Abstract
AIM:
To evaluate the effectiveness and safety of micro-needling therapy in atrophic acne scar treatment.
METHOD:
A prospective, single centred study was implemented in a total of 31 patients suffering from atrophic acne scar grade 2 to 4 of Goodman and Baron scaring grading system was recruited. They were treated by microneedle derma roller every week in 3 months. The scars were evaluated by a magic system camera and by dermatologists clinically using Goodman and Baron scaring grading system, and Lipper and Perez score at baseline, at final treatment, 1 month and 2 months after the final treatment.
RESULTS:
The results showed improvement in all patients. The mean of Goodman and Barron’s grade was decreased from 3.29 ± 0.59 at baseline, 2.23 ± 0.56 at final treatment, 1.93 ± 0.58 one month after the completion of therapy and to 1.77 ± 0.57 two months after the completion of therapy (with the p-value < 0.05). Similarly, Lipper and Perez score also dropped significantly from 36.48 ± 12.07 at baseline to 23.16 ± 15.01 at final treatment, to 17.83 ± 7.00 one month after the final treatment and to 16.37 ± 7.29 at two months after the final treatment (p-value < 0.05). Skin roughness and hyperpigmented spots got improved significantly. History of having nodular-cystic or vulgaris acne did not affect the effectiveness of the therapy. Side effects of the therapy were burning sensation, erythema but they were very mild and recovered in 1-2 days. No severe complication and post-inflammatory hyperpigmentation were noted. 83.3% of the patients satisfied after the completion of the therapy.
CONCLUSION:
Skin needling is an effective and safe method for the treatment of atrophic acne scars.
Keywords: Atrophic acne scarring, Skin needling, Derma roller
Introduction
Acne is a very common skin disease with the prevalence among adolescent is up to 80% [1]. The atrophic scar is a common acne complication, accounted for 11% of the acne vulgaris cases [2], [3] and affects patients’ quality of life very much. Effective atrophic acne scar treatment is desired and has been challenging dermatologists. Many techniques have been used to improve acne atrophic scars such as subcision, punch technique, chemical peeling, dermabrasion, laser, trichloroacetic acid application etc. Skin needling, one of the collagen induction therapy, is considered safe and effective. The technique uses sterilised microneedles to puncture skin superficially, resulting in stimulating new collagen synthesis and collagen deposition through activating an inflammatory response. Skin micro-needling induces normal wound healing, in which, collagen is formed in the dermis over 12 to 18 months in the remodelling stage [3], [4], [5], [6].
In 1994, Orentreich described the use of a skin needling to release fibrous strands responsible for depressed cutaneous scars and wrinkles [7]. The process involved the insertion and manoeuvring of a tri-bevelled hypodermic needle into the skin to disrupt the underlying connective tissue that tethered down the skin. In 1997, Dr Andre Camirand et al. reported that needle dermabrasion procedure using a tattoo gun devoid of ink could improve surgical scars both in their appearance and texture as well [1]. He experimented a needling procedure using high-speed tattoo gun to treat non-pigmented facelift scars once every 2 to 8 weeks. The expected end-point of the procedure was pinpoint bleeding at scars’ base. He found that the scars were improved in both texture and colour and no side effects or complication was documented. However, Dr Desmond Fernandes said that the procedure penetrated the skin too shallow and needles which penetrate deeper could stimulate the production of elastin fibres better. Based on these principles, Dr Fernandes designed a needle roller, consisting of a circular cylinder mounted on tiny needles. In 1999, he presented his invention of the needle at a conference in San Francisco [9]. In 2005, Dr Fernandes and colleagues conducted a study on concave scars, wrinkles, skin ageing of 480 patients in Germany and South Africa. The results were good in most patients [6].
Some studies showed that there was a substantial improvement from 400% up to 1000% in elastin and collagen fibre volume 6 months after derma roller therapy. One year after the therapy, epidermal thickness increased by 40% [10].
This study was implemented in Vietnam to evaluate the effectiveness and safety of micro- needling therapy in atrophic acne scar treatment.
