Introduction
A cancer diagnosis is associated with high levels of distress, particularly anxiety, depression, fear of recurrence, sleep disturbance, and fatigue in both patients and caregivers (Artherholt & Fann, 2012; Bower, 2014; Fann, Ell, & Sharpe, 2012). Although an estimated 35–55% of cancer patients report such psychological distress (Carlson et al., 2004; Carlson, Groff, Maciejewski, & Bultz, 2010; Sellick & Edwardson, 2007; Zabora, BrintzenhofeSzoc, Curbow, Hooker, & Piantadosi, 2001), clinicians often have few resources to help improve the quality of life (QoL) of cancer patients and their families. Evidence-based tools to address the psychosocial needs of cancer patients are urgently needed. Informal caregivers, including spouses, family members, and friends, often provide substantial support and care for patients. Cancer patients’ informal caregivers often exhibit high levels of stress and depression and poor physical health, yet receive little attention and care (Braun, Mikulincer, Rydall, Walsh, & Rodin, 2007; Pinquart & Sörensen, 2003; Ringdal et al., 2004). Because informal caregiving is essential to the overall well-being of patients, maintaining the health and wellness of caregivers is important to optimize health outcomes of both parties (Glajchen, 2004; Northouse, Katapodi, Song, Zhang, & Mood, 2010). To help cope with distress, cancer patients and their families are increasingly turning to complementary and integrative medicine including mindfulness practices (Huebner et al., 2014; Shumay, Maskarinec, Gotay, Heiby, & Kakai, 2002; Yates et al., 2005).
Mindfulness is defined as moment-to-moment awareness with an attitude of non-judgment, acceptance and openness (Kabat-Zinn, 1990). Mindfulness practice, offered widely in North America and Europe as Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn, 1990) or Mindfulness-Based Cognitive Therapy (MBCT) (Segal, Williams, & Teasdale, 2002), has shown efficacy in reducing distress and improving QoL among cancer patients (Haller et al., 2017; Musial, Bussing, Heusser, Choi, & Ostermann, 2011; Piet, Wurtzen, & Zachariae, 2012; Rush & Sharma, 2016; Zhang, Xu, Wang, & Wang, 2016). For instance, a recent meta-analysis of ten randomized clinical trials of mindfulness-based therapy involving 1,709 breast cancer patients reported that interventions reduced anxiety and depression and improved sleep quality, fatigue, and QoL (Haller et al., 2017). However, despite the promise of the benefits of mindfulness interventions, attending traditional mindfulness classes can be challenging for patients undergoing treatment because these classes often include over 30 hours of in-person instruction plus an additional 45 minutes of daily home practice. Cancer patients suffering from treatment side effects and their informal caregivers who are busy and distressed may find it extremely difficult to attend in-person classes (Lee, Colditz, Berkman, & Kawachi, 2003; Shrank et al., 2011).
The use of technology to deliver mindfulness interventions to cancer patients and caregivers is a promising but underresearched area of inquiry, and experts in the area of mindfulness and cancer recently indicated a need for non-face-to-face mindfulness interventions (Zernicke et al., 2016). We previously conducted a pilot study using audio CDs for cancer patients undergoing chemotherapy (n=23) and demonstrated the feasibility and acceptability of a self-paced, non-face-to-face mindfulness intervention and its preliminary efficacy in reducing anxiety (Altschuler, Rosenbaum, Gordon, Canales, & Avins, 2012). A recent study conducted in Canada also demonstrated the feasibility of offering an online cancer recovery mindfulness program for cancer survivors and preliminary efficacy to improve mood, stress, spirituality, post-traumatic growth, and mindfulness (Zernicke et al., 2016). Given the availability of rapidly-evolving technology and high user prevalence (Statista, 2015), interventions using mobile applications or the internet may provide greater practicality for distressed patients and caregivers. If feasible, use of technology may increase accessibility to mindfulness programs for distressed cancer patients and their overburdened caregivers in a cost-effective manner. We thus conducted a pilot feasibility study of an app-/online-based mindfulness program within an integrated health care delivery system.
Method
Participants
We included cancer patients actively undergoing chemotherapy and their primary informal caregivers. The inclusion criteria for both patients and caregivers included age 18+ years; owning a smartphone, tablet or computer with internet access; and understanding English. Patients were eligible if they had a diagnosis of cancer and had chemotherapy scheduled for at least 2 months after the time of enrollment. Caregivers were eligible and invited to participate if the enrolled patient considered the person their primary informal support person (i.e., family or friend). We excluded persons who meditated or currently participated in another type of stress reduction program, were severely hearing impaired, or had severe mental illness.
Procedure
This single-arm pilot study was conducted between November 2015 and August 2016 at three oncology clinics within Kaiser Permanente Northern California (KPNC), an integrated health care delivery system that provides comprehensive health care to a large, diverse community-based population of 3.9 million individuals. Written informed consent was obtained from participants, and study protocols and procedures were approved by the Kaiser Permanente Northern California Institutional Review Board.
Recruitment
Patients were recruited via several strategies, including presentations about the study at chemotherapy orientation classes; clinic referrals from oncology social workers and nurses; brochures at each clinic; and mailed invitation letters. Eligible patients were identified using the KPNC electronic health record and pharmacy database. Caregivers were recruited by patient-participant referral. Patients could participate with or without caregiver participation, but caregivers could only participate if associated with an enrolled patient. Participants who completed the study received a $40 gift card and an additional year’s subscription to the mindfulness program used for this intervention study.
