Abstract
AIM:
Compare itraconazole alone, fluconazole combined with ketoconazole and ketoconazole in the treatment of patients with pityriasis versicolor.
MATERIAL AND METHODS:
A group of 240 pityriasis versicolor patients (confirmed with KOH and culture) were classified into 3 groups: Fluconazole 300 mg a week and 2% ketoconazole foam twice a week for 2 weeks (Category I), Itraconazole 200 mg daily for one week (category II); Ketoconazole 2% foam daily for 2 weeks (Category 3). Clinical (colour of macule, scale, pruritus) and mycological assessment were done after 4 weeks of therapy.
RESULTS:
After 4 weeks of treatment, clinical cure was observed in 62.4% (Category I), 36.3% (Category II) and 37.5% (Category III).
CONCLUSION:
It was reported in our study that the most effective regimen for PV patients is fluconazole 300 mg per week combined with ketoconazole 2% twice a week for 2 weeks.
Keywords: Pityriasis versicolor, Malassezia, Yeast
Introduction
Pityriasis versicolor is a common, chronic, superficial fungal infection caused by Malassezia spp [1]. It is characterised by hyperpigmented, hypopigmented macules and patches on the face, upper trunk, back, chest paralleling the density of sebaceous gland. Several topical and systemic antifungal agents are effective against pityriasis versicolor. However, recurrence is common. Therefore, approaching an effective, safe and affordable treatment regimen should be taken in consideration.
Our study aimed to assess and compare the efficacy and the safety of oral fluconazole combined with foam ketoconazole, oral itraconazole and foam ketoconazole alone.
Material and Methods
A group of 240 patients with pityriasis versicolor over 16 years old attending our out-patient dermatology clinic from January 2016 to December 2016 were included in the study. Patients with other superficial and systemic fungal infections, history of treatment with oral antifungal drugs during the previous month or with topical anti-fungal drugs within 1-week, pregnant females, and patients with the serious concurrent disease were excluded from the study
Eligible patients were randomised to receive one of the following categories of treatment regimen: Category I: Fluconazole 300 mg a week for 2 weeks and foam ketoconazole 2% biweekly in 2 weeks; Category II: Itraconazole 200 mg daily for 1 week, Category III: foam ketoconazole 2% daily in 2 weeks.
Clinical signs and symptoms such as pruritus, hypo or hyperpigmentation, and desquamation were classified (0 = none, 1 = mild, 2 = moderate, 3 = severe), lesion measurement (0: none, 1: < 10% BSA, 2:10 - 30% BSA, 3: > 30% BSA).
A group of 240 pityriasis versicolor patients were randomly classified into 3 groups: Fluconazole 300 mg a week and 2% ketoconazole foam twice a week for 2 weeks (Group I), Itraconazole 200 mg daily for 1 week (Group II); Ketoconazole 2% foam daily for 2 weeks (Group 3).
Results
During the study period, 240 patients were enrolled in our study: the itraconazole group, the fluconazole associated with ketoconazole shampoo group and the ketoconazole foam group. There were no statistically significant differences regarding age, sex, disease severity for patients in the two groups as shown in Table 1 (p > 0,05).
Table 1.
Characteristics of patients
| Group 1 | Group 2 | Group 3 | P | |
|---|---|---|---|---|
| Gender (Male/Female) | 50/30 | 54/26 | 52/28 | > 0,05 |
| Age | ||||
| 16-19 | 6/80 | 6/80 | 5/80 | > 0,05 |
| 20-29 | 39/50 | 40/80 | 43/80 | |
| 30-39 | 23/80 | 22/80 | 23/80 | |
| 40-49 | 8/80 | 9/80 | 6/80 | |
| > 50 | 4/80 | 3/80 | 3/80 | |
| Disease severity | ||||
| Mild | 19/80 | 20/80 | 15/80 | > 0,05 |
| Moderate | 49/80 | 49/80 | 59/80 | |
| Severe | 12/80 | 11/80 | 6/80 | |
The mycological examination is considered the most important factor in determining the efficacy of treatment. The negative result showed that the patient had recovered from the microorganism despite still having skin lesions. It was reported in our study as shown in Table 2 that negative mycological examination was highest in group 1 (81.3%); lowest in group 3 (60%).
Table 2.
