Abstract
Objective
Arm injuries in baseball players are a common problem. The identification of modifiable risk factors, including range of motion (ROM), is essential for injury prevention. The purpose of this review was to assess the methodologic quality and level of evidence in the literature and to investigate the relationship between shoulder ROM and the risk of arm injuries in baseball players.
Data Sources
Relevant studies in PubMed, CINAHL, Embase, and SPORTDiscus published from inception to August 1, 2017.
Study Selection
Only studies that encompassed healthy baseball cohorts who were assessed for shoulder ROM and prospectively evaluated for injuries throughout a baseball season or seasons were included.
Data Extraction
Six articles met the search criteria. Only 3 studies were included in the meta-analysis due to disparate participant groups.
Data Synthesis
The modified Downs and Black scale (0–15 points) was used to analyze methodologic quality. Study quality ranged from 11 to 14. Four studies received high-quality (≥12) and 2 studies received moderate-quality (≥10) scores. The overall pooled analysis demonstrated that absolute and internal-rotation deficits (–5.93 [95% confidence interval {CI} = –9.43, –2.43], P < .001 and 4.28 [0.71, 7.86], P = .02, respectively) and absolute total ROM (TROM; –6.19 [95% CI = –10.28, –2.10]; P = .003) were predictors of injury, and these data exhibited homogeneity (absolute IR P value = .77, I2 = 0%; IR deficit P value = .41, I2 = 0%; absolute TROM P value = .78, I2 = 0%). No significance was observed for absolute external rotation (–2.86 [95% CI = –6.56, 0.83], P = .13), which had data with high heterogeneity (P = .003; I2 = 83%). A deficit in horizontal adduction was a predictor of injury (–8.32 [95% CI = –12.08, –4.56]; P < .001); these data were homogeneous but yielded a moderate heterogenic effect (P = .16; I2 = 50%).
Conclusions
High-quality evidence demonstrated that deficits in throwing-arm TROM and IR were associated with upper extremity injury in baseball players. Heterogeneity across studies for horizontal adduction suggested that this may be a modifiable risk factor for injury, but it requires further research.
Keywords: glenohumeral internal-rotation deficit, posterior shoulder tightness, pitching, retrotorsion
Upper extremity injuries in baseball players are a persistent and significant problem. Such injuries are common,1–3 and injury rates are increasing.4 In the last decade, the injury rates of high school, collegiate, and professional baseball players were 4.0, 5.8, and 3.61, respectively, per 1000 athlete-exposures, with the greatest incidence of injury at the shoulder and elbow.1–3 These injuries can be attributed to increases in overall playing volume5 and changes in shoulder range of motion (ROM)6 among other factors. As a result, clinicians have investigated shoulder ROM with the aims of understanding and predicting upper extremity injuries in baseball athletes.7
Throwing is a complex and high-demand movement that produces high segmental velocities and joint forces,8 with the highest proportion of forces occurring in the upper extremity.9–12 Previous researchers13–20 proposed that pitching forces can affect the osseous and soft tissue structures of the upper extremity. The large stresses caused by external-rotation (ER) torque during the pitching motion could induce adaptations in the humeral epiphyseal cartilage, orienting it to a more posterior and medial position.15,17 Due to throwing-shoulder structural alterations,13–15,21 some ROM differences between the throwing and nonthrowing limbs are necessary adaptations in high-level throwers.22 Although long-term, osseous, throwing-specific ROM adaptations occur,13–15,22 short-term soft tissue ROM changes have also been observed18,19,23 and have demonstrated disparate results in terms of upper extremity injuries.18,23 Given the multiple factors that affect shoulder ROM13–15,18,22,23 and differing conclusions concerning shoulder ROM changes,18,23 shoulder ROM changes have many confounding factors and are poorly understood.
Soft tissue pitching adaptations can be modified through specific interventions.24–26 The sleeper stretch reduced shoulder ROM recovery time compared with time alone.25 Instrumented soft tissue mobilization combined with self-stretching decreased shoulder ROM risk factors compared with self-stretching alone in baseball players.26 Due to the heterogeneity of studies investigating the association between shoulder ROM and injury in baseball players18,27 as well as the ability to effect soft tissue ROM adaptations through specific interventions,24–26 we need to investigate and summarize the evidence.
Shoulder injuries in baseball continue to be a significant problem for athletes, coaches, parents, and sports medicine providers.1–4 The identification of modifiable risk factors, including ROM, is essential for injury prevention.1,7 Several groups1,5,7,18,27 have prospectively examined modifiable risk factors for upper extremity injuries, but varied results made it unclear if shoulder ROM was a risk factor for upper extremity injury. This has limited the development and integration of effective upper extremity injury-prevention strategies for baseball players. Therefore, the purpose of our systematic review and meta-analysis was to critically assess the methodologic quality and level of evidence in the literature and to investigate the relationship between shoulder ROM and the risk of upper extremity injuries in baseball players. We anticipated that this systematic review would provide clinicians with evidence-based insights that could be used to develop and integrate injury-prevention strategies.24,25
METHODS
Study Design
To investigate the hypothesis, we performed a systematic and comprehensive literature review on the correlation between shoulder ROM and upper extremity injury among baseball players. After an initial search, we used the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines to evaluate and assess the study methods.28 This review was prospectively registered with Prospero (CRD42017060786) after completion of the preliminary search and the initiation of formal screening.
