Abstract
Background:
Recent trends in alcoholic liver disease, alcohol-related emergency room admissions, and alcohol use disorder prevalence as measured by general-population surveys have raised concerns about rising alcohol-related morbidity and mortality in the United States. In contrast, upward trends in per-capita alcohol consumption have been comparatively modest.
Methods:
To resolve these discordant observations, we sought to examine trends in the prevalence of alcohol use and binge drinking from six regularly or periodically administered national surveys using a meta-analytic approach. Annual or periodic prevalence estimates for past-12 month or past-30 day alcohol use and binge drinking were estimated for available time points between the years 2000 and 2016. Estimates were combined in a random-effects regression model in which prevalence was modeled as a log-linear function of time to obtain meta-analytic trend estimates for the full population and by sex, race, age, and educational attainment.
Results:
Meta-analysis-derived estimates of average annual percentage increase in the prevalence of alcohol use and binge drinking were 0.30% per year (95% CI: 0.22%, 0.38%) and 0.72% per year (95% CI: 0.46%, 0.98%), respectively. There was substantial between-survey heterogeneity among trend estimates, though there was notable consistency in the degree to which trends have impacted various demographic groups. For example, most surveys found that the changes in prevalence for alcohol use and binge drinking were large and positive for ages 50–64 and 65 and up, and smaller, negative, or non-significant for ages 18–29.
Conclusion:
Significant increases in the prevalence of alcohol use and of binge drinking over the past 10 to 15 years were observed, but not for all demographic groups. However, the increase in binge drinking among middle-aged and older adults is substantial and may be driving increasing rates of alcohol-related morbidity and mortality.
Introduction
A number of indicators point towards sharp increases in alcohol-related problems in the United States over the past 10 to 15 years. After a 25–30 year decline, the death rate from liver cirrhosis flattened in the mid-1990s and began to increase around 2006 (Yoon and Chen, 2016). Much of this increase appears to be driven by alcohol-related deaths. Between 2006 and 2016, the death rate from alcoholic liver disease increased over 40% from 4.1 per 100,000 in 2006 to 5.9 per 100,000 in 2016, while death rates from fibrosis and cirrhosis not specified as alcohol-related remained approximately unchanged between the years 2000 and 2016 (Centers for Disease Control and Prevention, 2017a). A sharp increase in alcohol-related emergency department visits over the years 2006–2014 has also been reported, with the majority of the increase occurring among people ages 45 and older (White et al., 2018). Finally, a recent analysis of data from two administrations of the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) concerning the prevalence of past 12-month DSM-IV alcohol use disorder (AUD) among US adults ages 18 and over suggested a nearly 50% increase over an 11-year period based on two surveys conducted in 2001/2 and 2012/13, respectively (Grant et al., 2017). This was accompanied by a nearly 30% increase in high-risk drinking, defined as engaging in one or more binge drinking episodes—four drinks in a day for women or five drinks in a day for men—on a weekly basis or more frequently during the prior 12 months.
Puzzlingly, these increases in alcohol-related morbidity and mortality have been accompanied by comparatively small increases in per-capita alcohol consumption as measured by excise tax receipts, which rose approximately 6% during the 2002–2013 time period (Haughwout and Slater, 2017). This does not rule out the possibility of large increases in AUD prevalence, but generally one would expect large increases in AUD prevalence to be accompanied by large increases in per capita consumption, because the vast majority of alcohol is consumed by the heaviest of drinkers (Kerr and Greenfield, 2007, Grucza and Plunk, 2016). Furthermore, data from other survey sources do not necessarily indicate large increases in the prevalence of AUD or binge drinking. The National Survey on Drug Use and Health (NSDUH)—the only other source of data for AUD trends in the US—suggests a roughly 5% decline in past-12 month AUD prevalence among adults during this same period (Cheng et al., 2018). Furthermore, NSDUH results indicated relatively flat rates of frequent binge episodic drinking among adults over 25 during this time period, and a decline for younger adults ages 18–25 (Substance Abuse and Mental Health Services Administration (SAMHSA), 2015). Estimates from the National Health Interview Survey (NHIS) suggested an increase in binge drinking prevalence during this time period (Centers for Disease Control and Prevention, 2004, Centers for Disease Control and Prevention, 2016), but not as large as the increase suggested by the NESARC. Thus, three high-quality series of epidemiological surveys of the US general population have yielded widely discrepant estimates of trends in binge drinking; estimated trends for AUD from the two available sources of data on that outcome diverged even more.
These discrepant survey results raise the question as to whether the trends in deaths from alcoholic liver disease and emergency department admissions are due to across-the-board increases in alcohol use and misuse, or whether changes in other risk factors, possibly coupled with demographic-specific increases in binge drinking, might explain these trends. For example, the prevalence of alcoholic liver disease could be impacted by population-level changes in obesity, viral hepatitis, demographic shifts that could include changes in the prevalence of genetic risk factors, shifts in beverage type and consumption patterns, or any combination of these factors (Ikeda et al., 1993, Wetterling et al., 1999, Hatton et al., 2009, Askgaard et al., 2015, Zaldivar Fujigaki et al., 2015). Similarly, the fact that the increases in emergency department admissions noted by White and colleagues (White et al., 2018) was largely concentrated among middle-aged people suggests that the increase might be driven by a combination of alcohol use and risk factors associated with age rather than acute alcohol consumption per se. Consistent with these observations, rates of alcohol-related traffic deaths and other alcohol-related injury deaths among young adults (ages 18 to 25) have declined in recent years (Hingson et al., 2017).