Methods
A prospective, single centred study with convenient sampling with a sample size of 31 was implemented in Vietnam National Hospital of Dermatology and Venereology from March 2013 to Dec 2013. Subject recruitment criteria were acne patients suffering atrophic acne scar of grade 2 to 4 of Goodman and Baron scaring grading system, having a good health condition, do not have any disease that affects wound healing such as diabetes, collagen diseases etc. Exclusion criteria included history of keloids or hypertrophic scars, skin infection (herpes simplex, wart, impetigo, tinea…), skin cancer or active skin disease other than mild acne, active systemic or local skin disease likely to alter wound healing, treatment within the last 6 months or pending treatment within the subsequent 6 months with injecting fillers or ablative or non-ablative laser resurfacing, medication with isotretinoin or other oral retinoids within the past 6 months, current treatment with anticoagulants or antithrombotics, or do not agree to participate in research. Patient participation was voluntary, and the subjects could stop their attendance at any time. Inform consent form was obtained before the subject entered the study.
The materials of the study included microneedle derma roller (MTS Roller, 192 needles in 8 rows, 0.25 mm diameter and 1.5 mm long needles), local anaesthetic (Emla 5%, lidocaine 10%), topical antibiotic cream (Fucidin cream), and facial skin analysis machine.
Each subject was treated by derma roller every week in 3 months. The patients’ faces were prepared by cleaning, applying local anaesthetic for 40 minutes, then washed off by saline and sterilised by 70% isopropyl alcohol. Derma roller then was rolled on the scar area in 4 directions (horizontal, vertical, both oblique directions) and repeated 4-10 times on a treatment area. Pinpoint bleeding at the base of the scar was expected end-point, and then saline pads were kept over the treated area, following by application of topical antibiotic cream. After treatment, all patients were recommended to avoid sun exposure, makeup and to swim.
The result was evaluated by facial skin analysis machine and clinically by dermatologists using Goodman and Baron’s global acne scar grading [11] and Lipper-Perez score [12] at baseline, at final treatment and 1, 2 months after the final treatment. According to Goodman and Baron grading, an improvement by ≥ 2 grades was labelled excellent, by 1 grade – labelled good, no change – labelled poor) [13]. Besides, acne scar severity score was assessed by Lipper and Perez score: M = number of rolling scars x 1 + number of boxcar x 2 + some icepick x 3 [12].
The study was approved by the Hospital reviewing Board. The subjects were explained about the study, and their participation was completely voluntary. The informed consent form was signed before the subject enters the study.
Data were analysed by SPSS 16.0 software. Descriptive analysis was used for continuous variables, the frequency for categorical variables. Chi-square test/Fisher’s exact test and paired T-test was used to compare the differences between variables. The results were statistically significant if p ≤ 0.05.
Results
General information
A total of 31 patients (10 males, aged 26.80 ± 7.87; 21 females, aged 23.95 ± 5.59) were recruited. 15 of them (accounted for 48.4%) had a history of nodular-cystic acne, and 14 patients (45.2%) had a history of acne vulgaris before attending the study. Percentage of nodular-cystic acne in male and female patients was not significantly different (60.0% vs. 47.4%, Fisher’s exact test, p = 0.4). The mean time of suffering acne of the subjects was 3.62 ± 2.09 years and of suffering scar was 4.00 ± 3.23 years. 19.4% of them had not got acne treatment; only 3.2% took isotretinoin orally. The most common location of acne was cheek (n = 31, 100%), followed by forehead (n = 19, 61.3%), chin (n = 7, 22.6%) and lastly nose (n = 1, 3.2%). Rolling scar and icepick were very common, accounted for 90.3% (n = 28), box scar was seen in 65.5% of the patients (n = 20).
