Abstract
Background
One quarter of the global population is of menstruating age, yet menstruation is shrouded in discrimination and taboos. Disability also carries stigma, so disabled people may face layers of discrimination when they are menstruating. The objective of the review is to assess the menstrual hygiene requirements of disabled people, the barriers they face, and the available interventions to help them manage their menstruation hygienically and with dignity.
Methods
Eligible studies, gathered across all countries, were identified by conducting searches across four databases (MEDLINE, PubMed, EMBASE, Global Health) in May 2017, with alerts set on each database to highlight new titles added until April 2018. Eligible studies incorporated analyses relevant to menstruating disabled people and/or how their carers provide support during their menstrual cycle.
Results
The 22 studies included were published since 1976; the majority after 2010 (n = 12; 55%). One study was a quasi-experiment; all others were observational. Most studies (n = 15; 68%) were from high income countries and most (n = 17; 77%) focused on people with intellectual impairments, so the review findings focus on this group and their carers. Outcomes investigated include choice and preference of menstrual product, ability to manage menstrual hygiene and coping strategies applied. Barriers faced included a lack of standardised guidance for professional carers; a lack of menstruation training, information and support provided to people with intellectual impairments and their carers; a lack of understanding of severity of symptoms experienced by people with intellectual impairments, the high cost of menstrual products and lack of appropriate options for people with physical impairments. Few interventions were found, and strategies for menstrual hygiene management applied by carers of persons with intellectual impairments include limiting the disabled person’s movements when menstruating and suppressing their menstruation.
Conclusions
Little evidence was identified on the requirements of disabled people and their carers in managing their menstruation, and only one intervention, but a range of barriers were identified. This gap in evidence is important, as the consequences of failing to meet menstrual hygiene needs of disabled people includes shame, social isolation, and even sterilisation.
Systematic review registration
PROSPERO CRD42018095497.
Introduction
Globally, 663 million people lack access to safe water and 2.4 billion people lack access to adequate sanitation [1]. There is extensive literature showing that disabled people face barriers in accessing appropriate water, sanitation and hygiene (WASH) services in low and middle income countries (LMICs) [2–4]. WASH services are vital for effective menstrual hygiene management (MHM).
UNICEF and the WHO define menstrual hygiene management as “Women and adolescent girls using a clean menstrual management material to absorb or collect blood that can be changed in privacy as often as necessary for the duration of the menstruation period, using soap and water for washing the body as required, and having access to facilities to dispose of used menstrual management materials. They understand the basic facts linked to the menstrual cycle and how to manage it with dignity and without discomfort or fear” [5]. Menstrual hygiene management also involves addressing harmful societal beliefs and taboos surrounding the issue [6].
Approximately 75% of people experience premenstrual syndrome (PMS), which includes emotional and physical symptoms that occur between one and two weeks before menstruation [7]. Regular menstruation is a sign of health and fertility; it is inherently female. However, drawing on feminist theory, femininity is linked to beauty, freshness and cleanliness [8]; these are opposed to the qualities associated with menstruation: dirty, bloody and smelly. This means menstruation does not conform to the gender stereotypes, is linked to inferiority and contributes to the devaluation of females [9]. This dichotomy may begin to explain menstrual taboos [9]. These points are demonstrated through the ‘Tampon Experiment’, which aimed to understand how a menstruating woman is perceived by others [8]. When an informed research participant dropped a tampon (a visible reminder than women menstruate) on the floor, she was viewed more negatively by men and women than when she dropped the hair clip (considered a feminine item that is not linked to bodily functions) [8].
Menstrual taboos are rooted in, and drive gender inequality. In some settings menstruating people are viewed as impure, so they are separated from men and banned from using the same water sources in order not to contaminate them [10, 11]. These taboos and social beliefs have led some people to internalise this stigma, reporting that they feel dirty when menstruating and are ashamed of it [12, 13].
Menstruation is not widely spoken about [14, 15]. Many pre-pubescent girls do not receive information about menstruation, so their first menstrual cycle can be a frightening experience. In India, a cross sectional study of 387 school going girls reported that only 37% of them were aware of menstruation before menarche [16].
Affordability of menstrual products is an issue in many countries, especially for people from lower socio-economic groups. In many LMICs, people use bark, paper, sand, mud or cloth to absorb menstrual blood [9]. Evidence exists that some adolescent girls in western Kenya engage in transactional sex to obtain sanitary pads [17–20], contributing to exposure to sexually transmitted diseases [21], pregnancy and school dropout [22].
Attention on MHM has increased over the last decade. Examples include the socio-ecological framework for MHM (developed for school girls and their families) to guide research and interventions in LMICs [23] and the inclusion of MHM in the Sustainable Development Goal 6 [24].
This shift is encouraging, but MHM efforts must be inclusive of disabled people.
This review applies the UN Convention on the Rights of Persons with Disabilities’ (CRPD) definition of disability: ‘Persons with disabilities include those who have long-term physical, mental, intellectual or sensory impairments which in interaction with various barriers may hinder their full and effective participation in society on an equal basis with others’ [25].
Like menstruation, disability often carries stigma [26]. Research in Uganda and Zambia demonstrate that disabled people are considered ‘dirty’ and contagious, so can be banned from using public latrines and water points [27]. It is likely that disabled people face layers of discrimination when they are menstruating, which will vary for people with different impairment types. Inaccessible latrines means disabled people who cannot stand or see often have to crawl, or sit on dirty latrine seats to change their pads or cloths [10]. People with visual impairments may be unable to identify when their period started and finished [3]. People with hearing, communication or intellectual impairments may be less able to communicate when they are in pain or need support [10]. There is a widespread misconception that disabled people are asexual, so do not receive information on sexual and reproductive health, or menstrual hygiene [10, 26, 28].
Objectives
The objective of the review is to assess the menstrual hygiene requirements of disabled people, the barriers they face, and the available interventions to help them manage their menstruation hygienically and with dignity. A review protocol is registered online with PROSPERO; registration number: CRD42018095497.
