Abstract
BACKGROUND:
The detection of pathogenic fungus is an important step and key to assessing the sensitivity of the antifungal drugs, and therefore choosing an effective treatment method.
AIM:
To identify Malassezia species from scales of a patient with pityriasis versicolor.
METHODS:
Three hundred patients with pityriasis versicolor who were positive with direct examination, were isolated by culture.
RESULTS:
Identification of Malassezia species by culture: the growth rate was 90.3%; the detection rate was 97.0%, including 11 species: M. globosa (42.4%), M. dermatitis (17.3%), M. furfur (14.4%). M. globosa was the most prevalent species in the 20-29 group 36.5%, in hyphae and yeast cells (42.2%).
CONCLUSION:
M. globosa is the main cause of pityriasis versicolor in Vietnam.
Keywords: Pityriasis versicolor, Yeast, Malassezia spp
Introduction
Malassezia spp. Is lipophilic yeast which is of the normal cutaneous commensal flora on humans and animals. Malassezia includes 14 species in which M. globosa, M. furfur, M. sympodialis are the most common. Symptoms of Malassezia fungal diseases include pityriasis versicolor, seborrheic dermatitis, atopic dermatitis, Malassezia folliculitis, psoriasis, even skin cancer [1], [2] in all parts of the world, especially in tropical countries (18% of the population) [3].
In the world, depending on climate, geographic conditions, there is a difference between the distribution of Malassezia species in other areas.
Therefore, we carried out a study to identify Malassezia species that caused pityriasis versicolor (PV) by the culture at National Hospital of Dermatology and Venereology (NHDV), Viet Nam.
Methods
A cross-section study of 300 patients with PV who had a positive direct examination test at NHDV from January 2016 to December 2016. Skin scales samples: Identification culture. MDixon media culture, SDA, TABLE 20, Tween 40, Tween 60, Tween 80, Malassezia Chromatase. Data were collected by SPSS 23.0 software and statistical tests study, to determine the incidence of Malassezia species.
Results
On 271 cultured samples, 11 Malassezia species were identified: M. globosa, M. furfur, M. dermatis, M. sympodialis, M. restricta, M. obtusa, M. slooffiae, M. pachydermatis, M. japonica, M. equina, and M. cuniculi.
We tested the development of M. pachydermatis on Sabouraud agar (SDA). M. restricta has a negative Catalase test. Then, proceeding with the reaction with Tween 20, Tween 40, Tween 60, Tween 80. Next, comparing with colony morphology and microscopic staining of three species including M. sympodialis, M. japonica, M. slooffiae. Some other species cultured in CHROM agar Malassezia, based on morphology, colour and colony characteristics, identified six species including M. furfur, M. dermatis, M. globosa, M. obtusa, M. cuniculi, and M. yamatoensis.
Figure 1.
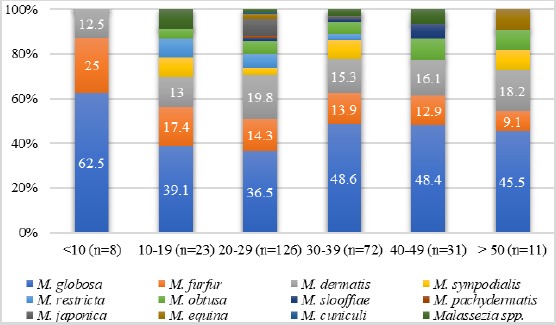
Distribution of Malassezia species isolated according to a group of ages
In different age groups, M. globosa is a common species, following M. dermatis, M. furfur. We did not find M. furfur in humans who was over 50 years old, while M. obtusa which was normal flora, had a higher rate. In the group of under 10 years old, only found 3 species: M. globosa, M. furfur, M. dermatis. The male/female ratio is approximately 2/1. Men may be the main occupational and physical activity partners, so exposure to a variety of environmental factors may be a favourable factor for the pathogenicity of the fungus, which can lead to infection rate.
Figure 2.
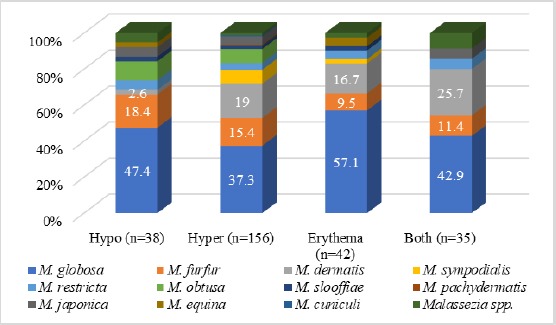
Distribution of Malassezia species isolated according to colour lesions
Fungus infection in the male is higher than female. In the study, we found that hyperpigmented was the most common with 58.3%, following Hypopigmented, Erythema and Both.
Figure 3.
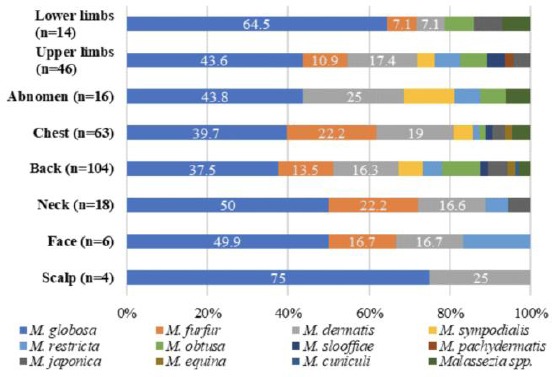
Distribution of Malassezia species isolated according to the site of lesions
Discussion
Results in the study showed a higher method of Abbas Rasi và cs (2009) [4], Kaneko Takamasa et al., (2011) [5], Rezvan Talaee et al., (2014) [6]. Nguyen Dinh Nga et al., (2007) [7]. However, in addition to the culture environment, climate and geography are also a major factor influencing the distribution of Malassezia species. Also, some new species have been discovered in recent years, such as M. equina, M. caprae (2007), M. cuniculi (2011), can increase the number of species discovered.