Resolving these discrepancies in alcohol trends among regularly or periodically administered general population survey series is essential for prioritizing prevention and treatment efforts. If rates of excessive alcohol use have increased as dramatically as suggested by NESARC trends, then primary universal prevention efforts should be prioritized and dramatic increases in the number of individuals seeking treatment can be anticipated. If, on the other hand, upward trends are more modest, then it might be more important to identify areas of progress and focus on subpopulations for which problems have increased. To this end, the objective of the work reported here was to conduct a meta-analysis of alcohol trend data across six publicly available and regularly administered nationally representative cross-sectional surveys. We focus on two measures: prevalence of any alcohol use and prevalence of engaging in one or more binge drinking episodes. These measures are available in six national surveys, allowing us to synthesize data from as many sources as possible. Further, binge drinking as measured by surveys is a strong predictor of both acute alcohol-related problems such as accidents and injuries, as well as long-term morbidity and mortality (National Institute of Alcohol and Alcoholism, 2000, Plunk et al., 2014). By combining data from these six series of national surveys from 2000 to 2016, we were able to assemble data from 61 individual survey administrations and over seven million participants.
Methods
Data Sources
In addition to the NESARC, NHIS, and NSDUH series, we utilized data from the Behavioral Risk Factor Surveillance System (BRFSS), the National Health and Nutrition Examination Survey (NHANES), and the National Alcohol Survey (NAS). The six sets of surveys we analyzed are all designed to be nationally representative of the non-institutionalized adult US population, but may vary with respect to the sampling universe and other methods. Links to sources with methodological details about each survey as well as available data are provided in Supplementary Table 1. All surveys utilize multi-stage complex sampling and all are administered at the national level, with the exception of the BRFSS, which is administered by individual states. All 50 states and the District of Columbia participated in the BRFSS during the period studied (Centers for Disease Control and Prevention, 2017b). Data for all surveys except the NESARC and NAS were downloaded from publicly available websites; for the BRFSS and NHANES, these data are curated by the Centers for Disease Control and Prevention. For the NHIS, we used the Integrated Health Interview System, which is part of the Integrated Public Use Microdata Series (IPUMS) maintained by the University of Minnesota Population Research Center (Minnesota Population Center, 2017). NSDUH data were obtained from the Inter-university Consortium for Political and Social Research housed at the University of Michigan (ICPSR, 2017). NAS data were analyzed at the Alcohol Research Group (ARG, Emeryville, CA), which oversees survey administration. Data from the 2001/2 NESARC survey were obtained when data were made publicly available via the NESARC website. NESARC-III data, collected in 2012/13, were obtained by a data use agreement from the National Institute on Alcohol Abuse and Alcoholism (to KJS). NESARC data were analyzed at the University of Missouri (Columbia, Missouri). For all surveys, we used available data from the year 2000 to the most recent available year. We accounted for word or other interview changes across years by dummy variable adjustment as described below. Selected key survey characteristics, including total sample sizes and the approximate range of response rates are summarized in Table 1.
Table 1:
Summary of surveys and measures
| Survey | Years | # of Waves | Total n (all years) | Survey Modea | Response Rate Range | Alcohol Use Time Frame | Binge Drinking Time Frame | Question Changes |
|---|---|---|---|---|---|---|---|---|
| NSDUH | 2002–2016 annual | 15 | 579,017 | In-Person ACASI | 72–77% | Past 12 Months | Past 30 days | None |
| NHIS | 2000–2016 annual | 17 | 520,180 | In-Person CAPI | ~80% | Past 12 Months | Past 12 Months | Binge drinking in 2014 |
| BRFSS | 2001–2016 annual | 16 | 6,201,64 | Telephone CATI | 42–55% | Past 30 Days | Past 30 Days | Binge drinking in 2006, Alcohol use in 2005, 2010. Major design change in 2011 |
| NESARC | 2001/2 and 2012/3 | 2 | 79,402 | In-Person CAPI | 81%, 60% | Past 12 Months | Past 12 Months | None |
| NHANES | 2001/2–2013/4 biannual | 7 | 33,645 | In-Person CAPI | 69–80% | Past 12 Months | Past 12 Months | Binge drinking in 2010 |
| NAS | 2000–2015 (every 5 years) | 4 | 28,781 | Telephone CATI | 44%−58% | Past 12 Months | Past 12 Months | None |
ACASI=Audio-computer self-interview. (For the NSDUH, consent and instructions are obtained in-person, but sensitive questions are administered via computer). CAPI=Computer-assisted personal interview. CATI=Computer-assisted telephone interview.
Alcohol Use Measures.
Our primary variables of interest were prevalence of alcohol use and prevalence of any binge drinking episode. All outcomes were assessed over either past 30-day or past 12-month time frames, as enumerated in Table 1. For brevity, we will use the terms “past month” and “past year” hereafter to describe the time frames. Alcohol use was assessed on a past year basis, except for the BRFSS, which assessed alcohol use over the past month. We operationalized alcohol use as one or more drinking days during the specified time frame. For all surveys except for the BRFSS, alcohol use was assessed by a question about whether the participant had consumed one or more drinks over the past year. The BRFSS utilized a similar question about past-month alcohol use during the 2005–2010 period, but for other years asked about the number of drinking days in the past month without a preceding conditional branching item. For all surveys except NESARC, binge drinking episodes were initially queried as five or more drinks during one day (NHIS, NHANES, NAS) or one occasion (BRFSS, NSDUH). The NESARC assessed the frequency of consuming five or more drinks for all participants, and four or more drinks for women specifically. For NESARC analyses, we opted to utilize the four-drink threshold for women and five-drink threshold for men for both waves. The NHIS, BRFSS, and NHANES switched to a four-drink threshold for women during the observation period (see Table 1). We examined the prevalence of any binge drinking episode over the past year (NHIS, NESARC, NHANES, NAS) or past month (NSDUH, BRFSS).
Demographics.