Intervention
We used a commercially available mindfulness program, Headspace™, a self-paced program that provides guided mindfulness meditation instructions via a website or mobile application (iOS and Android). A recent review identified Headspace as the best commercial mindfulness mobile application (Mani, Kavanagh, Hides, & Stoyanov, 2015).
Research staff gave individual participants a brief introduction to Headspace and then assisted them with the logistics of using the program (e.g., creating a login, downloading the application, etc.). For the 8-week intervention, participants were instructed first to complete the 30-day Foundation Course, which teaches users the basics of mindfulness meditation, followed by optional 10- to 30-day courses that are more condition-specific, such as “Anxiety,” “Stress,” “Acceptance,” or “Sleep.” All sessions last 10–20 minutes. In addition to the daily, progressive audio instruction, there are short (1–2 minute) lecture videos every several days designed to increase the understanding of mindfulness and to encourage its integration into daily life.
Measures
Recruitment
We aimed to achieve recruitment rates that would match what would be needed for a fully powered clinical trial. Power calculations determined that a recruitment rate >15% would yield the required number of participants for a fully powered trial. In KPNC, there are over 4,000 patients started annually on chemotherapy for cancer. Thus, a recruitment rate of 15% would yield 600 subjects for a large randomized study, which would provide sufficient power (i.e., minimum detectable difference of approximately 0.2 standard deviation unit for the outcomes of interest, which is considered “small” effect size.)(Cohen, 1988)(Cohen, 1988) For this pilot, recruitment rates were calculated as the number of individuals who signed the consent divided by the number of potentially eligible participants contacted using each of the two methods described above – in-person at oncology clinics and via recruitment letters.
Retention
The retention rate was measured as the proportion of enrolled participants who completed both first and final surveys. Feasibility was defined as >60% of the consented participants completing the study.
Adherence
The Headspace program automatically collects adherence data, including date, time, and name of each session to which participants listened, identified by a study ID. Headspace transferred these adherence data to the researchers bi-weekly during the course of the study. Using this data, we calculated the proportion of days during the 8-week intervention period that each participant used the program.
Participant-reported measures
We collected outcome data using DatStat online survey software at the time of consent and post-intervention. A research assistant administered the baseline survey at the patient’s home at enrollment. Participants were emailed a link to the post-intervention survey eight weeks later, and they independently completed the survey online. All data collection instruments were previously validated.
Distress
The National Comprehensive Cancer Network Distress Thermometer was used to assess current distress level (Carlson, Waller, & Mitchell, 2012; Network, 2014). Respondents were asked to rate their level of distress during the past week by choosing a number, with 0 indicating no distress and 10 extreme distress.
Anxiety and depression
We used the 14-item Hospital Anxiety and Depression Scale (HADS) to assess anxiety and depression (Bjelland, Dahl, Haug, & Neckelmann, 2002). This scale is frequently used to assess psychosocial outcomes in cancer patients and its reliability and validity have been confirmed (Zhang et al., 2015). Each subscale is scored from 0 to 21, with higher scores indicating greater anxiety and depression; 0–7 is generally considered within normal range.
Sleep quality
The 19-item Pittsburg Sleep Quality Index (PSQI) assesses sleep quality by asking a series of questions about sleep quality during the past month (Akman, Yavuzsen, Sevgen, Ellidokuz, & Yilmaz, 2015). A global score (ranging 0 to 21) is calculated based on the seven domain scores, with a higher score indicating poorer sleep quality.
Quality of life
The 10-item PROMIS Global Health Scale asks respondents to rate their health (overall, physical, and mental), QoL, satisfaction with social activities and roles, ability to perform selected functional activities, frequency of emotional problems, and severity of fatigue on a 5-point Likert scale (Broderick, DeWitt, Rothrock, Crane, & Forrest, 2013). Higher scores indicate higher QoL.
Fatigue
The 9-item Brief Fatigue Inventory assesses the severity and impact of cancer-related fatigue and the extent to which fatigue interfered with various aspects of life in the past 24 hours (e.g., mood, walking ability) on a 10-point Likert scale (Mendoza et al., 1999).
Post-intervention interview
We conducted phone interviews after participants completed the 8-week intervention. Using a four-point Likert scale, we asked patients to rate how useful they found the intervention, and then, using open-ended questions, we asked what they liked most and least about the program and in what ways the mindfulness practice benefited them, if any. Participants’ answers to these questions were written down as close to verbatim as possible by the interviewer due to insufficient funding for interview transcription.
Data analyses
Independent-sample t-tests and chi-square tests were used to compare differences between participants who completed the study (defined as completing the post-intervention survey) and those who dropped out. We then performed paired t-tests among those who completed both pre- and post-intervention surveys to examine the difference between scores. As a secondary analysis, we repeated the paired t-tests for patients stratified by paired or unpaired status to examine whether patients participating in the study with or without a primary caregiver had an impact on outcome measures.
Post-intervention open-ended questions were analyzed according to the thematic analysis approach (Braun & Clarke, 2006). Two experienced qualitative researchers (AA and EK) coded the responses independently. Codes were initially based on the questions asked, and then we expanded the coding during the review of participants’ answers to include themes that participants consistently expressed. Next, the two researchers discussed the codes to ensure consistency of coding. Any discrepancies were resolved by consensus, and the final dataset and coding were reviewed by a third researcher (AK). Together, the three researchers grouped codes into themes to describe participants’ reports of their intervention experiences. We used simple descriptive statistics to assess the closed-ended post-intervention question.
