Supplemental Digital Content is available in the text
Keywords: adolescent, child, diagnosis, hypertension, reference values
Abstract
Objective:
The American Academy of Pediatrics updated Clinical Practice Guidelines (CPG) for screening high blood pressure (HBP) in children and adolescents in 2017. This study aimed to assess differences in HBP classification applying this updated HBP definition in a large sample of Chinese youth.
Methods:
Data from 50 336 youth aged 6–17 participating in the 2013 Chinese national survey were analyzed. HBP was diagnosed according to the established (Fourth Report) and updated (2017 CPG) definitions. The associations between HBP with BMI, height, early life factors and behavioral factors were investigated using logistic regression models.
Results:
Applying the CPG definition, 16.7% of children (6–12 years) and 7.9% of adolescents (13–17 years) had HBP, compared with 10.8 and 6.3% applying the Fourth Report definition. Prevalence estimates for HBP differed the greatest for boys, children aged 11, those with high BMI, and those of tall stature. The odds ratios (ORs) for HBP with BMI, height, hip and waist circumference, early life factors and behavioral factors were comparable for the two definitions.
Conclusion:
The new criteria for HBP in young people will lead healthcare providers to diagnose more children as hypertensive. Notably, associations between HBP with BMI and other medical and behavioral factors remained strong, supporting validity of the new definition.
INTRODUCTION
High blood pressure (HBP), once considered rare in childhood and adolescence, has become a serious public health challenge and increases the risk of end organ damage, including coronary artery calcifications, ventricular hypertrophy, and increased carotid intima–media thickness [1,2]. HBP in childhood can be progressive into adulthood and is the strongest predictor of adulthood HBP [3,4]. It is important to identify HBP early, for controlling and preventing cardiovascular-related diseases.
Identifying pediatric HBP, however, is much more complicated than detecting HBP in adults. Since the ‘Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents’ (Fourth Report) published in 2004 [5], interest in childhood HBP has increased across the world. Though many countries and organizations have established their own childhood BP reference values, such as Canada's 2016 guidelines [6] and the European 2016 guidelines [7], the Fourth Report has been used globally, in the United States and in other nations, including China [8].
In 2017, the American Academy of Pediatrics (AAP) and its Council on Quality Improvement and Patient Safety developed a new pediatric Clinical Practice Guideline (CPG) and updated the diagnosis on childhood HBP [9]. The CPG guideline differs in significant ways from the Fourth Report with respect to the reference population and the clinical definition of childhood HBP. For example, the CPG reference values were established based on normal-weight children, whereas the Fourth Report values were established based on the entire population, at all weight levels, which would lead to the norms for BP in children to continue to increase with the rise in obesity over time [10]. As a result, the sex-specific, age-specific, and height-specific values for screening HBP in the updated CPG are lower than those in the Fourth Report. Another major change is HBP in the Fourth Report was defined as SBP and/or DBP at least 95th percentile (on the basis of age, sex, and height percentiles) in children up to 17 years of age. With the updated CPG, HBP was defined as measured SBP and/or DBP at least 95th percentile of age, sex, and height percentiles for children up to 12 years of age; however, for adolescents aged 13–17 years, HBP was defined as at least 130/80 mmHg, with no adjustment for age, sex, or height [11]. The change for adolescents with the CPG criterion was made to align with cut-points in a new adult HBP criterion developed by the American College of Cardiology and the American Heart Association [12]. BP levels in young people are influenced by height [13]; hence, both the Fourth Report and the updated CPG guidelines for HBP in children, but not adolescents, consider height percentiles.
With the new CPG definition of HBP in youth the implication for clinical practice with consideration of large populations is unknown. Of interest is how prevalence estimates may differ when applying the new CPG standard instead of the established Fourth Report in screening for HBP, overall and by age, sex, height, and BMI subgroups. Further, to the best of our knowledge, research has not assessed whether the new HBP classification has strengthened or weakened associations with risk factors of interest, including BMI, early life factors, behavioral factors, and other factors closely related with HBP [11].
Analyzing a large national cross-sectional survey of children and adolescents in China, the current study aimed to compare HBP prevalence, and to assess the association between HBP with comprehensive related factors, including BMI, height, hip and waist circumference, early life factors, and behavioral factors using different HBP definitions.
