Abstract
Lack of condom use among youth is a major contributor to the spread of sexually transmitted infections (STIs) including HIV/AIDS, which has life-long deleterious health consequences. College students (N = 262) completed the Sexual Probability Discounting Task in which participants reported their likelihood of condom use under various probabilities of contracting an STI. Each participant completed the task in regard to different STIs including HIV/AIDS, and different partners. Results showed that the likelihood of condom-protected sex generally decreased as HIV/AIDS and other STI contraction became less probable. Moreover, condom-protected sex likelihood was related to STI type (e.g., decreased condom-protected sex in chlamydia relative to HIV/AIDS condition) and partner desirability (decreased condom-protected sex with more desirable partners). Results are the first to show that compared to other STIs, HIV/AIDS had the most influence on condom-protected sex. Results showed probability discounting contributed to lack of condom-protected sex, and offers a novel framework for examining determinants of within-subject variability in condom use.
Keywords: Sexual Health, HIV/AIDS, Sexually Transmitted Infections, Condom Use, Sexual Probability Discounting Task
The American healthcare system spends roughly 16 billion dollars annually on diagnosis and treatment of sexually transmitted infections (STIs; Centers for Disease Control and Prevention [CDC], 2013; Owusu-Edusei, Chesson, Gift, Tao, Mahajan, Ocfemia, & Kent, 2013) and HIV infection alone accounts for more than 80% of this total cost (Owusu-Edusei et al., 2013). Nearly half of the 20 million new cases of STIs diagnosed each year are among young people ages 15–24. Roughly 80% of college-age youths are sexually active and at risk for STIs (Rimsza, 2005), yet only a minority of college students report consistently using condoms (e.g., only 45% report using condoms more than half the time: Bontempi, Mugno, Bulmer, Danvers, & Vancour, 2009; only 32% report consistent condom use: de Visser & Smith, 2001; only 25–32% report consistent condom use: Douglas, Collins, Warren, Kann, Gold, Clayton, Ross & Kolbe, 1997). HIV/AIDS and STIs more generally are a major public health concern for young people, with potentially long-term and serious health consequences (e.g., persisting immunodeficiency caused by HIV/AIDS, cervical cancer caused by HPV). One of the most effective methods to prevent the spread of STIs, including HIV/AIDS, in sexually active individuals is to engage in condom-protected rather than unprotected sex (CDC, 2013).
Educational efforts intended to promote condom use specifically have increased in recent decades -- and are seen as a partial solution to risky youth sex practices (Dick, Ferguson & Ross, 2006; Kirby Laris & Rolleri, 2007). Many of these educational approaches focus on disseminating information about STI prevalence and pregnancy, sexual communication, safer sex practices such as condom use, and in some cases, abstinence (Kirby et al., 2007; Ku, Sonenstein & Pleck, 1992; Stanger-Hall & Hall, 2011; for a meta-analysis reviewing sexual communication, see Widman, Noar, Choukas-Bradley & Francis, 2014). Recent evidence shows, however, that condom use among certain youth populations has shown little improvement in the past decade, remained low, or even declined (CDC, 2012), suggesting that such efforts do not necessarily translate into increased condom use. The pervasive lack of condom use among sexually active young people at risk for STIs necessitates investigation of novel techniques that shed light on environmental influences of condom-use decisions.
One important factor that influences condom-use decisions is the uncertainty, or risk perception of contracting HIV/AIDS or another potential STI (e.g., Fehr, Vidourek & King, 2015; Lammers, van Wijnbergen, Willebrands, 2013; Maharaj & Cleland, 2005; Prata, Morris, Mazive, Vahidnia & Stehr, 2006). Although risk perceptions of STI contraction and reported condom use have been explored (e.g., Haque & Soonthorndhada, 2009) the influence of risk in condom-use decisions is still not well understood (Lammers, et al., 2013). Importantly, previous research has largely focused on characterizing between-subject differences in risk perception, but risk has rarely been experimentally manipulated within individual subjects to understand its influence on condom-use.
Although experimental investigation of the influence of specific STI risk on condom-use decisions is lacking, decades of behavioral research have firmly established that uncertainty systematically decreases an event’s value or impact on behavior, a phenomenon known as probability discounting (e.g., Rachlin, Raineri, & Cross, 1991; Du, Green & Myerson, 2002). Probability discounting has been demonstrated with many outcomes including money and food (e.g., Green & Myerson, 2004). The novel Sexual Probability Discounting Task (SPDT) was developed to systematically examine the potential influence of probability discounting (the likelihood/risk of contracting an STI), on choice for condom-protected versus unprotected sex in casual sex scenarios (e.g., Johnson, Johnson, Herrmann & Sweeney, 2015). Though some individuals may use condoms consistently in all situations regardless of probabilistic HIV/AIDS or STI contraction, others may show sensitivity to the likelihood of contraction -- and therefore vary condom-use based on perceived risk. Determining the influence of risk on condom-protected sex is especially important, given recent evidence showing uncertainty is a dynamic within-subject process, which may be highly dependent on context (Holt, Newquist, Smits, & Tiry, 2014). Although the focus of this particular manuscript was on sexual probability discounting, the data collection efforts were part of a larger study that also examined sexual delay discounting using the same sample (see Collado, Johnson, Loya, Johnson & Yi, 2017). Delay and probability discounting represent fundamentally different decision-making processes (Green & Myerson, 2004). The aim of the previously published study (Collado et al. 2017) was to determine if delay discounting plays a role in decisions to engage in unprotected sex. Alternatively, the aim of this study was to determine if probability discounting plays a role in decisions to engage in unprotected sex.
Johnson and colleagues (2015) examined sexual probability discounting among individuals with cocaine use disorders, a population disproportionately affected by HIV/AIDS, in part due to unprotected sex leading to transmission and contraction. The results showed that decreases in the likelihood of STI contraction resulted in substantial decreases in condom use likelihood. This pattern was found for both cocaine-using individuals and demographically matched non-cocaine using individuals, suggesting that probability discounting contributes to unprotected sex in a wide range of populations (see also Wongsomboon & Robles, 2017 for an extension of sexual probability discounting to college students).