For all analyses, we estimated outcome prevalence for each survey administration for the full population and by demographic groups, and examined overall and demographic-specific trends for each outcome. Demographics included sex, race/ethnicity, age, and educational attainment. Recoded variable definitions followed those used by Grant et al (Grant et al., 2017) except in the case of age, for which we divided the samples into the following groups: 18–29, 30–49, 50–64, and 65 and older. We divided the samples this way because single-year age groups are not available in public-use NSDUH files, so the available NSDUH age recodes were applied to other surveys. Race/ethnicity was categorized as White, Black, Native American (including Alaskan Native), Asian/Pacific Islander—all non-Hispanic, and Hispanic of any race. NHANES did not include “Native American” as a response option, so prevalence estimates for this group are not included for NHANES. For the NAS, because of a survey design change eliminating oversampling of the least populated states, the estimates for Native American/Alaskan Natives for the most recent NAS are much lower than estimates for previous years. Therefore, this group is omitted from NAS trend analyses. Education was coded as less than high school, high school only, or more than high school (e.g., college degree, some college, or other postsecondary education). We did not examine all sociodemographic categories studied by Grant and colleagues (Grant et al., 2017) because of difficulties in harmonizing categories across surveys and across years within some surveys.
Statistical Methods.
All analyses were conducted in SAS version 9.3, Stata version 14, or SUDAAN version 11, and utilized procedures capable of incorporating survey weights and design variables into variance estimation algorithms. Full population prevalence estimates were calculated for each administration of each survey and analyzed graphically. To characterize time-trends for both the full population and for demographic subpopulations within each survey, we used log-binomial regression to model prevalence as a function of year. This yields an estimate of the relative risk (RR) associated with year, which is related to the average annual percentage change in prevalence, calculated as 100*(RR-1). For example, an RR of 1.02 indicates that the relative increase in prevalence is 2% per year. To summarize overall and demographic trend analyses graphically, we utilized forest plots of the estimated trend regression coefficients (β) from each survey. The regression coefficient is the natural logarithm of the RR; for small values of β (e.g., −.09 to 0.09), the RR can be approximated by 1+β with accuracy to the second decimal place and the average annual percentage change is 100*β. We sometimes refer to the estimated 10-year percentage change for a given outcome and/or group, which can be calculated as 100*(RR10-1). To account for changes in item content, such as the switch to a four-drink binge-drinking threshold for women, we incorporate dummy variables into the model to estimate separate intercepts for years assessed with separately worded items, while assuming a constant slope. Accordingly, the change from a five- to a four-drink threshold will appear as a step-function in the modeled trend line (see Figure 1). An additional dummy variable was incorporated to account for a major redesign in the BRFSS in 2011 (Centers for Disease Control and Prevention, 2012).
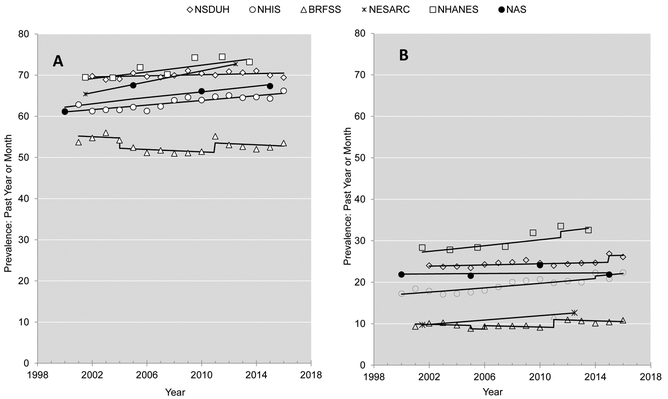
Figure 1:
Yearly prevalence estimates for (A) past year or past month alcohol use and (B) past year or past month binge drinking. Trend lines are derived from regression analyses of outcome as a function of year with dummy-indicators used to specify additional intercept parameters to reflect changes in item wording or other design changes.
Meta-Analysis.
To estimate a meta-analytic regression coefficient related to the average annual change in prevalence, we used the PROC MIXED procedure in SAS to regress the logarithm of annual prevalence estimates on year with a class variable for survey incorporated as a random intercept term. Prevalence estimates were weighted by the inverse variance (square of the standard error). A random effect for survey was chosen over a fixed-effects approach because there was clear heterogeneity in the estimates for overall time trends. (For example, I2 is a parameter often used in meta-analyses to quantify the proportion of total variance that is due to differences in effect sizes as opposed to sampling error. I2 for both full-sample trend analyses of both outcomes was greater than 99%.) As with the trend analyses described previously, dummy variables were used to adjust for any effects that changes in item wording may have had on prevalence estimates while maintaining the assumption of linearity for year-to-year change in the logarithm of the prevalence. Sensitivity analyses were also conducted to gauge the relative influence of each survey on the meta-analytic trend estimate. Specifically, each survey was removed from the analysis one at a time and the remaining five surveys were used to conduct the analyses described above.
Simulated Trends Based on Meta-analysis.
Although the meta-analysis yields an overall estimate of relative change, the random intercepts result in separate prevalence estimates for each survey (which are expected to differ as evident from Figure 1). To visually compare magnitudes of absolute change and rank-order prevalence over time, we used the meta-analysis trend estimates in conjunction with prevalence for each outcome and each demographic group from the 2002 NSDUH to calculate overall and demographic-specific trend lines. The NSDUH prevalence estimates and the survey year (2002) are simply reference points to establish the intercepts in the modeled trend lines and are somewhat arbitrary, though the choice to use NSDUH is partially justified by the results showing that NSDUH trends were closest to those from the meta-analysis. Simulated prevalence for each outcome was calculated as Piy=exp(ln(Pi,NSDUH02)+(Y-2002)*βi)), where Piy is the simulated prevalence for that group as a function of year, Pi,NSDUH02 is the NSDUH prevalence estimate for 2002 for group i, Y is year, and βi is the meta-analytic trend estimate for that group.
Results
Substantive results for both the alcohol use and binge drinking analyses are presented first, focusing on overall trends and meta-analysis estimates. Brief summaries of between-survey differences in estimates for both outcomes are presented afterward. When describing differences between demographic groups with respect to meta-analysis trend estimates, differences in estimates are significant at p<.001 unless otherwise noted.
Alcohol Use Prevalence.