Clinical assessment
Goodman and Baron’s global acne scar grading system has 4 grades ranging from 1 to 4 in which grade 1 meaning least severe and grade 4 meaning most severe. At baseline, scar grade of 2, 3 and 4 accounted for 6.5%, 58.1% and 35.5% consecutively, meaning most of the scars were severe. The therapy improved the scar grading significantly, with the decrease of the mean of Goodman and Baron’s grade from 3.29 ± 0.59 at baseline, to 2.23 ± 0.56 at final treatment, to 1.93 ± 0.58 one month after the completion of therapy and to 1.77 ± 0.57 two months after the completion of therapy (with the p-value of paired T-test comparing the mean of baseline to the final treatment, the final treatment to one month after final treatment, the one month to two months after the final treatment was 0.0001, 0.002 and 0.023 consecutively). About 43.3% (n = 13) of the patients had good improvement and 53.3 % (n = 16) had excellent improvement. History of having nodular-cystic or vulgaris acne did not affect the effectiveness of the therapy (percentage of good improvement in nodular-cystic acne group was 66.7%, and in acne, vulgaris group was 46.2%, Chi-square test, p = 0.239).
Lipper and Perez’s scoring system also was used to evaluate the efficacy of the modality. The score dropped dramatically from 36.48 ± 12.07 at baseline to 23.16 ± 15.01 at final treatment, to 17.83 ± 7.00 one month after the final treatment and to 16.37 ± 7.29 at two months after the final treatment, as shown in Figure 1. The differences were statically significant.
Figure 1.
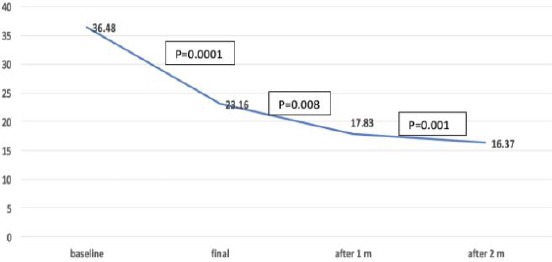
Changing in Lipper and Perez score
Assessment by magic machine
The measurement by facial skin analysis showed that the skin roughness got improved significantly from baseline to final treatment (p = 0.0001), from final treatment to 1 month after that (p = 0.045) but not significantly from 1 month after the final treatment to 2 months after final treatment (p = 0.063), as shown in Table 1.
Table 1.
Changes in roughness and hyperpigmented spot by Magic camera
| Time of assessment | p-value | Roughness score (m ± SD) | p-value | Spot score (m ± SD) |
|---|---|---|---|---|
| Baseline | 37.66 ± 11.27 | 33.58 ± 20.09 | ||
| P = 0.0001 | P = 0.009 | |||
| Final treatment | 31.46 ± 7.29 | 26.76 ±15.44 | ||
| P = 0.045 | P = 0.024 | |||
| 1m after final treatment | 29.04 ±6.98 | 22.41 ±13.58 | ||
| P = 0.063 | P = 0.006 | |||
| 2m after final treatment | 27.26 ±6.67 | 16.71 ± 9.56 |
Hyperpigmented spot score also got decreased by the time significantly from baseline to final treatment, 1 month after that and 2 months after that (p = 0.009, p = 0.024 and p = 0.006 consecutively).
Figure 2.
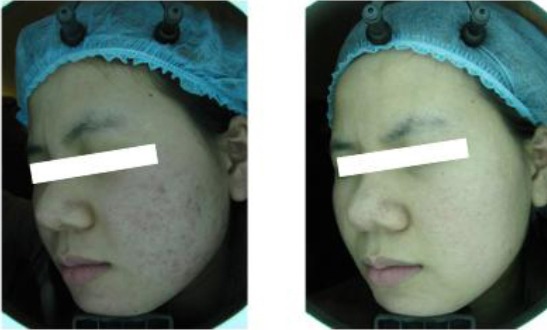
a 20-year-old female showing improvement following three sessions of micro needling
Two months after the final treatment, most of the patient was satisfied with the result (n = 25, accounting for 83.3%). Regarding the side effects, all patients felt burning and had erythema after the therapy, 16.7% (n = 5) had to scale. However, the burning feeling disappeared right after the rolling process, erythema reduced after 1-2 days; scaly skin only lasted for 2-3 days. No severe side effect including itchy, blister, pustules, and hyperpigmentation was noted.