Clinical and mycological assessment after 4 weeks of therapy
| Group 1 (n = 80) | Group 2 (n = 80) | Group 3 (n = 80) | |||||
|---|---|---|---|---|---|---|---|
| Baseline | 28 days | Baseline | 28 days | baseline | 28 days | ||
| Scale | Present | 80 | 17 | 79 | 25 | 80 | 26 |
| Absent | 0 | 63 | 1 | 55 | 0 | 54 | |
| Pruritus | Present | 67 | 26 | 64 | 37 | 63 | 28 |
| Absent | 13 | 54 | 16 | 43 | 17 | 52 | |
| Disease activity score | 4.7 ± 1.5 | 2.2 ± 1.2 | 4.5 ± 1.6 | 2.5 ± 1.4 | 4.6 ± 1.4 | 2.5 ± 1.2 | |
| Decrease in DAS | 2.5 ± 1.1 | 2.0 ± 1.0 | 2.1 ± 0.8 | ||||
| Mycological culture | Positive | 80 | 15 | 80 | 27 | 80 | 32 |
| Negative | 0 | 65 | 0 | 53 | 0 | 48 | |
It was also reported in Table 2 that 53/80 patients (66.3%) treated with itraconazole 200 mg daily for 7 days have negative KOH examination.
As reported in our research, the highest cure rate was observed in group 1 (81.2%), followed by Group 2 (66.3%) and Group 3 (60.0%). There were statistical significant difference meaning between Group 1 and Group 2 (p < 0,01), Group 1 and 3 (p < 0,05).
In our study, a new regimen-oral fluconazole 300 mg a week combined with ketoconazole 2% foam 3 times a week for 2 weeks was first applied. The overall cure rate after 4 weeks was 81.2%. It was lower than Badri T’s study (90%), relapse rate was not assessed in both study. Compared with fluconazole treatment alone in Montero-Gei’s research, ninety patients with tineaversicolor were randomly assigned to treatment with either a single 450 mg dose of fluconazole, two 300mg doses of fluconazole given for one week, or itraconazole 200 mg daily for 7 days. At the end of treatment, the cure rate for itraconazole (20%) was significantly higher (P = 0.024) than that for fluconazole 450 mg (0%).
Figure 1.
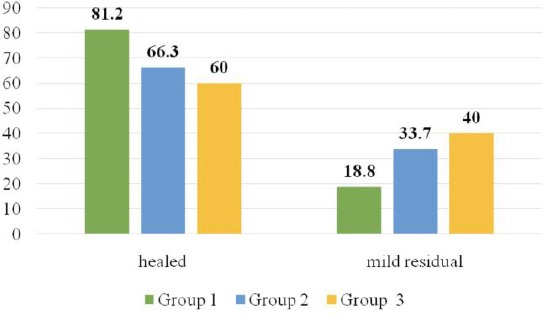
Treatment efficacy after 4 weeks
Discussion
It was 91% in Talel Badri’s research on patients treated with oral fluconazole and 2% for ketoconazole [2]. 100% of patients had negative KOH result after 5weeks of ketoconazole cream 2% in Fonzo’s study [3]. It was demonstrated by Mehme Karakas’s study that 77% and 77.5% of patients treated with fluconazole 300 mg for 2 weeks have negative mycological result after 4 weeks, respectively [4], [5]. There were several studies in which fluconazole was applied in various durations and dosages in the treatment of tinea versicolor (450 mg/single dose, 400 mg/single dose, 300 mg with a 1-week interval, 300 mg a week for 2 weeks, 150mg a week for 4 weeks). In these studies, the mycological cure varied between 44%-100% [3]. Accordingly, the clinician may opt to use regimen 300 mg a week for 2 weeks for treating tinea versicolor.
There were several studies in which ketoconazole shampoo and foam was applied in treatment tinea versicolor. According to Di Fonzo [3], the cure rate was observed in 100% of patients after 2 weeks of ketoconazole shampoo 1% and 2%. It was 81%, 55% and 72% in Rigoponlos (2007), Cantrell (2014) and Shi (2014)’s study [6], [7], [8].
In our research, we have assessed one of the most common regimen antifungal drugs in Vietnam – itraconazole 200mg daily for 7 days. Kose et al. reported equivalent efficacy between a daily 200 mg dose of itraconazole for 7 days and a single 400 mg dose [9]. Kokturk et al., reported greater efficacy of 400 mg of itraconazole a day over 3 days and 200 mg a day over 5 days than 400 mg in 1 day [5]. It was demonstrated in our study that the cure rate was seen in 66.3% of patients when they were treated by itraconazole 200mg daily for 7 days. When cure plus improvement was considered, response rates among the three treatment groups were comparable (97, 100, and 97% for fluconazole 450 mg, fluconazole 300 mg, and itraconazole, respectively) [10].
The unsimilar result between authors can be explained by the difference in criteria for efficacy assessment. The mycological cure rate was always higher than the clinical cure rate in all study groups. As a mycological cure is the only reliable criterion in assessing treatment efficacy, this implies that a proportion of patients rated as clinically improved were cured with residual colour changes (mostly hypopigmentation) [11], [12].
In conclusion, topical combined with systemic therapy is effective against tinea versicolor, especially extensive disease, frequent relapses, or history of failed topical treatment. In the current study, we found the highest mycological cure rate, 62.4%, with a single oral dose of fluconazole 300mg along with ketoconazole foam 2% twice a week, higher than with itraconazole 200 mg daily for one week (35.3%) and ketoconazole foam (37.5%).