A plot of the annual estimates for prevalence of past year (or past month for BRFSS) alcohol use for each survey is presented in Figure 1A with trend lines derived from log-binomial regression analyses as described in the Methods section. The individual and meta-analytic regression parameter estimates describing trends in prevalence for the full population and for each specific demographic group are shown in Figure 2 in forest-plot format; regression coefficient estimates and standard errors are tabulated in Supplementary Table 2. Those estimates were converted to parameters describing the average 10-year change and these are summarized in Supplementary Table 3. Prevalence estimates for years 2002 and 2013 for each survey and each demographic group are provided in Supplementary Table 4 to provide readers with baseline prevalence and reference points to gage the magnitude of observed absolute change within each survey.
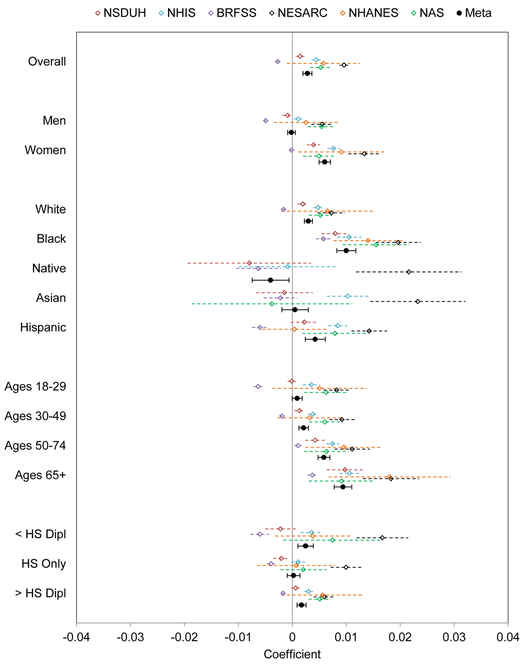
Figure 2:
Forest plot of regression coefficients describing the association between prevalence of alcohol use and year for each of the six survey series and meta-analysis regression coefficient. Error bars represent 95% confidence intervals
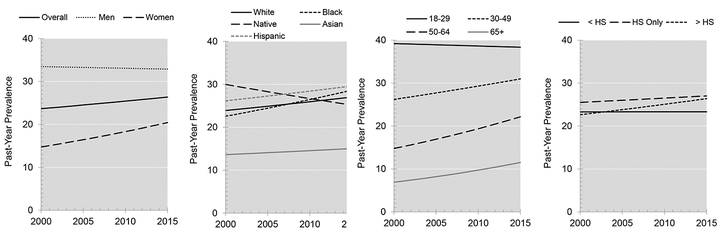
Meta-analytic estimates suggested an overall significant increase in the prevalence of alcohol use of approximately 0.3% per year (β=.0030) or a net increase of 3.0% per decade. This increase was larger among women (~0.6% per year) and was not significant among men. With respect to race/ethnicity, the largest net increase of nearly 1.0% per year was observed among Blacks; smaller increases were observed for Whites and Hispanics (0.3% and 0.5% per year, respectively), no significant change was observed for the Asian/Pacific Islander group, and a significant decrease in prevalence was observed for Native Americans (β=−.0040, SE=.0017, p=.02). The rate of increase in alcohol use varied markedly as a function of age, with no significant increase observed in the 18–29 year group. A small but significant increase was observed for the 30–49 year group, but much larger increases were observed for the 50–64 and 65+ age groups with an annual increase of nearly 1% for the 65 and over group. Differences by educational attainment were comparatively small. Simulated trend lines for past-year alcohol use prevalence using reference data from the NSDUH and calculated based on the meta-analytic trend estimates are plotted in Figure 3.
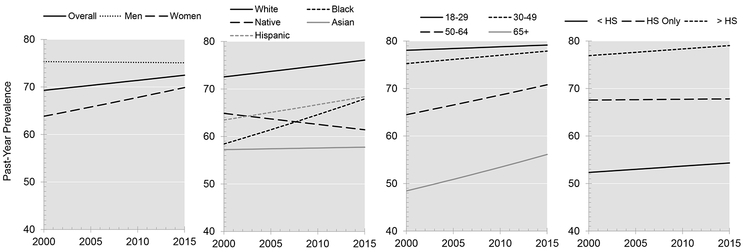
Figure 3:
Simulated trend lines for past year alcohol use prevalence based on trend estimates from meta-analysis and using 2002 NSDUH data to establish baseline prevalence.
Results of sensitivity analyses, in which each survey was omitted from the meta-analysis while the other five were analyzed, are shown in Supplementary Figure 1. Full sample estimates were relatively insensitive to the omission of any given survey, though there was some variation in estimates for smaller demographic subgroups.
Binge Drinking Episodes.
A plot of the prevalence of past-month or past-year binge drinking is provided in Figure 1B (past month for NSDUH and BRFSS, past year for others). Survey-specific and meta-analytic parameter estimates are shown in Figure 4; parameter estimates are tabulated in Supplementary Table 5, with net change parameters provided in Supplementary Table 6. Prevalence estimates by demographic group for each survey for years 2002 and 2013 are provided in Supplementary Table 7.
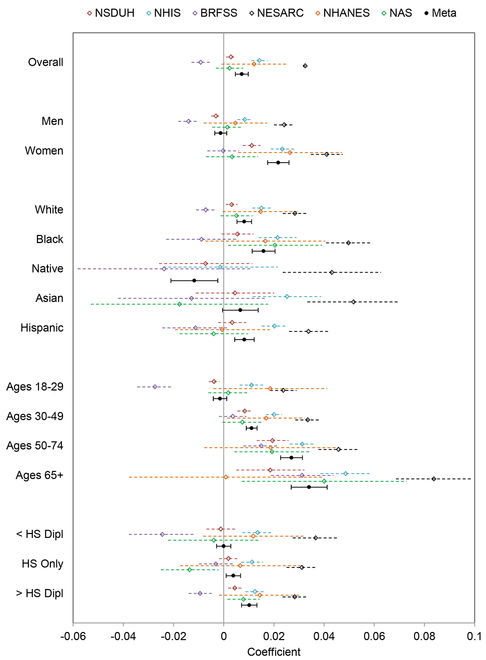
Figure 4:
Forest plot of regression coefficients describing the association between prevalence of binge drinking and year for each of the six survey series and meta-analysis regression coefficient. Error bars represent 95% confidence intervals.