Results
Feasibility outcomes
Recruitment rate
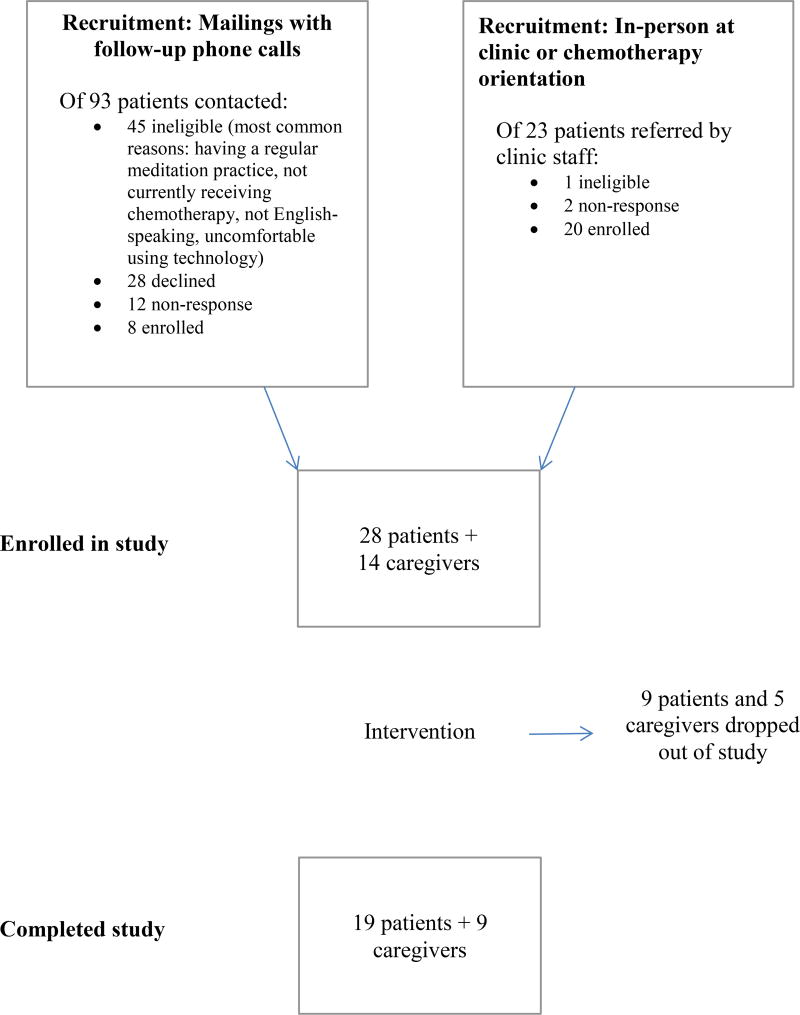
Figure 1 shows the overall flow of participants through the study. Of the 23 patients who were recruited by clinic-based means, one was ineligible and two did not respond to attempts to contact them; the remaining 20 enrolled yielding an 87% response rate. Of 93 patients contacted by letter, 45 were ineligible, 28 declined, and 12 did not respond/were unreachable. Eight patients enrolled, yielding a 17% response rate (assuming those who were unreachable were all eligible to participate). The most common reasons for ineligibility included already having a meditation practice, not actively receiving chemotherapy at the time of recruitment; not speaking English, and being uncomfortable using technology (Figure 1). The most common reasons given for declining to join the study were being busy and lack of interest.
Fig. 1.
Overall flow of participants through the study
Retention rate
A total of 28 patients and 14 caregivers enrolled in the study; 19 patients (68%) and 9 caregivers (64%) completed the study. We attempted to obtain reasons for drop-out among those who did not complete the study. Reasons provided for discontinuation included: too sick from the side effects of chemotherapy; never established a meditation practice; illness progressed; caregiving responsibility increased; and holiday schedules interfered.
Adherence
Among those who completed the study, 20 (71%) practiced meditation >50% of the days during the 8-week study period, and 12 of those 20 individuals practiced >70% of the days. In addition, 64% of participants meditated at least once during the month after the intervention period ended.
Participant characteristics
Demographic characteristics
Table 1 describes the baseline demographic characteristics of all individuals who completed the study. Patients who completed the study tended to have slightly higher education and income than patients who did not complete the study (p=.01 and p=.04, respectively). Similarly, among caregivers, completers tended to have higher levels of education compared with non-completers (p=.02).
Table 1.