Search Strategy
A systematic, computerized search of the literature in PubMed, CINAHL, Embase, and SPORTDiscus was conducted by a medical research librarian (L.L.) using a controlled vocabulary and key words related to shoulder anatomy and ROM. This coauthor did not participate in the screening, full-text review, or data abstraction. Our search time frame was from database inception to August 1, 2017. The search strategies are shown in the Appendix. The reference lists of all selected publications were checked to retrieve relevant publications that were not identified in the computerized search. References in screened and included articles, abstracts, and available conference proceedings (including abstracts, posters, and publications) were also hand searched by 1 author (G.S.B.). To identify relevant articles, 2 reviewers (G.S.B., M.S.F.) independently screened the titles and abstracts of all identified citations. Full-text articles were retrieved if the abstract provided insufficient information to establish eligibility or if the article passed the first eligibility screening.
Inclusion and Exclusion Criteria
We inspected identified articles to determine if they met the following inclusion and exclusion criteria. The inclusion criteria were baseball players aged 13 years or older at any competition level (professional, college, high school or middle school, or amateur). Shoulder ROM (internal rotation [IR], total ROM [TROM], external rotation [ER], or horizontal adduction [HA]) had to be assessed in either the supine or prone position. Study prerequisites were healthy cohorts who were tracked prospectively or retrospectively for injury and full-text articles that were published in a peer-reviewed journal. Each study was required to include injury incidence or injury rate. Exclusion criteria consisted of cross-sectional studies that compared healthy participants and those who were in pain or injured, case studies, papers written in a language other than English, shoulder ROM measurements not taken in the prone or supine position, participation in a sport other than baseball, or any study that lacked injury data.
Study Selection
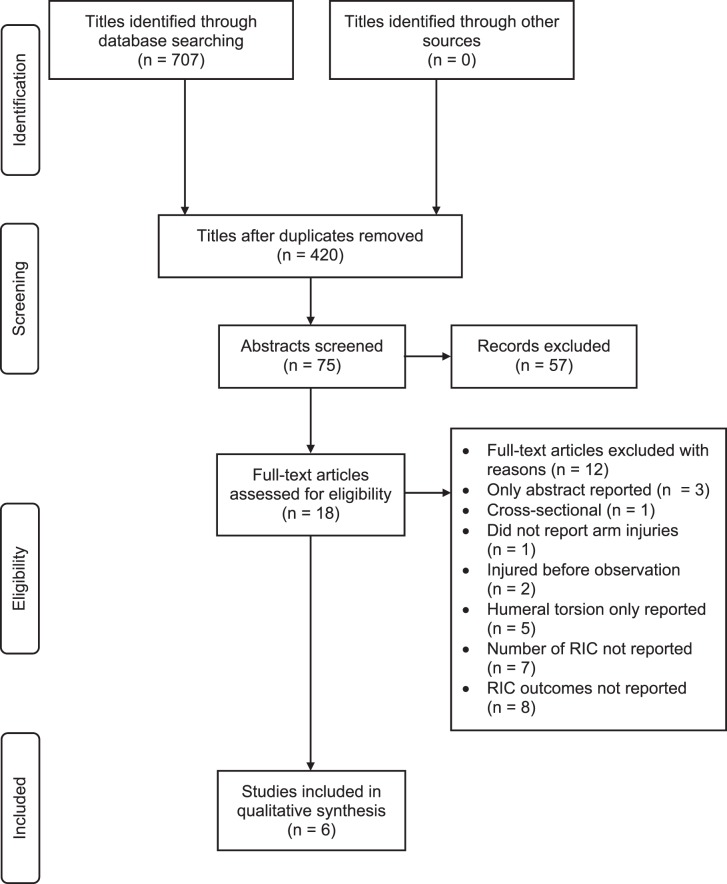
Two reviewers (G.S.B., M.S.F.) assessed the titles and abstracts for adherence to the inclusion and exclusion criteria. Full-text documents identified by either reviewer as possibly applicable were then held for further examination (Figure 1). In case of disagreement between the 2 reviewers, a third reviewer (T.C.S.) was asked to resolve the discrepancy.
Figure 1.
PRISMA flow diagram. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Quality Assessment
Two reviewers (G.S.B., M.S.F.) independently performed quality assessment using a modified Downs and Black scale.28 This scale has been established as a reliable tool (test-retest r = 0.88; interrater r = 0.75) for case-control and cohort studies.28 The modified version is scored from 0 to 15. Any disputes about methodologic quality were debated between the 2 reviewers. If a consensus could not be reached, a third author (T.C.S.) resolved the disagreement.
Data Extraction
Data were extracted by 1 reviewer (G.S.B.) and input into a database by a second reviewer (M.S.F.). Disputes concerning the study inclusion and exclusion criteria were resolved through deliberation between the 2 reviewers. If the dispute could not be solved, a third reviewer (T.C.S.) arbitrated the disagreement to achieve a consensus. Data elements were sample size; competition level; injury rates; reinjury rates; shoulder IR, ER, TROM, and HA; quality characteristics; athletes' demographic characteristics (ie, age and handedness); and level of evidence.
