Abstract
Background:
In sub-Saharan Africa, cardiovascular disease is becoming a leading cause of death, with high blood pressure as number one risk factor. In Nigeria, access and adherence to hypertension care are poor. A pharmacy-based hypertension care model with remote monitoring by cardiologists through mHealth was piloted in Lagos to increase accessibility to quality care for hypertensive patients.
Objectives:
To describe patients’ and healthcare providers’ perceptions and practices regarding hypertension, pharmacy-based care, and mHealth and explore how this information may improve innovative hypertension service delivery.
Methods:
This study consisted of observations of patient–pharmacy staff interactions and hypertension care provided, four focus group discussions and in-depth interviews with 30 hypertensive patients, nine community pharmacists, and six cardiologists, and structured interviews with 328 patients.
Results:
Most patients were knowledgeable about biomedical causes and treatment of hypertension, but often ignorant about the silent character of hypertension. Reasons mentioned for not adhering to treatment were side effects, financial constraints, lack of health insurance, and cultural or religious reasons. Pharmacists additionally mentioned competition with informal, cheaper healthcare providers. Patients highly favored pharmacy-based care, because of the pharmacist–patient relationship, accessibility, small-scale, and a pharmacy's registration at an association. The majority of respondents were positive towards mHealth.
Conclusion:
Facilitating factors for innovative pharmacy-based hypertension care were: patients’ biomedical perceptions, pharmacies’ strong position in the community, and respondents’ positive attitude towards mHealth. We recommend health education and strengthening pharmacists’ role to address barriers, such as misperceptions that hypertension always is symptomatic, treatment nonadherence, and unfamiliarity with mHealth. Future collaboration with insurance providers or other financing mechanisms may help diminish patients’ financial barriers to appropriate hypertension treatment.
Keywords: hypertension perceptions, mHealth, pharmacy-based care, sub-Saharan Africa, task shifting
INTRODUCTION
In 2014, the World Health Organization estimated a hypertension prevalence in Nigeria of 21.6% [1]. The prevalence keeps rising [2,3] and is associated with mass migration from rural to urban areas, uptake of ‘Western’ lifestyles including consumption of fast food, processed foods (high in fats and salt), alcohol, and tobacco amongst others [4,5]. Despite the availability of a wide variety of antihypertensive drugs [6], treatment adherence among patients remains low [7]. Several studies showed that there is a need for innovative healthcare interventions to address this tension [8–10]. Qualitative studies generate a deeper understanding of patients’ and healthcare providers’ experiences with hypertension care that may be used to address facilitators and barriers to such interventions [11,12].
The paradox of patients’ poor hypertension control despite the availability of effective antihypertensive drugs is partially explained by socioeconomic, organizational [1,5,13], and cultural barriers [14]. Financial constraints hinder accessing care for many patients [6,15]. Nigeria is the biggest economy of Africa [16], yet unemployment is high and most people live under the poverty line. Healthcare is mainly financed by patients, through out-of-pocket payments. The public health infrastructure is often poor [17] and healthcare staff shortages lead to high workloads resulting in long-waiting times [18]. A hospital visit can command considerable opportunity costs for patients (lost time, transport costs) and negatively impacts treatment compliance [19,20]. These challenges of the public health system entice many patients to seek treatment elsewhere. The Nigerian healthcare system consists of a plethora of public and private care facilities, and a wide range of community-based care providers, such as pharmacists, chemists, and traditional healers. Additionally, various studies have shown that Nigerians hold diverse beliefs on the presumed cause of hypertension, effective treatments, and appropriate health providers [21].
Given the challenges facing public sector healthcare, hypertensive patients often prefer to attend providers closer to home, for instance, community pharmacies or private and proprietary medicine vendors (PPMVs) [22,23]. These providers have an important position within the community and the first line of care, as they are easily accessible and constitute for many patients a cost-effective way of receiving care. The Nigerian Ministry of Health regulates most pharmacy healthcare providers through registration with the Pharmacist Council of Nigeria (PCN) and a variety of associations exist to warrant quality care [24]. Pharmacists are highly educated professionals, yet their skills remain underutilized [18]. According to Nigerian law, they are allowed to dispense prescription drugs, retail, and wholesale medicines [25]. However, pharmacists are often additionally involved in, for example, prescribing drugs over the counter for various illnesses, disease screening and monitoring, identifying drug therapy problems, and health promotion [26].
Pharmacy-based hypertension care that includes remote patient monitoring by cardiologists through mHealth may be an innovative and effective way to improve access to hypertension care and blood pressure control and subsequently contribute to reducing cardiovascular disease in sub-Saharan Africa. To assess the feasibility of such an approach, a pharmacy-based hypertension care model employing mHealth was piloted in Lagos, Nigeria, for 6 months and evaluated in a mixed-methods study. Here we report on the objective to describe patients’ and healthcare providers’ perceptions and practices regarding hypertension, pharmacy-based care, and mHealth to assess the context of facilitators and barriers of implementing this innovative care model. The feasibility of the pilot program, including patient retention, changes in blood pressure, the quality and satisfaction of participants [Nelissen HE, Cremers AL, Okwor TJ, Kool S, Van Leth F, Brewster L, et al. Pharmacy-based hypertension care employing mHealth in Lagos, Nigeria – a mixed-methods feasibility study. Submitted for publication], and the effectiveness of recruitment activities [Nelissen HE, Okwor TJ, Van’t Hoog AH. Effectiveness of blood pressure screening events to recruit patients in a decentralized pharmacy-based hypertension care program in Lagos, Nigeria. Submitted for publication] will be presented elsewhere.