No studies to date, however, have systematically determined the effects of probability of contracting HIV/AIDS, or other specified STIs, on the likelihood of condom-protected sex. If, for example, an individual suspects a potential sexual partner could have a curable condition (e.g., chlamydia), this information may have less influence on condom use than suspecting their partner could have a much more severe or life-threatening condition such as HIV/AIDS. Moreover, few studies in college students have examined how probability discounting affects sexual decision making (although see Dariotis & Johnson, 2015; Collado et al., 2017 for studies assessing the effects of delay on condom-protected sex in youth). Three studies in college students have examined probability discounting in the context of sexual activity (Lawyer, Williams, Prihodova, Rollins, & Lester, 2010; Lawyer & Schoepflin, 2013; Wongsomboon & Robles, 2017). While these studies showed that the value of sexual activity systematically decreased as a result of the uncertainty of sexual activity itself, the tasks used differed from the SPDT in that they did not examine the clinically relevant effect of STI uncertainty. Therefore, the present study was designed to compare the effects of risk of contracting HIV/AIDS and other specific STIs, varying in severity and curability, and demographic characteristics, on the likelihood of condom-protected sex among undergraduate students. We hypothesized that 1) greater discounting of condom-protected sex would be observed in the less severe STI conditions relative to the more severe STI condition (HIV/AIDS), and 2) condom-protected sex would be discounted significantly more when the potential partner was more as opposed to less desirable.
Method
Participants
Undergraduate students were recruited from an online study pool within the Department of Psychology at a large Mid-Atlantic university to participate in the present study (N = 262). Participants provided their written informed consent and received extra credit for participation. The associated Institutional Review Board approved all study procedures.
Materials
Demographic Questionnaire
Participants answered basic demographic questions (e.g., age, sex), as well as additional questions including alcohol use and sorority or fraternity affiliation, and Centers for Disease Control and Prevention Sexual Behavior Questions (CSBQ; CDC, 2011).
Picture Selection and Training
Participants were told to imagine they were not currently in a committed relationship. Participants then viewed 60 color photographs (30 male, 30 female) of diverse, clothed individuals. Photographs were selected to provide a diverse sample within each gender in terms of race/ethnicity, age, weight, body type, body shape, clothing style and attractiveness (Johnson & Bruner, 2012). Participants then identified individuals with whom they would consider having casual sex. From the subset of selected photographs identifying with whom they would consider having casual sex, participants then identified the person with whom they most wanted to have sex, as well as the person with whom they least wanted to have sex. Following photograph selection, participants were trained to use a visual analog scale to indicate condom use likelihood in the Sexual Probability Discounting Task.
Sexual Probability Discounting Task
Prior to beginning the computerized SPDT, participants were asked to imagine: (1) that they were not in a committed relationship, (2) that the photographed individual wanted to have sex now, and (3) that there was no risk of pregnancy if a condom was not used. During each partner condition, a photograph of the participant’s selection (depending on the condition, either the photograph of the person the participant most or least wanted to have sex with) was displayed as he/she made choices in the SPDT. The order of partner conditions was counterbalanced across participants.
On the first trial, the participant was told that if he/she did not use an immediately available condom when having sex, that there was a 1 in 1 (100%) chance of contracting an STI from the photographed individual. Below the text display was a visual analog scale that ranged from “I will definitely have sex with this person without a condom” (0% likelihood of having condom-protected sex) to “I will definitely have sex with this person with a condom” (100% likelihood of having condom-protected sex). Across subsequent trials, the risk of STI contraction was varied systematically (1 in 3 [33%], 1 in 13 [8%], 1 in 100 [1%], 1 in 400 [0.25%], 1 in 700 [0.14%], 1 in 2,000 [.05%], and 1 in 10,000 [0.01 %]). Risk was presented to the participant as both odds in favor and percent chance of STI contraction.
The SPDT was completed four times, one for each of the following STIs: chlamydia, genital herpes, HIV/AIDS, and an unspecified STI condition. Participants completed each of the four STI conditions twice, once for each of the “most want to have sex with” and “least want to have sex with” partner conditions for a total of eight STI-partner condition combinations. The initial partner and STI condition presentation was counterbalanced across participants via block randomization with the stipulation that the unspecified STI condition was never presented first (the unspecified STI condition was always presented last). For any particular participant, the order of the “most want to have sex with” and the “least want to have sex with” conditions was the same for every STI condition.
Procedure
Participants completed the procedure in a quiet experimental room using a computer. Following picture selections, the Sexual Probability Discounting Task (SPDT) was completed. Participants then answered questions as to whether they thought each specified STI (chlamydia, genital herpes, HIV/AIDS) was curable (T/F), and also to rank the order of each specified STI (1 = “most severe” to 3 = “least severe”). Lastly, demographic and substance use questions were answered, and CDC Sexual Behavior Questionnaire (CSBQ) was completed.
Data Analysis
Orderliness of data
Participant data were excluded if he/she selected fewer than two pictures in the picture selection component. Female participants who selected a female partner in either most/least want to have sex with partner condition were also excluded from analyses because transmission of female-to-female HIV/AIDS is extremely rare (CDC, 2014). Participant data were also excluded listwise from analysis if the data were nonsystematic. Data were considered nonsystematic (Johnson & Bickel, 2008; Johnson et al., 2015; Johnson, Herrmann & Johnson, 2015) if across consecutive trials (in which probability of contracting an STI decreased) likelihood of condom use increased by more than 20% of the previous trial, and/or if condom-use likelihood increased by more than 10% from the first to the last trial.
Two measures of discounting were used to characterize the remaining data sets: proportion likelihood of condom use at each risk level, and Area Under the Curve (AUC). First, we visually assessed that median likelihood of condom use decreased as an orderly function of likelihood of STI contraction. Although risk was described to participants in all trials as odds in favor of contracting an STI (percentage chance of contracting an STI), we analyzed the odds against as our independent variable for ease of graphical display and presentation, and consistency with previous probability discounting analyses (e.g., Johnson et al., 2015).
Second, we also calculated the area under the discounting curve (AUC; Myerson, Green & Warusawithrana, 2001). AUC ranges from 0 to 1 (proportion of total area), with lower values indicating greater probability discounting (less likely to engage in condom-protected sex), and higher values indicating less probability discounting (more likely to engage in condom protected sex). Nearly all participants in all cases reported a 100% likelihood of condom-protected sex at the highest chance of contracting an STI (1 in 1, or 100%) across both partner conditions (most/least want to have sex with). AUC calculations performed using GraphPad Prism v.6.0 (GraphPad Software, La Jolla, CA).