Meta-Analysis
Injured and uninjured group differences for absolute shoulder ROM and throwing- versus nonthrowing-shoulder ROM deficits for IR, ER, and TROM were incorporated into the meta-analysis. Injured and uninjured group differences for HA were assessed solely for absolute ROM due to a lack of data reporting for throwing- versus nonthrowing-shoulder ROM deficits. Participants were divided into groups by comparing the injured versus the uninjured,1,7,18 those with values 1 standard deviation above or below sample normative values,27 or previously established passive ROM measurements.6,29 Due to the disparate data groupings in the included investigations, only 3 studies1,7,18 that compared injured versus noninjured participants were considered in the meta-analysis. Furthermore, authors of the 3 studies that were not included in the meta-analysis did not report shoulder ROM values but instead provided the number of participants in each group. As a result, it was not possible to determine the shoulder ROM means or standard deviations for each individual or group or to include these studies in the meta-analysis. A χ2 test and a pooled 95% confidence interval (CI) for studies that analyzed shoulder ROM as a continuous variable were calculated. Random-effects models with inverse variance weighting were used for all analyses. Heterogeneity was assessed using the Cochrane Q and I2; high heterogeneity was determined by a Q P value < .10 and I2 > 50%. Analyses were performed in Review Manager (version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
RESULTS
A total of 707 studies were identified in an initial exploration of database and reference searches. After duplicates were removed (n = 287), 420 titles were screened. Eligibility for inclusion was assessed in 75 abstracts, and 18 studies were evaluated via full-text review. Six studies were included in the quality assessment and analysis (n = 1056 participants).
Study Quality Assessment
All 6 studies reviewed1,6,7,18,27,29 were prospective; therefore, all provided level 2b evidence (Table 1).30 Study quality scores (modified Downs and Black scale28) ranged from 11 to 14 out of a maximum of 15. Comparison groups were included in all 6 studies. The authors of all 6 studies compared throwing with nonthrowing arms.1,6,7,18,27,29 Three sets of authors1,7,18 blinded examiners to the participant's throwing arm. One group27 considered confounding variables (eg, pitch count) in the data analysis. Lastly, investigators in 3 studies1,18,27 calculated sample size a priori, and only 2 studies18,27 had sufficient power (Table 2).
Table 1.
Study Demographics and Design
| Article |
No. of Participants |
Age, y (Mean ± SD) |
Competition Level(s) |
No. of Seasons Followed |
Participant Grouping Methodology |
Injury Definition |
Range-of-Motion Correlation to Injury, P Value |
| Shanley et al1 (2011) | 143 | 15.8 ± 1.3 (range, 13–18) | High school | 1 | Injured versus uninjured | >7 d missed in baseball activities | IR = .04a |
| ER = .25 | |||||||
| Total = .05 | |||||||
| HA = .01a | |||||||
| Shanley et al7 (2015) | 115 | 14.9 ± 1.2 (range, 13–19) | High school | 1 | Injured versus uninjured | >7 d missed in baseball activities | IR = .06 |
| ER = .50 | |||||||
| Total = .32 | |||||||
| HA = .005a | |||||||
| Shitara et al18 (2017) | 78 | 16.3 ± 0.6 | High school | 1 | Injured versus uninjured | >7 d missed in baseball activities | IR = .02a |
| ER: not given | |||||||
| Total = .04a | |||||||
| Tyler et al27 (2014) | 101 | Not given | High school | 4 | Above, normal, or below 1 standard deviation for mean range of motion | 1 missed game or practice | IR = .03a |
| ER = .35 | |||||||
| Total = .56 | |||||||
| HA = .21 | |||||||
| Wilk et al29 (2014) | 296 | 24.7 ± 4.1 | Professional (Major League Baseball and Minor League Baseball) | 8 | Previously determined injury cut points | Disabled list | IR = .55 |
| ER = .32 | |||||||
| Total = .007a | |||||||
| Flexion = .008a | |||||||
| Wilk et al6 (2015) | 296 | 24.7 ± 3.9 | Professional (Major League Baseball and Minor League Baseball) | 8 | Previously determined injury cut points | Disabled list | IR = .20 |
| ER = .01a | |||||||
| Total = .21 | |||||||
| Flexion = .20 |
Abbreviations: ER, external rotation; HA, horizontal adduction; IR, internal rotation.
Indicates difference (P < .05).
Table 2.
Methodologic Quality Scores of Included Studies (Modified Downs and Black Scale)
| Study |
Item No. |
Total Score |
||||||||||||||
| 1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
11 |
12 |
13 |
14 |
15 |
||
| Shitara et al18 (2017) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 14 |
| Shanley et al1 (2011) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 13 |
| Tyler et al27 (2014) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 13 |
| Shanley et al7 (2015) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 12 |
| Wilk et al29 (2014) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 11 |
| Wilk et al6 (2015) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 11 |
Shoulder ROM Assessments
Three sets of authors1,7,18 analyzed shoulder ROM as a continuous variable, whereas 1 group27 categorized participants by shoulder ROM into ordinal groups (1 standard deviation above or below the mean); the other 2 sets of researchers6,29 used shoulder ROM as a nominal risk factor variable, as established from previous studies. All 6 groups1,6,7,18,27,29 measured IR, ER, and TROM, whereas 3 sets of investigators1,7,27 measured HA, and 2 sets of authors6,29 measured shoulder flexion.