The consensus estimate for the rate of increase in proportion reporting one or more binge drinking episodes was higher than that for alcohol use: β=.0072, which corresponds to a net increase of 7.5% per decade. As with drinking prevalence, a significant increase was observed among women but not for men. Increases in binge drinking prevalence were significant for White, Black, and Hispanic race/ethnicity groups, but not for Asians/Pacific Islanders. There was a significant trend toward lower rates for Native Americans (β=−.012, SE=.0048, p=0.02). Binge drinking prevalence for both Blacks and Hispanics increased significantly faster than it did for Whites; the increase for both of those minority groups was over 1% per year, whereas that for Whites was approximately 0.6% per year. As was the case for alcohol use prevalence, the magnitude of the increase in binge drinking prevalence was non-significant for 18–29 year olds and increased strongly with age. Average annual increases were 1.1% for 30–49 year olds, 2.7% for ages 50–64, and 3.4% for individuals aged 65 and over. Differences in the rate of increase in binge drinking prevalence by education was relatively small, although the increase for those with education beyond high school was significantly larger than that for those without a high school education for whom there was no increase (approximately 1.0% annually for post-secondary group vs. 0.0% for less than high-school, z=4.7, p<.001). Simulated trend lines using reference data from the NSDUH and calculated based on the meta-analytic trend estimates are plotted in Figure 5.
Figure 5:
Simulated trend lines for past year binge drinking prevalence based on trend estimates from meta-analysis and using 2002 NSDUH data to establish baseline prevalence.
Results of sensitivity analyses examining the impact of each individual survey on the overall results are shown in Supplementary Figure 2. As with the alcohol prevalence analyses, full sample estimates were relatively insensitive to the omission of any given survey with the exception that omission of the NSDUH would have resulted in larger estimated increases in binge drinking for most demographic groups. For example, omitting the NSDUH would have resulted in significant estimated increases in binge drinking prevalence for both men and 18–29 year olds, whereas estimates for these groups were not significant when all surveys were analyzed.
Between-Survey Differences.
Estimates for rates of change in the prevalence of alcohol use and the prevalence of one or more binge-drinking episodes varied markedly across surveys. In fact, for the four surveys with the largest sample sizes (NSDUH, NHIS, BRFSS, NESARC), there was no overlap in the 95% confidence intervals between any two surveys for the full-sample analyses of either alcohol use prevalence or binge drinking prevalence. Estimated rates of change were highest for the NESARC, both overall and for individual demographic groups, and lowest for BRFSS, for which estimates suggested downward trends in both alcohol use and binge drinking for most demographic groups. (BRFSS was the only survey to suggest overall downward trends.) For the overall analyses, and for most demographic subgroup analyses, NSDUH estimates deviated the least from the meta-analytic estimates, whereas NESARC estimates deviated the most. The difference between NESARC estimates and meta-analytic estimates were particularly pronounced for binge drinking outcomes. For example, the NESARC estimated a 10-year increase of 38% in the prevalence of binge drinking from 2002–2013 (95% CI: 37.2, 39.6) compared with a meta-analytic estimate of 7.5% (95% CI: 4.8, 10.3).
Discussion
Overview of Results.
Using a random-effects meta-analysis to synthesize data from 61 administrations of six nationally representative surveys of the US adult population covering the years 2000 through 2016, we estimate that the prevalence of past-year alcohol use has been increasing at a relative rate of 0.3% per year and that the prevalence of binge drinking has been increasing at a relative rate of 0.7% per year. The increase in alcohol use was particularly pronounced among women, Blacks, and individuals ages 50 and older; prevalence increased for these groups at more than twice the rate than for the general population. The same groups underwent notable increases in binge drinking, along with individuals ages 30–49 and individuals with at least some postsecondary education; all of these groups experienced relative increases in the prevalence of binge drinking of more than 1% per year. For both outcomes, however, it is important to emphasize that the groups that underwent the largest relative increases often had lower baseline rates for alcohol use and binge drinking than comparison groups (See Figures 3 and 5). For example, for both outcomes, prevalence was consistently higher for men than for women, and for younger age groups than older, both at the beginning and end of the observation period.
The estimates for rates of increase of both outcomes are much smaller than those derived from the analysis of two administrations of the NESARC in 2001–2002 and 2012–2013, which served as the basis of an earlier analysis of trends in drinking outcomes (Grant et al., 2017). Our analysis of NESARC data yielded an estimated increase in the prevalence of alcohol use of approximately 1% per year, with an increase in prevalence of binge drinking of over 3% per year. These correspond to increases of 11% and 38% per decade, which are four and five times higher than the meta-analysis estimates, respectively. The NESARC results suggest that increases in both alcohol use and binge drinking have occurred among men and women, all race/ethnicity groups, all ages, and all educational attainment categories. In contrast, the meta-analysis found no increases in the prevalence of either outcome for men, Native Americans, Asians, or individuals aged 18–29. Thus, the meta-analysis suggests smaller but still concerning increases in alcohol outcomes, and highlights particular demographic groups that underwent especially large increases.
