Abstract
AIM:
This study aimed to evaluate the effect of the fractional Radiofrequency microneedle treatment for facial atrophic acne scars.
METHODS:
A group of 52 patients were recruited for the study. Goodman & Baron’s acne scar grading system was used for assessment at their first visit and the end of 3 months after the last treatment session.
RESULTS:
The results displayed that 73.1% of patients have the improvement of the Goodman scar level after four times of treatment. The Goodman and Baron scar point mean was reduced from 16 ± 7.6 to 5.6 ± 5.0 (p < 0.01). Post-inflammatory hyperpigmentation was experienced in 5 patients (9.6%).
CONCLUSION:
The microneedle fractional Radiofrequency is an effective treatment method of facial atrophic acne scars, with minor side effects and a short downtime.
Keywords: facial atrophic acne scars, Radiofrequency, fractional RF microneedle
Introduction
Atrophic acne scars are dermal depressions commonly caused by the destruction of collagen after inflammatory acne [1].
Recently, fractional radiofrequency microneedle (FRM) technique has been shown to be clinically effective in managing acne scars and less post-inflammatory hyperpigmentation (PIH) [2], inducing collagen shrinkage, collagen neogenesis and stimulating remodelling [3].
This study aimed to evaluate the effect of the fractional Radiofrequency microneedle treatment for facial atrophic acne scars.
Material and Methods
The study was performed on 52 patients with acne scars and skin phototypes III–V. The average age is 26.7 ± 6.1 years (range 15-43 years old). Male and female ratios are roughly equal.
The observed scars were mainly rolling scars and boxcar, and the ice pick was relatively low (19.5%). Patients with post-acne scars were mostly severely scarred, Goodman 4 (71.2%); Goodman 3 (28.8%) [4], [5].
All subjects were treated with two consecutive passes of an FRM (INTRAcel TM, Jeisys Medical, Seoul, Korea) with minimal or no overlapping. The subjects were treated for a total of four sessions at 1 month intervals.
Results
At the 3-month follow-up visit, the colour of the scar was significantly improved with 92.5% of normal skin colour and 3.8% of acne related post-inflammatory erythema (PIE) as shown in Figure 1. This improvement was statistically significant compared with pretreatment (p < 0.05).
Figure 1.
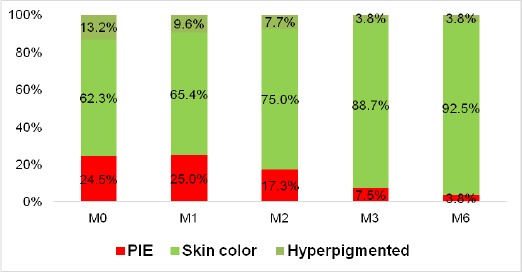
Improvement of the color of scars (PIE: Post-inflammatory erythema-M0: Baseline-M1: first month-M2: second month-M3: third month-M6: sixth month)
The improvement of scars according to Goodman and Baron qualitative scar grading began to be apparent only after 2 treatments. Grade 4 scars were decreased from 71.2% to 59.6%. The improvement was stronger after 3 treatments and 3 months after the end of treatment. Grade 4 showed a significant decrease from 71.2% to 38.5% and 25% (p < 0.01). There were 73.1% of patients who showed improvement by 1 grade. These were presented in Figure 2.
Figure 2.
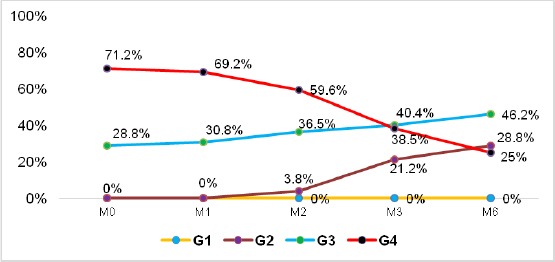
Improvement of Goodman’s qualitative acne scar grading system. (M0: Baseline- M1: first month- M2: second month- M3: third month- M6: sixth month- G1: Grade 1-G2: Grade 2- G3: Grade 3- G4: Grade 4)
The acne scar scores improvement was almost negligible after one treatment. However, after 4 treatments, mean scars decreased from 16 ± 7.6 (before treatment) to 5.6 ± 5.0 (t = 17.62; df = 51; p < 0.01), Figure 3.
Figure 3.