Meta-Analysis
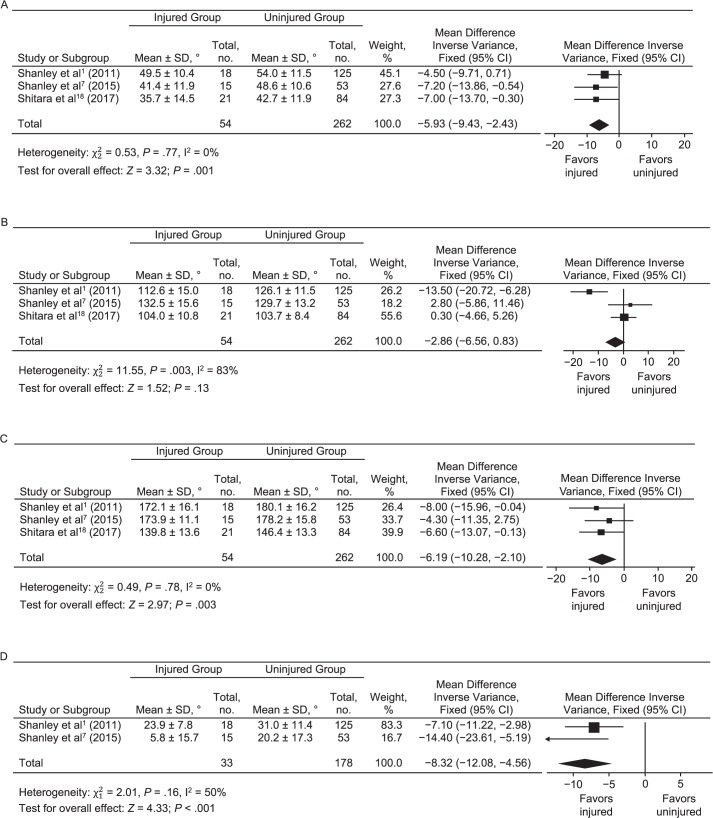
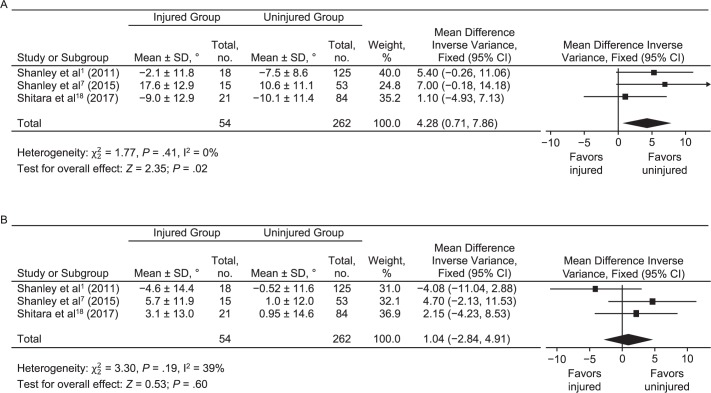
We analyzed the absolute shoulder ROM pooled variance for IR, ER, and TROM from 3 studies1,7,18 and HA from 2 studies.1,7 The pooled ROM bilateral deficit was assessed for IR1,7,18 and TROM.1,7,18 The overall pooled assessment demonstrated that the absolute shoulder IR ROM was a predictor of injury (P < .001; –5.93 [95% CI = –9.43, –2.43]) that exhibited homogeneity (P = .77; I2 = 0%; Figure 2).1,7,18 The IR shoulder ROM pooled bilateral deficit was a predictor of injury (P = .02; 4.28 [95% CI = 0.71, 7.86]) that had homogeneous data (P = .41; I2 = 0%; Figure 3).1,7,18 The overall pooled assessment for absolute shoulder TROM was a predictor of injury (P = .003; –6.19 [95% CI = –10.28, –2.10]) that had homogeneous data (P =.78; I2 = 0%; Figure 2).1,7,18 The shoulder TROM pooled bilateral deficit was not a predictor of injury (P = .60; 1.04 [95% CI = –2.84, 4.91]); the data were homogeneous, with a moderate heterogeneous effect (P = .19; I2 = 39%; Figure 3).1,7,18 The overall pooled assessment for absolute shoulder ER ROM was not a predictor of injury (P = .13; –2.86 [95% CI = –6.56, 0.83]), which had highly heterogeneous data (P = .003; I2 = 83%; Figure 2).1,7,18 The overall pooled assessment for absolute shoulder HA was a predictor of injury (P < .001; –8.32 [95% CI = –12.08, –4.56]); the data were homogeneous, with a moderate heterogenic effect (P = .16; I2 = 50%; Figure 2).1,7
Figure 2.
Pooled proportion for absolute shoulder range of motion. A, Internal rotation. B, External rotation. C, Total range of motion. D, Horizontal adduction. Abbreviation: CI, confidence interval.
Figure 3.
Pooled proportion for shoulder range-of-motion deficit. A, Internal rotation. B, Total range of motion. Abbreviation: CI, confidence interval.
DISCUSSION
The purpose of this systematic review was to evaluate the methodologic quality and level of evidence in the literature and to investigate the relationship between shoulder ROM and the risk of upper extremity injuries among baseball players. A total of 6 articles met the inclusion criteria for the review. We found that absolute shoulder IR and TROM and the throwing versus nonthrowing upper extremity deficit were associated with time-loss upper extremity injuries. The meta-analysis revealed absolute shoulder IR and TROM less than 44° and 160° and side-to-side deficits in excess of 5° and 8,° respectively, which should be considered when designing upper extremity injury-prevention programs. These values should be measured as part of baseline injury and return-to-sport screening in an effort to decrease the upper extremity injury risk.
All 6 groups1,6,7,18,27,29 used prospective cohort designs, and their study scores ranged from 11 to 15 on the modified Downs and Black scale.28 Investigators were blinded in only 3 studies,1,7,18 indicating that the other studies may have had potential investigator bias. Only 1 group27 accounted for a confounding variable: pitch count, which has been associated with fatigue and pain.5,31 Furthermore, the number of pitches and pitch types thrown during a game and over a season were associated with pain.5 Finally, only 3 sets of authors quantified power a priori,1,18,27 and only 2 had sufficient samples.18,27 This shows that the majority of studies lacked ample sample size to adequately compare shoulder ROM and injuries.