Several methodological differences between the 2001–2002 NESARC and the 2012–2013 NESARC-III may have contributed to higher prevalence estimates for the latter survey, possibly resulting in NESARC trend estimates that were much higher than those for other surveys. These include the use of private-sector interviewers for NESARC-III in contrast to interviewers from the US Census for the 2001/2 survey, the introduction of biological sample collection for NESARC-III, changes in survey content, and the use of incentives for the latter survey (Grant et al., 2014, Center for Behavioral Health Statistics and Quality, 2017, Lopez, 2017, Grucza et al., 2016). These factors may explain why the NESARC estimates suggested larger increases for both outcomes and for every demographic subgroup than any of the other surveys analyzed. In contrast, NSDUH estimates were closest to the meta-analytic estimates for both outcomes and for the majority of demographic subgroup analyses. The NSDUH conducts in-person interviews with audio-computer-assisted self-interview (ACASI), which is less sensitive to social desirability bias. NSDUH survey content and methodology were fairly consistent over the 2002–2016 period, which was the period we included here.
Between-Survey Differences.
Estimated trends from the six survey series were widely discrepant. There are many reasons to expect prevalence estimates to vary from survey to survey related to the wording of questions, social desirability bias, differences in survey coverage, and other factors (Tourangeau et al., 2000, Groves et al., 2009). One might reasonably assume that the error induced by these factors is relatively constant from year to year; i.e., that under a given set of measurement conditions, a proportion of people who actually drink will report doing so and that this proportion should be fairly stable over time. This is clearly not the case here: for the larger surveys (NSDUH, NESARC, NHIS, BRFSS), there was no overlap in confidence intervals between any two surveys for full-population trend estimates for either outcome. While this might seem to be a cause for pessimism about alcohol survey research, there are areas of agreement across surveys. For example, estimates of change in both outcomes were consistently more positive for women than for men and for older age groups compared to younger ones. Thus, although there was little consistency in the trend estimates themselves, there was reasonable consistency in the demographic differences among the trends.
Perhaps the main lesson to be drawn is that it is essential to consider more than one survey data source whenever possible when drawing conclusions about trends in alcohol use and other health behaviors and to look for areas of concordance across surveys. This is straightforward for alcohol use and smoking, measures of which are contained in all six of the surveys described here. Because most of these data sources are publicly available, the meta-analytic approach described here is accessible to all investigators. However, measures of adult illicit drug use are more limited; this is assessed annually by the NSDUH and periodically by the NAS (since 1984) and the NESARC and its predecessor, the National Longitudinal Alcohol Epidemiologic Survey (NLAES), administered in 1991/1992.
Implications for Public Health.
Although the estimates for rates of increase in alcohol use prevalence and binge drinking prevalence are much lower than expected based on the earlier results from the NESARC (Grant et al., 2017), the fact that these increases are occurring in the context of an aging population raises significant public health concerns. The largest increases for both outcomes were observed among individuals ages 50 and older, and substantial increases in binge drinking were observed for individuals aged 30–49. Using NSDUH data, Keyes and Miech have previously observed that the birth cohorts with the highest rates of binge episodic drinking—adjusting for age and period effects—were born approximately between 1950 and 1984 (Keyes and Miech, 2013). Similarly, age-period-cohort analyses using NAS data found elevated alcohol use and binge drinking among the 1976–1985 birth cohorts (Kerr et al., 2009, Kerr et al., 2013). These individuals were between the ages of 31 and 65 toward the end of our observation period, which may account for the increases in the 30–49 and 50–64 year age groups. Keyes and Miech (Keyes and Miech, 2013) also found that women born between 1935 and 1949 had high rates of binge drinking, particularly in comparison to women born prior to 1935, for whom rates were very low. NAS data also showed higher binge drinking among women in the 1956–1960 birth cohort relative to the earlier birth cohorts. These cohort effects may have contributed to the increases in binge drinking among the oldest age group and women. It remains to be seen whether period effects or age-period interactions are responsible for the uptick in binge drinking in these groups. In other words, the increase in binge drinking among adults ages 30 and older may stem from birth cohorts with elevated risk for binge drinking with a continued higher risk as they age, or from a normalization of binge drinking among older age groups, or from a combination of these factors.
Regardless of the specific trend explanations, it is clear that elevated binge drinking rates among older Americans correspond to a significant increase in alcohol-related morbidity. These observations shed some light on the apparent paradox between relatively small increases in per capita alcohol consumption and large increases in alcohol-related health problems (Yoon and Chen, 2016, Mullins et al, 2017, Haughwout and Slater, 2017, Mellinger et al, 2018). White and colleagues recently documented a 62% increase in the rate of alcohol-related emergency department visits over the years 2006 to 2015 (White et al., 2018). The largest increases were among individuals aged 45–64 and were due to increases in rates of visits for both chronic and acute conditions. Remarkably, baseline rates of visits were also highest for these ages, despite the fact that binge drinking rates are highest among younger age groups (Supplementary Table 7). Similarly, Kanny and colleagues (2015) found that 76% of fatal alcohol poisonings occur among men ages 35–64. Analyses presented here used different age categorizations than White and colleagues, so we cannot make direct comparisons, but the risk for both alcohol-related injury and chronic illness among binge drinkers appears to increase dramatically as a function of age. Thus, even small absolute increases in rates of binge drinking among older Americans—which correspond to large relative increases—likely account for a substantial increase in alcohol-related injury and disease burden.
Despite being able to derive meta-analytic estimates from a large number of administrations of six repeated national surveys, there are several limitations to these findings. The first is the assumption of the random-effects meta-analysis model: that the trend estimates from the surveys are drawn from a theoretical normally distributed sample. In other words, differences between estimates constitute random error rather than bias. It may be that some surveys are inherently better at measuring alcohol-related behaviors than others, or that some surveys are more methodologically consistent from year to year than others. Perhaps ideally, some surveys should be weighted more highly than the others. The agnostic meta-analytic approach may not be optimal, but our results underscore the importance of synthesizing data from multiple sources. Relatedly, we emphasize that this analysis of relative change in outcomes over time does not help clarify differences among point-prevalence estimates. The random-effects model assumes all prevalence estimates are influenced by unobservable factors that are specific to each survey. Additionally, we noted that some surveys changed the threshold for women in binge drinking questions, and that the BRFSS changed the gateway questions for alcohol use. These changes were dealt with using dummy variables in the regression equation, which necessarily assumes that the same wording change would have had the same effect in any given year. This is a face-valid but ultimately untestable assumption. Finally, we should note that all surveys based on self-reported alcohol use result in substantial under-reporting of consumption when compared with alcohol sales data (Kerr and Greenfield, 2007).