METHODS
Study design and study participants
Data analyzed in the current study were collected at baseline in a national multicenter randomized controlled, school-based obesity intervention program conducted in September 2013. The sample was 50 554 children and adolescents aged 6–17 years from seven provinces in China: Liaoning, Tianjin, Ningxia, Shanghai, Chongqing, Hunan, and Guangdong. Using a multistage cluster sampling method, a total of 94 elementary and middle schools were selected to recruit a representative sample of Chinese children and adolescents. Study design and sampling procedures have been reported in detail elsewhere [14,15]. The children and their parents provided signed informed consent, and the protocol was approved by the research ethics committee of Peking University (No: IRB0000105213034). In the current study, only baseline data were included, and 218 participants (0.43%) were removed because of missing data or extreme values of height, weight, or BP (>5 SDs of sex- specific and age-specific means of the survey), leaving 50 336 participants for analysis.
Measurements and definitions
Height (cm), weight (kg), waist circumference (cm), hip circumference (cm), and BP (mmHg) were measured by a team of trained technicians following a standardized procedure. Height was measured to the nearest 0.1 cm with a portable wall-mounted stadiometer, and weight was measured to the nearest 0.1 kg with a standardized scale. Both waist circumference and hip circumference were measured to the nearest 0.1 cm with a steel tape, located at 1 cm above the umbilicus for waist circumference and at maximal protrusion of the buttocks for hip circumference. Height, weight, waist circumference, and hip circumference were measured twice and the mean values were recorded. Both the stadiometers and scales were calibrated before use. BMI was calculated as body weight (kg) divided by height (m) squared (kg/m2). Different BMI groups, including thinness, normal, overweight, and obesity, were classified using the sex-specific and age-specific BMI reference values suggested by the International Obesity Task Force (IOTF) [16,17]. Extreme height groups, including a high-height group and a low-height group, were categorized using sex-specific and age-specific height z scores according to the Centers for Disease Control Growth Charts (www.cdc.gov/growthcharts) [18]. The high-height group was defined as a sex-specific and age-specific height z-score at least 2.0, and the low height group was classified as a sex-specific and age-specific height z-score −2.0 or less; low-middle, high middle, and medium-height groups were classified as −2.0 to −1.0, 1.0 –2.0 and −1.0 to 1.0 of z-scores, respectively.
Waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) were calculated as waist circumference (cm) divided by height (cm) and hip circumference, respectively. Due to the lack of uniform international reference values, high WHR were determined using Chinese sex-specific and age-specific 85th percentile cut-off points [19]. A suitable global boundary value (0.5) was used for classifying high WHtR, which was regarded as a screening tool for the prediction of cardiovascular diseases [20]. Abdominally overweight and obesity were also identified using the international standard based on CDC Growth Chart of sex-specific and age-specific 85th and the 95th percentiles of WC, respectively [21].
Blood pressure (BP) was measured according to the recommendation of the National High Blood Pressure Education Program (NHBPEP) Working Group in Children and Adolescents [5], using an auscultation mercury sphygmomanometer (model XJ1ID, China). The cuff with an inflatable bladder and a width that could cover at least 40% and a length that could cover 80–100% of the circumference of the arm was used. BP was measured after resting at least 5 min in the sitting position. SBP was determined by onset of the first ‘tapping’ Korotkoff sound (K1), and DBP was determined by the fifth Korotkoff sound (K5). An average of three BP measurements at a single occasion was calculated for each child.
The reference values from both the Fourth Report and the updated CPG guideline were applied to define HBP in the current sample [5,11]. In the Fourth Report, HBP was defined as SBP and/or DBP at least 95th percentile on the basis of age, sex, and height percentiles [5]. With the updated CPG, HBP was defined as measured SBP and/or DBP at least 95th percentile of age, sex, and height percentiles for children aged 6–12 years and as at least 130/80 mmHg for adolescents aged 13–17 years [11].
Questionnaire survey
Standard questionnaires completed by participants’ parents assessed demographic information (age, sex, and family income), early life factors and behavioral factors. The self-report measures and methods have been described prior [14,15]. Household economic level was identified by family income, which was divided into four groups on the basis of the ‘household monthly income’ item of this study and subsequently defined as 2000 RMB/month or below (below poverty), 2000–5000 RMB/month (poverty), 5000–8000 RMB/month (middle class), and 8000 RMB/month or above (upper class). Early life factors included birth weight (as recorded on the health clinic card or birth certificate); delivery method (i.e. vaginal versus cesarean); gestational age; feeding patterns (breastfeeding or not); and family hypertension history, as diagnosed by a doctor, in the immediate or extended family. Birth weight was categorized into three groups as normal birth weight (2500–3999 g), low birth weight (<2500 g) and high birth weight (≥4000 g). Gestational age was categorized into three groups as preterm delivery (<37 weeks), normal delivery (37–42 weeks) and postterm delivery (≥42 weeks).