METHODS
Care model
The piloted care model involves remotely monitored hypertensive care services delivered through private community-based pharmacies. Cardiologists remotely monitor patients accessing hypertension care at the pharmacy by review of their blood pressure data, related complaints, and drug prescriptions as through the mHealth app and secure quality of hypertensive care. The pharmacist counsels the patient on drugs and lifestyle interventions, performs routine blood pressure monitoring, and dispenses drugs to the patients. The patients pay a monthly contribution for participating in the pilot program and pharmacists and cardiologists receive a fee for each monitored patient. The care model will be extensively described elsewhere. [Nelissen HE, et al. Submitted for publication].
Study design and data collection
A feasibility study was conducted in Lagos, Nigeria from February 2016 to March 2017. For qualitative data collection, recruitment of 30 hypertensive patients and nine pharmacists took place at the five pharmacies included in the pilot program and additionally in four pharmacies in the neighborhood that provided similar hypertension care but were not included in the pilot. Convenience sampling was used to recruit patients with the help of the pharmacists. Inclusion criteria for patients were age 18 years and above and being on hypertension treatment at one of the pharmacies. Six cardiologists from Lagos University Teaching Hospital (LUTH) were recruited and the chairman of the Association of Community Pharmacists of Nigeria (ACPN) via the researchers in Lagos. About half of all the respondents (five pharmacists, 15 patients, three cardiologists) participated in the pilot program, the other half did not. For the baseline interviews of the feasibility study, only hypertensive patients participating in the pilot program were recruited (Fig. 1). Data was collected by two independent research teams, one trained in qualitative methods and the other in quantitative methods, under supervision of researchers from Lagos and Amsterdam. All respondents were approached in English. Data saturation was considered achieved when no new themes were found indicating that for the qualitative study the number of respondents (N = 68) was sufficient [27].
FIGURE 1.
Feasibility study timeline.
The following data sources were used for our objective to assess patients’ and healthcare providers’ perceptions and practices regarding hypertension, pharmacy-based care, and mHealth:
-
1.
In-depth interviews (IDIs, 30 min to 1.5 h) with 30 patients, nine pharmacists, six cardiologists, and one chairman of the ACPN about perceptions and healthcare seeking practices regarding hypertension. IDIs were semi-structured, using open-ended questions to assess respondents’ own formulation of their experiences and minimize influence of researcher-constructed themes or assumptions [28].
-
2.
Focus group discussions (FGDs, 2–3 h): two with five hypertensive patients each and one with five pharmacists participating in the pilot program to evaluate the barriers and facilitators of the care model. One FGD took place during a qualitative research training with 12 medical doctors to assess why people were reluctant to go to LUTH. An important component of FGDs is group interaction often taking research in unexpected directions [29].
-
3.
At nine pharmacies during different time points of the day (morning, afternoon, evening), observations were conducted without interfering in ongoing activities. Fluctuating amount of customers attending the pharmacy, role of the pharmacy in the community, and relationships between pharmacists and patients were assessed.
-
4.
Structured baseline interviews with 328 patients of whom 206 patients were already in hypertension care before participating in the pilot program. Data on healthcare-seeking behavior for hypertension, transport, time spent, and healthcare expenditure of patients stratified by provider is used [Nelissen HE, et al. Submitted for publication].
Data analysis
Qualitative data was analyzed using thematic content analysis [30]. Research assistants transcribed digital recordings of IDIs, FGDs, and fieldnotes of observations. ALC and research assistants blindly double-coded data and meticulously analyzed content for patterns and meaning using Dedoose Version 7.0.23 (Web application for managing, analyzing, and presenting qualitative and mixed method research data; SocioCultural Research Consultants, LLC, Los Angeles, California, USA). Emerging themes and interpretations were tested by looking for disconfirming cases and variations in the data. Data from the baseline interviews was described by descriptive statistics using Stata version 12 (StataCorp LP, College Station, Texas, USA).
Ethics
Ethical clearance was obtained from the Lagos University Teaching Hospital Health Research and Ethics Committee (reference number ADM/DCST/HREC/APP/635). Respondents gave their written informed consent (in Yoruba or English). Patients included in the pilot program additionally received patient information and privacy statement before consent procedure. Anonymity and confidentiality were maintained throughout the pilot program.
RESULTS
Study group
Observations showed that most pharmacies had a waiting area and consultation room(s) and sold drugs in addition to items such as cosmetics or household items. Pharmacies were frequently visited by patients, with peaks in the morning and late afternoon. Two pharmacists explained they had a shortage of staff. Most pharmacists were registered at a pharmacy association. Pharmacies were located in low-income or middle-income areas. Pharmacists explained most patients lived nearby. Patients participating in IDIs were on average 53.5 years old (range 25–88), 47% were women, and 53% was married. In total, 13% reported not having any education, 30% went to primary and/or secondary school, and 57% had a higher education. About a quarter (27%) had no job or was retired and 37% had their own business. Characteristics of patients participating in the baseline interviews will be reported elsewhere [Nelissen HE, et al. Submitted for publication].