Using AUC values as the dependent measure, two separate repeated measures analyses of variance (ANOVA) were conducted (an ANOVA for each partner condition – most and least want to have sex with) to determine potential differences in discounting of condom-protected sex between STI conditions (AUC values for chlamydia, genital herpes, HIV/AIDS, and unspecified STI conditions). Paired t-tests were conducted to evaluate differences in discounting across partner conditions (most versus least want to have sex with) for each STI condition, using a Bonferroni correction to account for familywise error rate for the multiple t-tests (α criterion of .01).
Multiple linear regression was also used to determine participant characteristics predictive of, and therefore influential in sexual probability discounting across conditions. Understanding demographic factors influential in sexual probability discounting could facilitate tailored safer sex programs targeting college age youths most at risk for STI transmission. Specifically, age, gender, ethnicity, Greek status (i.e., fraternity/sorority membership; yes/no), and number of alcoholic beverages consumed in the past week were entered as independent variables in the regression model, as these variables have been identified as potentially important predictors of discounting in either sexual (gender, alcohol use; Dariotis & Johnson, 2015; Jarmolowicz, Bickel & Gatchalian, 2013) or monetary (age, ethnicity; e.g., Du et al., 2002; Green, Myerson & Ostaszewski, 1999) discounting, and/or in the present sample yielded significant relations to AUC at the p ≤ .10 level in at least one of the eight conditions using a one way ANOVA (Greek Status; one way ANOVA comparing those with and without Greek affiliation). A regression model was considered significant at α < .006 to account for familywise error rate using a Bonferroni correction. Multiple linear regression analyses were performed using SPSS v.21.0. (IBM, Armonk, NY).
Results
Orderliness of Data
Two-hundred and sixty-two participants began the survey. Of these, 11 participants did not finish the survey, 13 participants selected fewer than two pictures in the picture selection component, 11 female participants selected at least one female partner across partner conditions, and 10 participants responded in a nonsystematic fashion. Therefore, data from 217 participants were included in subsequent data analyses.
Demographic Characteristics and CDC Sexual Behavior Questionnaire Data
Table 1 presents participant demographics, substance use, Greek affiliation, and curability ratings and severity rankings for each STI. Participants were on average 19.7 years old and 50% were male. Fifty-five percent were Caucasian/white. Seventy-eight percent reported using alcohol in the past week, 27% reported using marijuana in the past month, and 8% reported smoking cigarettes. Average number of total lifetime sexual partners was four, and 17% reported belonging to a sorority or fraternity. Additionally, curability ratings showed that most participants rated chlamydia as curable, but fewer believed genital herpes was curable, and almost none believed HIV/AIDS was curable (Cochran’s Q test used for nonparametric binomial within-subject data; Cochran’s Q = 214.9; p < .0001; follow-up McNemar tests p < .0001 for each STI comparison). Severity rankings also showed that chlamydia was viewed as the least severe STI, followed by genital herpes and HIV/AIDS (Friedman nonparametric test; χ2 = 269.7; p < .0001), although only the rankings between HIV/AIDS and chlamydia (p < .0001), and HIV/AIDS and genital herpes (p < .0001) reached statistical significance using Dunn’s post hoc multiple comparisons.
Table 1.
| Demographics (n=217) | |
|---|---|
| Age in years, mean (SD) | 19.7 (1.9) |
| Gender, count (%) | |
| Male | 109 (50) |
| Female | 108 (50) |
| Sexual attraction to male/female | 1 (38) |
| Scale 1–7; 1=male, 4=both, 7=female (%) | 2 (8) |
| 3 (2) | |
| 4 (3) | |
| 5 (1) | |
| 6 (3) | |
| 7 (45) | |
| Ethnicity, count (%) a, b | |
| Caucasian/white | 120 (55) |
| Asian/Southeast Asian | 41 (19) |
| African-American/black | 51 (24) |
| Hispanic/Latino | 32 (15) |
| Native American | 3 (1) |
| Other | 5 (2) |
| Greek Affiliation (%) | 37 (17) |
| Substance Use | |
| Alcohol | |
| Number reporting use in past week (%) | 170 (78) |
| Average number consumed in past week (SD) | 6.9 (16.1) |
| Marijuana | |
| Number reporting use in past month (%) | 59 (27) |
| Average number of times smoked in past month (SD) | 14 (24.5) |
| Cigarettes | |
| Number reporting smoking (%) | 18 (8) |
| Average number smoked in past week | 2.3 (4.5) |
| Average number of total sexual partners (SD) | 4.2 (6.3) |
| Curability Ratings | |
| Chlamydia is curable: Count True (%) | 152 (70) |
| Genital Herpes is curable: Count True (%) | 57 (26) |
| HIV/AIDS is curable: Count True (%) | 4 (2) |
| Severity Rankings (1= Most severe, 3 = Least severe) | |
| Chlamydia, Average (SD) | 2.5 (.6) |
| Genital Herpes, Average (SD) | 2.4 (.5) |
| HIV/AIDS, Average (SD) | 1.1 (.4) |
Participants could identify as more than one ethnicity
In statistical analyses, ethnicity categories were evaluated as Caucasian/white versus other
Table 2 further characterizes the sample, displaying the CDC Sexual Behavior Questionnaire data. Most of the sample had previously engaged in vaginal sex (75%), or oral sex (85%). Approximately 22% had engaged in anal sex. Twelve percent had no previous sexual experience (i.e., no previous vaginal, anal, or oral sexual experience).
Table 2.