Our pooled analysis demonstrated that absolute IR <44° and side-to-side dominant-shoulder deficit >5° indicated a greater risk of arm injury. Decreased IR has been associated with posterior shoulder tightness and increased humeral retrotorsion.32,33 Pitchers with internal impingement developed greater posterior shoulder tightness (deficits in HA and IR) than healthy pitchers.32 In addition, increased posterior shoulder tightness may affect the biomechanics by increasing the subacromial contact pressure and contact area during pitching.34 The increased contact pressure and greater contact area may contribute to the risk of rotator cuff injury during pitching.34
The studies not included in the meta-analysis had conflicting results. Tyler et al27 observed an injury incidence of 1.14/1000 pitches for the below-normative mean, whereas Wilk et al6,29 did not detect a relationship between shoulder IR ROM deficit and injury. This disparity may have been because their participants were professional pitchers rather than adolescent amateur athletes. Previous authors35,36 have observed that athletes at higher competition levels have greater proficiency in fundamental movements. Also, pitchers at higher competition levels may receive more specifically tailored screening for shoulder IR ROM discrepancies.
Our pooled results further showed that absolute TROM <160° and side-to-side deficits >10° increased the arm injury risk. During the pitching motion, the greatest degree of ER occurs during the late-cocking phase.37 The extreme ER is followed by an acute acceleration and subsequent IR torque, increasing the susceptibility to injury.8 Other researchers38 detected that a decrease in TROM correlated with a decrease in IR ROM. As stated earlier, IR has been shown to be a factor in pitching injuries.1,7,18,27 This highlights the fact that TROM may also be a risk factor in upper extremity injuries among baseball players.
Interestingly, shoulder ER was not related to upper extremity injury. This supports previous retrospective and cross-sectional studies.39,40 In all of the studies included in the meta-analysis, ER for total and increased ROM was analyzed.1,7,18 However, a deficit in ER ROM was associated with injury in 1 study6 that was not included in the meta-analysis. Pitchers who had less than 5° greater ER in their throwing versus nonthrowing shoulder were more likely to incur an upper extremity injury.6 It has been hypothesized22 that some ROM changes between the throwing and nonthrowing limbs are a necessary adaptation in high-level throwers. Previous authors41,42 have described an inverse relationship between humeral retrotorsion and shoulder injuries in overhead athletes. These findings suggest that humeral retrotorsion offers protection to the shoulder joint in overhead throwers.6,41,42 Furthermore, humeral retrotorsion explained 24% of the difference in ER and 16% of the difference in IR between limbs.43 Thus, while screening for the risk of arm injury, measuring ER alone may not be sufficient; further inquiry into the relationship between ER and humeral retrotorsion as well as pitching development is needed.
Absolute shoulder HA had a statistically significant correlation with injury. However, the effect was heterogeneous, which reflects the data inconsistencies. The discrepancy within the meta-analysis may be due to the smaller samples that were assessed for HA: only 2 groups1,7 assessed HA. Other researchers27 assessed HA but did not find any association with injury. Loss of shoulder HA ROM has been postulated to be due primarily to shoulder capsule and rotator cuff decrements, which hinder humeral head translation during pitching and cause subsequent injury.44 In other studies,32,45 decreased HA with shoulder impingement symptoms was noted. Although decreased HA ROM has been associated with shoulder injury in individual studies, data discrepancies mean that the current evidence is insufficient to support this relationship.
Of the 2 sets of authors6,29 who measured shoulder flexion, one29 found a relationship only with elbow injuries in professional pitchers. The authors hypothesized that this relationship may have been due to decreased tissue flexibility, specifically within the latissimus dorsi,29 which is highly active during pitching.46 The greatest latissimus dorsi electromyography activity occurs during the late-cocking and acceleration phases of pitching, with the highest power generation during the latter.46 Due to the latissimus dorsi's contribution to pitching power production, decreased flexibility could correlate with a deficit in shoulder flexion, a measurement that may be clinically important.
These summary results should be considered in light of the limitations of the available studies. Only English-language articles were used in this review, which is a publication bias, and only American baseball players were investigated. As a result, these data cannot be generalized to other countries or cultures. Most investigators followed the athletes for only 1 season. Little is known about how changes in shoulder ROM over multiple years affect injury rates. Shanley et al19 observed that shoulder ROM in professional pitchers changed over the course of 2 seasons. These findings suggest that shoulder ROM alters over time; however, to date, no researchers have looked at the effects of these changes on upper extremity injuries. Most authors assessed athletes at only 1 competition level, the majority of whom were adolescents. Pitchers at higher competition levels throw at greater velocities and play more games in a season compared with those at lower competition levels.47,48 Furthermore, the studies we reviewed included players from young adolescents to professionals. Due to the physical differences among the varying age ranges, these findings should not be considered ubiquitous for all baseball player ages and competition levels. Understanding age- and competition-level normative data for shoulder ROM may be beneficial in elucidating specific athletes' prophylactic needs. Finally, the cut-off values of 5° and 8° were statistically significant in the larger samples and our pooled analysis. However, it is likely that 10° of IR and 15° of TROM are the smallest changes that can be measured clinically.49 Clinicians should carefully consider their ROM assessment techniques to optimize the meaningfulness of their measures. Given that the purpose of screening is to identify athletes who may be at risk and to provide relatively simple, noninvasive, effective stretching interventions, smaller cut-offs may be considered.