Perceptions of hypertension
Most patients described hypertension as dangerous and a silent killer. As causes of hypertension, patients frequently mentioned pregnancy, heredity, stress, ‘overthinking,’ and trauma after hearing bad news. Often-mentioned symptoms because of high blood pressure were headache, restlessness, inability to sleep, and constipation. Most patients said hypertension is not curable. Few stated it was curable, provided that patients strictly adhered to hypertension treatment, equating cure with stabilization of high blood pressure. All patients mentioned taking drugs, healthy diet, rest, and doing exercise as ways to control high blood pressure. However, during observations, a patient explained: ‘I reject it [hypertension] in Jesus’ name! It is not my portion.’ Pharmacists explained that denying hypertension based on religious beliefs happened occasionally.
Hypertension treatment and adherence
All patients included in the study were on hypertension treatment at one of the pharmacies and recognized the importance of taking antihypertensive drugs. Reasons given were that it was the only way to stay healthy or that it was recommended by God.
We shouldn’t test God, so we should take his recommendation to attend these medical people. The death should not come through my own hand. So that's why I am taking the drugs. (IDI patient)
Some patients did not adhere to prescribed treatment, skipping drugs at times or on a regular basis. The most cited reasons for not adhering were feeling healthy, being fed up taking drugs, and side effects (e.g. impotence). Various pharmacists and patients mentioned ‘the Nigerian factor’ to refer to a widely held local belief that ‘something must be responsible for someone's death’ (IDI pharmacist). The idea was that if someone felt healthy, there was no need to worry too much about his/her health status, because eventually everyone will die one way or another. Various pharmacists and patients explained people did not have or take the time to care for their health: ‘The Nigerian attitude towards healthcare is that they are not taking their healthcare serious. To them it is a waste of money. It is a waste of time’ (IDI pharmacist).
Nevertheless, there were many patients who said anything concerning their health was worth paying for and stressed that antihypertensive drugs were not expensive. Meanwhile, half of the patients faced financial constraints, at times making it difficult to purchase drugs. Pharmacists emphasized that the current economic recession negatively affected patients’ ability to afford drugs. Only two out of 30 patients had a health insurance. Both medical doctors and pharmacists stressed that diagnosis and treatment were relatively expensive.
Pharmacists explained that patients preferred buying foreign drugs, believing that these drugs are of higher quality than those manufactured in Nigeria. At times patients decided to take nothing if they could not afford foreign drugs, despite Nigerian drugs sometimes being twice as cheap. During FGDs, patients described the perceived low quality of local drugs referring to a Nigerian proverb: ‘The soup wey good na money kill am’ (translation: if you want the best, you will use money). ACPN posters of some pharmacies may unintentionally influence this perception, reading: ‘The bitterness of low quality drugs remains long after the sweetness of low price is forgotten’. Many patients expressed their worries regarding the sales of expired or fake (also called chalk). ‘In this pharmacy they don’t sell fake drugs. […] There are very many [pharmacists] that do this. Even if you bring a prescription, some of them sell chalks as a drug’ (FGD patients). In addition, pharmacists stressed that their reputation for selling high-quality drugs is important. ‘We have customers that don’t go anywhere else and come to this place because […] we don’t sell chalk’ (IDI pharmacist).
Pharmacists emphasized their good relations with patients and their influence on their treatment adherence, informing patients about the danger of hypertension and the advantage of regular treatment intake. If blood pressure was low, some pharmacists at times advised patients to pause treatment while keeping an eye on their blood pressure. However, sometimes this led to misunderstandings: ‘Once their [patients’] blood pressure comes down, we tell them to go on drug holiday. But after that, they don’t bother to come back and check. They assume they don’t have it anymore’ (IDI pharmacist).
Hypertension care at the pharmacy
Pharmacies are a popular first point of healthcare. Visiting nearby pharmacies saved patients time and travel costs. Some patients only attended the pharmacy when they experienced symptoms:
If I am feeling a one-sided headache, I will presume that my blood pressure is becoming high and I will just run here. If it is high, they will ask if I am taking my drugs. If I say no, they will say go and continue taking your drugs. I comply with drugs and the headache will go. (IDI patient)
Various patients described the possibility of getting discounts and drugs on credit at the pharmacy and explained this as signs of caring. Pharmacists explained that such financial agreements were possible with hypertensive patients as they are tied for a long time to the pharmacy leading to trustful relations. This way, they could additionally attract more customers and improve drug-adherence.
Pharmacies were appreciated by patients for their small scale and accessibility. The pharmacy was often a place for casual chatting or buying groceries or cosmetics. Most patients explained that they valued having a good relationship with their pharmacist. ‘You could even notice when I came in that all of them [pharmacists] are greeting me here, because we are friends. We deal with ourselves like father and children’ (IDI patient). Pharmacists took time to attend to patients and treated them with respect (observation). Patients explained this gave them the feeling that the pharmacist took good care of their health and was additionally personally involved in their well being. All patients perceived pharmacists as trusted health professionals with substantial expertise and credibility. Some additionally stressed the importance of their pharmacist's registration at a recognized pharmacy association.
I can see that it is not just any shop. It is not a chemist! And that it is being managed by a registered pharmacist. […] It is important to know that the pharmacist is a credible learned person. And that when the medication expires he throws the darn thing out instead of leaving it on the shelf for somebody to buy and die. (IDI patient)
Pharmacists not only fulfilled the role of hypertension care-taker, but additionally functioned as the gateway to the hospital. However, patients often had contradictory expectations regarding this role, as they wanted pharmacists to comply with national-recognized guidelines, but at the same time expected to be diagnosed and taken care of by the pharmacist. Pharmacists described patients were generally reluctant towards the hospital and affirmed that these expectations at times led to tensions.