Disclaimer
This review recognises that gender is a social construct, non-binary and fluid. People who menstruate may identify themselves as male, female, or neither. Therefore, this review uses the terms ‘person’, or ‘people’ who menstruate rather than ‘female’, ‘women’ or ‘girl’, unless these terms are pertinent to the study or theory referenced. The authors also chose to use the terminology ‘disabled people’ rather than ‘people with disabilities’.
Materials and methods
Search strategy
The search strategy was designed to identify peer reviewed published studies researching disability and MHM. The review covered all countries; no date limit was set to ensure the widest range of articles could be identified. The searches were conducted in May 2017, with alerts set on each database to highlight new titles added since then. Four online databases were used: MEDLINE, PubMed, EMBASE and Global Health through Ovid SP. Additional relevant studies were identified by reviewing references of included studies and scanning the internet for relevant studies after the database searches were completed. Search terms were generated to encapsulate three main concepts: disability, menstruation and hygiene management. Disability included both specific impairments and broad assessments (e.g. self-reported functional or activity limitations) (S1 Table).
Inclusion / Exclusion criteria
To be eligible, papers had to in English, published in a peer reviewed journal; be original primary research including experimental, observational and qualitative studies, but excluding economic analyses, systematic reviews, project reports, and policy analysis. No exclusion criteria were set on world region or date of publication. Studies were excluded if they reported no empirical qualitative or quantitative data on MHM and if they analysed disability without the inclusion of MHM and vice versa.
Eligible participants were menstruating disabled persons and/or the carers of disabled persons who provide support during their menstrual cycle. Carers were professionals or family members working in institutions or at home. Disabled persons had specific impairments, activity limitations or self-identified as disabled.
Papers were required to investigate the extent to which disabled people and their carers are able to understand and manage their menstrual cycle hygienically and with dignity. The relevant outcomes explored were purposefully broad as there were anticipated to be limited published studies on the issue. Example outcomes include choice of menstrual management material and preference, ability to manage menstrual hygiene and the menstrual cycle; challenges experienced during menstruation and coping strategies applied; changes in behaviour through the menstrual cycle and its management.
Study selection
All studies identified through the search process were exported to EndNote version X7. Duplicates were removed. Two authors independently double screened the titles, abstracts and key words against the eligibility criteria. Results were compared and contrasted and full-text records of potentially relevant publications were obtained and screened using the inclusion criteria for final selection of studies for the systematic review.
Data extraction
Data was extracted from the final selection of studies using pre-designed tables and the socio-ecological framework for menstrual hygiene management [23]. Through the data abstraction process for this review, a number of gaps in the socio-ecological framework in relation to the MHM requirements of disabled people and their carers were identified and additions were made to fill these gaps (Table 1, with changes marked in italic).
Table 1. Socio-ecological framework for menstrual hygiene management [23].
| Factors that support MHM | Outcomes |
|---|---|
| Societal and government policy factors | Policies, strategies and curriculum; training standards and practices; traditional norms, practices and cultural beliefs |
| Environmental and resource availability factors | Water and sanitation facilities including for solid waste management; availability of affordable, usable and culturally appropriate sanitary protection materials |
| Interpersonal factors–disabled person | Relationship with family, carer (family and / or professional); relationships with healthcare workers, teachers and other people in authority; relationships with peers; perceptions of changes in gender roles post-menarche |
| Interpersonal factors–Carer | Relationship with family, the disabled person; relationships with healthcare workers and other people in authority; relationships with the wider community; perceptions of changes in gender roles post-menarche |
| Personal factors–disabled person | Knowledge about the biology of menstruation and MHM, information on menstruation and MHM; skills in coping and behavioural adaptions (including pain relief); attitudes, beliefs and feelings about menstruation (including sterilisation / long-term contraception); ability to manage menstruation independently, and support required |
| Personal factors–Carer | Knowledge about the biology of menstruation and MHM, information on menstruation and MHM; skills in coping and behavioural adaptions (including pain relief); attitudes, beliefs and feelings about menstruation (including sterilisation / long-term contraception); ability to manage another person's menstruation independently, support required and caring tasks related to MHM |
| Biological factors | Menstrual variations due to age and features of menstrual cycle (regular, irregular, heavy, light) and any other biological changes related to menstruation; intensity of menstruation (pain) and influences on behaviour, health and concentration; biological issues that impact on MHM, such as incontinence |
Data was extracted into Microsoft Excel against the following study and framework components:
Publication details: author/s, year, title
Study location: low, middle or high-income country, country name
Methods: study design
Participants: source of participants (household, institution), disability type (e.g. intellectual impairments, physical impairments), means of assessing disability, carer type (family member, professional), sample size
Aspect of MHM considered
Quality assessment
A meta-analysis was not conducted due to the lack of consistency in study designs, population types and outcomes included. The review was conducted to meet the requirements of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA) [29].
Quality assessment
Studies were assessed for their potential risk of various types of bias, by applying an approach used by Banks et al. [30]. This quality scoring used modified versions of the assessment tools STROBE and RATS for quantitative and qualitative studies [31, 32]. Assessment focused on the risk of potential biases stemming from study design, sampling methods, data collection, data analysis and interpretation. As study methodologies varied widely, papers were evaluated to assess their overall risk of bias instead of applying a rigid cut off criteria. Studies were graded as having a low risk of bias when all or almost of the criteria were fulfilled, and those that were not fulfilled were thought unlikely to alter the conclusions of the study; medium risk of bias when some of the criteria were fulfilled, and those not fulfilled were thought unlikely to alter the conclusions of the study; and high risk of bias when few or no criteria were fulfilled, and the conclusions of the study were thought likely or very likely to alter the conclusions of the study [30] (S2 Table).