In summary, the moderate to high methodologic scores demonstrated that a relationship was present between IR and TROM and upper extremity injury in baseball pitchers. Overall, ER did not have a significant correlation with injury; however, 1 group6 observed that a deficit in ER ROM was associated with injury. Although HA and shoulder flexion ROM were associated with injury, an association between HA and shoulder flexion and injury cannot be claimed because of data heterogeneity and low sampling power. Future research is necessary to confirm these results in larger prospective studies. Also, more work is required to understand the effect of multiple years of shoulder ROM changes in relation to injury and normative shoulder ROM data for athletes at different competition levels. This systematic review and meta-analysis demonstrated important relationships between shoulder ROM and the future risk of upper extremity injury. These data provide the foundation for screening tools and the design of individualized or team-based injury-prevention programs.
Appendix. Search Strategy: PubMed
With All Studies Filter
(“shoulder”[MeSH Terms] OR “shoulder”[tiab] OR Glenohumeral[tiab] OR “Shoulder Injuries”[Mesh] OR “Shoulder Joint”[Mesh] OR “Scapula”[Mesh]) AND (“range of motion, articular”[MeSH Terms] OR “range of motion”[tiab] OR “External rotation”[tiab] OR “internal rotation”[tiab] OR “horizontal adduction”[tiab] OR “joint motion”[tiab]) AND (“baseball”[MeSH Terms] OR “baseball”[tiab] OR pitcher[tiab] OR pitchers[tiab])) AND (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR randomised[tiab] OR randomization[tiab] OR randomisation[tiab] OR placebo[tiab] OR drug therapy[sh] OR randomly[tiab] OR trial[tiab] OR groups[tiab] OR Clinical trial[pt] OR “clinical trial”[tiab] OR “clinical trials”[tiab] OR “evaluation studies”[Publication Type] OR “evaluation studies as topic”[MeSH Terms] OR “evaluation study”[tiab] OR evaluation studies[tiab] OR “intervention studies”[tiab] OR “intervention study”[tiab] OR “intervention studies”[tiab] OR “case-control studies”[MeSH Terms] OR “case-control”[tiab] OR “cohort studies”[MeSH Terms] OR cohort[tiab] OR “longitudinal studies”[MeSH Terms] OR “longitudinal”[tiab] OR longitudinally[tiab] OR “prospective”[tiab] OR prospectively[tiab] OR “retrospective studies”[MeSH Terms] OR “retrospective”[tiab] OR “follow up”[tiab] OR “comparative study”[Publication Type] OR “comparative study”[tiab] OR systematic[subset] OR “meta-analysis”[Publication Type] OR “meta-analysis as topic”[MeSH Terms] OR “meta-analysis”[tiab] OR “meta-analyses”[tiab]) NOT (Editorial[ptyp] OR Letter[ptyp] OR Case Reports[ptyp] OR Comment[ptyp]) NOT (animals[mh] NOT humans[mh])
Embase
(‘shoulder'/de OR shoulder:ab,ti OR glenohumeral:ab,ti OR ‘shoulder injury'/de OR ‘scapula'/de OR scapula:ab,ti) AND (‘joint characteristics and functions'/de OR ‘range of motion'/de OR ‘range of motion':ab,ti OR ‘joint motion':ab,ti OR ‘external rotation':ab,ti OR ‘joint mobility'/de OR ‘internal rotation'/de OR ‘horizontal adduction':ab,ti) AND (‘baseball'/de OR baseball:ab,ti OR pitcher:ab,ti OR pitchers:ab,ti) AND ([article]/lim OR [article in press]/lim OR [conference abstract]/lim OR [conference paper]/lim OR [review]/lim OR [short survey]/lim) AND [humans]/lim AND [english]/lim AND [embase]/lim
CINAHL
Limiters: Research Article; English Language; Peer Reviewed
((MH “Shoulder”) OR “shoulder” OR (MH “Shoulder Injuries+”) OR (MH “Shoulder Joint+”) OR (MH “Scapula+”) OR “scapula”) AND ((MH “Range of Motion”) OR “range of motion” OR “External rotation” OR “internal rotation” OR “horizontal adduction” OR “joint motion”) AND ((MH “Baseball”) OR “baseball” OR pitcher OR pitchers)
SPORTDiscus
(DE “SHOULDER” OR DE “SHOULDER joint” OR shoulder OR DE “SCAPULA”) AND (DE “JOINTS (Anatomy) – Range of motion” OR OR “range of motion” OR “External rotation” OR “internal rotation” OR “horizontal adduction” OR “joint motion”) AND (DE “BASEBALL” OR OR pitcher OR pitchers)
REFERENCES
- 1.Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med. 2011;39(9):1997–2006. doi: 10.1177/0363546511408876. [DOI] [PubMed] [Google Scholar]
- 2.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 3.Posner M, Cameron KL, Wolf JM, Belmont PJ, Jr, Owens BD. Epidemiology of Major League Baseball injuries. Am J Sports Med. 2011;39(8):1676–1680. doi: 10.1177/0363546511411700. [DOI] [PubMed] [Google Scholar]
- 4.Conte S, Camp CL, Dines JS. Injury trends in Major League Baseball over 18 seasons: 1998–2015. Am J Orthop (Belle Mead NJ) 2016;45(3):116–123. [PubMed] [Google Scholar]
- 5.Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–1810. doi: 10.1097/00005768-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of shoulder injury in professional baseball pitchers: a prospective study. Am J Sports Med. 2015;43(10):2379–2385. doi: 10.1177/0363546515594380. [DOI] [PubMed] [Google Scholar]