Results matched with Karakas et al., (2009) [8] with 47.7%. As such, M. globosa was found in the different area of the world and Vietnam. M. furfur was referred to as the most frequent species and most common disease, but in our study, only 14.4% was ranked third after M. globosa (42.4%) and M. dermatis (17.3%). In particular, M. furfur grows well in mDixon agar, which is more easily indentified than other species. Our results are similar to those of other authors: Karakas et al., (2009) [8], Rezvab Talaee et al., (2014) [6].
A study by Nguyen Dinh Nga et al., (2007) conducted in Vietnam showed that the majority of species were M. furfur (57.33%) and M. globosa [7]. Our results from Table 1 show that M. globosa is the common species (42.4%), M. furfur (14.4%).
Table 1.
Identification of Malassezia species by culture
| Species | N | % |
|---|---|---|
| M. globosa | 115 | 42.4 |
| M. furfur | 39 | 14.4 |
| M. dermatis | 47 | 17.3 |
| M. sympodialis | 13 | 4.8 |
| M. restricta | 12 | 4.4 |
| M. obtusa | 16 | 5.9 |
| M. slooffiae | 5 | 1.8 |
| M. pachydermatis | 1 | 0.4 |
| M. japonica | 11 | 4.1 |
| M. equine | 3 | 1.1 |
| M. cuniculi | 1 | 0.4 |
| Malassezia spp. | 8 | 3.0 |
| Total | 271 | 100 |
In comparable climates, our findings are similar with other authors: Talaee et al., (2014) [6] with hyperpigmented 50%; Karakas et al., (2009) [8] with 47.4%. We found that the hyperpigmented lesions were mainly related to M. globosa by Talaee et al., (2014), Karakas et al., (2009) M. dermatis is quite common in erythema lesions [6], [8]. M. sympodialis is mainly found in hyperpigmented [9].
In conclusion, using culture method, we identified 11 Malassezia species including M. globosa (42.4%); M. dermatis (17.3%); M. furfur (14.4%). M. globosa is the main cause of pityriasis versicolor in Vietnam.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Pedrosa AF, Lisboa C, Rodrigues AG. Malassezia infections with systemic involvement:Figures and facts. The Journal of Dermatology. 2018;45(11):1278–82. doi: 10.1111/1346-8138.14653. https://doi.org/10.1111/1346-8138.14653 PMid:30264900. [DOI] [PubMed] [Google Scholar]
- 2.Prohic A, Jovovic Sadikovic T, Krupalija-Fazlic M, Kuskunovic-Vlahovljak S. Malassezia species in healthy skin and in dermatological conditions. International Journal of Dermatology. 2016;55(5):494–504. doi: 10.1111/ijd.13116. https://doi.org/10.1111/ijd.13116 PMid:26710919. [DOI] [PubMed] [Google Scholar]
- 3.Velegraki A, Cafarchia C, Gaitanis G, Iatta R, Boekhout T. Malassezia infections in humans and animals:pathophysiology, detection, and treatment. PLoS Pathogens. 2015;11(1):e1004523. doi: 10.1371/journal.ppat.1004523. https://doi.org/10.1371/journal.ppat.1004523 PMid:25569140 PMCid:PMC4287564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasi A, Naderi R, Behzadi AH, Falahati M, Farehyar S, Honarbakhsh Y, et al. Malassezia yeast species isolated from Iranian patients with pityriasis versicolor in a prospective study. Mycoses. 2010;53(4):350–5. doi: 10.1111/j.1439-0507.2009.01727.x. PMid:19500258. [DOI] [PubMed] [Google Scholar]
- 5.Kaneko T. A study of culture-based easy identification system for Malassezia. Medical mycology journal. 2011;52(4):297–303. doi: 10.3314/mmj.52.297. https://doi.org/10.3314/mmj.52.297 PMid:22123328. [DOI] [PubMed] [Google Scholar]
- 6.Talaee R, Katiraee F, Ghaderi M, Erami M, Kazemi Alavi A, Nazeri M. Molecular Identification and Prevalence of Malassezia Species in Pityriasis Versicolor Patients From Kashan, Iran. Jundishapur Journal of Microbiology. 2014;7(8) doi: 10.5812/jjm.11561. https://doi.org/10.5812/jjm.11561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyên Đinh Nga, LêThịNgọc Huê, Phạm Ngọc Hiên Vy. isolating and identifying Malassezia spp. from scales of Vietnameses volunteered. Ho Chi Minh City Medicine Magazine. 2007;11(2):186–91. [Google Scholar]
- 8.Karakas M, Turac-Bicer A, Ilkit M, Durdu M, Seydaoglu G. Epidemiology of pityriasis versicolor in Adana, Turkey. The Journal of dermatology. 2009;36(7):377–82. doi: 10.1111/j.1346-8138.2009.00663.x. https://doi.org/10.1111/j.1346-8138.2009.00663.x PMid:19583685. [DOI] [PubMed] [Google Scholar]
- 9.Chokoeva AA, Wollina U, Lotti T, Maximov GK, Lozev I, Tchernev G. Psoriasiform Dermatophytosis in a Bulgarian Child. Open Access Maced J Med Sci. 2018;6(1):118–119. doi: 10.3889/oamjms.2018.009. https://doi.org/10.3889/oamjms.2018.009 PMid:29484004 PMCid:PMC5816278. [DOI] [PMC free article] [PubMed] [Google Scholar]