Results
Study selection
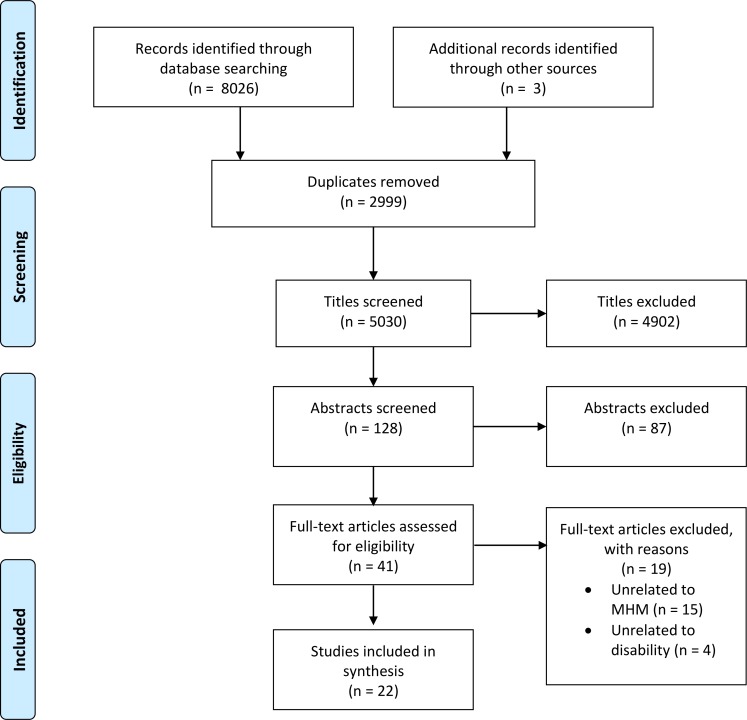
8026 records were identified through database searches. An additional 3 records were sourced through the authors’ knowledge of the available literature. 2999 duplicates were found and removed. An additional 4902 studies were excluded in the title screening process and a further 87 records were excluded through screening the abstracts. 41 full text articles were assessed and 19 were excluded. The remaining 22 studies were included. No additional studies were sourced through database alerts (Fig 1).
Fig 1. Search strategy with PRISMA flow diagram.
Study characteristics
A summary of the characteristics of included studies are presented in Table 2. Data extracted from all studies against study framework components is captured in Table 3. Studies were published between 1976 and 2017, with the majority published after 2010 (n = 12; 55%). Most of the studies were conducted in high income settings (n = 15, 68%), including Northern Europe (UK, Netherlands and Denmark) (n = 6; 27 Eastern Asia (Taiwan, n = 4, 18%) Northern America (USA and Canada, n = 4, 18%) and Australia and New Zealand (n = 1, 5%). Only seven were conducted in LMICs (32%), including in Southern Asia (India, n = 3, 14%); Eastern Europe (Turkey, Bosnia and Herzegovina, n = 2, 9%); Eastern Africa (Malawi, n = 1, 5%); and South Africa (n = 1, 5%). The majority of studies were quantitative (n = 14; 64%); one study was a quasi-experiment; all others were qualitative.
Table 2. Characteristics of included studies.
| Variable | Detail | Number | % |
|---|---|---|---|
| World Bank region | Low-middle income country | 7 | 32 |
| High-income country | 15 | 68 | |
| Location | Northern America | 4 | 18 |
| Northern Europe | 6 | 27 | |
| Eastern Europe | 2 | 9 | |
| Eastern Africa | 1 | 5 | |
| Southern Africa | 1 | 5 | |
| Eastern Asia | 4 | 18 | |
| Southern Asia | 3 | 14 | |
| Australia and New Zealand | 1 | 5 | |
| Decade of publication | 1970 | 1 | 5 |
| 1980 | 2 | 9 | |
| 1990 | 1 | 5 | |
| 2000 | 6 | 27 | |
| 2010 | 12 | 55 | |
| Study design | Qualitative | 7 | 32 |
| Quantitative—Cross-sectional survey | 11 | 50 | |
| Quantitative—Case-control | 3 | 14 | |
| Quasi-experimental | 1 | 5 |
Table 3. Data extracted against study framework components.
| First author | Year | World Bank region | Country | Study Design | Disability sub-group | Disabled person (n) | Carer (n) | Main focus |
|---|---|---|---|---|---|---|---|---|
| Carnaby, S. | 2002 | HIC | UK | Qualitative | Intellectual | 0 | Number not specified in paper | Carers' KAP* |
| Charlifue, S.W. | 1992 | HIC | USA | Quantitative | Physical | 231 | 0 | Menstrual product |
| Chou, Y. C. | 2009 | HIC | Taiwan | Quantitative | Intellectual | 92 | 0 | PMS |
| Chou, Y. C. | 2012 | HIC | Taiwan | Qualitative | Intellectual | 13 | 12 | Carers' KAP |
| Patage, D.P. | 2015 | LMIC | India | Quantitative | Multiple | 198 | 0 | Menstrual product |
| Goldstein, H. | 1988 | HIC | Denmark | Quantitative | Intellectual | 15 | 0 | Menstrual cycle |
| Hamilton, A. | 2011 | HIC | USA | Quantitative | Intellectual | 124 | Number not specified in paper | PMS |
| Ibralic, I. | 2010 | LMIC | Bosnia and Herzegovina | Quantitative | Intellectual | 31 | 0 | PMS |
| Kirkham, Y. A. | 2013 | HIC | Canada | Quantitative | Multiple | 300 | Number not specified in paper | Menstrual suppression |
| Kyrkou, M. | 2005 | HIC | Australia and New Zealand | Quantitative | Intellectual | 24 | 0 | PMS |
| Lin, L. P. | 2011 | HIC | Taiwan | Quantitative | Intellectual | 0 | 1152 | Menstrual suppression |
| Lin, L. P. | 2011 | HIC | Taiwan | Quantitative | Intellectual | 0 | 1152 | Carers' KAP |
| Mason, L. | 2007 | HIC | UK | Qualitative | Intellectual | 6 | 53 | Training for disabled persons |
| Obaydi, H. | 2008 | HIC | UK | Qualitative | Intellectual | 26 | Number not specified in paper | PMS |
| Perrin, J. C. | 1976 | HIC | USA | Qualitative | Intellectual | 20 | Number not specified in paper | Menstrual suppression |
| Ranganath, P. | 2012 | LMIC | India | Quantitative | Intellectual | 0 | 10 | PMS |
| Rodgers, J. | 2005 | HIC | UK | Quantitative | Intellectual | 452 | 217 | Training for disabled persons |
| Altundağ | 2015 | LMIC | Turkey | Quasi-experimental | Intellectual | 54 | 0 | Training for disabled persons |
| Thapa, P. | 2017 | LMIC | India | Qualitative | Intellectual | 0 | 23 | Menstrual suppression |
| Van der Merwe | 1987 | LMIC | South Africa | Quantitative | Multiple | 152 | 0 | Menstrual suppression |
| van Schrojenstein Lantman-deValk | 2011 | HIC | Netherlands | Quantitative | Intellectual | 234 | 0 | Menstrual suppression |
| White, S. | 2016 | LMIC | Malawi | Qualitative | Multiple | 36 | 15 | Barriers and outcomes |
*Knowledge, attitudes and practices
Description of studies
Of the 22 studies, disabled persons were the primary research participant in the majority (n = 13; 59%), followed by the carer (n = 6; 27%), or the carer and the disabled person (n = 3; 14%) (Table 4). These participants were sourced through institutions (n = 13; 59%), such as hospitals and residential homes; households (n = 6; 27%) and households and institutions (n = 3; 14%). The means of assessing disability ranged from clinical (n = 8; 36%), self-reported (n = 4; 18%) to government lists (n = 2; 9%). Seventeen (77%) studies focused on people with intellectual impairments, followed by multiple impairments (n = 3; 14%) and physical impairments (n = 2; 9%).