Discussion
Skin needling is a modality for skin rejuvenation, tightening and scar remodelling. This method enhances dermal extracellular matrix proteins [3], [13] without ablation of the epidermis, so limiting side effects and minimising downtime. Many studies have been implemented to evaluate the efficacy of skin needling method. Authors found that skin needling was simple, effective and safe technique to treat atrophic scars. It did not damage the skin, had a short recovery time and created more dermal papillae [14].
Our results showed that this modality was safe and good effects in atrophic acne scars, fairly similar to the results of other studies such as of Imran Majid [13], Fabbrocini et al., [15]. In Imran Majid’s study, 37 patients suffering atrophic acne scars of Goodman grade 2 to 4 were treated by derma roller up to 4 months. The assessment was carried out at baseline, last treatment, one month and two months after the last treatment. The results showed that 26 patient (accounted for 72.2%) reached good response, 6 patients (accounted for 16.7%) reached moderate response — about 80% of the subjects satisfied with the therapy. No significant side effect and short recovery time were noted [13]. The higher good response compared with our results may be due to the differences in duration and type of the acne scars.
Another study implemented by Fabbocini and his team in Italy [15] recruited 32 patients (aged 17-45, 20 females, 12 males) having rolling scars. The good and classification were used to evaluate the results. The patients were treated by derma roller for 4 months. Similarly to our study, after 4 months, the scars got marked improvement (p < 0.05) and the skin became thicker and smoother. No side effect and no post-inflammatory hyperpigmentation was reported [15].
Acne atrophic scars are very common and affect patients’ quality of life. Therefore, there are many therapies used to deal with this problem such as chemical peeling, dermabrasion, laser, TCA.
CO2 laser and Erbium YAG laser could lead to 50% to 80% scar improvement but had a risk of infection, long-lasting erythema, hyper/hypopigmentation. According to Elizabeth LT et al., (2002), after YAG laser treatment, all of 25 acne atrophic scar patients got erythema lasting 3 weeks, 11 patients (accounted for 44%) developed post inflammatory hyperpigmentation. Other side effects such as dermatitis and infections were noted [8].
A study of Woraphong Manuskiatti et al., [17] treating 13 patients showed that after 3 treatments (7- week interval) by fractional CO2 laser, 50% of the patient had good response, erythema lasted 7-10 days, some other complications included light hyperpigmentation seen in 92%, acne in 31%, herpes in 7.7%, allergic contact dermatitis in 15% of the patients [17].
Tran Thi Thai Ha et al. implemented a study in which 100% TCA was applied to atrophic acne scars of 30 patients [18]. Only 14.3% of them reached good response. Side effects including itchiness, erythema, scaling, lasted longer, about 2 weeks [18].
In conclusion, micro needling therapy is effective and safe for atrophic acne scar treatment. It does not damage the skin, causes a little side effect, short recovery time. Also, it does not require expensive equipment leading to less expenditure in comparison to laser or dermabrasion modality. It could be done in all skin type patients as post-inflammatory hyperpigmentation is rarely seen after the therapy.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Camirand A, Doucet J. Needle dermabrasion. Aesthetic plastic surgery. 1997;21(1):48–51. doi: 10.1007/s002669900081. https://doi.org/10.1007/s002669900081 PMid:9204168. [DOI] [PubMed] [Google Scholar]
- 2.Fife D. Practical evaluation and management of atrophic acne scars:tips for the general dermatologist. The Journal of clinical and aesthetic dermatology. 2011;4(8):50–57. PMid:21909457 PMCid:PMC3168245. [PMC free article] [PubMed] [Google Scholar]