Behavioral factors assessed were dietary behavior, physical activity, and screen time. Dietary behaviors included estimates of the average daily and weekly consumption of fruits, vegetables, meat products, breakfast, fried food (e.g. fried chicken, fried potatoes) and western fast food (e.g. KFC, McDonald's), as well as eating speed. Dietary intakes were categorized according to the dietary guidelines of Chinese school-age children [22]. Cut-points were at least two servings/day of fruits and at least three servings/day of vegetables daily. The weekly frequency cutoffs of fried food and western fast food were 0 time/week versus at least one time/week. The recommended daily intake of meat products is two to three servings/day; hence, we created three categories as follows: less than two servings/day, two to three servings/day and more than three servings/day. Eating speed was assessed by student response to the question, ‘What do you think of your eating speed compared with peers?’ with three options of: ‘slower than peers’, ‘as fast as peers,’ and ‘faster than peers.’ The weekly frequency cutoffs of breakfast were less than 7 days/week versus 7 days/week. Screen time assessed the total time spent watching TV, playing computer or video games, and using the Internet, categorized into two groups: less than 2 h/day and at least 2 h/day, in accordance with the guidelines of the American Academy of Pediatrics [23]. The International Physical Activity Questionnaire (IPAQ) [24] was used to assess daily engagement in vigorous-to-moderate-intensity physical activities, categorized as less than 1 h/day versus at least 1 h/day [22].
Statistical analysis
Descriptive statistics were calculated for all of the measured variables. Differences in HBP prevalence applying the different definitions were tested by Cochran's Q test. Polynomial regression models were run to investigate the HBP prevalence across the BMI or height spectrums in both sexes of two age groups, and the results were presented graphically. The association of HBP with BMI and height (original values), as well as BMI groups and height groups (categorical groups), was assessed by using multivariate logistic regression models with OR and 95% confidence intervals (95% CIs) after adjusting for age, regions, rural/urban areas, household economic level, height (only in BMI groups), birth weight, breastfeeding, delivery method, gestational age, and family hypertension history. As the updated CPG HBP definition adopted different standards in children aged 13 years or less and adolescents aged at least 13 years, the analyses above were stratified by age groups accordingly (aged 6–12 years and 13–17 years, respectively). In addition, multivariate logistic regression models were also performed to assess the association of early life factors, behavioral factors (i.e. dietary behaviors, activity behaviors), and adiposity indicators (i.e. high WHR, high WHtR, and high-waist circumference) with HBP in children using CPG and Fourth Report after adjusting for age, regions, rural/urban areas and household economic level. All analyses were performed with Stata V.14 software (College Station, Texas, USA).
RESULTS
The characteristics of participants are summarized in Table S1 by sex with a total of 25 558 boys and 24 778 girls. Applying the CPG definition, 16.7% of children (6–12 years) and 7.9% of adolescents (13–17 years) had HBP, compared with 10.8 and 6.3% applying the Fourth Report definition (Table 1). In the stratified analysis, the prevalence of HBP was consistently higher applying the CPG than the Fourth Report definition, except in girls aged 13–17 years and in children of short stature. A larger gap between the two definitions was detected in children with obesity and among those of tall stature, especially in boys.
TABLE 1.