CDC Sexual Behavior Questionnaire
| n=217 | |
|---|---|
| Vaginal Sex | |
| Ever engaged in vaginal sex? Count (%) | 162 (75) |
| How old were you the first time? Mean (SD) | 17 (1.7) |
| Ever with an individual working as prostitute? Count (%) | 0 (0) |
| Ever with an individual with HIV/AIDS? Count (%) | 0 (0) |
| Ever with an individual who has injected drugs? Count (%) | 4 (2) |
| Ever with an individual whose sexual history you did not know well? Count (%) | 83 (38) |
| How many times in the past 6 months have you had vaginal sex? Mean (SD) | 32 (49.4) |
| Of these times, how often did you use condoms/latex protection? Mean (SD) | 10 (19.1) |
| Anal Sex | |
| Ever engaged in anal sex? Count (%) | 47 (22) |
| How old were you the first time? Mean (SD) | 18 (1.7) |
| Ever with an individual working as prostitute? Count (%) | 0 (0) |
| Ever with an individual with HIV/AIDS? Count (%) | 0 (0) |
| Ever with an individual who has injected drugs? Count (%) | 1 (0.5) |
| Ever with an individual whose sexual history you did not know well? Count (%) | 13 (6) |
| How many times in the past 6 months have you had anal sex? Mean (SD) | 2 (2.1) |
| Of these times, how often did you use condoms/latex protection? Mean (SD) | 1 (1.1) |
| Oral Sex | |
| Ever engaged in oral sex? Count (%) | 184 (85) |
| How old were you the first time? Mean (SD) | 16 (1.8) |
| Ever with an individual working as prostitute? Count (%) | 0 (0) |
| Ever with an individual with HIV/AIDS? Count (%) | 0 (0) |
| Ever with an individual who has injected drugs? Count (%) | 3 (1) |
| Ever with an individual whose sexual history you did not know well? Count (%) | 85 (39) |
| How many times in the past 6 months have you had oral sex? Mean (SD) | 21 (34.5) |
| Of these times, how often did you use condoms/latex protection? Mean (SD) | 0.1 (.84) |
Probability Discounting of Condom-Protected Sex
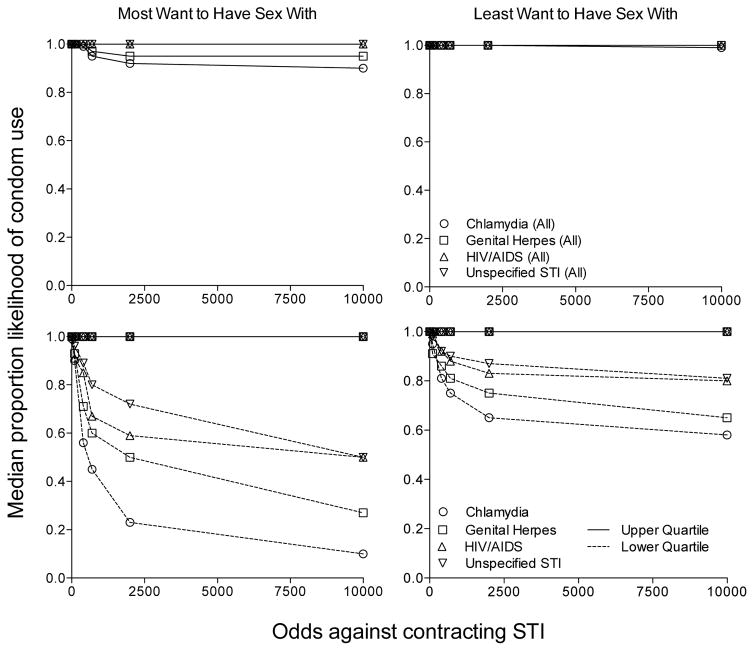
Figure 1 displays the median proportion likelihood of condom-protected sex as a function of odds against STI contraction by STI type and partner condition – most (left column) and least (right column) want to have sex with. The top panels show median proportion likelihood of condom-protected sex was high across conditions when all participants are included. Given the relatively low rates of discounting reflected in the median data, a post-hoc analysis was conducted in which we analyzed the upper and lower quartiles of discounting data (n = 54 for each quartile displayed). Specifically, the bottom panels display the upper and lower quartile discounting data (i.e., based on each participant’s mean AUC value across partner conditions, the 25% who discounted condom-protected sex the least, and the 25% of the sample who discounted condom-protected sex the most). Data in the bottom panels show that the highest risk group precipitously discounted condom-protected sex in all STI conditions, and especially so with the partner that they most wanted to have sex with. Moreover, the data from these participants show that in all partner conditions, condom-protected sex likelihood decreased as a systematic function of STI acquisition uncertainty.
Figure 1.
Median proportion likelihood of condom use as a function of odds against contracting STI in the “most want to have sex with” partner condition (top left panel), and the “least want to have sex with” partner condition (top right panel). Bottom left and right panels show the median proportion likelihood of condom use of the upper and lower quartiles.
Participants discounted condom-protected sex more (i.e., were less likely to use condoms) for less harmful STI conditions (i.e., chlamydia, genital herpes) relative to the more harmful STI HIV/AIDS, or the unspecified STI. Repeated measures ANOVAs confirmed these visual outcomes, and showed a significant main effect of STI condition in the most want to have sex with partner condition, F(2.50, 540.36) = 31.54, p < .0001; η2 = .03. Post hoc Bonferroni multiple comparison tests revealed significantly greater discounting of condom-protected sex as measured by AUC in the chlamydia STI condition (M = .76, SD = .32) compared to the the HIV/AIDS (M = .87, SD = .25) condition and the chlamydia condition compared to the unspecified STI (M = .88, SD = .23) condition (in both cases, p < .001). Significantly greater discounting of condom-protected sex in the genital herpes STI condition (M = .80, SD = .28) relative to the HIV/AIDS and unspecified STI conditions (in both cases, p < .001) was also revealed. No significant differences in discounting of condom-protected sex were revealed between the chlamydia and genital herpes conditions, or between the HIV/AIDS and unspecified STI conditions.
A significant main effect of STI condition in the least want to have sex with partner condition was also revealed, F(2.45, 528.56) = 18.11, p < .0001; η2 = .02. Similar to the most want to have sex with condition, post hoc Bonferroni multiple comparison tests revealed significantly greater discounting of condom-protected sex as measured by AUC in the chlamydia STI condition (M = .86, SD = .22) compared to the HIV/AIDS (M = .91, SD = .20) condition, and the chlamydia condition compared to the unspecified STI (M = .93, SD = .18) condition (in both cases, p < .001). Significantly greater discounting of condom-protected sex in the genital herpes STI condition (M = .89, SD = .21) relative to the HIV/AIDS and unspecified STI (in both cases, p < .012) conditions was also revealed. No significant differences in discounting of condom-protected sex were revealed between the chlamydia and genital herpes conditions, or between the HIV/AIDS and unspecified STI conditions (in both cases, p > .23).