- 7.Shanley E, Kissenberth MJ, Thigpen CA, et al. Preseason shoulder range of motion screening as a predictor of injury among youth and adolescent baseball pitchers. J Shoulder Elbow Surg. 2015;24(7):1005–1013. doi: 10.1016/j.jse.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Fleisig GS, Barrentine SW, Escamilla RF, Andrews JR. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21(6):421–437. doi: 10.2165/00007256-199621060-00004. [DOI] [PubMed] [Google Scholar]
- 9.Fleisig GS, Escamilla RF, Andrews JR, Matsuo T, Satterwhite Y, Barrentine SW. Kinematic and kinetic comparison between baseball pitching and football passing. J Appl Biomech. 1996;12(2):207–224. [Google Scholar]
- 10.Aguinaldo AL, Chambers H. Correlation of throwing mechanics with elbow valgus load in adult baseball pitchers. Am J Sports Med. 2009;37(10):2043–2048. doi: 10.1177/0363546509336721. [DOI] [PubMed] [Google Scholar]
- 11.Oyama S, Yu B, Blackburn JT, Padua DA, Li L, Myers JB. Improper trunk rotation sequence is associated with increased maximal shoulder external rotation angle and shoulder joint force in high school baseball pitchers. Am J Sports Med. 2014;42(9):2089–2094. doi: 10.1177/0363546514536871. [DOI] [PubMed] [Google Scholar]
- 12.Anz AW, Bushnell BD, Griffin LP, Noonan TJ, Torry MR, Hawkins RJ. Correlation of torque and elbow injury in professional baseball pitchers. Am J Sports Med. 2010;38(7):1368–1374. doi: 10.1177/0363546510363402. [DOI] [PubMed] [Google Scholar]
- 13.Chant CB, Litchfield R, Griffin S, Thain LMF. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther. 2007;37(9):514–520. doi: 10.2519/jospt.2007.2449. [DOI] [PubMed] [Google Scholar]
- 14.Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- 15.Greenberg EM, Fernandez-Fernandez A, Lawrence JT, McClure P. The development of humeral retrotorsion and its relationship to throwing sports. Sports Health. 2015;7(6):489–496. doi: 10.1177/1941738115608830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carter DR. Mechanical loading history and skeletal biology. J Biomech. 1987;20(11–12):1095–1109. doi: 10.1016/0021-9290(87)90027-3. [DOI] [PubMed] [Google Scholar]
- 17.Sabick MB, Kim Y-K, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005;33(11):1716–1722. doi: 10.1177/0363546505275347. [DOI] [PubMed] [Google Scholar]
- 18.Shitara H, Kobayashi T, Yamamoto A, et al. Prospective multifactorial analysis of preseason risk factors for shoulder and elbow injuries in high school baseball pitchers. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3303–3310. doi: 10.1007/s00167-015-3731-4. [DOI] [PubMed] [Google Scholar]
- 19.Shanley E, Thigpen CA, Clark JC, et al. Changes in passive range of motion and development of glenohumeral internal rotation deficit (GIRD) in the professional pitching shoulder between spring training in two consecutive years. J Shoulder Elbow Surg. 2012;21(11):1605–1612. doi: 10.1016/j.jse.2011.11.035. [DOI] [PubMed] [Google Scholar]
- 20.Reinold MM, Wilk KE, Macrina LC, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36(3):523–527. doi: 10.1177/0363546507308935. [DOI] [PubMed] [Google Scholar]
- 21.Greenberg EM, Lawrence JT, Fernandez-Fernandez A, McClure P. Humeral retrotorsion and glenohumeral motion in youth baseball players compared with age-matched nonthrowing athletes. Am J Sports Med. 2017;45(2):454–461. doi: 10.1177/0363546516676075. [DOI] [PubMed] [Google Scholar]
- 22.Wyland DJ, Pill SG, Shanley E, et al. Bony adaptation of the proximal humerus and glenoid correlate within the throwing shoulder of professional baseball pitchers. Am J Sports Med. 2012;40(8):1858–1862. doi: 10.1177/0363546512452720. [DOI] [PubMed] [Google Scholar]
- 23.Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39(2):329–335. doi: 10.1177/0363546510384223. [DOI] [PubMed] [Google Scholar]
- 24.Bailey LB, Shanley E, Hawkins R, et al. Mechanisms of shoulder range of motion deficits in asymptomatic baseball players. Am J Sports Med. 2015;43(11):2783–2793. doi: 10.1177/0363546515602446. [DOI] [PubMed] [Google Scholar]
- 25.Reuther KE, Larsen R, Kuhn PD, Kelly JD IV, Thomas SJ. Sleeper stretch accelerates recovery of glenohumeral internal rotation after pitching. J Shoulder Elbow Surg. 2016;25(12):1925–1929. doi: 10.1016/j.jse.2016.07.075. [DOI] [PubMed] [Google Scholar]
- 26.Bailey LB, Thigpen CA, Hawkins RJ, Beattie PF, Shanley E. Effectiveness of manual therapy and stretching for baseball players with shoulder range of motion deficits. Sports Health. 2017;9(3):230–237. doi: 10.1177/1941738117702835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tyler TF, Mullaney MJ, Mirabella MR, Nicholas SJ, McHugh MP. Risk factors for shoulder and elbow injuries in high school baseball pitchers: the role of preseason strength and range of motion. Am J Sports Med. 2014;42(8):1993–1999. doi: 10.1177/0363546514535070. [DOI] [PubMed] [Google Scholar]
- 28.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. Am J Sports Med. 2014;42(9):2075–2081. doi: 10.1177/0363546514538391. [DOI] [PubMed] [Google Scholar]
- 30.Oxford Centre for Evidence-based Medicine. Levels of Evidence (March 2009) CEBM Web site. http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ Accessed January 15, 2017.