Comparison of high blood pressure prevalence according to different definitions in Chinese children and adolescents
| Prevalence (95% CI), % | |||||
| Variables | N | Fourth Report | CPG | Differencea | P† |
| Sample (6–12 years) | |||||
| Sex | |||||
| Boys | 17 912 | 10.9 (10.5–11.4) | 18.1 (17.5–18.7) | 7.2 (6.4–7.9) | <0.001 |
| Girls | 16 550 | 10.7 (10.2–11.2) | 15.3 (14.7–15.8) | 4.6 (3.8–5.3) | <0.001 |
| BMI group | |||||
| Thinness | 3598 | 4.8 (4.1–5.6) | 7.5 (6.7–8.4) | 2.7 (1.6–3.8) | <0.001 |
| Normal | 22 544 | 9.1 (8.7–9.5) | 13.9 (13.5–14.4) | 4.8 (4.2–5.4) | <0.001 |
| Overweight | 5647 | 15.5 (14.6–16.5) | 24.6 (23.5–25.8) | 9.1 (7.6–10.6) | <0.001 |
| Obesity | 2673 | 23.5 (21.9–25.1) | 36.6 (34.8–38.5) | 13.1 (10.7–15.6) | <0.001 |
| Height group | |||||
| High-height group | 1658 | 13.9 (12.2–15.6) | 27.5 (25.3–29.9) | 13.6 (10.9–16.5) | <0.001 |
| Low-height group | 271 | 11.8 (8.2–16.3) | 12.7 (8.9–17.5) | 0.9 (−4.7 to 6.5) | 0.756 |
| Total | 34 462 | 10.8 (10.5–11.2) | 16.7 (16.4–17.1) | 5.9 (5.4–6.4) | <0.001 |
| Sample (13–17 years) | |||||
| Sex | |||||
| Boys | 7646 | 8.0 (7.4–8.6) | 11.4 (10.7–12.2) | 3.4 (2.5––4.4) | <0.001 |
| Girls | 8228 | 4.8 (4.3–5.3) | 4.7 (4.2–5.2) | −0.1 (−0.7–0.6) | 0.776 |
| BMI group | |||||
| Thinness | 1762 | 2.3 (1.6–3.1) | 2.8 (2.1–3.7) | 0.5 (−0.5–1.6) | 0.279 |
| Normal | 11 148 | 4.7 (4.3–5.1) | 5.8 (5.3–6.2) | 1.1 (0.5–1.7) | <0.001 |
| Overweight | 2184 | 11.1 (9.8–12.5) | 13.8 (12.4–15.4) | 2.7 (0.7–4.7) | 0.007 |
| Obesity | 780 | 25.5 (22.5–28.7) | 34.0 (30.6–37.4) | 8.5 (3.9–13.0) | <0.001 |
| Height group | |||||
| High-height group | 142 | 12.0 (7.1–18.5) | 26.1 (19.0–34.2) | 14.1 (5.0–23.2) | 0.002 |
| Low-height group | 396 | 4.8 (2.9–7.4) | 3.4 (1.8–5.8) | −1.4 (−4.2–1.4) | 0.333 |
| Total | 15 874 | 6.3 (6.0–6.7) | 7.9 (7.5–8.4) | 1.6 (1.0–2.2) | <0.001 |
CPG, Clinical Practice Guidelines; HBP, high blood pressure.
aThe difference in HBP prevalence.
†Tested by Cochran's Q test.
With both the CPG and the Fourth Report definitions, the highest prevalence of HBP was observed in children aged 9–11 years relative to other ages (Fig. 1 and Table S2). This age group (9–11 years old) also had the largest difference in HBP prevalence between the CPG and Fourth Report (gaps ranged from 4.2 to 11.2%). By sex, the difference in HBP prevalence for the two different definitions increased with increasing age in boys aged 13–17 years, whereas the difference between the two definitions was quite minor in girls of the same ages.
FIGURE 1.
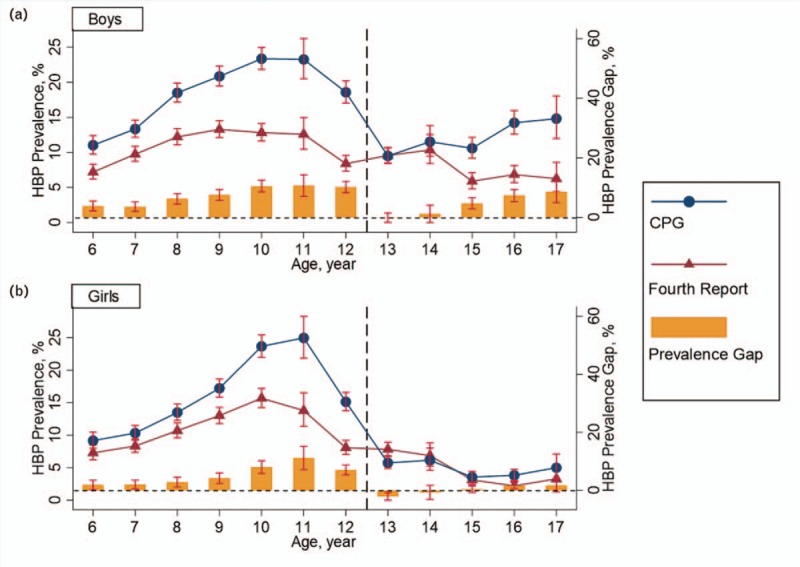
Prevalence of high blood pressure in Chinese boys (a) and girls (b) aged 6–17 years according to definitions of the Fourth Report and Clinical Practice Guidelines. The navy solid lines with circles and maroon solid lines with triangles represent the prevalence using the CPG guideline and the Fourth Report, respectively. The dark-orange bars represent the differences between the two definitions. Error bars represent 95% confidence intervals. CPG, Clinical Practice Guidelines.