Significantly greater discounting of condom-protected sex was also observed in the more desirable partner condition (i.e., “most want to have sex with” relative to “least want to have sex with”). Follow-up paired t-tests comparing AUC of each STI across partner conditions (accounting for familywise error rate using a Bonferroni correction) showed that in all cases participants discounted condom-protected sex more in the most relative to the least want to have sex with partner condition (chlamydia, most vs. least; t(1, 216) = 7.39, p < .001; genital herpes, most vs. least t(1, 216) = 7.23, p < .001; HIV/AIDS most versus least t(1, 216) = 5.75, p < .001; unspecified most versus least t(1, 216) = 5.63, p < .001).
Demographic predictors of probability discounting of condom-protected sex
Multiple linear regression was used to examine the predictive value of age, gender, ethnicity (Caucasian or other), Greek status (yes or no), and alcoholic beverages consumed in the past week on likelihood of condom-protected sex across each partner and STI condition. Initial regression diagnostics showed no multicollinearity among any of the predictor variables (all tolerance > .5). One outlier (number of alcoholic drinks per week = 200) was removed, but inclusion/exclusion of this did not influence whether the regression analysis reached significance.
For the chlamydia condition, the regression model accounted for a significant amount of the variance in likelihood of condom-protected sex in the most F(5, 211) = 5.66, p < .000, R2 = .118, and least want to have sex with partner conditions F(5, 211) = 4.49, p = .001, R2 = .096, as well as in the genital herpes most F(5, 211) = 3.92, p = .002, R2 = .085 (but not least) want to have sex with partner conditions. The model did not account for significant variability in either the most or least want to have sex with partner conditions within the HIV/AIDS or unspecified STI conditions. In the significant models, only gender as a predictor had significant partial effects in the full model (p < .0001), suggesting that women reported a higher likelihood of condom-protected sex (as measured by AUC) relative to men in both partner conditions. Participant responses from the Sexual Behavior Questions (CSBQ), as well as each STI curability rating and severity score were also tested in exploratory correlations and regression models. Although taken together these variables accounted for additional variability in the regression models, not one offered significant predictive value for discounting of condom-protected sex across STI and partner conditions.
Discussion
Several notable results emerged from the present study in which we examined the effects of probability of contracting HIV/AIDS and other STIs, and partner desirability on likelihood of hypothetical condom-protected sex using a within-subject design in undergraduate students. First, as odds against contracting an STI increased (i.e., risk of contracting an STI decreased), the reported likelihood of condom-protected sex generally decreased – a decrease that was especially sharp in the highest risk portion of the sample. Second, degree of probability discounting of condom-protected sex significantly differed as a function of STI type, with greater discounting of condom-protected sex observed for less severe STIs (chlamydia, genital herpes) relative to a more severe STI (HIV/AIDS) or an unspecified STI. Third, condom-protected sex was discounted more when the potential partner was more rather than less desirable based on appearance and especially so when the STI type was less severe. Lastly, the regression model revealed that gender was the main significant predictor of likelihood of condom-protected sex. Women reported a higher likelihood of condom-protected sex within the chlamydia (for most and least want to have sex with partner) and genital herpes (most want to have sex with partner) conditions. Each of these findings will be discussed in turn.
Although typically only studied with monetary rewards in humans, the level of uncertainty associated with receipt of that outcome influences decision-making processes (e.g., Green & Myerson, 2004). In the present experiment, condom-protected sex was discounted as a function of STI risk, indicating these relations were well described by the probability discounting framework (e.g., Green & Myerson, 2004; Poltavski & Weatherly, 2013). In research assessing risk perceptions and condom use, Crosby, Milhausen, Graham, Yarber, Sanders, Charnigo, and Shrier (2014) showed that when STI clinic attendees suspected a sex partner of having an STI, condom use was significantly higher than when a sex partner was not suspected of having an STI. Specifically, when this suspicion was present, condom use was more than twice as likely during intercourse than when this suspicion was not present. Results from our study align with and extend the findings of Crosby et al. (2014) to show that when perceived risk is parametrically manipulated across a number of risk levels and varying STIs, that likelihood of condom-protected sex versus unprotected sex is directly impacted. The larger proportion of participants that endorsed 100% likelihood of condom-protected sex at the 100% contraction risk level for all STI and partner conditions demonstrated that reductions in likelihood of condom-protected sex are purely a product of probability discounting (i.e., a direct function of reduced probabilities of contraction). Although other studies have offered meaningful insight into the probabilistic value of sexual activity (e.g., Lawyer, 2008; Lawyer & Schoepflin, 2013; Lawyer et al., 2010), this study directly addressed the influence of HIV/AIDS and other STI probabilities on likelihood of engaging in condom-protected sex.
The decrease in likelihood of condom-protected sex for many participants was modest (see top panels, Figure 1), which is consistent with desirable public health behavior. However, the sharp decrease in likelihood of condom-protected sex in even the most severe conditions (i.e., HIV/AIDS) in the lower quartile of participants (see bottom panels, Figure 1) was alarming. The decrease in likelihood of condom-protected sex was also more or less prominent under certain STI and partner conditions (discussed in detail below), which is similar to recent evidence documenting the effects of delay to obtaining a condom on likelihood of condom-protected sex in a study conducted with 18- to 24-year olds (e.g., Dariotis & Johnson, 2015). For example, Dariotis and Johnson showed that the decrease in likelihood of condom-protected sex was systematic across increasing delays to obtaining a condom (i.e., the longer an individual had to wait for a condom, the less likely he/she was to use it). The observed effect of discounting the likelihood of condom-protected sex was influenced similarly by variables that were also explored in the present study (i.e., partner characteristics). As it is likely that real world sexual situations involve both temporal and probabilistic aspects of choice, better understanding how the interaction of these decision-making processes influence likelihood of condom-protected sex represents an important area of future research. There is also some indication that aspects of delay and probability decision-making processes are domain specific (i.e., factors influencing choice of delayed and probabilistic monetary outcomes are not necessarily similar for delay and probabilistic sexual outcomes, e.g., Johnson et al., 2015). Therefore, future studies might investigate factors that specifically increase the likelihood of condom-protected sex across sexual probability and delay discounting tasks, and the resulting implications for real world condom-protected sex decisions.