Table 4. Characteristics of participants and quality assessment.
| Variable | Detail | Number | % |
|---|---|---|---|
| Primary research participants | Carer | 6 | 27 |
| Disabled person and carer | 3 | 14 | |
| Disabled person | 13 | 59 | |
|
Source of participants |
Household | 6 | 27 |
| Institution | 13 | 59 | |
| Household and institution | 3 | 14 | |
|
Means of assessing disability |
Clinical | 8 | 36 |
| Self-reported | 4 | 18 | |
| Government list | 2 | 9 | |
| Not given | 8 | 36 | |
| Disability type | Multiple | 3 | 14 |
| Intellectual | 17 | 77 | |
| Physical | 2 | 9 | |
| Quality assessment: risk of bias | Low | 13 | 59 |
| Medium | 7 | 32 | |
| High | 2 | 9 |
The quality assessment identified 13 (59%) studies as having low, seven (32%) as medium and two (9%) as high risk of bias. The main reasons for potential bias was the limitations in generalisability of results due to a small sample and response rate being lower than 70%.
Impacts of menstruation
Pre-menstrual symptoms and communication difficulties experienced by people with intellectual impairments
Nine papers (41%) covered pre-menstrual symptoms (PMS) [33–41]. Eight reported PMS symptoms and related behaviour, including menstrual cramps, mood swings, fatigue, irritability, anger, social withdrawal, decreased concentration, increased hyperactivity, self-injury and inappropriate handling of menstrual blood or hygiene products experienced by people with intellectual impairments [34–41]. Six papers assessed the frequency and severity of pain [36–41], three of which compared these between disabled and non-disabled people [37, 38, 41].
Obaydi and Puri stated that PMS was experienced by 92% of the group of people with autism, compared to 11% in the control group of non-disabled people [38]. This study had the lowest risk of bias. Kyrkou also concluded that people with Down syndrome or autism experienced higher rates of pain than the general population [37]. Due to the challenges in communicating the extent and location of pain, Kyrkou deduced this through changes in behavior [37]. However, Ibralic et al. [41] and Ranganath and Ranganath [39] contradicted this finding. Ibralic et al. reported that PMS symptoms were almost equally distributed between non-disabled people and people with an intellectual impairment [41]. Ranganath and Ranganath reported that no one with Down syndrome experienced menstrual pain or premenstrual tension, but the authors did not include an assessment of the participant’s communication abilities or factor this into the results [39]. Ranganath and Ranganath’s study was marked as having a high risk of bias [39].
Three studies investigated the severity of PMS symptoms by disability type [34, 37, 40]. All studies concluded that there is divergence within groups. Kyrkou [37] and Hamilton et al. [40] recognised that the ability to report and locate pain was a determining factor. For instance, within the intellectual impairment group, Kyrkou found that 67% (n = 8) of the research participants with Down syndrome were able to say that they were in pain or point to where they had pain, even those with limited communication abilities [37]. Only one of the nine participants on the autistic spectrum was able to point to, or state when she was in pain, even though all participants had good communication skills.
Three studies stated that the inability of some people with an intellectual impairment to understand the source of pain and communicate affected their behaviour [34, 35, 37].
"She gets short tempered. But it’s not her fault. She can’t speak very well, so I think that’s how she expresses herself” (carer from India) [35].
Concerns of carers of people with intellectual impairments
Six (27%) studies investigated the key concerns of carers who support people with intellectual impairments [34–37, 42, 43].
Carers (mothers) of people with an intellectual impairment in Thapa and Sivakami’s study in India reported that difficulties with communicating to daughters, and vice versa, were a major challenge [35]. Challenges with communication lead mothers to rely on observing changes in their daughter’s behaviour to anticipate menstruation [34]. Predictors include irritability, restlessness, crying, self-harm, decreased appetite and disruptions in sleeping patterns [34].
Other challenges reported by carers included an aversion to wearing a menstrual product, a lack of adherence to social and cultural norms, such as inappropriate handling of menstrual blood and product, talking to others about their menstruation and changing the used menstrual product in front of others [35–37, 43].
"She will leave the door open while changing her pad, and doesn’t understand that her elder brother is at home. So I tell her, ‘Always bolt this door from inside.’ Sometimes she understands, but sometimes she starts changing in front of them" (carer from India) [35]".
One of these six studies investigated professional carers’ levels of satisfaction of intimate care tasks, finding that menstrual care was the second most disliked aspect for residential staff (after giving enemas), and the most disliked aspect for day unit staff (who do not give enemas) [42].