Pharmacists are accessible. For doctors, you have to go through procedures before you can see them. […] Most of the patients don’t go to the hospital, they don’t get a prescription. We are the ones trying to see what we can do to help them. (IDI pharmacist)
Pharmacists wanted to deliver good quality work, assuring patient visits, patients’ health, and therefore income, but at times were asked to go beyond what they were ought to do. Pharmacists had to balance between providing good care requested by patients and sending those critically ill patients to the hospital. Additionally, they explained they needed to avoid patients thinking complications arose from their management.
Some patients viewed pharmacists as medical doctors, calling them doctor, yet most patients were able to describe the differences between a medical doctor and a pharmacist. The majority of patients said that pharmacists were the next best thing after medical doctors. Overall, patients’ satisfaction with pharmacists regarding hypertension care was high.
Hypertension care at the hospital
Observations at the pharmacies showed that patients generally rejected pharmacists’ recommendations to go to a hospital. Medical doctors participating in an FGD confirmed this finding. Reasons mentioned for avoiding the hospital were time and money needed, because of the distance between patients’ homes and the hospital, traffic, and long queues and waiting times at the hospital. Patients explained during an FGD that the hospital is not a place for a poor person, as a hospital visit led to extra costs related to, for example, transport, tests, consultations, and drugs. Most medical doctors mentioned that the healthcare system at hospitals was not working optimal leading to overcrowding of patients, excessive workload for medical doctors and nurses, and stressful situations. Other reasons for avoiding the hospital included the large scale of the hospital, not knowing anyone, and getting lost. Patients’ perceptions of hospital staff (not only medical doctors, but also nurses, cleaners, etc.) were considered to be negative, referring to rudeness, impatience, and indifferent attitudes. Most patients explained they had the impression that hospital staff would not even care if patients would die on the hospital's doorstep. Various patients, pharmacists, and medical doctors described a widespread distrust among patients towards hospitals, referring to hospitals using poor patients for students to practice on, medical doctors overcharging by over-diagnosing and other suspicions of illicit financial deals at the expense of patients. Medical doctors were aware of patients’ distrust, but stated that they often discovered comorbidities that called for additional procedures. A widespread conviction that the hospital was a place where people died, made many patients fearful of this location.
One time the doctor [pharmacist] asked me if I had been referred to LUTH. I said: God forbid, I won’t be referred to that place in Jesus’ name. […] My brother's wife died in LUTH. Some friends I know died in LUTH because they are not caring. If you don’t know anybody in LUTH, you don’t dare to go there. (FGD patients)
Hypertension care by other healthcare providers
Most patients reported not using alternative ways of treating their hypertension apart from taking antihypertensive drugs and making lifestyle modifications (exercising and a strict diet). Some patients mentioned they additionally took ginger or herbal supplements. Few reported visiting traditional healers for herbal treatment. Various patients used prayers and two patients mentioned they previously had fasted, but explained they ceased this practice as during fasting, a patient was not supposed to take antihypertensive drugs.
Several patients, healthcare providers, and the ACPN chairman mentioned that medical vendors, chemists, and laboratories (where diagnostic tests are done) were for many people the first point of healthcare. They explained that these were cheaper healthcare options, where they often lacked training and registration. ‘So during the recession, it reduced patients’ purchasing power. […] Patients often want to cut cost and go to quacks, because they view the pharmacy as expensive’ (IDI ACPN chairman).
Few patients attended private hospitals. These facilities were perceived more positively than public hospitals, because they had fewer units, were smaller in scale, obtained friendlier staff, and offered shorter waiting times. The costs, however, were higher. Some patients had a ‘family nurse’, also called auxiliary nurse. According to a cardiologist, these nurses received an informal training and certificate from a medical doctor and often started a business with their own clientele having a store or giving home-visits. Nurses employed at hospitals rarely engaged in such businesses, because they would risk losing their license.
Patients’ time and costs for hypertension care providers
The diversity of healthcare providers for hypertension care that patients attended for hypertension care was confirmed in the structured baseline interviews. In total, 206 of the 328 patients were previously diagnosed with hypertension and in care before participating in the pilot program. Of them, 176 patients (85%) reported to have visited a pharmacy for hypertension care, followed by public facilities (32%), private facilities (17%), and PPMVs (4%). Over half (56%) of the patients solely visited a pharmacy, 28% reported to have additionally visited a public facility, 13% a private facility, and 3% went to another facility or combined more facilities. The most important reasons for visiting the pharmacy for hypertension care were familiarity with, and proximity to the provider. Patients who visited private facilities gave similar reasons and additionally mentioned they went there because a specialist was available.
Travel time and travel costs were the highest for patients visiting public facilities and lowest for those visiting pharmacies (Fig. 2). Time spent at public facilities was higher (median: 152 min) compared with private facilities (median: 70 min) and pharmacies (median: 25 min). Difference in costs can be explained by mode of transport: most patients visiting a pharmacy went by foot (61%), patients attending a private facility went by foot (34%) or private car or motorcycle (34%), and patients visiting a public provider often went by bus (48%). At the most recent pharmacy visit, 79% of patients had to pay, at public facilities 58%, and at private facilities 43%. For patient that had to pay, the median total amount spent was lowest at pharmacies and highest at private providers, irrespective of the services they received.