Baseline demographic and clinical characteristics of participants
| Patients | Caregivers | ||
|---|---|---|---|
| n=19 | n=9 | ||
| Age, mean (range) | 64.7 (48–78) | 58.8 (38–73) | |
| Female gender, n (%) | 13 (68.4) | 7 (77.8) | |
| Marital status, n (%) | |||
| Married | 14 (73.7) | 8 (88.9) | |
| Living as married/domestic partner | 0 (0) | 0 (0) | |
| Widowed | 2 (10.5) | 0 (0) | |
| Divorced | 1 (5.3) | 0 (0) | |
| Never married | 2 (10.5) | 1 (11.1) | |
| Ethnicity, n (%) | |||
| White | 15 (79.0) | 7 (77.8) | |
| African-American | 3 (15.8) | 1 (11.1) | |
| Asian | 1 (5.3) | 1 (11.1) | |
| Native Hawaiian or Pacific Islander | 0 (0) | 0 (0) | |
| Education, n (%) | |||
| High school graduate or GED | 0 (0)* | 0 (0)* | |
| Some college | 4 (21.1) | 0 (0) | |
| College graduate | 1 (5.3) | 6 (66.7) | |
| Postgraduate study | 14 (73.7) | 3 (33.3) | |
| Income, n (%) | |||
| $25,000 to $49,999 | 0 (0)* | 1 (11.1) | |
| $50,000 to $74,999 | 5 (27.8) | 2 (22.2) | |
| $75,000 to $99,999 | 5 (27.8) | 2 (22.2) | |
| $100,000 or more | 8 (44.4) | 4 (44.4) | |
| Primary delivery of the mindfulness program, n (%) | |||
| iOS (iPad or iPhone) | 11 (57.9) | 4 (44.4) | |
| Android | 2 (10.5) | 0 (0) | |
| Computer with internet | 5 (26.3) | 1 (11.1) | |
| >1 type of device | 1 (5.3) | 4 (44.4) | |
| Cancer Type, n (%) | |||
| Breast | 6 (33.3) | ||
| Gastrointestinal | 3 (16.7) | ||
| Hematologic | 4 (22.2) | ||
| Lung/bronchus | 2 (11.1) | ||
| Uterine | 1 (5.6) | ||
| Prostate | 1 (5.6) | ||
| Ill-defined | 1 (5.6) | ||
| Cancer Stage, n (%), curative/palliative | |||
| I | 2 (11.8) | ||
| II | 7 (41.2) | ||
| III | 1 (5.9) | ||
| IV | 4 (23.5) | ||
| N/A | 3 (17.7) | ||
| Time since diagnosis (in months), mean (range) | 18.1 | ||
| Spouse/Partner | 6 (66.7) | ||
| Child | 2 (22.2) | ||
| Friend | 1 (11.1) | ||
| How often take care of patient, n (%) | |||
| Every day | 7 (77.8) | ||
| 3–5 times a week | 1 (11.1) | ||
| 1–2 times a week | 1 (11.1) | ||
p ≤ 0.05
p ≤ 0.01
Baseline clinical and health characteristics
Table 1 also presents clinical characteristics of the enrolled patients. The most common cancer site among patients who completed the study was breast (31.6%), and 40% of all patients were diagnosed with either stage III or IV cancers. Those who completed the study had a longer period since diagnosis (18.1 months) than those who did not complete the study (7.3 months).
Participant-reported outcomes
The baseline, post-intervention and change in scores for the outcome variables, stratified by patient/caregiver status, are shown in Table 2. Baseline distress and anxiety levels were higher among caregivers (mean distress 6.4; mean anxiety 11.4) than patients (mean distress 5.5; mean anxiety 7.5). Caregivers who completed the study had higher anxiety (p=0.0001) and fatigue levels (p=.03) at baseline (mean anxiety score 11.4; mean fatigue score 1.8) than did non-completers (mean anxiety score 2.8; mean fatigue score 0.8).
Table 2.
Baseline and post-intervention scores of patients and caregivers
| Patients | Caregivers | ||||||
|---|---|---|---|---|---|---|---|
| Baseline (n=19) |
Post- interven tion (n=19) |
Change | Baseline (n=9) |
Post- interventi on (n=9) |
Change | ||
| Mean (SD) |
Mean (SD) |
Mean (SD) |
Mean (SD) |
Mean (SD) |
Mean (SD) |
||
| Distress Thermometer score | 5.5 (2.4) | 2.8 (1.9) | −2.7 (2.1)** | 6.4 (1.7) | 4.6 (2.1) | −1.9 (2.0)* | |
| Hospital Anxiety and Depression Scale (HADS) | |||||||
| Anxiety | 7.5 (3.8) | 4.7 (3.3) | −2.8 (4.7)* | 11.4 (3.4) | 9.3 (3.2) | −2.1 (3.3) | |
| Depression | 6.9 (3.5) | 5.1 (3.3) | −1.8 (3.9) | 5.7 (3.9) | 3.9 (3.2) | −1.8 (2.1)* | |
| PROMIS Global Health Scale | |||||||
| Physical Health | 12.5 (2.5) | 13.5 (2.7) | 1.1 (2.2) | 15.0 (1.9) | 16.5 (2.4) | 1.4 (1.1)** | |
| Mental Health | 11.6 (2.9) | 13.3 (3.1) | 1.7 (1.6)** | 12.3 (2.4) | 13.1 (1.9) | 0.9 (2.0) −0.5 | |
| Brief Fatigue Inventory score | 1.9 (0.8) | 1.6 (0.8) | −0.3 (0.8) | 1.8 (0.7) | 1.3 (0.7) | (0.5)* | |
| Pittsburgh Sleep Quality Index score | 8.0 (2.8) | 6.2 (3.5) | −1.8 (3.5)* | 6.1 (2.2) | 6.1 (2.4) | −0.3 (2.1) | |
p ≤ 0.05
p ≤ 0.01
Patients experienced a statistically significant reduction in distress levels (−2.7, p<0.01) and in anxiety (−2.8, p<0.05). They showed an increase in the QoL mental health domain scores (+1.7, p<0.01) and a decrease in PSQI scores (indicating improved sleep quality; −1.8, p<0.05) between baseline and post-intervention assessments. No significant changes were observed for depression, the QoL physical health domain score, or fatigue.
The caregivers experienced a statistically significant reduction in distress levels (−1.9, p<0.05) and in depression (−1.8, p<0.05). They demonstrated an increase in the QoL physical domain scores (+1.4, p<0.01) and a decrease in fatigue (−0.5, p<0.05). No significant changes were observed for anxiety, the QoL mental health domain score, or sleep quality.