Strategies for menstrual hygiene management
Menstrual product acceptability for people with physical impairments
Four studies (18%) investigated the menstrual product used and preference [34, 35, 44, 45]. Two of these studies considered the product used [44, 45]. One [44] explored the product acceptability from the perspective of people with spinal cord injuries, and the remaining two [34, 35] investigated the carers’ product preference. 19% of the sample in the study focusing on people with spinal cord injuries (conducted in the USA), reported discomfort and difficulty in positioning the menstrual product to ensure its maximum absorbency, as well as increasing difficulties with catheters and urinary management during menstruation [44].
Menstrual product acceptability for people with intellectual impairments
Three of the 22 studies explored the disabled person’s preference through the carer [34, 35, 43]. The studies reported that the people with an intellectual impairment often refused to wear the menstrual product, leading to stress felt by the carer and constant negotiation with the disabled person.
"My biggest problem was that she didn’t want to wear a pad. The understanding isn’t there (carer from England) [43].”
In a study, undertaken in India, mothers limited their daughter’s physical movements during menstruation so that she would not go outside with blood stained clothes [35]. Another coping mechanism applied by carers in Taiwan, was sewing the pad into the underwear or buying adult sized nappies for their daughters [34].
In two of the four studies, mothers were caring for daughters with incontinence [34, 35]. These carers felt that menstruation added another layer of complication [35], and that the cost of nappies and pads were a major concern [34]
MHM training and support for people with intellectual impairments
Five studies (23%) investigated MHM training given to people with intellectual impairments [35, 37, 43, 46, 47]. One study highlighted a lack of training and support provided to this group because carers did not believe that the individual would understand MHM information [35]. The authors hypothesised that some people with intellectual impairments refused to wear a menstrual product because they were not given any MHM information, including being shown a menstrual product, or practice wearing it prior to their first menstrual cycle. Consequently, they did not understand the purpose of a menstrual product, did not feel comfortable wearing it and associated it with menstrual cramps [35].
One of these fives studies explored the teaching on MHM provided to people with intellectual impairments in institutions [47]. It highlighted a lack of correlation between training provided and the person’s level of understanding [47]. Three studies showed positive correlations between providing MHM training to people with intellectual impairments and an increased ability to manage menstruation independently [35, 37, 46]. In Kyrkou’s study, conducted in Australia and New Zealand, people with Down syndrome who had been given MHM information prior to puberty were better able to cope with their menstrual cycle than those who were not [37]. Altundağ and Calbayram showed in their study in Turkey, that using a doll to practice changing and disposing of a used menstrual product, was an effective way to increase the MHM skills of people with intellectual impairments [46].
MHM training and support for carers
Five studies investigated the level of training and support provided to carers (professionals and mothers) on how to manage menstruation of a person with an intellectual impairment [34, 35, 42, 48, 49]. Three of these studies [42, 48, 49] focused on professional carers working in institutions and two studies on mothers at home [34, 35]. The three studies conducted in institutions highlighted limited MHM training and standards for intimate and personal care tasks; that the task’s importance was under-recognised by management; understanding of the menstruation of people with intellectual impairments was low, and support provided on menstrual issues was lower than sex education, but higher than menopause [42, 48, 49].
The mothers in the two studies focusing on care provided within the family were given no guidance, information or support on how to manage their daughter’s menstruation, leaving them feeling overwhelmed and unsupported [34]. In the Indian and Taiwanese settings, mothers believe that menstruation is a private issue so did not discuss their daughter’s menstrual cycle with anyone else, including professionals [34, 35].
Menstrual suppression
Six papers included an analysis of menstrual suppression of people with intellectual impairments [34–36, 50–52]. Menstrual suppression includes long-term contraception (i.e. oral contraceptive pill and the patch) and sterilisation (i.e. hysterectomy, tubal ligation). Two of these six studies were from the LMIC and the remaining four studies were from HICs [35, 50]. Two studies [50, 52] were published before 2000 and four after 2010 [34–36, 51].
Of these six papers, five reported that people with intellectual impairments were sterilised or on long-term contraception. Reasons for sterilisation cited by carers including a perception that menstruation care is a “burden”, a fear of unwanted pregnancies [35, 36, 50–52], difficulties related to the menstrual care tasks; the perceived lack of benefit for the person with an intellectual impairment, as well as mothers’ desire not to “burden” an older daughter with the menstrual care tasks when she is no longer able to undertake these tasks [35, 50, 52].
"I used to do everything–changing the pads every three–four hours, taking her to the toilet. But she was not aware at all; there were no feelings in her. Then when she was 16 years old, I realised that I could not do it anymore, and it was not benefitting her in anyway. Then we got her operated upon. We got her surgery done, and got her uterus removed” (carer from India) [35].
Three studies included satisfaction levels of carers post sterilisation [35, 50, 52]. All of these reported high levels of carer satisfaction. One study from Taiwan challenged this trend of menstrual suppression [34]. In this study, regular menstruation was seen as an indication of good bodily health and daughters with an intellectual impairment were given medicine to help regulate their cycles. However, almost all mothers in this study were advised by relatives and medical professionals to sterilise their daughters in order to eliminate the ‘tedious’ menstrual care, for better hygiene and to prevent unwanted pregnancies [34].
Discussion
Our search sought to identify studies exploring the MHM requirements of disabled persons, but only found 22 studies that met the inclusion criteria. The majority of studies focused on people with intellectual impairments and their carers.