FIGURE 2.
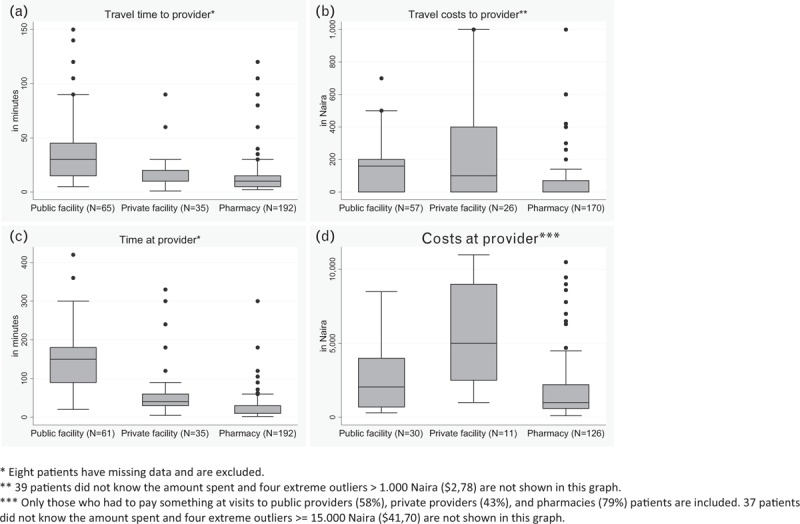
(a-d) Reported cost and time of transportation, and of hypertension care at the most recent visit to a healthcare provider. On the basis of response of 206 patients in the pilot program who had attended hypertension care in the 6 months preceding the interview.
Perceptions of mHealth
Pharmacists and cardiologists were very positive towards (the idea of) remote monitoring of patients through mHealth for providing hypertension care at the pharmacy. Some cardiologists mentioned concerns about Nigeria's readiness for mHealth interventions and the need for a stable internet connection. But in general, they pointed at advantages, such as improved monitoring of patients and bridging the gap between pharmacists and cardiologists. Both cardiologists and pharmacists additionally underlined that patients would mostly benefit from pharmacy-based care with mHealth as it provided them faster, cheaper, and more accessible healthcare. The medical app was only used by cardiologists and pharmacists. Patients enrolled in the pilot program were not involved in the functioning of the medical app and were often unsure about the added value of mHealth to the quality of hypertensive care. Generally among patients, the idea of an mHealth app was unclear. Pharmacists explained that lack of knowledge and understanding may additionally be caused by the often old age of hypertensive patients and associated unfamiliarity with such technology.
DISCUSSION
This study was part of a larger study that investigated the feasibility of pharmacy-based hypertension care including an mHealth app for remote monitoring in Lagos, Nigeria. We assessed the context of facilitators and barriers for implementation of such a model by analyzing patients and healthcare providers’ perceptions and practices regarding hypertension, pharmacy-based care, and mHealth (Table 1). These insights showed that the care model can be considered feasible if targeted at pharmacies that are accessible for the nearby community, already monitor hypertensive patients, have strong patient–pharmacy relationships, and obtain a registration at an association for pharmacists. A clear explanation of the function of mHealth would additionally facilitate implementation. These insights are important to consider for the evaluation of the care model that has been piloted [Nelissen HE, et al. Submitted for publication].
TABLE 1.
Facilitators and barriers of hypertensive patients and healthcare providers that may influence expanding the pilot program of the care model
| Themes | Facilitators | Barriers |
| Perceptions of hypertension | Mainly mentioning of biomedical hypertension cause, such as hereditary, pregnancy, stress, and overthinking | General belief in symptoms of hypertension |
| Belief in efficacy of biomedical treatment for hypertension | Rejection of cheaper local hypertensive drug | |
| Awareness of hypertension's chronic nature and necessity of continuous drug-intake | Patients’ reasons for nonadherence: feeling healthy, being tired of drugs, side effects, not taking health too serious, religious factors | |
| Pharmacy as primary hypertension care provider | Five-year training of pharmacists is of high quality | Double expectations of patients towards role pharmacist: expecting good care, but often refusing hospital referral |
| Patients appreciate pharmacist: trusted relationship, small community, respect, expertise, credibility, trust, registration, small-scale, accessible, proximity, time-efficient, good quality drugs, drugs on credit | Tension for pharmacists: satisfying clientele by not referring too fast to hospitals, delivering good quality care, and functioning as gateway to hospital | |
| Patients consider pharmacists better option than medical doctors or next best thing, reluctance towards hospitals and unregistered pharmacists, chemists, market salesmen selling fake or low-quality drugs (’chalk’) | Half of the patients experienced financial constraints, for some aggravated by the recession in Nigeria and almost no patients having health insurance | |
| Task shifting from medical doctors towards pharmacists reduces costs for public healthcare system and for patients (less travel time, as majority of patients can go by foot and can avoid expensive transport modes, less costs of care) | Competition with cheaper, informal, and often untrained healthcare providers, such as PPMVs, chemists, labs, often providing low-quality hypertension care | |
| Nigerian government and various associations in place that regulate pharmacists to warrant quality care | ||
| Perceptions of mHealth | mHealth enables improved blood pressure monitoring, controlling of nonadherent patients | mHealth is a new thing in Nigeria |
| Bridges the gap between pharmacists and cardiologists | Need for stable internet connection | |
| Combination remote monitoring through mHealth and task-shifting to pharmacies leads to cheaper, faster, and accessible hypertension care for patients | Technology may increase insecurity among some (older) patients |
Regarding perceptions, our study showed that most patients drew on biomedical causes to explain hypertension. In contrast, a study in South-West Nigeria described how some people believed hypertension was caused by an evil spirit and referred to God as the only possible healer [31]. Another study described discordant patient–medical doctor illness perceptions and causes as potential obstacles to hypertension-treatment adherence [14]. In our study, most patients recognized the potentially harmful character of hypertension and the need for hypertension care. This contrasted with other studies in Nigeria stating that most patients considered hypertension curable [32] or treatable with a combination of biomedical and complementary and alternative medicine [33,34]. The fact that patients in our study generally reported biomedical understandings and positively viewed hypertension control through antihypertensive drugs, could be drawn on in efforts to enhance treatment adherence, and thus facilitate the implementation of the care model.