Limitations notwithstanding, the heterogeneity in estimates of alcohol trends is surprising, and underscores the importance of quantitative comparison of data from multiple sources when drawing inferences about national trends. Against the backdrop of this heterogeneity, however, surveys consistently found increasing rates of alcohol use for adults ages 50 and over, and increasing rates of binge drinking for adults ages 30 and over, with the largest increases seen in the oldest age group, 65 and over. Despite significant disagreements among survey series, these results leave little doubt that excessive alcohol use among Americans in middle-adulthood and beyond is on the rise, and this observation is concordant with data from other sources. A strong majority of binge drinkers likely do not meet criteria for severe AUD and so these findings do not necessarily portend a large increase in conventional treatment needs (Esser et al., 2014). Thus, targeted screening and brief intervention may be an effective strategy, particularly when implemented in primary care or emergency department settings, given that utilization of both types of services increase with age (Schappert and Burt, 2006). Furthermore, it may be important to understand the differential impact by age of various types of policy interventions such as alcohol tax and price increases and restrictions on outlet density and to implement alcohol policies that are most effective at curbing drinking for those in mid-adulthood (Grucza and Plunk, 2016). Another area for further research and possible intervention is the co-use of alcohol and prescription drugs, particularly other central nervous system depressants such as benzodiazepines and opioids. While the role of interactions involving these drugs in alcohol-related morbidity trends is largely uncharacterized, higher usage with age combined with increasing prescription rates for psychotropic medications over time among US adults in combination with rising rates of binge drinking is clearly a cause for concern (Olfson et al., 2014; Bachhuber et al., 2016; Hirschtritt et al., 2018). This emerging public health problem warrants a deeper understanding and targeted pragmatic alcohol-related interventions in middle-adulthood and beyond.
Supplementary Material
Acknowledgements:
We thank Mr. Glennon M. Floyd for editorial assistance while developing this manuscript. The authors have no financial relationships relevant to this article to disclose. We gratefully acknowledge the Centers for Disease Control, the Inter-University Consortium for Political and Social Research, the Minnesota Population Center, the Alcohol Research Group, and the National Institute for Alcohol Abuse and Alcoholism for making data publicly available.
Funding Source: This work was supported by grants from National Institutes of Health R01AA024133 (KJS) P50AA005595 (WCK, CKL), R21 AA025689, R01DA042195 (RAG), R01DA036583, U10AA008401 (LJB). The funding agency and data providers had no role in the design, conduct, collection, management, analysis, or interpretation of data, or the preparation, review, or approval of this paper.
Footnotes
Interests: LJB is listed as an inventor on issued U.S. patent 8,080,371, “Markers for Addiction,” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction. Other authors have no interests to declare.
References
- Askgaard G, Gronbaek M, Kjaer MS, Tjonneland A, Tolstrup JS (2015) Alcohol drinking pattern and risk of alcoholic liver cirrhosis: a prospective cohort study. Journal of hepatology 62:1061–1067. [DOI] [PubMed] [Google Scholar]
- Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL (2016) Increasing Benzodiazepine Prescriptions and Overdose Mortality in the United States, 1996–2013. Am J Public Health 106:686–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady JE, Li G (2014) Trends in alcohol and other drugs detected in fatally injured drivers in the United States, 1999–2010. American Journal of Epidemiology 179:692–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality (2017) 2016 National Survey on Drug Use and Health: Methodological summary and definitions, in Series 2016 National Survey on Drug Use and Health: Methodological summary and definitions, Rockville, MD. [Google Scholar]
- Centers for Disease Control and Prevention (2004) Health behavior of adults, 1999–2001, in Series Health behavior of adults, 1999–2001, Centers for Disease Control and Prevention, Hyattsville, MD. [Google Scholar]
- Centers for Disease Control and Prevention (2012) Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates MMWR Morb Mortal Wkly Rep 61:410–413. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2016) Health behavior of adults, 2011–2014, in Series Health behavior of adults, 2011–2014, Centers for Disease Control and Prevention, Hyattsville, MD. [Google Scholar]
- Centers for Disease Control and Prevention (2017a) CDC Wonder: Multiple Cause of Death, 1999–2016, in Series CDC Wonder: Multiple Cause of Death, 1999–2016.
- Centers for Disease Control and Prevention (2017b) Behavioral Risk Factor Surveillance System, 2016 Summary Data Quality Report, in Series Behavioral Risk Factor Surveillance System, 2016 Summary Data Quality Report.