No other studies to date have systematically examined contraction risk of HIV/AIDS and other STIs, which differ on dimensions of curability and treatability, on the likelihood of condom-protected sex within a sexual discounting framework. Likelihood of condom-protected sex was discounted most with the curable STI, chlamydia, and similarly so for the treatable, although currently not curable STI genital herpes. The likelihood of condom-protected sex was higher across all risk levels with HIV/AIDS as well as the unspecified STI condition, compared to the other STI conditions, possibly indicating similar underlying decision-making processes for both severe STIs and uncertainty of a potential STI. Little knowledge of a partner’s history, as is often the case in casual sex scenarios, may translate into a high likelihood of condom-protected sex as a result of caution driven by uncertainty of contracting a severe, albeit relatively rarer STI such as HIV/AIDS (e.g., Rosengard, Clarke, DaSilva, Hebert, Rose & Stein, 2005; van Empelen, Schaalma, Kok, & Jansen, 2001). Situations in which a partner’s sexual history and therefore health is not well known -- as in the presently explored unspecified STI condition -- may also be most reflective of real world casual sex circumstances.
The observed effect of decreased likelihood of condom-protected sex with less severe STI conditions was especially exacerbated with a more versus less sexually desirable partner (i.e., “most want to have sex with” partner condition versus “least want to have sex with” partner condition). Other studies that examined the related phenomenon of sexual delay discounting with older populations have shown similar associations between decreased likelihood of condom-protected sex and partner desirability (e.g., Herrmann, Johnson, & Johnson, 2015; Johnson & Bruner, 2012; Johnson et al., 2015). This study is the first to show in a youth population of undergraduate students, that similar to delay discounting, likelihood of condom-protected sex is discounted across specified probability levels more so when the desirability of the potential partner is high (e.g., Dariotis and Johnson, 2015). Desirability of a potential partner therefore, may be a particularly relevant factor driving sexual decision-making processes related to both risk and delay, especially so in undergraduate students and youths. Sexual education efforts might highlight that risk of STI contraction is associated with all partners, regardless of physical appearance (Dariotis & Johnson, 2015).
A large number of studies investigating predictors of condom-use have focused on between subject variables including gender, age, health beliefs or attitudes, and risk perception (e.g., Buhi et al., 2007; Haque & Soonthorndhada, 2009; Orr & Langefeld, 1993). The present experiment employed within-subject experimental manipulations, with data suggesting that environmental variables (STI contraction probability and partner characteristics) caused changes in condom-use behavior for the same individual in different situations. These data suggest that even individuals who engage in safer sex practices much of the time are likely to be vulnerable to risky sexual influences as a result of environmental factors.
It is also important to note, that although the majority of participants were sensitive to probability of STI contraction, some participants responded with 100% likelihood of condom use across all STI contraction probabilities and conditions. These individuals may be risk averse in all situations, and their condom use behavior might be considered rule-governed (e.g., Galizio, 1979) and unaffected by environmental factors. One important extension for future research will be the examination of factors that lead “risk takers” to instead engage in “risk averse” condom-protected sex behavior (i.e., condom-use despite perceived low risk of STI contraction).
The present dataset suggests that risk of contracting a severe STI (i.e., HIV/AIDS) resulted in an increased likelihood of condom-protected sex relative to the same risk of contracting less severe STIs (i.e., chlamydia, herpes). Occurrences of chlamydia and herpes, however, are far more common than HIV/AIDS (CDC, 2017, 2015; a, b). Chlamydia and herpes can also result in potential lifelong detrimental consequences (CDC, 2015; a, b), and such information should also be conveyed effectively in sexual health programs specifically designed for youths.
We used multiple regression to examine the influence of five demographic predictor variables on likelihood of condom-protected sex across all conditions. In the overall five-predictor model, gender was the major driver of reported likelihood of condom-protected sex in casual sex encounters – and showed that men discounted condom-protected sex more than women. This finding extends previous research on discounting of sexual outcomes. Specifically, Johnson and Bruner (2013) showed that women report a higher likelihood of condom-protected sex with casual sexual encounters compared to men in a sexual delay discounting task – and the present results extend these findings to probability discounting of sexual outcomes. The convergence of the present results with previous findings further adds to the validity and reliability of the newly established sexual probability discounting task, and supports the notion of STI prevention programs tailored to the sexes (i.e., men may require more in-depth education regarding STI risk and safer sex practices). These data also warrant further exploration of how to influence risk perceptions and preparatory behaviors (e.g., condom-carrying) for situations in which risk of STI contraction may arise (i.e., unexpected casual and risky sex scenarios), specifically among youth populations.
Several limitations exist. First, our scenarios are necessarily hypothetical in nature. However, research shows that decision making with hypothetical decisions in laboratory tasks is related real world behavior involving probabilities, such as gambling (e.g., Holt, Green & Myerson, 2003; Madden, Petry & Johnson, 2009). Along similar lines, the task is necessarily contrived, as calculating the precise odds of STI contraction in a casual sex scenario would be impossible. By using this scenario, however, we showed that condom use decisions were systematically influenced by risk. Therefore, the present methods may represent the best way to study such relations under controlled conditions. Another limitation of the present research was that condom-protected sex was only examined across two partner conditions -- the “most” and “least want to have sex with” partner conditions. It is possible that degree of condom-protected sex would diverge from the present results if an “intermediate” partner (a partner somewhere between “most” and “least want to have sex with”) was also selected. We suspect that condom-protected sex would be discounted to an intermediate degree (somewhere between the degree of discounting observed for “most” and “least want to have sex with” partners), although more research is needed to test this hypothesis.
Additionally, while the overall linear regression model was able to account for a significant amount of variability in reported likelihood of condom use in both chlamydia and genital herpes conditions, it did not account for significant variability in some other (incurable) STI conditions (i.e., HIV/AIDS least want to have sex with) or the unspecified STI condition. These results are likely influenced by the limited variability in AUC across many of the STI and partner conditions. Variability in AUC, however, was largely attributable to experimentally manipulated contraction likelihoods, showing probabilistic discounting of condom-protected sex. These data showed that risky behavior can be heavily influenced by not only preexisting trait variables (e.g., gender), but also contextual variables (e.g., risk) -- and therefore warrant additional investigation of environmental factors influencing condom use within youth populations.