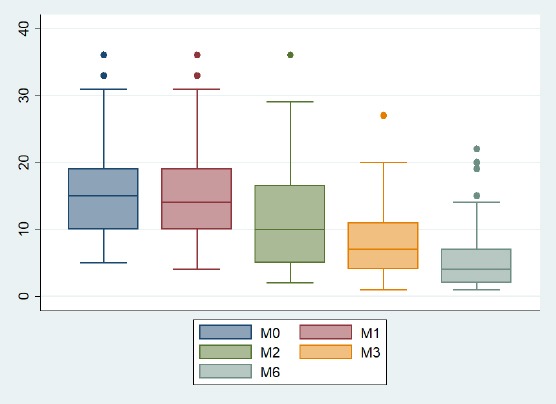
Improvement of Goodman and Baron’s quantitative acne scar grading system (M0: Baseline-M1: first month-M2: second month-M3: third month-M6: sixth month)
The treatment was generally well tolerated. Only five patients (9.6%) reported post-inflammatory hyperpigmentation and subsided spontaneously within 1 month without any recurrences after the remaining treatment sessions.
Discussion
Scars can occur early in acne patients, about the severity of acne, duration of untreated acne and duration of acne.
At the 3-month follow-up visits, the colour of the scar was significantly improved with 92% of normal skin colour and 3.8% of acne-related post-inflammatory erythema (PIE). This improvement was statistically significant compared with pretreatment (p-value = 0.001 < 0.05). This was consistent with another study in the literature [6]. PIE is very common following inflammatory acne and is often cosmetically unacceptable to patients. FMR treatment could improve erythema by reducing inflammation and abnormal vessel proliferation, by inhibiting NF-κB expression and angiogenesis VEGF directly or indirectly [6].
The improvement was stronger after 3 treatments and 3 months after the end of treatment, showing a significantly decrease in the severity levels of the scars. Grade 4 scars were reduced from 71.2% to 38.5% and 25% (p = 0.000 <0.01). 73.1% of patients showed improvement by 1 grade.
The median Goodman and Baron’s global scores for acne severity was significantly lower than baseline at the 3-month follow-up visit, from 16 ± 7.6 to 5.6 ± 5.0 (t = 17.62; df = 51; p-value = 0.00 < 0.01).
In conclusion, FRM treatment can be considered as an effective modality of treatment for acne scars in patients with an added advantage of minimal downtime and effective improvement. This method can be considered as a good solution for the treatment of atrophic acne scar in Asians with low post inflammatory hyperpigmentation.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Bencini PL, Tourlaki A, Galimberti M, Longo C, Pellacani G, De Giorgi V, Guerriero G. Nonablative fractional photothermolysis for acne scars:clinical and in vivo microscopic documentation of treatment efficacy. Dermatologic therapy. 2012;25(5):463–7. doi: 10.1111/j.1529-8019.2012.01478.x. https://doi.org/10.1111/j.1529-8019.2012.01478.x PMid:23046026. [DOI] [PubMed] [Google Scholar]
- 2.Abdel Hay R, Shalaby K, Zaher H, Hafez V, Chi CC, Dimitri S, Nabhan AF, Layton AM. Interventions for acne scars. The Cochrane Library. 2016:CD011946. doi: 10.1002/14651858.CD011946.pub2. https://doi.org/10.1002/14651858.CD011946.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forbat E, Al-Niaimi F. Fractional radiofrequency treatment in acne scars:Systematic review of current evidence. J Cosmet Laser Ther. 2016;18(8):442–447. doi: 10.1080/14764172.2016.1225964. https://doi.org/10.1080/14764172.2016.1225964 PMid:27592504. [DOI] [PubMed] [Google Scholar]
- 4.Goodman GJ, Baron JA. Postacne scarring:a quantitative global scarring grading system. J Cosmet Dermatol. 2016;5(1):48–52. doi: 10.1111/j.1473-2165.2006.00222.x. https://doi.org/10.1111/j.1473-2165.2006.00222.x PMid:17173571. [DOI] [PubMed] [Google Scholar]
- 5.Goodman GJ, Baron JA. Postacne scarring:A qualitative global scarring grading system. Dermatologic Surgery. 2006;32:1458–1466. doi: 10.1111/j.1524-4725.2006.32354.x. https://doi.org/10.1097/00042728-200612000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Min S, Park SY, Yoon JY, Kwon HH, Suh DH. Fractional Microneedling Radiofrequency Treatment for Acne-related Post-inflammatory Erythema. Acta Derm Venereol. 2016;96(1):87–91. doi: 10.2340/00015555-2164. https://doi.org/10.2340/00015555-2164 PMid:26059315. [DOI] [PubMed] [Google Scholar]