Most hypertensive patients mentioned a variety of biomedical symptoms of hypertension and did not recognize the often silent character of this disease, similar to other Nigerian studies [33–35]. This may partially explain why sometimes patients pause or halt treatment when feeling healthy. However, this may also be because of a lack of funds to purchase medicines. Nevertheless, such perceptions may form a barrier towards the implementation of the care model. Pharmacists are a key player in providing health education that emphasizes the silent and asymptomatic character of hypertension and stimulate patients to regularly take treatment.
An important finding is that the selected pharmacies played a central role in the community. Most patients had a strong preference for hypertension care at a pharmacy. Our patients’ satisfaction with pharmacists’ quality of hypertension care was overall high. This is in contrast with a study in urban South-Nigeria that showed moderate service satisfaction with pharmacies, mostly because of dissatisfaction with provision of nondrug services such as healthcare promotion [36]. Differences in patient satisfaction with pharmacy care may be related to various facilitators, such as the pharmacy having a registration with a recognized Nigerian association, sufficient staff, a consultation room, and a shop offering a wide variety of services and products. Moreover, both IDIs, FDGs, and baseline interviews showed a higher satisfaction with pharmacy care amongst patients living nearby the pharmacy, as they often had personal, trustful relations with their pharmacist. Such pharmacy characteristics and strong pharmacy–patient relationships seemed important elements for patients’ adherence to hypertension care and their perceived high quality of care. Therefore, proximity and access to trusting care relations are key to fostering the success of the care model.
Our study highlighted that both patients and pharmacists had conflicting expectations regarding the pharmacist's role in the community. Officially, pharmacists were limited to dispensing prescription drugs and functioned as the gateway to the hospital, yet patients were generally reluctant to seek care at larger healthcare facilities. Similarly, two Nigerian studies described that most hypertensive patients do not attend hospitals and go to pharmacies instead [20,22]. Pharmacists had to balance between patients’ requests and patients’ health and had to keep their business running. Cardiologists expressed worries about pharmacists taking over the cardiologist's role. The care model may overcome such tensions as pharmacists provide hypertension services using feedback from a cardiologist through an mHealth app. Through this collaborative approach, patients can receive improved quality hypertension care at the pharmacy.
An important barrier to implementing the care model was that half of the patients faced financial constraints while adhering to hypertension care. Our results show pharmacy-based care is less time-consuming and generates far lower opportunity costs to patients making a care model based at pharmacies attractive. Pharmacists and cardiologists described concerns regarding the lack of health insurance and the low socioeconomic status of hypertensive patients aggravated by the recession. In 2005, the National Health Insurance Scheme was implemented [37], yet over 70% of total health expenditure in Nigeria is private out-of-pocket expenditure [38]. A study in rural Nigeria [15] demonstrated that hypertensive patients with health insurance were better monitored, reported good treatment adherence, and incurred lower out-of-pocket expenditures compared with the control group without insurance. The latter group often obtained cheaper, yet poorer quality medication from informal providers. Nigerian healthcare providers also face financial obstacles regarding hypertension care. A study in rural Nigeria on cardiovascular disease prevention showed that task-shifting from medical doctors to nurses reduced direct costs with 42% [39]. Our feasibility study of this care model did not quantitatively investigate the costs of task-shifting from cardiologists to pharmacists and the reduction of cardiovascular disease. Therefore, further research is needed whether costs are reduced for both patients and healthcare providers with this care model. Additionally, this information would be of interest for health insurance providers or other healthcare financers.
In this study, most patients received antihypertensive drugs from the studied pharmacies, but both patients and healthcare providers stressed that pharmacies and their medicines were still for many people too expensive. As a result, for many people the first point of (hypertension) care were PPMVs, chemists, and laboratories. Some studies advocate task-shifting to PPMVs [22]. PPMVs do not need to have formal medical training, although many have been trained and deliver health services complementing the Nigerian healthcare infrastructure [22]. Inclusion of PPMVs in the care model is debatable and would require extensive research regarding the quality of care and the support needed.
An encouraging result was that both cardiologists and pharmacists positively viewed remote monitoring employing mHealth and stressed advantages such as improved cardiologist–pharmacist communication, blood pressure monitoring, and accessibility for patients. With mHealth, we may overcome often-mentioned challenges regarding task-shifting from pharmacists to cardiologists, such as inadequate collaboration and the sharing of patient information [18]. Potential barriers included the fairly new character of mHealth potentially leading to confusion amongst both patients and healthcare providers. Most patients (including those enrolled in the pilot program [Nelissen HE, et al. Submitted for publication]) were unaware of the added value of mHealth. Despite positive attitudes found among cardiologists and pharmacists, the evaluation of the care model's pilot program showed barriers regarding usability of the mHealth app that need to be addressed [Nelissen HE, et al. Submitted for publication].