Acknowledgments
This research was supported in part by National Institute on Drug Abuse (NIDA) grants R01DA032363 and T32DA07209.
Footnotes
Compliance with Ethical Standards
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Bontempi JB, Mugno R, Bulmer SM, Danvers K, Vancour ML. Exploring gender differences in the relationship between HIV/STD testing and condom use among undergraduate college students. American Journal of Health Education. 2009;40(2):97–105. [Google Scholar]
- Buhi ER, Goodson P. Predictors of adolescent sexual behavior and intention: A theory-guided systematic review. Journal of Adolescent Health. 2007;40(1):4–21. doi: 10.1016/j.jadohealth.2006.09.027. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Control HIV/STD behavioral surveillance working group. CDC Sexual behavior questions (CSBQ) 2011 Retrieved from http://chipts.ucla.edu/wp-content/uploads/downloads/2012/01/CDC-Sexual-Behavior-Questions-_CSBQ_.pdf.
- Centers for Disease Control and Prevention. Trends in HIV-Related Risk Behaviors Among High School Students – United States, 1991–2011. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6129a4.htm?s_cid=mm6129a4_w.
- Centers for Disease Control and Prevention. Incidence, prevalence, and cost of sexually transmitted infections in the united states. 2013 Retrieved from Http://www.Cdc.gov/std/stats/sti-Estimates-Fact-Sheet-Feb-2013.Pdf.
- Centers for Disease Control and Prevention. Likely female-to-female sexual transmission of HIV. Morbidity and Mortality Weekly Report. 2014;63:209–210. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Chlamydia – CDC fact sheet (detailed) 2015a Retrieved from Http://www.Cdc.gov/std/chlamydia/stdfact-Chlamydia-Detailed.Htm.
- Centers for Disease Control and Prevention. Genital herpes – CDC fact sheet. 2015b Retrieved from Http://www.Cdc.gov/std/herpes/stdfact-Herpes.Htm.
- Centers for Disease Control and Prevention. HIV/AIDS Basic Statistics. 2017 Retrieved from https://www.cdc.gov/hiv/basics/statistics.html.
- Collado A, Johnson PS, Loya JM, Johnson MW, Yi R. Discounting of condom-protected sex as a measure of high risk for sexually transmitted infection among college students. Archives of Sexual Behavior. 2017;46(7):2187–2195. doi: 10.1007/s10508-016-0836-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby RA, Milhausen RR, Graham CA, Yarber WL, Sanders SA, Charnigo R, Shrier LA. Likelihood of condom use when sexually transmitted diseases are suspected: Results from a clinic sample. Health Education & Behavior. 2014;41(4):449–454. doi: 10.1177/1090198114529588. [DOI] [PubMed] [Google Scholar]
- Dariotis JK, Johnson MW. Sexual discounting among high-risk youth ages 18–24: Implications for sexual and substance use risk behaviors. Experimental and Clinical Psychopharmacology. 2015;23(1):49–58. doi: 10.1037/a0038399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Visser R, Smith A. Relationship between sexual partners influences rates and correlates of condom use. AIDS Education and Prevention. 2001;13(5):413–427. doi: 10.1521/aeap.13.5.413.24146. [DOI] [PubMed] [Google Scholar]
- Dick B, Ferguson J, Ross DA. Preventing HIV/AIDS in young people. A systematic review of the evidence from developing countries. Introduction and rationale. World Health Organization Technical Report Series. 2006;938:1–13. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=16921915&site=ehost-live&scope=site. [PubMed] [Google Scholar]
- Douglas KA, Collins JL, Warren C, Kann L, Gold R, Clayton S, … Kolbe LJ. Results from the 1995 national college health risk behavior survey. Journal of American College Health. 1997;46(2):55–67. doi: 10.1080/07448489709595589. [DOI] [PubMed] [Google Scholar]
- Du W, Green L, Myerson J. Cross-cultural comparisons of discounting delayed and probabilistic rewards. Psychological Record. 2002;52(4):479–492. doi: 10.1007/BF03395199. [DOI] [Google Scholar]
- Fehr S, Vidourek R, King K. Intra- and inter-personal barriers to condom use among college students: A review of the literature. Sexuality & Culture. 2015;19(1):103–121. doi: 10.1007/s12119-014-9249-y. [DOI] [Google Scholar]
- Galizio M. Contingency-shaped and rule-governed behavior: Instructional control of human loss avoidance. Journal of the Experimental Analysis of Behavior. 1979;31(1):53–70. doi: 10.1901/jeab.1979.31-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green L, Myerson J. A discounting framework for choice with delayed and probabilistic rewards. Psychological Bulletin. 2004;130(5):769–792. doi: 10.1037/0033-2909.130.5.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green L, Myerson J, Ostaszewski P. Discounting of delayed rewards across the life span: Age differences in individual discounting functions. Behavioural Processes. 1999;46(1):89–96. doi: 10.1016/S0376-6357(99)00021-2. [DOI] [PubMed] [Google Scholar]
- Haque MR, Soonthorndhada A. Risk perception and condom-use among Thai youths: Findings from Kanchanaburi demographic surveillance system site in Thailand. Journal of Health, Population & Nutrition. 2009;27(6):772–783. doi: 10.3329/jhpn.v27i6.4329. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=49119034&site=ehost-live&scope=site. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann E, Johnson P, Johnson M. Examining delay discounting of condom-protected sex among men who have sex with men using crowdsourcing technology. AIDS & Behavior. 2015;19(9):1655–1665. doi: 10.1007/s10461-015-1107-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt DD, Green L, Myerson J. Is discounting impulsive? Evidence from temporal and probability discounting in gambling and non-gambling college students. Behavioural Processes. 2003;64(3):355–367. doi: 10.1016/S0376-6357(03)00141-4. [DOI] [PubMed] [Google Scholar]
- Holt DD, Newquist MH, Smits RR, Tiry AM. Discounting of food, sex, and money. Psychonomic Bulletin & Review. 2014;21(3):794–802. doi: 10.3758/s13423-013-0557-2. [DOI] [PubMed] [Google Scholar]