Post-intervention interviews
Seventeen of the 19 patients and all nine caregivers completed the post-intervention phone interview. Eighty-two percent of patients reported that Headspace was extremely or very useful (35% and 47% respectively). Caregivers gave similar ratings; 77% found the program extremely (35%) or very (44%) useful. In coding the three open-ended questions (what they liked most and least, and what were the most important benefits of this mindfulness practice, if any), we developed the following coding domains: 1) components and content of the program (e.g., how people were taught and learned to meditate); 2) design elements and technical issues (e.g., how the app functioned and how content was delivered); 3) challenges and barriers to meditation; and 4) benefits of meditating.
“Benefits of meditating” was the only domain that had a number of differentiated answers that prompted creation of the following subdomains: 1) having a tool to use when stressed; 2) enjoyment of meditation; 3) allowing oneself to stay in the moment and not become anxious/engage in catastrophic thinking; 4) practicing acceptance and avoiding judgment; 5) becoming calm; 6) increased feelings of gratitude; and 7) benefits associated with physical functioning, such as better sleep quality and less pain.
We found that patients’ and caregivers’ responses to the open-ended questions were very similar. There were only three subdomains in which patients’ reports suggested they may have derived more benefits than the caregivers. While nearly a third of the patients reported enjoying meditation, no caregivers reported their experiences in this manner. In parallel, while approximately 10% of the patients described feeling increased gratitude as a result of their practice, none of the caregivers provided similar responses. Finally, more than half the patients reported benefits regarding sleep or pain as a result of meditating, while only one caregiver reported such a result.
Comments about specific design features of the meditation program were mostly positive. Participants generally found it easy to use, although a few mentioned having some technical issues with the app or wanting additional features. Participants said they appreciated the app’s flexibility, specifically that they could do the meditations whenever and wherever they wanted, and that the meditations were short.
Several patients felt it might be better to start a meditation program later in their treatment course, feeling that receiving the diagnosis left them overwhelmed for a time and that it was difficult to keep up the practice while going through chemotherapy.
Discussion
This study evaluated the feasibility and acceptability of delivering a self-paced app-/online-based mindfulness intervention to cancer patients actively undergoing chemotherapy and their informal caregivers. We found that patients and caregivers appreciated the intervention and that many participants learned mindfulness skills using this technology. Our methods provide a practical strategy for conducting a larger, fully powered clinical trial and our learnings in this pilot have provided important insights that will increase the likelihood of a successful intervention study in this and similar trials in the future. The feasibility results offer some insights regarding strategies to improve recruitment and adherence for future studies. Although not designed as an efficacy trial, the preliminary results suggested improvement in anxiety, depression, QoL, sleep, and fatigue.
Along with physical and medical challenges, cancer patients, their families, and close friends face emotional upheavals that can make life incredibly stressful. Due to the new Commission on Cancer requirement to screen for psychosocial distress among all cancer patients, it is likely that more patients will be identified as ‘distressed’ (Cherkin et al., 2016). Providers will need efficient strategies to offer support to those in need. Underscoring the importance of providing patients psychosocial and emotional support, research indicates that the levels of stress and depression that patients experience not only affect cancer symptom severity and psychological functioning (Roscoe et al., 2002; Walker, Zona, & Fisher, 2006), but survival and prognosis (Giese-Davis et al., 2011),. This study extends existing knowledge regarding the potential of using mindfulness interventions for cancer patients in reducing distress and improving QoL in several ways.
First, we used mobile technology to deliver the mindfulness intervention. Attending an in-person program, despite its reported efficacy in improving QoL and reducing distress among cancer patients, is extremely challenging for patients undergoing treatment or those with advanced disease. They face challenges of cancer-related illness, fatigue, and geographic distance, among other logistical barriers (Zernicke et al., 2016). The few mindfulness studies that included patients with advanced cancers reported that recruitment was challenging due to patients’ difficulty in committing to an 8-week, in-person schedule, and that there is a need to tailor interventions to make them less intensive for cancer patients (Eyles et al., 2015). In the present study, participants greatly appreciated the ease of using the mobile application/online program, especially during blocks of time when they might otherwise be unoccupied and anxious, such as time in waiting rooms and while receiving chemotherapy infusions.
Second, our study is one of the few mindfulness intervention studies that also included patients' informal caregivers (Birnie, Garland, & Carlson, 2010; Schellekens et al., 2014; Schellekens et al., 2017; van den Hurk, Schellekens, Molema, Speckens, & van der Drift, 2015). As the number of individuals living with cancer increases, from 14 million in 2012 to a projected 18 million by 2022, the number of informal caregivers will grow in parallel (de Moor et al., 2013). Overburdened caregivers seldom seek mental health care to deal with their depression or emotional distress (Given, Given, & Kozachik, 2001), despite the fact that caregivers of patients with advanced cancer sometimes report more depression than the patients themselves (Braun et al., 2007). In our study, the baseline distress level was higher among the caregivers than the patients, corroborating these findings. Higher stress and more severe depression often lead to poorer health among caregivers and decreased ability to effectively provide care (Pinquart & Sörensen, 2003; Schulz & Sherwood, 2008). Despite their tremendous burden, caregivers’ emotional, spiritual, and physical needs are often not supported (Braun et al., 2007; Ringdal et al., 2004). Given the significant reciprocal emotional relationship between caregivers and patients, it is imperative to offer caregivers psychosocial and educational support to improve their own QoL and physical and mental health (Glajchen, 2012). Our preliminary data suggest that patients who participated jointly with their informal caregivers demonstrated greater improvement in QoL and reductions in anxiety and depression. These results may have been observed simply by chance, but the adherence data show that patients who participated with a caregiver had a slightly greater adherence rate than those who did not (completed sessions on 65% vs. 54% of study days, respectively). Although our study was not powered to detect such differences with statistical significance, our results may suggest that involvement of informal caregivers may improve adherence, thereby increasing the efficacy of the intervention.