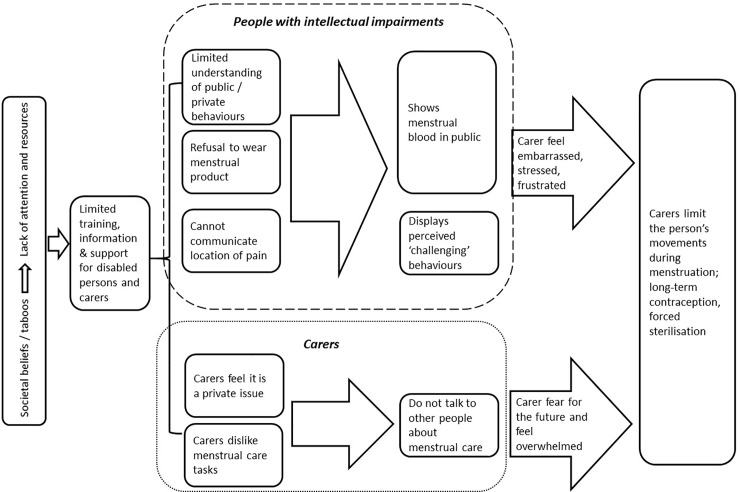
Fig 2 summarises the key findings in this review that relate to people with intellectual impairments and their carers. It shows that societal beliefs and taboos around menstruation and disability means the issue is shrouded in silence, and that it lacks attention and resources. The silence surrounding disabled people’s menstrual hygiene requirements is demonstrated by the limited number of peer reviewed studies gathered for this review. Without rigorous evidence from different contexts, it is difficult to advocate for greater attention and resourcing to meet the MHM requirements of disabled people and their carers. The subsequent dearth of MHM training, information and support tailored to meet disabled people and their carers requirements means some people struggle to manage. Strategies for MHM applied by carers include limiting the disabled person’s movements when menstruating and suppressing their menstruation.
Fig 2. Flow diagram of review findings.
The top box in Fig 2 focuses on people with intellectual impairments. This review has shown that some people with intellectual impairments do not always understand or follow social and cultural norms [35–37, 43], or wear a menstrual product [34, 35]. This group face challenges in understanding PMS and communicating when in discomfort [33–41]. Carers reported subsequent ‘menstrual behaviours’ make them feel stressed, embarrassed and they coped by not letting their daughters leave the home or sought ways to supress their menstruation [35]. The authors propose that if repetitive, accessible MHM information and training is provided regularly to the persons with intellectual impairments, they may get a deeper understanding of cultural and social norms and be better able to manage their menstruation more independently.
The bottom box in Fig 2 focuses on findings related to carers, which highlights an absence of standards and training on providing menstrual care in the institutions covered in the studies [42, 48, 49]. Findings show that professional carers dislike providing menstrual care [42]. If combined, these two factors might mean that a disabled person’s dignity and personal hygiene is compromised in these institutional settings.
The review found that MHM training and support is not provided to family members who care for daughters with intellectual impairments [34], and that mothers also dislike providing menstrual care [35, 50, 52]. Mothers reported an inability to see how menstruation benefit their daughters [35], which is intertwined with the societal belief that disabled people should not be parents or sexual beings [53]. Disability and menstruation related taboos discourages open dialogue, meaning mothers do not seek advice or support, because they view the provision of menstrual care as a private issue [34, 35].
In addition to the findings captured in Fig 2, included studies also investigated the disabled person’s preference of menstrual product [34, 35, 44, 45]. Research participants, with a physical disability, reported low levels of satisfaction with the menstrual product used (sanitary pads with and without tampons), stating that they find the products uncomfortable, difficult to place and use with catheters [44].
Implications for future research
There is limited evidence about the MHM requirements of disabled people, interventions to meet these and an assessment of their impact. This is particularly stark in LMICs, so research to investigate these topics must be carried out in these settings. Another key research gap is around the development of standardised measurements of MHM related outcomes for disabled people and their carers [54], and here the socioecological framework for MHM, adapted to include disabled persons and their carers (Table 1), could be a start. It is useful as the framework recognises MHM outcomes have individual, social and environmental influences that affect menstrual experiences and MHM among the target population.
More research is required to explore the severity of PMS experienced by disabled people compared to non-disabled people, and compared within disability groups with the view of developing mechanisms that enable disabled people to better locate and communicate pain. Finally, research on menstrual product preference and effectiveness for people with different impairments, to understand if the current products on the market are suitable and acceptable, should also be conducted.
Review strengths and limitations
To the authors’ knowledge, this is the first systematic review of the MHM requirements of disabled people and their carers. This review restricted the search to studies in the English language and the number of datasets (such as excluding the CINAHL database), so some relevant studies may have been missed. Few studies met the inclusion criteria and across those, there was no standardised measurement of outcomes, meaning an outcome assessment across the studies was difficult. For instance, only seven (32%) studies defined symptoms and practices associated with menstruation, and only 12 (55%) studies identified the means for assessing disability.
There were not enough studies with consistent methods for a meta-analysis. The authors mitigated this by using Banks et al.’s [30] quality assessment that combines the STROBE and RATS assessment tools for quantitative and qualitative studies [31, 32]. The main reasons for risk of bias are due to a sample size being smaller than 100 and the response rate being less than 70%, or not reported. This could lead to an over estimation of impacts. However, there are no great divergences between the findings in papers that have a high risk of bias and those with a medium or high risk of bias, which alleviates concerns.
Conclusion
In conclusion, limited evidence was identified on the MHM requirements of disabled people and their carers, though a number of barriers were identified. This evidence gap is important and must be filled with future research. MHM interventions that address these barriers must be developed, tested and scaled up in partnership with disabled people. If the inaction continues, disabled people’s rights will continue to be violated; they will continue to face social exclusion and potentially sterilisation.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
The authors would like to thank WaterAid for seconding the lead author to the LSHTM to carry out this research.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
Funding for this review was gratefully received from the Bill and Melinda Gates Foundation (https://www.gatesfoundation.org), Development Grant number OPP1159651, Global and Country-Level WSH Advocacy. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO, UNICEF. Progress on drinking water, sanitation and hygiene: 2017 update and SDG baselines. Geneva: 2017.