- Jarmolowicz DP, Bickel WK, Gatchalian KM. Alcohol-dependent individuals discount sex at higher rates than controls. Drug and Alcohol Dependence. 2013;131(3):320–323. doi: 10.1016/j.drugalcdep.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. An algorithm for identifying nonsystematic delay-discounting data. Experimental and Clinical Psychopharmacology. 2008;16(3):264–274. doi: 10.1037/1064-1297.16.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR. The sexual discounting task: HIV risk behavior and the discounting of delayed sexual rewards in cocaine dependence. Drug and Alcohol Dependence. 2012;123(1–3):15–21. doi: 10.1016/j.drugalcdep.2011.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR. Test-retest reliability and gender differences in the sexual discounting task among cocaine-dependent individuals. Experimental and Clinical Psychopharmacology. 2013;21(4):277–286. doi: 10.1037/a0033071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Johnson PS, Herrmann ES, Sweeney MM. Delay and probability discounting of sexual and monetary outcomes in individuals with cocaine use disorders and matched controls. PLoS ONE. 2015;10(5):1–21. doi: 10.1371/journal.pone.0128641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PS, Herrmann ES, Johnson MW. Opportunity costs of reward delays and the discounting of hypothetical money and cigarettes. Journal of the Experimental Analysis of Behavior. 2015;103(1):87–107. doi: 10.1002/jeab.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: Their impact on sexual behaviors of young people throughout the world. Journal of Adolescent Health. 2007;40(3):206–217. doi: 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- Ku LC, Sonenstein FL, Pleck JH. The association of AIDS education and sex education with sexual behavior and condom use among teenage men. Family Planning Perspectives. 1992;24(3):100–106. [PubMed] [Google Scholar]
- Lammers J, van Wijnbergen SJ, Willebrands D. Condom use, risk perception, and HIV knowledge: A comparison across sexes in Nigeria. HIV/AIDS (Auckland, NZ) 2013;5:283–293. doi: 10.2147/HIV.S31687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawyer SR. Probability and delay discounting of erotic stimuli. Behavioural Processes. 2008;79(1):36–42. doi: 10.1016/j.beproc.2008.04.009. [DOI] [PubMed] [Google Scholar]
- Lawyer SR, Schoepflin FJ. Predicting domain-specific outcomes using delay and probability discounting for sexual versus monetary outcomes. Behavioural Processes. 2013;96:71–78. doi: 10.1016/j.beproc.2013.03.001. [DOI] [PubMed] [Google Scholar]
- Lawyer SR, Williams SA, Prihodova T, Rollins JD, Lester AC. Probability and delay discounting of hypothetical sexual outcomes. Behavioural Processes. 2010;84(3):687–692. doi: 10.1016/j.beproc.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Petry NM, Johnson PS. Pathological gamblers discount probabilistic rewards less steeply than matched controls. Experimental and Clinical Psychopharmacology. 2009;17(5):283–290. doi: 10.1037/a0016806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maharaj P, Cleland J. Risk perception and condom use among married or cohabiting couples in KwaZulu-Natal, South Africa. International Family Planning Perspectives. 2005;31(1):24–29. doi: 10.1363/3102405. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106488031&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- Myerson J, Green L, Warusawitharana M. Area under the curve as a measure of discounting. Journal of the Experimental Analysis of Behavior. 2001;76(2):235–243. doi: 10.1901/jeab.2001.76-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr DP, Langefeld CD. Factors associated with condom use by sexually active male adolescents at risk for sexually transmitted disease. Pediatrics. 1993;91(5):873–879. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=f5h&AN=4751992&site=ehost-live&scope=site. [PubMed] [Google Scholar]
- Owusu-Edusei K, Jr, Chesson HW, Gift TL, Tao G, Mahajan R, Ocfemia MCB, Kent CK. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sexually Transmitted Diseases. 2013;40(3):197–201. doi: 10.1097/OLQ.0b013e318285c6d2. [DOI] [PubMed] [Google Scholar]
- Poltavski DV, Weatherly JN. Delay and probability discounting of multiple commodities in smokers and never-smokers using multiple-choice tasks. Behavioural Pharmacology. 2013;24(8):659–667. doi: 10.1097/FBP.0000000000000010. [DOI] [PubMed] [Google Scholar]
- Prata N, Morris L, Mazive E, Vahidnia F, Stehr M. Relationship between HIV risk perception and condom use: Evidence from a population-based survey in Mozambique. International Family Planning Perspectives. 2006;32(4):192–200. doi: 10.1363/3219206. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106282596&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- Rachlin H, Raineri A, Cross D. Subjective probability and delay. Journal of the Experimental Analysis of Behavior. 1991;55(2):233–244. doi: 10.1901/jeab.1991.55-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimsza ME. Sexually transmitted infections: New guidelines for an old problem on the college campus. Pediatric Clinics of North America. 2005;52(1):217–228. doi: 10.1016/j.pcl.2004.10.010. [DOI] [PubMed] [Google Scholar]
- Rosengard C, Clarke JG, DaSilva K, Hebert M, Rose J, Stein MD. Correlates of partner-specific condom use intentions among incarcerated women in Rhode Island. Perspectives on Sexual & Reproductive Health. 2005;37(1):32–38. doi: 10.1363/psrh.37.32.05. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106548427&site=ehost-live&scope=site. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger-Hall K, Hall DW. Abstinence-only education and teen pregnancy rates: Why we need comprehensive sex education in the U.S. PLoS ONE. 2011;6(10):1–11. doi: 10.1371/journal.pone.0024658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Empelen P, Schaalma HP, Kok G, Jansen MWJ. Predicting condom use with casual and steady sex partners among drug users. Health Education Research. 2001;16(3):293–305. doi: 10.1093/her/16.3.293. [DOI] [PubMed] [Google Scholar]
- Widman L, Noar SM, Choukas-Bradley S, Francis DB. Adolescent sexual health communication and condom use: A meta-analysis. Health Psychology. 2014;33(10):1113–1124. doi: 10.1037/hea0000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wongsomboon V, Robles E. Devaluation of safe sex by delay or uncertainty: A within-subjects study of mechanisms underlying sexual risk behavior. Archives of Sexual Behavior. 2017;46(7):2131–2144. doi: 10.1007/s10508-016-0788-1. [DOI] [PubMed] [Google Scholar]