Third, our sample population included a diverse group of patients actively undergoing chemotherapy. We successfully recruited men, non-whites, and patients with different types of cancer; 32% of patients were male, 20% were non-white, and over 60% of patients had cancers other than breast. Previous mindfulness studies for cancer patients overwhelmingly consisted of white, early stage breast cancer patients who had completed all of their initial treatment (Piet et al., 2012; Ulrichsen et al., 2016). Few mindfulness studies have focused on patients who are actively undergoing chemotherapy or patients with more advanced stages (Chambers et al., 2017; Lengacher et al., 2012). Ongoing treatment and concerns about the disease course itself cause substantial distress for both patients and their loved ones, and these populations have been comparatively understudied (Artherholt & Fann, 2012; Bower, 2014; Fann et al., 2012; Hilton et al., 2017). Forty percent of the patients we enrolled had stage III or IV disease, demonstrating that it is possible to conduct a technology-based mindfulness intervention among a diverse population with a variety of cancer types and stages.
Lastly, we have learned several important lessons from this feasibility study. First, enrollment was substantially higher when recruitment was initiated by clinic-based means compared to recruitment letters. Our group’s future studies will take this into consideration and further engage clinical staff to maximize enrollment. A brief introductory conversation with a clinician about the benefits of stress-reduction and/or an introduction to the program might increase patient engagement with future research. Second, as mentioned above, patients who participated with the caregivers had greater adherence. We also observed stronger reductions in depression and improvement in QoL in this group. Although we cannot determine the causal association because of the single-arm nature of the study, future studies will continue to involve caregivers, who are in need of spiritual and emotional health support. Lastly, although we were able to recruit some non-white participants, we observed that the completion rate was lower among this group. During the next stage, it will be important to investigate how to increase the enrollment, adherence, and completion rates among these understudied populations. We will consider the feasibility of offering the intervention in languages other than English to improve minority population participation.
Limitations
The present study has several limitations. First, since it is a single-arm feasibility study, the lack of a control group and small sample size make it impossible to draw conclusions regarding the potential efficacy of the intervention on participant-reported outcomes. The observed improvements in depression, anxiety, QoL, sleep, and fatigue may simply represent natural improvements after cancer treatment begins and/or regression to the mean (Carlson, Waller, Groff, Giese-Davis, & Bultz, 2013). However, our post-interview survey results indicate that participants appreciated the resources and reported that mindfulness meditation helped them cultivate calmness, and acceptance, providing sufficient justification to further investigate the efficacy of technology-based interventions through larger randomized clinical trials. Ultimately, we demonstrated that both patients and caregivers were able to follow the protocol and accept the intervention.
Second, because we required the use of technology as a part of the intervention, the study results may not be generalizable to the general population due to the “digital divide.” However, mobile devices are increasingly used by all segments of the population (Statista, 2015), and the majority of the patients and caregivers who we attempted to recruit owned mobile devices or computers with an internet connection. The main reasons reported for declining to participate were lack of time or interest, not lack of access to technology.
A third limitation was failing to include a measure of mindfulness as an outcome measure because of our effort to keep the study questionnaires as short as possible. In future studies, we will consider including mindfulness measures to assess its role as a mediator. Finally, we did not record or transcribe the post-intervention interviews due to limited resources. However, the questions and responses were fairly brief and simple, which allowed the interviewer to take notes close to verbatim. Therefore, it is unlikely that this limitation affected data quality.
This pilot study provided encouraging evidence that a mobile application or an online-based mindfulness intervention is acceptable to cancer patients undergoing chemotherapy and their informal caregivers. Future larger-scale randomized studies involving diverse populations are needed to establish the efficacy of technology-based mindfulness interventions. Pragmatic trials of this type of intervention within large health care systems will help provide evidence regarding the effectiveness of implementing a low-cost, technology-based stress reduction program for cancer patients and their informal caregivers.
Acknowledgments
We thank participants of the POEM (Practice of Embracing Each Moment) study. This work was supported by the National Institutes of Health (grant KL2TR000143, K07CA166143) and Kaiser Permanente Planned Giving Fund.
Footnotes
Author Disclosure Statement
Conflict of Interest: All authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Kaiser Permanente Northern California Institutional Review Board provided IRB approval for the study. This article does not contain any studies with animals performed by any of the authors.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Author Contributions
AK: Obtained funding, designed and executed the study, assisted with the data analyses, and wrote the paper. AA: collaborated on the design of the study, the data analysis, and writing and editing of the final manuscript. EK: collaborated on the data analysis and writing and editing of the final manuscript. SH: collaborated on the study protocol, recruitment, participant contacts, and the data collection. CL: Organized and conducted the statistical analyses. TK: collaborated on the design and execution of the study. YL: collaborated on the design and execution of the study. AA: collaborated on the design of the study, the data analysis, and editing of the final manuscript.