For both the CPG and the Fourth Report definitions, the prevalence of HBP increased consistently with increasing BMI z-scores among various sex and age groups (Fig. 2). Except for girls aged 13–17 years, the difference in HBP prevalence between the CPG and Fourth Report definitions became larger with an increase in BMI, especially among young children. The likelihood of HBP is greater with an increase in BMI and more so for the CPG reference values, which were established based on normal-weight children, than for the Fourth Report values, which were established based on the entire population, at all weight levels. Across the height spectrum, a larger difference in HBP prevalence between the two definitions was detected in children who were tall, which was more obvious in young children as well (Fig. 3). Again, however, no statistical difference in HBP prevalence by stature was found in girls aged 13–17 years.
FIGURE 2.
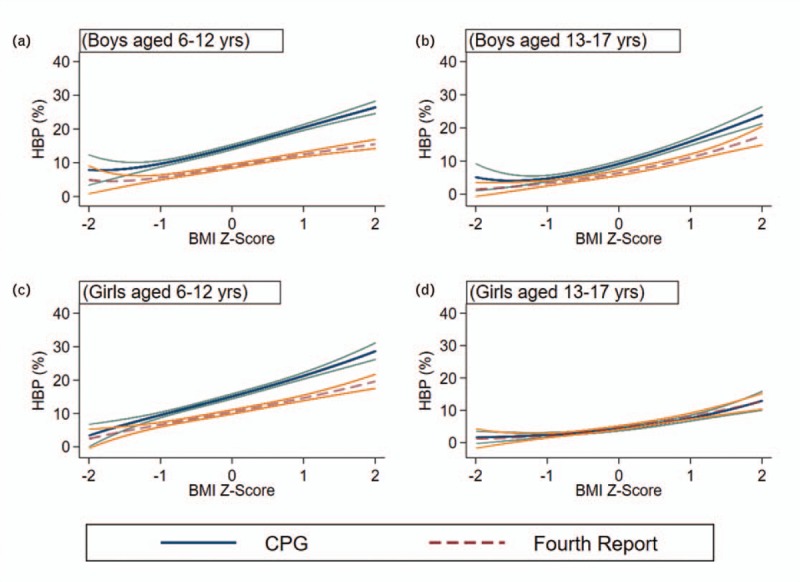
The prevalence of high blood pressure across BMI z-scores according to the different high blood pressure definitions, stratified by sex and age. The navy solid lines and maroon dash lines represent the prevalence according to the CPG and the Fourth Report, respectively. The teal and dark-orange solid lines represent 95% confidence intervals. Comparison of HBP prevalence across BMI z-scores was presented for boys aged 6–12 years (a) and 13–17 years (b), and for girls aged 6–12 years (c) and 13–17 years (d) using two definitions. CPG, Clinical Practice Guidelines; HBP, high blood pressure.
FIGURE 3.