- 2.Cavill S, Roose S., Stephenson C., Wilbur J. Putting the hardest to reach at the heart of the SDGs. Petra Bongartz NVaJF, editor. UK: actical Action Publishing; 2016. [Google Scholar]
- 3.White S, Kuper H, Itimu-Phiri A, Holm R, Biran A. A qualitative study of barriers to accessing water, sanitation and hygiene for disabled people in Malawi. PLoS ONE. 2016;11 (5) (no pagination)(e0155043). 10.1371/journal.pone.0155043 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilbur J, Jones H. Disability: Making CLTS Fully Inclusive. CLTS Knowledge Hub: Institute of Development Studies; 2014. [Google Scholar]
- 5.WHO, UNICEF, JMP. Consultation on Draft Long List of Goal, Target and Indicator Options for Future Global Monitoring of Water, Sanitation and Hygiene 2012. Available from: http://www.rural-water-supply.net/en/resources/details/378.
- 6.Sahin M. Guest editorial: Tackling the stigma and gender marginalization related to menstruation via WASH in schools programmes. Waterlines. 2015;34(1):3–6. [Google Scholar]
- 7.Lobo RA, Pinkerton J. Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD). The Journal of Clinical Endocrinology & Metabolism. 2010;95(4):E1–E. 10.1210/jcem.95.4.999820534755 [DOI] [Google Scholar]
- 8.Roberts T-A, Goldenberg J, Power C, Pyszczynski T. 'Feminine protection': the effects of menstruation on attitudes towards women. Psychology of Women Quarterly. 2002;26:131–9. [Google Scholar]
- 9.Winkler I, Roaf V. Taking the bloody linen out of the closet: menstrual hygiene as a priority for achieving gender equality. Cardozo Journal of Law and Gender 2015. [Google Scholar]
- 10.House S, Mahon T, Cavill S. Menstrual Hygiene Matters; A resource for improving menstrual hygiene around the world. 2012. [Google Scholar]
- 11.Garg S, Sharma N, Sahay R. Socio-cultural aspects of menstruation in an urban slum in Delhi, India 2001. 16–25 p. [DOI] [PubMed] [Google Scholar]
- 12.Lee J. Menarche and the (Hetero) Sexualization of the Female Body. 1993. [Google Scholar]
- 13.Naeem K, Klawitter S, Aziz A. Learning, acting, and learning (LAL) research on schools’ menstrual hygiene management (MHM): Pakistan. Waterlines. 2015;34(1):104–12. [Google Scholar]
- 14.McMahon SA, Winch PJ, Caruso BA, Obure AF, Ogutu EA, Ochari IA, et al. 'The girl with her period is the one to hang her head' Reflections on menstrual management among schoolgirls in rural Kenya. BMC international health and human rights. 2011;11(1):7 10.1186/1472-698x-11-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castañeda X, García C, Langer A. Ethnography of fertility and menstruation in rural Mexico. Social Science & Medicine. 1996;42(1):133–40. 10.1016/0277-9536(95)00077-1. [DOI] [PubMed] [Google Scholar]
- 16.SHN. Z, A. S, D. JR. Menstrual hygiene and sanitation practices among adolescent school going girls: a study from a South Indian town. Int J Community Med Public Health (London). 2915;(2):189–94. [Google Scholar]
- 17.Mason L, Nyothach E, Alexander K, Odhiambo FO, Eleveld A, Vulule J, et al. ‘We Keep It Secret So No One Should Know’–A Qualitative Study to Explore Young Schoolgirls Attitudes and Experiences with Menstruation in Rural Western Kenya. PLOS ONE. 2013;8(11):e79132 10.1371/journal.pone.0079132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Juma M, Askew I, Alaii J, Bartholomew LK, van den Borne B. Cultural practices and sexual risk behaviour among adolescent orphans and non-orphans: a qualitative study on perceptions from a community in western Kenya. BMC Public Health. 2014;14(1):84 10.1186/1471-2458-14-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wamoyi J, Wight D, Plummer M, Mshana GH, Ross D. Transactional sex amongst young people in rural northern Tanzania: an ethnography of young women's motivations and negotiation. Reproductive Health. 2010;7(1):2 10.1186/1742-4755-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phillips-Howard P, Otieno G, Burmen B, Otieno F, Odongo F, Oduor C, et al. Menstrual Needs and Associations with Sexual and Reproductive Risks in Rural Kenyan Females: A Cross-Sectional Behavioral Survey Linked with HIV Prevalence 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerubo E, Laserson KF, Otecko N, Odhiambo C, Mason L, Nyothach E, et al. Prevalence of reproductive tract infections and the predictive value of girls’ symptom-based reporting: findings from a cross-sectional survey in rural western Kenya. Sexually transmitted infections. 2016;92(4):251 10.1136/sextrans-2015-052371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amornkul PN, Vandenhoudt H, Nasokho P, Odhiambo F, Mwaengo D, Hightower A, et al. HIV Prevalence and Associated Risk Factors among Individuals Aged 13–34 Years in Rural Western Kenya. PLOS ONE. 2009;4(7):e6470 10.1371/journal.pone.0006470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.UNICEF, University E. WASH in Schools Empowers Girls' Education—tools for assessing menstrual hygiene management in schools. 2013. [Google Scholar]
- 24.UN. Sustainable Development Goal 6: Ensure availability and sustainable management of water and sanitation for all 2015. Available from: https://sustainabledevelopment.un.org/sdg6. [DOI] [PMC free article] [PubMed]
- 25.OHCHR. Convention on the Rights of Persons with Disabilities 2008. [Google Scholar]
- 26.WHO, World Bank. World report on disability. 2011. [Google Scholar]
- 27.Wilbur J, Jones H, Gosling L, Groce N, Challenger E. Undoing Inequity: inclusive water, sanitation and hygiene programmes that deliver for all in Uganda and Zambia 336th WEDC International Conference; Nakuru, Kenya: WEDC; 2013. [Google Scholar]
- 28.WHO, UNFPA. Promoting sexual and reproductive health for persons with disabilities WHO/UNFPA guidance note. 2009. [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–9, w64. Epub 2009/07/23. . [DOI] [PubMed] [Google Scholar]
- 30.Banks LM, Mearkle R, Mactaggart I, Walsham M, Kuper H, Blanchet K. Disability and social protection programmes in low- and middle-income countries: a systematic review. Oxford Development Studies. 2016. [Google Scholar]
- 31.Erik von Elm MDGA, DSc; Matthias Egger, MD; Stuart J. Pocock PhD,; Peter C. Gøtzsche, MD; Jan P. Vandenbroucke, MD; for the STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Annals of Internal Medicinevol. 2007:573–7. [DOI] [PubMed] [Google Scholar]
- 32.Clark JP. How to peer review a qualitative manuscript. Books B, editor. London2003. 219–35 p.