Strengths and limitations
The use of a wide variety of data collection techniques (IDIs, FGDs, observation) enabled us to gain an in-depth understanding of perceptions regarding hypertension and mHealth, the role of pharmacies, and patients’ healthcare-seeking behavior. The baseline interviews gave additional insights in the healthcare facilities attended by patients, transport mode, and costs emphasizing the time and cost-efficient role of the pharmacist found during qualitative data collection.
The exploratory nature of our study imposes some limitations on our results. We aimed at investigating whether there is a ground to implement a pharmacy-based care model with mHealth. Therefore, we recruited patients at the pharmacy who were often already regularly attending this healthcare provider. Follow-up research could assess whether our results are generalizable to a larger population. We did gain insights regarding the central role pharmacists play in the community. Moreover, our observations at the pharmacies provided us with in-depth data, but a long-term ethnographic study or an economically focused study could have led to more detailed data about every-day circumstances in pharmacies. We have collected data about the role of public, private, and informal healthcare providers, but because of the limited scope of the pilot program no observations have been done at these locations. Future research could include these providers, as they form an important part of healthcare infrastructure in Lagos. Moreover, future research about mHealth may contain probes to better explain the (potential) role of medical apps in healthcare.
In conclusion, we identified various potential facilitators for the implementation of the care model, such as understanding of patients’ biomedical cause and treatment, high satisfaction with pharmacy-based care, pharmacy–patient relationship, pharmacist registration, and cardiologists’ and pharmacists’ positive attitude towards mHealth. Building on these facilitators will help strengthen the care model. The identified barriers included ignorance regarding the silent character of hypertension, nonadherence among some patients, financial constraints, patients seeking care at informal healthcare providers, lack of health insurance, and patients’ unfamiliarity with new technology. Health education and strengthening of the pharmacist's role may address several of these barriers, for example, increase awareness regarding the asymptomatic character of hypertension, importance of continuous drug-intake, and mHealth. Collaboration with health insurance providers or other financing mechanisms may help diminish financial barriers faced by patients.
ACKNOWLEDGEMENTS
We would like to thank all patients, pharmacists, and cardiologists for participating in the feasibility study, CEHD staff for collecting the data, Winny Koster and Marleen Hendriks for their initial input regarding study design, AIGHD staff for the data management and project management, and LUTH, the pharmacies and PharmAccess Nigeria for facilitation in Lagos.
Sources of funding: This feasibility study was funded by OMRON Healthcare Europe through a contract with the Amsterdam Institute for Global Health and Development. The pilot program was funded and implemented by OMRON Healthcare Europe. OMRON Healthcare Europe was not involved in the feasibility study, including the analysis and interpretation of data, the writing of the manuscript nor in the decision to submit the manuscript for publication.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Abbreviations: ACPN, Association of Community Pharmacists of Nigeria; FGD, focus group discussion; IDI, in-depth interview; LUTH, Lagos University Teaching Hospital; PCN, Pharmacist Council of Nigeria; PPMV, private and proprietary medicine vendor
REFERENCES
- 1.The World Health Organization. Global Status Report on noncommunicable diseases 2014. WHO Library Cataloguing-in-Publication Data: 2014. [Google Scholar]
- 2.Ekwunife OI, Aguwa CN. A meta analysis of prevalence rate of hypertension in Nigerian populations. J Public Health Epidemiol 2011; 3:604–607. [Google Scholar]
- 3.Adeyemo A, Tayo BO, Luke A, Ogedegbe O, Durazo-Arvizu R, Cooper RS. The Nigerian antihypertensive adherence trial: a community-based randomized trial. J Hypertens 2013; 31:201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akinroye K. Nigerians wake up to high blood pressure. Bull World Health Organ 2013; 91:242–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens 2015; 33:230–242. [DOI] [PubMed] [Google Scholar]
- 6.Osibogun A, Okwor TJ. Antihypertensive prescription and cost patterns in an outpatient department of a teaching hospital in Lagos State Nigeria. Open J Prev Med 2014; 4:156. [Google Scholar]
- 7.Egbi OG, Ofili AN, Oviasu E. Hypertension and diabetes self-care activities: a hospital based pilot program survey in Benin City, Nigeria. Niger Postgrad Med J 2015; 22:117–122. [PubMed] [Google Scholar]
- 8.Soyemi OI, Hunponu-Wusu OO. Knowledge, attitudes and participation of community pharmacists in Lagos State, Nigeria towards primary healthcare (PHC). J Public Health Epidemiol 2015; 7:15–19. [Google Scholar]
- 9.AbuDagga A, Resnick HE, Alwan M. Impact of blood pressure telemonitoring on hypertension outcomes: a literature review. T Telemed J E Health 2010; 16:830–838. [DOI] [PubMed] [Google Scholar]
