies for hemodialysis. Clin J Am Soc Nephrol 9: 1418–1425, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.US Department of Health and Human Services. IDEA Lab: What is KidneyX? 2018. Available at: https://www.hhs.gov/idealab/kidneyx/. Accessed September 12, 2018 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.