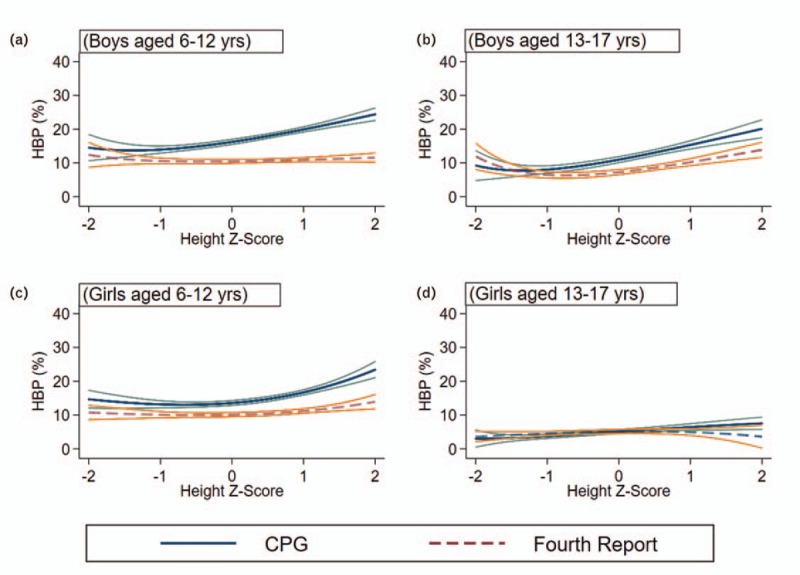
The prevalence of high blood pressure across height z-scores according to the different high blood pressure definitions, stratified by sex and age group. The navy solid lines and maroon dash lines represent the prevalence according to the CPG and Fourth Report, respectively. The teal and dark-orange solid lines represent 95% confidence intervals. Comparison of HBP prevalence across height z-scores was presented for boys aged 6–12 years (a) and 13–17 years (b), and for girls aged 6–12 years (c) and 13–17 years (d) using two definitions. CPG, Clinical Practice Guidelines; HBP, high blood pressure.
Figure 4 shows the association between HBP and BMI after controlling for relative confounders. There was no difference in odd ratios (ORs) between CPG and the Fourth Report HBP guidelines for ORs of HBP with BMI, as well as HBP with height, in different subgroups. For example, the ORs of HBP in thinness, overweight and obesity subgroups were 0.60 (95% CI 0.52–0.69), 1.96 (95% CI 1.80–2.13), and 3.53 (95% CI 3.18–3.92) in both sexes aged 6–12 years using CPG, and the ORs in the same BMI groups were 0.57 (95% CI 0.48–0.68), 1.87 (95% CI 1.69–2.07), and 3.49 (95% CI 3.09–3.93) using the Fourth Report. Similar results were observed in different sex and age groups, and similar patterns were found for the association between HBP and height. (Table S3 and Table S4). Among participants with overweight and obesity, the prevalence of HBP was greater in taller than shorter children. Though this pattern was detected regardless of which definition was used, the difference of HBP prevalence between shorter and taller children was larger when the CPG definition was applied (Table S5).
FIGURE 4.
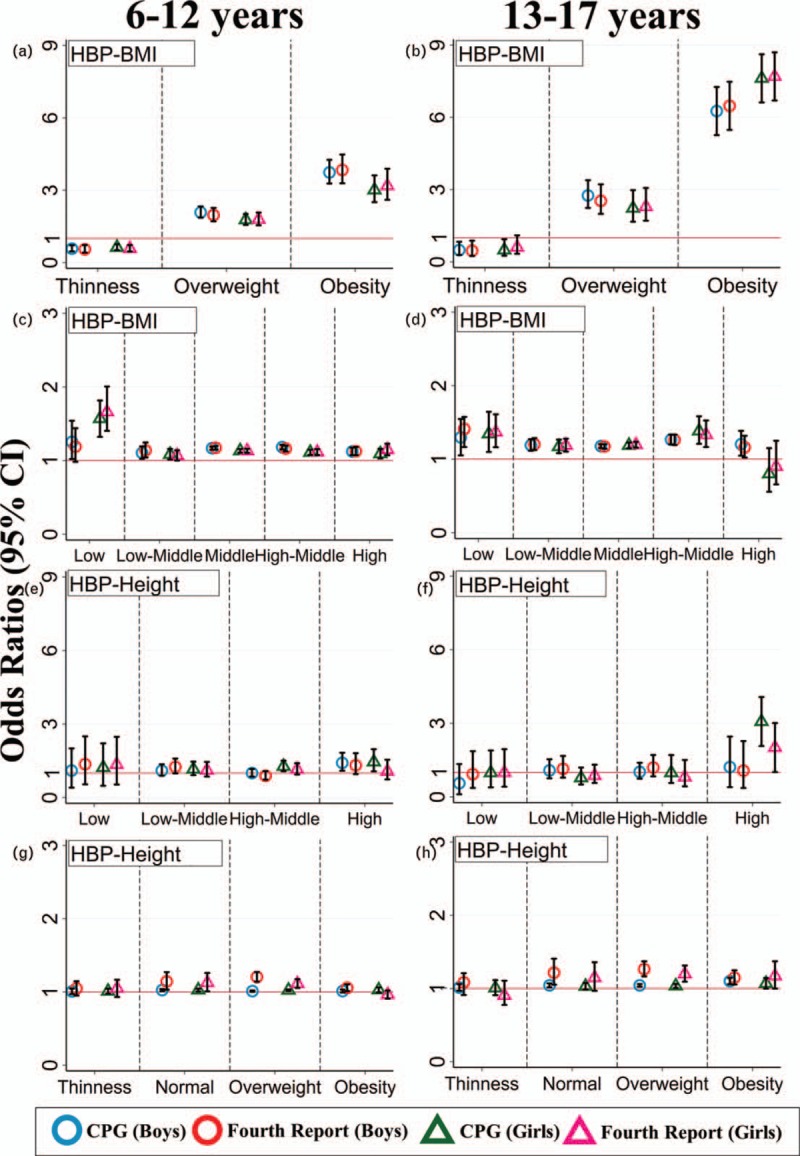