- 10.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA 2013; 310:46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sabaté E. Adherence to long-term therapies: evidence for action. World Health Organization. 2003. [PubMed] [Google Scholar]
- 12.Boulware LE, Daumit GL, Frick KD, Minkovitz CS, Lawrence RS, Powe NR. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med 2001; 21:221–232. [DOI] [PubMed] [Google Scholar]
- 13.Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord 2013; 13:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayoade A, Oladipo I. Evaluation of the correlation between self-report and electronic monitoring of adherence to hypertension therapy. Blood Press 2012; 21:161–166. [DOI] [PubMed] [Google Scholar]
- 15.Hendriks ME, Rosendaal NT, Wit FW, Bolarinwa OA, Kramer B, Brals D, et al. Sustained effect of health insurance and facility quality improvement on blood pressure in adults with hypertension in Nigeria: A population-based study. Int J Cardiol 2016; 202:477–484. [DOI] [PubMed] [Google Scholar]
- 16.Economist T. Africa's new Number One. Available at: http://www.economist.com/news/leaders/21600685-nigerias-suddenly-supersized-economy-indeed-wonder-so-are-its-still-huge2014 [Accessed 18 July 2016] [Google Scholar]
- 17.Barnes J, Chandani T, Feeley R. Nigeria private sector health assessment. Country Report USAID; 2008. [Google Scholar]
- 18.Auta A, Strickland-Hodge B, Ma J. Stakeholders’ views on granting prescribing authority to pharmacists in Nigeria: a qualitative study. Int J Clin Pharm 2016; 38:960–967. [DOI] [PubMed] [Google Scholar]
- 19.Afolabi MO, Erhun WO. Patients\’response to waiting time in an out-patient pharmacy in Nigeria. Trop J Pharm Res 2003; 2:207–214. [Google Scholar]
- 20.Erhun WO, Agbani EO, Bolaji EE. Positive benefits of a pharmacist-managed hypertension clinic in Nigeria. Public Health 2005; 119:792–798. [DOI] [PubMed] [Google Scholar]
- 21.Akinlua JT, Meakin R, Fadahunsi P, Freemantle N. Beliefs of healthcare providers, lay healthcare providers and lay persons in Nigeria regarding hypertension. A systematic mixed studies review. PloS One 2016; 11:e0154287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J, Prach LM, Treleaven E, Hansen M, Anyanti J, Jagha T, et al. The role of drug vendors in improving basic health-care services in Nigeria. Bull World Health Organ 2016; 94:267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sieverding M, Liu J, Beyeler N. Social support in the practices of informal providers: the case of patent and proprietary medicine vendors in Nigeria. Soc Sci Med 2015; 143:17–25. [DOI] [PubMed] [Google Scholar]
- 24.Pharmacists Council of Nigeria. Available at: http://www.pcn.gov.ng/index.php [Accessed 18 July 2016]. [Google Scholar]
- 25.Federal Ministry of Health Nigeria. National Drug Policy Nigeria. 2005. Available at: http://collections.infocollections.org/whocountry/en/d/Js6865e/8.html [Accessed 20 July 2016] [Google Scholar]
- 26.Oparah AC, Arigbe-Osula EM. Evaluation of community pharmacists’ involvement in primary healthcare. Trop J Pharm Res 2002; 1:67–74. [Google Scholar]
- 27.Pope C, Ziebland S, Mays N. Qualitative research in healthcare: analysing qualitative data. BMJ 2000; 320:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Britten N. Qualitative research: qualitative interviews in medical research. BMJ 1995; 311:251–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kitzinger J. Qualitative research. Introducing focus groups. BMJ 1995; 311:299–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15:1277–1288. [DOI] [PubMed] [Google Scholar]
- 31.Osamor PE. Healthcare seeking for hypertension in South West Nigeria. MSo 2011; 6:5–10. [Google Scholar]
- 32.Oparah AC, Adje DU, Enato EF. Outcomes of pharmaceutical care intervention to hypertensive patients in a Nigerian community pharmacy. Int J Pharm Pract 2006; 14:115–122. [Google Scholar]
- 33.Taylor KD, Adedokun A, Awobusuyi O, Adeniran P, Onyia E, Ogedegbe G. Explanatory models of hypertension among Nigerian patients at a University Teaching Hospital. Ethn Health 2012; 17:615–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Odusola AO, Hendriks M, Schultsz C, Bolarinwa OA, Akande T, Osibogun A, et al. Perceptions of inhibitors and facilitators for adhering to hypertension treatment among insured patients in rural Nigeria: a qualitative study. BMC Health Serv Res 2014; 14:624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okwuonu C, Emmanuel C, Ojimadu N. Perception and practice of lifestyle modification in the management of hypertension among hypertensives in south-east Nigeria. IJBR 2014; 3:121–131. [Google Scholar]
- 36.Oparah AC, Kikanme LC. Consumer satisfaction with community pharmacies in Warri, Nigeria. RSAP 2006; 2:499–511. [DOI] [PubMed] [Google Scholar]
- 37.Odeyemi I, Nixon J. Assessing equity in healthcare through the national health insurance schemes of Nigeria and Ghana: a review-based comparative analysis. Int J Equity Health 2013; 12:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.WorldBank. Out-of-pocket health expenditure. Available at: http://data.worldbank.org/indicator/SH.XPD.OOPC.TO.ZS?view=chart2014 [Accessed 5 July 2016]. [Google Scholar]
- 39.Hendriks ME, Bolarinwa OA, Nelissen HE, Boers AC, Gomez GB, Tan SS, et al. Costs of cardiovascular disease prevention care and scenarios for cost saving: a micro-costing study from rural Nigeria. J Hypertens 2015; 33:376–684. [DOI] [PubMed] [Google Scholar]