- 3.O'Daniel TG. Multimodal management of atrophic acne scarring in the aging face. Aesthetic plastic surgery. 2011;35(6):1143–50. doi: 10.1007/s00266-011-9715-y. https://doi.org/10.1007/s00266-011-9715-y PMid:21491169 PMCid:PMC3236289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zduńska K, Kołodziejczak A, Rotsztejn H. Is skin microneedling a good alternative method of various skin defects removal. Dermatologic therapy. 2018;31(6):e12714. doi: 10.1111/dth.12714. https://doi.org/10.1111/dth.12714 PMid:30246914. [DOI] [PubMed] [Google Scholar]
- 5.Cunliffe W. Acne Vulgaris, Treatment of skin disease, Mosby. 2002:6–13. [Google Scholar]
- 6.Fernandes D. Minimally invasive percutaneous collagen induction. Oral and Maxillofacial Surgery Clinics. 2005;17(1):51–63. doi: 10.1016/j.coms.2004.09.004. https://doi.org/10.1016/j.coms.2004.09.004 PMid:18088764. [DOI] [PubMed] [Google Scholar]
- 7.Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatologic Surgery. 1995;21(6):543–9. doi: 10.1111/j.1524-4725.1995.tb00259.x. https://doi.org/10.1111/j.1524-4725.1995.tb00259.x. [DOI] [PubMed] [Google Scholar]
- 8.Tanzi EL, Alster TS. Treatment of atrophic facial acne scars with a dual-mode Er:YAG laser. Dermatologic surgery. 2002;28(7):551–5. doi: 10.1046/j.1524-4725.2002.01319.x. PMid:12135504. [DOI] [PubMed] [Google Scholar]
- 9.Fernandes D. Paper presented at the IPRAS Conference. San Francisco, CA: 1999. Skin needling as an alternative to laser. [Google Scholar]
- 10.Jacob CI, Dover JS, Kaminer MS. Acne scarring:a classification system and review of treatment options. Journal of the American Academy of Dermatology. 2001;45(1):109–17. doi: 10.1067/mjd.2001.113451. https://doi.org/10.1067/mjd.2001.113451 PMid:11423843. [DOI] [PubMed] [Google Scholar]
- 11.Goodman GJ, Baron JA. Postacne scarring:a qualitative global scarring grading system. Dermatologic Surgery. 2006;32(12):1458–66. doi: 10.1111/j.1524-4725.2006.32354.x. https://doi.org/10.1097/00042728-200612000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Lipper GM, Perez M. Nonablative acne scar reduction after a series of treatments with a short-pulsed 1,064-nm neodymium:YAG laser. Dermatologic surgery. 2006;32(8):998–1006. doi: 10.1111/j.1524-4725.2006.32222.x. PMid:16918561. [DOI] [PubMed] [Google Scholar]
- 13.Majid I. Microneedling therapy in atrophic facial scars:an objective assessment. Journal of cutaneous and aesthetic surgery. 2009;2(1):26. doi: 10.4103/0974-2077.53096. https://doi.org/10.4103/0974-2077.53096 PMid:20300368 PMCid:PMC2840919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verbaan FJ, Bal SM, Van den Berg DJ, Groenink WH, Verpoorten H, Lüttge R, Bouwstra JA. Assembled microneedle arrays enhance the transport of compounds varying over a large range of molecular weight across human dermatomed skin. Journal of Controlled Release. 2007;117(2):238–45. doi: 10.1016/j.jconrel.2006.11.009. https://doi.org/10.1016/j.jconrel.2006.11.009 PMid:17196697. [DOI] [PubMed] [Google Scholar]
- 15.Fabbrocini G, Fardella N, Monfrecola A, Proietti I, Innocenzi D. Acne scarring treatment using skin needling. Clinical and Experimental Dermatology:Experimental dermatology. 2009;34(8):874–9. doi: 10.1111/j.1365-2230.2009.03291.x. https://doi.org/10.1111/j.1365-2230.2009.03291.x PMid:19486041. [DOI] [PubMed] [Google Scholar]
- 16.Imthurn B. Pathogenesis and treatment of acne in children. Pediatr-Dermatol. 1997;14(1) doi: 10.1111/j.1525-1470.1997.tb00420.x. [DOI] [PubMed] [Google Scholar]
- 17.Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R. Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. Journal of the American Academy of Dermatology. 2010;63(2):274–83. doi: 10.1016/j.jaad.2009.08.051. https://doi.org/10.1016/j.jaad.2009.08.051 PMid:20633798. [DOI] [PubMed] [Google Scholar]
- 18.Ha TT. Efficacy of 100% Trichloroacetic Acid in acne atrophic scar. Medical University internal circulation. Master Thesis. 2009 [Google Scholar]