Association between BMI, height, and high blood pressure in different BMI and height groups in both sexes of two age groups using Clinical Practice Guidelines and the Fourth Report. HBP represents high blood pressure; Red lines represents the base line (OR = 1). The ORs in BMI groups (a and b) and height groups (e and f) were calculated based on the normal weight group (categorical variables) and medium height group (categorical variables), respectively after adjusting for age, regions, rural/urban areas, height, birth weight, breastfeeding, delivery method, gestational age, family hypertension history, and household economic level. The ORs between hypertension and original values of BMI (continuous variables), as well as original values of height (continuous variables), were also calculated in different height groups and BMI groups using the two HBP definitions adjusting for the confounders mentioned above (c, d, g, and h). the dots and triangles represent the ORs in boys and girls using two HBP definitions respectively. Stitch lines represent 95% confidence intervals. HBP, high blood pressure; OR, odds ratio.
The associations of HBP with early life factors, behavioral factors, and adiposity indicators were investigated (Table 2). Similar ORs in magnitude and direction were observed for both HBP definitions. For example, boys with preterm delivery had an elevated risk of HBP, with the ORs of 1.66 (95% CI 1.25–2.19) using the CPG definition and 1.92 (95% CI 1.40–2.62) applying the Fourth Report definition. Similar ORs was also observed in the corresponding association for girls. However, for some factors, differences in the magnitudes of the associations were revealed. For instance, whereas the OR of HBP for cesarean delivery was 1.17 (95% CI 1.09–1.25) with the CPG definition, no significant association was observed when the Fourth Report was applied. As for dietary behaviors, similar ORs were observed for both HBP definitions, nonsignificant with consumption of fruits and vegetables and significant for consumption of meat products. Screen time was significantly positively correlated, whereas physical activity in boys only was negatively correlated with HBP, consistent with both definitions. As for adiposity indicators, such as WHR, waist circumference, and WHtR, similar ORs were observed for both HBP definitions.
TABLE 2.