- 33.Chou YC, Lu JZY, Pu CY. Prevalence and severity of menstrual symptoms among institutionalised women with an intellectual disability. Journal of Intellectual and Developmental Disability. 2009;34(1):36–44. 10.1080/13668250802688322 . [DOI] [PubMed] [Google Scholar]
- 34.Chou YC, Lu ZY. Caring for a daughter with intellectual disabilities in managing menstruation: a mother's perspective. Journal of intellectual & developmental disability. 2012;37(1):1–10. . [DOI] [PubMed] [Google Scholar]
- 35.Thapa P, Sivakami M. Lost in transition: menstrual experiences of intellectually disabled school-going adolescents in Delhi, India Waterlines. 2017;36(4):317–38. [Google Scholar]
- 36.Kirkham YA, Allen L, Kives S, Caccia N, Spitzer RF, Ornstein MP. Trends in menstrual concerns and suppression in adolescents with developmental disabilities. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2013;53(3):407–12. Epub 2013/06/15. 10.1016/j.jadohealth.2013.04.014 . [DOI] [PubMed] [Google Scholar]
- 37.Kyrkou M. Health issues and quality of life in women with intellectual disability. Journal of Intellectual Disability Research. 2005;49(10):770–2. . [DOI] [PubMed] [Google Scholar]
- 38.Obaydi H, Puri BK. Prevalence of premenstrual syndrome in autism: a prospective observer-rated study. The Journal of international medical research. 2008;36(2):268–72. Epub 2008/04/03. 10.1177/147323000803600208 . [DOI] [PubMed] [Google Scholar]
- 39.Ranganath P, Rajangam S. Menstrual history in women with Down Syndrome—A review. Indian Journal of Human Genetics. 2004;10(1):18–21. . [Google Scholar]
- 40.Hamilton A, Marshal MP, Murray PJ. Autism spectrum disorders and menstruation. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2011;49(4):443–5. Epub 2011/09/24. 10.1016/j.jadohealth.2011.01.015 . [DOI] [PubMed] [Google Scholar]
- 41.Ibralic I, Sinanovic O, Memisevic H. Age at menarche and premenstrual syndrome in adolescent girls with intellectual disability in Bosnia and Herzegovina. Research in Developmental Disabilities. 2010;31(3):800–3. 10.1016/j.ridd.2010.02.004 . [DOI] [PubMed] [Google Scholar]
- 42.Carnaby S, Cambridge P. Getting personal: an exploratory study of intimate and personal care provision for people with profound and multiple intellectual disabilities. Journal of intellectual disability research: JIDR. 2002;46(Pt 2):120–32. Epub 2002/03/01. . [DOI] [PubMed] [Google Scholar]
- 43.Mason LaC C. An Exploration of Issues around Menstruation for Women with Down Syndrome and their Carers. Journal of Applied Research in Intellectual Disabilities. 2007;21:257–67. [Google Scholar]
- 44.Charlifue SW, Gerhart KA, Menter RR, Whiteneck GG, Manley MS. Sexual issues of women with spinal cord injuries. Paraplegia. 1992;30(3):192–9. Epub 1992/03/01. 10.1038/sc.1992.52 . [DOI] [PubMed] [Google Scholar]
- 45.Patage DP, Sharankumar H, Bheemayya B, Ayesha N, Kiran S. Reproductive and sexual health needs among differently abled individuals in the rural field practice area of a medical college in Karnataka, India. International Journal of Medical Science and Public Health. 2015;4(7):964–8. . [Google Scholar]
- 46.Altundağ S, Cakırer Calbayram N. Teaching menstrual care skills to intellectually disabled female students. Journal of Clinical Nursing. 2016;25:1962–8. 10.1111/jocn.13215 [DOI] [PubMed] [Google Scholar]
- 47.Rodgers J, Lipscombe J. The nature and extent of help given to women with intellectual disabilities to manage menstruation. Journal of Intellectual and Developmental Disability. 2005;30(1):45–52. . [Google Scholar]
- 48.Lin LP, Lin PY, Chu CM, Lin JD. Predictors of caregiver supportive behaviors towards reproductive health care for women with intellectual disabilities. Res Dev Disabil. 2011;32(2):824–9. Epub 2010/12/21. 10.1016/j.ridd.2010.10.015 . [DOI] [PubMed] [Google Scholar]
- 49.Lin LP, Lin PY, Hsu SW, Loh CH, Lin JD, Lai CI, et al. Caregiver awareness of reproductive health issues for women with intellectual disabilities. BMC public health. 2011;11:59 10.1186/1471-2458-11-59 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Van der Merwe JV, Roux JP. Sterilization of mentally retarded persons. Obstetrical & Gynecological Survey. 1987;42(8):489–93. ; PubMed Central PMCID: PMCSource: KIE. 27486 Source: PIP. 057513 Source: POP. 00187897. [DOI] [PubMed] [Google Scholar]
- 51.van Schrojenstein Lantman-deValk HMJ, Rook F, Maaskant MA. The use of contraception by women with intellectual disabilities. Journal of Intellectual Disability Research. 2011;55:434–40 10.1111/j.1365-2788.2011.01395.x [DOI] [PubMed] [Google Scholar]
- 52.Perrin JC, Sands CR, Tinker DE, Dominguez BC, Dingle JT, Thomas MJ. A considered approach to sterilization of mentally retarded youth. American journal of diseases of children (1960). 1976;130(3):288–90. Epub 1976/03/01. . [PubMed] [Google Scholar]
- 53.Stein MA. Mommy has a blue wheelchair—recognising the rights of persons with disabilities. 1994. [Google Scholar]
- 54.Moore G, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ (Clinical research ed). 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.