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Prohic A, Jovovic-Sadikovic T, Krupalija-Fazlic M, Kuskunovic-Vlahovljak S. Malassezia species in healthy skin and in dermatological conditions. Int J Dermatol. 2016;55(5):494–504. doi: 10.1111/ijd.13116. https://doi.org/10.1111/ijd.13116 PMid:26710919. [DOI] [PubMed] [Google Scholar]
- 2.Badri T, Hammami H, Bzioueche N, Zouari B, Mokhtar I. Comparative clinical trial:fluconazole alone or associated with topical ketoconazole in the treatment of pityriasisversicolor. Tunis Med. 2016;94(2):107–111. PMid:27532525. [PubMed] [Google Scholar]
- 3.Di Fonzo EM, Martini P, Mazzatenta C, Lotti L, Alvino S. Comparative efficacy and tolerability of Ketomousse (ketoconazole foam 1%) and ketoconazole cream 2% in the treatment of pityriasisversicolor:results of a prospective, multicentre, randomised study. Mycoses. 2008;51(6):532–535. doi: 10.1111/j.1439-0507.2008.01508.x. https://doi.org/10.1111/j.1439-0507.2008.01508.x PMid:18422916. [DOI] [PubMed] [Google Scholar]
- 4.Karakas M, Durdu M, Memisoglu HR. Oral fluconazole in the treatment of tineaversicolor. J Dermatol. 2005;32(1):19–21. doi: 10.1111/j.1346-8138.2005.tb00707.x. https://doi.org/10.1111/j.1346-8138.2005.tb00707.x PMid:15841655. [DOI] [PubMed] [Google Scholar]
- 5.Kokturk A, Kaya TI, Ikizoglu G, Bugdayci R, Koca A. Efficacy of three short-term regimens of itraconazole in the treatment of pityriasisversicolor. J Dermatolog Treat. 2002;13(4):185–187. doi: 10.1080/09546630212345676. https://doi.org/10.1080/09546630212345676 PMid:19753739. [DOI] [PubMed] [Google Scholar]
- 6.Rigopoulos D, Gregoriou S, Kontochristopoulos G, Ifantides A, Katsambas A. Flutrimazole shampoo 1% versus ketoconazole shampoo 2% in the treatment of pityriasisversicolor. A randomised double-blind comparative trial. Mycoses. 2007;50(3):193–195. doi: 10.1111/j.1439-0507.2006.01352.x. https://doi.org/10.1111/j.1439-0507.2006.01352.x PMid:17472615. [DOI] [PubMed] [Google Scholar]
- 7.Cantrell WC, Elewksi BE. Can pityriasisversicolor be treated with 2% ketoconazole foam? J Drugs Dermatol. 2014;13(7):855–859. PMid:25007370. [PubMed] [Google Scholar]
- 8.Shi TW, Zhang JA, Tang YB, Yu HX, Li ZG, Yu JB. A randomized controlled trial of combination treatment with ketoconazole 2% cream and adapalene 0.1% gel in pityriasisversicolor. J Dermatolog Treat. 2015;26(2):143–146. doi: 10.3109/09546634.2014.921661. https://doi.org/10.3109/09546634.2014.921661 PMid:24802530. [DOI] [PubMed] [Google Scholar]
- 9.Mohanty J, Sethi J, Sharma M. Efficacy of itraconazole in the treatment of tineaversicolor. Indian J Dermatol Venereol Leprol. 2001;67(5):240–241. PMid:17664760. [PubMed] [Google Scholar]
- 10.Kose O, BulentTastan H, RizaGur A, Kurumlu Z. Comparison of a single 400 mg dose versus a 7-day 200 mg daily dose of itraconazole in the treatment of tineaversicolor. J Dermatolog Treat. 2002;13(2):77–79. doi: 10.1080/095466302317584430. https://doi.org/10.1080/095466302317584430 PMid:12060506. [DOI] [PubMed] [Google Scholar]
- 11.Mohanty J, Sethi J, Sharma M. Efficacy of itraconazole in the treatment of tineaversicolor. Indian J Dermatol Venereol Leprol. 2001;67(5):240–241. PMid:17664760. [PubMed] [Google Scholar]
- 12.Chokoeva AA, Wollina U, Lotti T, Maximov GK, Lozev I, Tchernev G. Psoriasiform Dermatophytosis in a Bulgarian Child. Open Access Maced J Med Sci. 2018;6(1):118–119. doi: 10.3889/oamjms.2018.009. https://doi.org/10.3889/oamjms.2018.009 PMid:29484004 PMCid:PMC5816278. [DOI] [PMC free article] [PubMed] [Google Scholar]