- Cheng HG, Kaakarli H, Breslau J, Anthony JC (2018) Assessing changes in alcohol use and alcohol use disorder prevalence in the United States: evidence from national surveys from 2002 through 2014. JAMA psychiatry 75:211–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS (2014) Prevalence of alcohol dependence among US adult drinkers, 2009–2011. Prev Chronic Dis 11:E206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, Jung J, Zhang H, Fan A, Hasin DS (2017) Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA psychiatry 74:911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chu A, Sigman R, Amsbary M, Kali J, Sugawara Y, Jiao R, Ren W, Goldstein RB (2014) National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) - III, in Series National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) - III, Bethesda, MD. [Google Scholar]
- Groves RM, Fowler FJ Jr, Couper MP, Lepkowski JM, Singer E, Tourangeau R (2009) Survey Methodology. 2 ed, Wiley, Hoboken, NJ. [Google Scholar]
- Grucza RA, Agrawal A, Krauss MJ, Cavazos-Rehg PA, Bierut LJ (2016) Recent trends in the prevalence of marijuana use and associated disorders in the United States. JAMA psychiatry 73:300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Plunk AD (2016) Public policy and alcohol use, in Prevention Policy, and Health Public, Prevention, Policy, and Public Health (MORELAND-RUSSELL S, BROWNSON RC eds), Oxford University Press, New York. [Google Scholar]
- Hatton J, Burton A, Nash H, Munn E, Burgoyne L, Sheron N (2009) Drinking patterns, dependency and life-time drinking history in alcohol-related liver disease. Addiction 104:587–592. [DOI] [PubMed] [Google Scholar]
- Haughwout SP, Slater ME (2017) Survelliance Report #108: Apparent per capita alcohol consumption: national, state, and regional trends, 1977–2015. Figure 1: Total per capita ethanol consumption, United States, 1935–2015, in Series Survelliance Report #108: Apparent per capita alcohol consumption: national, state, and regional trends, 1977–2015. Figure 1: Total per capita ethanol consumption, United States, 1935–2015, National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Hingson R, Zha W, Smyth D (2017) Magnitude and Trends in Heavy Episodic Drinking, Alcohol-Impaired Driving, and Alcohol-Related Mortality and Overdose Hospitalizations Among Emerging Adults of College Ages 18–24 in the United States, 1998–2014. J Stud Alcohol Drugs 78:540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschtritt ME, Delucchi KL, Olfson M (2018) Outpatient, combined use of opioid and benzodiazepine medications in the United States, 1993–2014. Preventive medicine reports 9:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICPSR. National Survey on Drug Use and Health (NSDUH) Series. Available at: https://www.icpsr.umich.edu/icpsrweb/ICPSR/series/64.
- Ikeda K, Saitoh S, Koida I, Arase Y, Tsubota A, Chayama K, Kumada H, Kawanishi M (1993) A multivariate analysis of risk factors for hepatocellular carcinogenesis: a prospective observation of 795 patients with viral and alcoholic cirrhosis. Hepatology (Baltimore, Md) 18:47–53. [PubMed] [Google Scholar]
- Kanny D, Brewer RD, Mesnick JB, Paulozzi LJ, Naimi TS, Lu H (2015) Vital signs: alcohol poisoning deaths - United States, 2010–2012. MMWR Morb Mortal Wkly Rep 63:1238–1242. [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK (2007) Distribution of alcohol consumption and expenditures and the impact of improved measurement on coverage of alcohol sales in the 2000 National Alcohol Survey. Alcohol Clin Exp Res 31:1714–1722. [DOI] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J (2009) Age-period-cohort modelling of alcohol volume and heavy drinking days in the US National Alcohol Surveys: divergence in younger and older adult trends. Addiction 104:27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Ye Y, Bond J, Rehm J (2013) Are the 1976–1985 birth cohorts heavier drinkers? Age-period-cohort analyses of the National Alcohol Surveys 1979–2010. Addiction 108:1038–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Miech R (2013) Age, period, and cohort effects in heavy episodic drinking in the US from 1985 to 2009. Drug and alcohol dependence 132:140–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez G A study finding a huge increase in alcoholism may have been seriously flawed. Available at: https://www.vox.com/science-and-health/2017/8/16/16150548/alcoholism-study.
- Mellinger JL, Shedden K, Winder GS, Tapper E, Adams M, Fontana RJ, Volk ML, Blow FC, Lok AS (2018) The High Burden of Alcoholic Cirrhosis in Privately Insured Persons in the United States Hepatology 2018 Mar 26 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Minnesota Population Center. Integrated Public Use Microdata Series (IPUMS) International: version 6.5 [dataset]. Available at: 10.18128/D020.V6.5,2017. [DOI]
- Mullins PM, Mazer-Amirshahi M, Pines JM (2017) Alcohol-Related Visits to US Emergency Departments, 2001–2011. Alcohol Alcohol 52:119–125. [DOI] [PubMed] [Google Scholar]
- National Institute of Alcohol and Alcoholism (2000) Tenth Special Report to the U.S. Congress on Alcohol and Health, in Series Tenth Special Report to the U.S. Congress on Alcohol and Health, National Institutes of Health, Bethesda, MD. [Google Scholar]
- Olfson M, Blanco C, Wang S, Laje G, Correll CU (2014) National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA psychiatry 71:81–90. [DOI] [PubMed] [Google Scholar]
- Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, Bierut LJ, Grucza RA (2014) Alcohol consumption, heavy drinking, and mortality: rethinking the j-shaped curve. Alcohol Clin Exp Res 38:471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schappert SM, Burt CW (2006) Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001–02. Vital and health statistics. Series 13, Data from the National Health Survey:1–66. [PubMed] [Google Scholar]
- Abuse Substance and Mental Health Services Administration (SAMHSA) (2015) Behavioral health trends in the United States: results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUH Series H-50) [Google Scholar]
- Tourangeau R, Rips LJ, Rasinski K (2000) The Psychology of Survey Response, Cambridge University Press, Cambridge. [Google Scholar]
- Wetterling T, Veltrup C, Driessen M, John U (1999) Drinking pattern and alcohol-related medical disorders. Alcohol and alcoholism 34:330–336. [DOI] [PubMed] [Google Scholar]
- White AM, Slater ME, Ng G, Hingson R, Breslow R (2018) Trends in alcohol-related emergency department visits in the United States: results from the Nationwide Emergency Department Sample, 2006 to 2014. Alcohol Clin Exp Res 42:352–359. [DOI] [PubMed] [Google Scholar]
- Yoon YH, Chen CM (2016) Mortality in the United States: national, state, and regional trends, 2000–2013, in Series Mortality in the United States: national, state, and regional trends, 2000–2013, National Institute on Alcohol Abuse and Alcoholism, Rockville, MD. [Google Scholar]
- Zaldivar Fujigaki JL, Arroyo Valerio AG, Lopez Alvarenga JC, Gutierrez Reyes EG, Kershenobich D, Hernandez Ruiz J (2015) Alterations in activation, cytotoxic capacity and trafficking profile of peripheral CD8 T cells in young adult binge drinkers. PLoS One 10:e0132521. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.