References
- Akman T, Yavuzsen T, Sevgen Z, Ellidokuz H, Yilmaz AU. Evaluation of sleep disorders in cancer patients based on Pittsburgh Sleep Quality Index. European Journal of Cancer Care. 2015;24(4):553–559. doi: 10.1111/ecc.12296. [DOI] [PubMed] [Google Scholar]
- Altschuler A, Rosenbaum E, Gordon P, Canales S, Avins AL. Audio recordings of mindfulness-based stress reduction training to improve cancer patients' mood and quality of life--a pilot feasibility study. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2012;20(6):1291–1297. doi: 10.1007/s00520-011-1216-7. [DOI] [PubMed] [Google Scholar]
- Artherholt SB, Fann JR. Psychosocial care in cancer. Current Psychiatry Reports. 2012;14(1):23–29. doi: 10.1007/s11920-011-0246-7. [DOI] [PubMed] [Google Scholar]
- Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR) Psycho-oncology. 2010;19(9):1004–1009. doi: 10.1002/pon.1651. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Bower JE. Cancer-related fatigue--mechanisms, risk factors, and treatments. Nature Reviews Clinical Oncology. 2014;11(10):597–609. doi: 10.1038/nrclinonc.2014.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: spouse caregivers. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2007;25(30):4829–4834. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- Broderick J, DeWitt E, Rothrock N, Crane P, Forrest C. Advances in Patient-Reported Outcomes: The NIH PROMIS® Measures. eGEMs. 2013;1(1) doi: 10.13063/2327-9214.1015. Article12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson LE, Angen M, Cullum J, Goodey E, Koopmans J, Lamont L, Bultz BD. High levels of untreated distress and fatigue in cancer patients. British Journal of Cancer. 2004;90(12):2297–2304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson LE, Groff SL, Maciejewski O, Bultz BD. Screening for distress in lung and breast cancer outpatients: a randomized controlled trial. Journal of Clinical Oncology. 2010;28(33):4884–4891. doi: 10.1200/JCO.2009.27.3698. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Waller A, Groff SL, Giese-Davis J, Bultz BD. What goes up does not always come down: patterns of distress, physical and psychosocial morbidity in people with cancer over a one year period. Psycho-oncology. 2013;22(1):168–176. doi: 10.1002/pon.2068. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Waller A, Mitchell AJ. Screening for distress and unmet needs in patients with cancer: review and recommendations. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2012;30(11):1160–1177. doi: 10.1200/JCO.2011.39.5509. [DOI] [PubMed] [Google Scholar]
- Chambers SK, Occhipinti S, Foley E, Clutton S, Legg M, Berry M, Smith DP. Mindfulness-Based Cognitive Therapy in Advanced Prostate Cancer: A Randomized Controlled Trial. Journal of Clinical Oncology. 2017;35(3):291–297. doi: 10.1200/jco.2016.68.8788. [DOI] [PubMed] [Google Scholar]
- Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, Turner JA. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA. 2016;315(12):1240–1249. doi: 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, Kent EE, Rowland JH. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiology, Biomarkers & Prevention: a Publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2013;22(4):561–570. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyles C, Leydon GM, Hoffman CJ, Copson ER, Prescott P, Chorozoglou M, Lewith G. Mindfulness for the self-management of fatigue, anxiety, and depression in women with metastatic breast cancer: a mixed methods feasibility study. Integrative Cancer Therapies. 2015;14(1):42–56. doi: 10.1177/1534735414546567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fann JR, Ell K, Sharpe M. Integrating psychosocial care into cancer services. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2012;30(11):1178–1186. doi: 10.1200/JCO.2011.39.7398. [DOI] [PubMed] [Google Scholar]
- Giese-Davis J, Collie K, Rancourt KM, Neri E, Kraemer HC, Spiegel D. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: a secondary analysis. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2011;29(4):413–420. doi: 10.1200/JCO.2010.28.4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given BA, Given CW, Kozachik S. Family support in advanced cancer. CA: A Cancer Journal for Clinicians. 2001;51(4):213–231. doi: 10.3322/canjclin.51.4.213. [DOI] [PubMed] [Google Scholar]
- Glajchen M. The emerging role and needs of family caregivers in cancer care. Journal of Supportive Oncology. 2004;2(2):145–155. [PubMed] [Google Scholar]
- Glajchen M. Physical well-being of oncology caregivers: an important quality-of-life domain. Seminars in Oncology Nursing. 2012;28(4):226–235. doi: 10.1016/j.soncn.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller H, Winkler MM, Klose P, Dobos G, Kummel S, Cramer H. Mindfulness-based interventions for women with breast cancer: an updated systematic review and meta-analysis. Acta Oncologica. 2017;56(12):1665–1676. doi: 10.1080/0284186x.2017.1342862. [DOI] [PubMed] [Google Scholar]
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Maglione MA. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Annals of Behavioral Medicine. 2017;51(2):199–213. doi: 10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner J, Prott FJ, Micke O, Muecke R, Senf B, Dennert G, Muenstedt K. Online survey of cancer patients on complementary and alternative medicine. Oncology Research and Treatment. 2014;37(6):304–308. doi: 10.1159/000362616. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delacorte; 1990. [Google Scholar]
- Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. American Journal of Preventive Medicine. 2003;24(2):113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Kip KE, Barta M, Post-White J, Jacobsen PB, Groer M, Shelton MM. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. Journal of Holistic Nursing: Official Journal of the American Holistic Nurses' Association. 2012;30(3):170–185. doi: 10.1177/0898010111435949. [DOI] [PubMed] [Google Scholar]