- 31.Grantham WJ, Byram IR, Meadows MC, Ahmad CS. The impact of fatigue on the kinematics of collegiate baseball pitchers. Orthop J Sports Med. 2014;2(6):2325967114537032. doi: 10.1177/2325967114537032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34(3):385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 33.Myers JB, Oyama S, Goerger BM, Rucinski TJ, Blackburn JT, Creighton RA. Influence of humeral torsion on interpretation of posterior shoulder tightness measures in overhead athletes. Clin J Sport Med. 2009;19(5):366–371. doi: 10.1097/JSM.0b013e3181b544f6. [DOI] [PubMed] [Google Scholar]
- 34.Muraki T, Yamamoto N, Zhao KD, et al. Effect of posteroinferior capsule tightness on contact pressure and area beneath the coracoacromial arch during pitching motion. Am J Sports Med. 2010;38(3):600–607. doi: 10.1177/0363546509350074. [DOI] [PubMed] [Google Scholar]
- 35.Butler RJ, Bullock G, Arnold T, Plisky P, Queen R. Competition-level differences on the lower quarter Y-balance test in baseball players. J Athl Train. 2016;51(12):997–1002. doi: 10.4085/1062-6050-51.12.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sell TC, Tsai YS, Smoliga JM, Myers JB, Lephart SM. Strength, flexibility, and balance characteristics of highly proficient golfers. J Strength Cond Res. 2007;21(4):1166–1171. doi: 10.1519/R-21826.1. [DOI] [PubMed] [Google Scholar]
- 37.Konda S, Yanai T, Sakurai S. Configuration of the shoulder complex during the Arm-cocking phase in baseball pitching. Am J Sports Med. 2015;43(10):2445–2451. doi: 10.1177/0363546515594379. [DOI] [PubMed] [Google Scholar]
- 38.Amin NH, Ryan J, Fening SD, Soloff L, Schickendantz MS, Jones M. The relationship between glenohumeral internal rotational deficits, total range of motion, and shoulder strength in professional baseball pitchers. J Am Acad Orthop Surg. 2015;23(12):789–796. doi: 10.5435/JAAOS-D-15-00292. [DOI] [PubMed] [Google Scholar]
- 39.Scher S, Anderson K, Weber N, Bajorek J, Rand K, Bey MJ. Associations among hip and shoulder range of motion and shoulder injury in professional baseball players. J Athl Train. 2010;45(2):191–197. doi: 10.4085/1062-6050-45.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37(3):566–570. doi: 10.1177/0363546508326712. [DOI] [PubMed] [Google Scholar]
- 41.Polster JM, Bullen J, Obuchowski NA, Bryan JA, Soloff L, Schickendantz MS. Relationship between humeral torsion and injury in professional baseball pitchers. Am J Sports Med. 2013;41(9):2015–2021. doi: 10.1177/0363546513493249. [DOI] [PubMed] [Google Scholar]
- 42.Pieper HG. Humeral torsion in the throwing arm of handball players. Am J Sports Med. 1998;26(2):247–253. doi: 10.1177/03635465980260021501. [DOI] [PubMed] [Google Scholar]
- 43.Lee BJS, Garrison JC, Conway JE, Pollard K, Aryal S. The relationship between humeral retrotorsion and shoulder range of motion in baseball players with an ulnar collateral ligament tear. Orthop J Sports Med. 2016;4(10):2325967116667497. doi: 10.1177/2325967116667497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meister K. Injuries to the shoulder in the throwing athlete. Part one: biomechanics/pathophysiology/classification of injury. Am J Sports Med. 2000;28(2):265–275. doi: 10.1177/03635465000280022301. [DOI] [PubMed] [Google Scholar]
- 45.Tyler TF, Nicholas SJ, Roy T, Gleim GW. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000;28(5):668–673. doi: 10.1177/03635465000280050801. [DOI] [PubMed] [Google Scholar]
- 46.Jobe FW, Radovich Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching. A second report. Am J Sports Med. 1984;12(3):218–220. doi: 10.1177/036354658401200310. [DOI] [PubMed] [Google Scholar]
- 47.Stodden DF, Fleisig GS, McLean SP, Andrews JR. Relationship of biomechanical factors to baseball pitching velocity: within pitcher variation. J Appl Biomech. 2005;21(1):44–56. doi: 10.1123/jab.21.1.44. [DOI] [PubMed] [Google Scholar]
- 48.Karakolis T, Bhan S, Crotin RL. Injuries to young professional baseball pitchers cannot be prevented solely by restricting number of innings pitched. J Sports Med Phys Fitness. 2016;56(5):554–559. [PubMed] [Google Scholar]
- 49.Muir SW, Corea CL, Beaupre L. Evaluating change in clinical status: reliability and measures of agreement for the assessment of glenohumeral range of motion. N Am J Sports Phys Ther. 2010;5(3):98–110. [PMC free article] [PubMed] [Google Scholar]