- Mani M, Kavanagh DJ, Hides L, Stoyanov SR. Review and Evaluation of Mindfulness-Based iPhone Apps. Journal of Medical Internet Research mHealth and uHealth. 2015;3(3):e82. doi: 10.2196/mhealth.4328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85(5):1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Musial F, Bussing A, Heusser P, Choi KE, Ostermann T. Mindfulness-based stress reduction for integrative cancer care: a summary of evidence. Forschende Komplementarmedizin. 2011;18(4):192–202. doi: 10.1159/000330714. [DOI] [PubMed] [Google Scholar]
- Network NCC. Distress Management Clinical Practice Guidelines in Oncology Version. 2014:1. [Google Scholar]
- Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians. 2010;60(5):317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piet J, Wurtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80(6):1007–1020. doi: 10.1037/a0028329. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychology and aging. 2003;18(2):250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Ringdal K, Jordhoy MS, Ahlner-Elmqvist M, Jannert M, Kaasa S. Health-related quality of life (HRQOL) in family members of cancer victims: results from a longitudinal intervention study in Norway and Sweden. Palliative Medicine. 2004;18(2):108–120. doi: 10.1191/0269216304pm878oa. [DOI] [PubMed] [Google Scholar]
- Roscoe JA, Morrow GR, Hickok JT, Bushunow P, Matteson S, Rakita D, Andrews PL. Temporal interrelationships among fatigue, circadian rhythm and depression in breast cancer patients undergoing chemotherapy treatment. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2002;10(4):329–336. doi: 10.1007/s00520-001-0317-0. [DOI] [PubMed] [Google Scholar]
- Rush SE, Sharma M. Mindfulness-Based Stress Reduction as a Stress Management Intervention for Cancer Care: A Systematic Review. Journal of Evidence-Based Complementary & Alternative Medicine. 2016 doi: 10.1177/2156587216661467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schellekens MP, van den Hurk DG, Prins JB, Molema J, Donders AR, Woertman WH, Speckens AE. Study protocol of a randomized controlled trial comparing Mindfulness-Based Stress Reduction with treatment as usual in reducing psychological distress in patients with lung cancer and their partners: the MILON study. BMC Cancer. 2014;14:3. doi: 10.1186/1471-2407-14-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schellekens MPJ, van den Hurk DGM, Prins JB, Donders ART, Molema J, Dekhuijzen R, Speckens AEM. Mindfulness-based stress reduction added to care as usual for lung cancer patients and/or their partners: A multicentre randomized controlled trial. Psycho-oncology. 2017;26(12):2118–2126. doi: 10.1002/pon.4430. [DOI] [PubMed] [Google Scholar]
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. American Journal of Nursing. 2008;108(9 Suppl):23–27. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: Guilford Press; 2002. [Google Scholar]
- Sellick SM, Edwardson AD. Screening new cancer patients for psychological distress using the hospital anxiety and depression scale. Psycho-oncology. 2007;16(6):534–542. doi: 10.1002/pon.1085. [DOI] [PubMed] [Google Scholar]
- Shrank WH, Liberman JN, Fischer MA, Kilabuk E, Girdish C, Cutrona S, Choudhry NK. Are caregivers adherent to their own medications? Journal of the American Pharmacists Association (2003) 2011;51(4):492–498. doi: 10.1331/JAPhA.2011.10006. [DOI] [PubMed] [Google Scholar]
- Shumay DM, Maskarinec G, Gotay CC, Heiby EM, Kakai H. Determinants of the degree of complementary and alternative medicine use among patients with cancer. Journal of Alternative and Complementary Medicine. 2002;8(5):661–671. doi: 10.1089/107555302320825183. [DOI] [PubMed] [Google Scholar]
- Statista. Number of smartphone users in the U.S. from 2010 to 2018 (in millions) 2015 Retrieved from http://www.statista.com/statistics/201182/forecast-of-smartphone-users-in-the-us/
- Ulrichsen KM, Kaufmann T, Dorum ES, Kolskar KK, Richard G, Alnaes D, Nordvik JE. Clinical Utility of Mindfulness Training in the Treatment of Fatigue After Stroke, Traumatic Brain Injury and Multiple Sclerosis: A Systematic Literature Review and Meta-analysis. Frontiers in Psychology. 2016;7:912. doi: 10.3389/fpsyg.2016.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Hurk DG, Schellekens MP, Molema J, Speckens AE, van der Drift MA. Mindfulness-Based Stress Reduction for lung cancer patients and their partners: Results of a mixed methods pilot study. Palliative Medicine. 2015 doi: 10.1177/0269216315572720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker MS, Zona DM, Fisher EB. Depressive symptoms after lung cancer surgery: Their relation to coping style and social support. Psycho-oncology. 2006;15(8):684–693. doi: 10.1002/pon.997. [DOI] [PubMed] [Google Scholar]
- Yates JS, Mustian KM, Morrow GR, Gillies LJ, Padmanaban D, Atkins JN, Colman LK. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2005;13(10):806–811. doi: 10.1007/s00520-004-0770-7. [DOI] [PubMed] [Google Scholar]
- Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-oncology. 2001;10(1):19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Zernicke KA, Campbell TS, Speca M, Ruff KM, Flowers S, Tamagawa R, Carlson LE. The eCALM Trial: eTherapy for Cancer Applying Mindfulness. Exploratory analyses of the associations between online mindfulness-based cancer recovery participation and changes in mood, stress symptoms, mindfulness, posttraumatic growth, and spirituality. Mindfulness. 2016;7(5):1071–1081. [Google Scholar]
- Zhang J, Xu R, Wang B, Wang J. Effects of mindfulness-based therapy for patients with breast cancer: A systematic review and meta-analysis. Complementary Therapies in Medicine. 2016;26:1–10. doi: 10.1016/j.ctim.2016.02.012. [DOI] [PubMed] [Google Scholar]
- Zhang MF, Wen YS, Liu WY, Peng LF, Wu XD, Liu QW. Effectiveness of Mindfulness-based Therapy for Reducing Anxiety and Depression in Patients With Cancer: A Meta-analysis. Medicine (Baltimore) 2015;94(45):e0897–0890. doi: 10.1097/md.0000000000000897. [DOI] [PMC free article] [PubMed] [Google Scholar]