Comparison of the association of early life factors, behavioral factors, and adiposity indicators with high blood pressure using Clinical Practice Guidelines and Fourth Report in both sexes
| Boys | Girls | Total | ||||
| Variables | CPG | Fourth Report | CPG | Fourth Report | CPG | Fourth Report |
| Early life factors | ||||||
| Breastfeedinga | 1.04 (0.90–1.19) | 1.05 (0.89–1.24) | 0.92 (0.79–1.07) | 0.92 (0.78–1.10) | 0.98 (0.89–1.09) | 0.98 (0.87–1.11) |
| Cesarean deliveryb | 1.14 (1.04–1.26) | 0.99 (0.88–1.12) | 1.20 (1.08–1.33) | 1.04 (0.91–1.18) | 1.17 (1.09–1.25) | 1.02 (0.93–1.11) |
| Hypertension historyc | 1.08 (1.01–1.16) | 1.19 (1.06–1.33) | 1.11 (1.03–1.20) | 1.24 (1.09–1.40) | 1.07 (1.02–1.13) | 1.20 (1.10–1.30) |
| Birth weight (reference: 2.5–4.0 kg) | ||||||
| Low birth weight | 0.96 (0.71–1.31) | 0.96 (0.66–1.39) | 0.90 (0.66–1.22) | 1.04 (0.74–1.46) | 0.94 (0.76–1.16) | 1.01 (0.79–1.30) |
| High birth weight | 0.80 (0.71–0.90) | 0.86 (0.74–0.99) | 0.77 (0.68–0.88) | 0.86 (0.74–0.99) | 0.79 (0.72–0.86) | 0.86 (0.77–0.95) |
| Gestational Age (reference: 37–42 weeks) | ||||||
| < 37 weeks | 1.66 (1.25–2.19) | 1.92 (1.40–2.62) | 0.91 (0.62–1.33) | 0.98 (0.64–1.50) | 1.30 (1.04–1.62) | 1.45 (1.13–1.86) |
| ≥42 weeks | 0.85 (0.61–1.19) | 0.94 (0.63–1.39) | 1.17 (0.83–1.64) | 1.38 (0.96–1.98) | 0.99 (0.78–1.25) | 1.14 (0.87–1.49) |
| Dietary behavioral factors | ||||||
| Fruits (<2 serving/day)d | 0.96 (0.87–1.07) | 1.02 (0.90–1.15) | 0.91 (0.81–1.02) | 0.98 (0.86–1.12) | 0.94 (0.87–1.01) | 1.00 (0.91–1.09) |
| Vegetables (<3 servings/d)e | 1.02 (0.94–1.10) | 1.08 (0.98–1.18) | 1.02 (0.94–1.12) | 1.03 (0.93–1.14) | 1.02 (0.96–1.08) | 1.06 (0.98–1.13) |
| Breakfast (<7 days/week)f | 1.07 (0.94–1.22) | 1.15 (0.99–1.35) | 1.07 (0.92–1.24) | 1.14 (0.96–1.34) | 1.07 (0.97–1.18) | 1.15 (1.02–1.28) |
| Fried food (≥1 time/week)g | 1.12 (1.04–1.20) | 1.16 (1.07–1.26) | 1.07 (0.98–1.15) | 1.11 (1.01–1.21) | 1.09 (1.04–1.15) | 1.13 (1.07–1.21) |
| Western fast food (≥1 time/week)h | 1.10 (1.00–1.21) | 1.07 (0.95–1.20) | 1.08 (0.97–1.20) | 1.02 (0.90–1.15) | 1.08 (1.01–1.16) | 1.04 (0.95–1.13) |
| Screen time (≥2 h/day)i | 1.09 (1.01–1.16) | 1.13 (1.04–1.23) | 1.23 (1.14–1.34) | 1.24 (1.13–1.36) | 1.14 (1.09–1.21) | 1.18 (1.11–1.25) |
| Physical activity (<1 h/day)j | 0.90 (0.84–0.97) | 0.90 (0.83–0.98) | 1.07 (0.99–1.16) | 1.04 (0.94–1.13) | 0.98 (0.91–1.05) | 1.03 (0.94–1.12) |
| Meat products (reference: two to three servings/day)k | ||||||
| Less than two servings/day | 1.21 (1.10–1.33) | 1.22 (1.08–1.37) | 1.20 (1.05–1.36) | 1.22 (1.05–1.41) | 1.19 (1.11–1.29) | 1.21 (1.10–1.32) |
| More than three serving/day | 1.18 (1.03–1.34) | 1.10 (0.93–1.29) | 1.20 (1.01–1.42) | 1.27 (1.04–1.54) | 1.18 (1.06–1.30) | 1.16 (1.03–1.31) |
| Eating speed (reference: as fast as peers) | ||||||
| Slower than peers | 0.86 (0.76–0.97) | 0.89 (0.79–0.99) | 0.84 (0.74–0.95) | 0.80 (0.72–0.89) | 0.84 (0.77–0.92) | 0.84 (0.78–0.91) |
| Faster than peers | 1.14 (1.02–1.27) | 1.17 (1.06–1.29) | 1.06 (0.92–1.22) | 1.07 (0.95–1.20) | 1.10 (1.01–1.20) | 1.12 (1.04–1.21) |
| Adiposity indicators | ||||||
| High WHR | 3.01 (2.64–3.43) | 2.79 (2.40–3.25) | 1.63 (1.41–1.89) | 1.73 (1.47–2.04) | 2.29 (2.07–2.52) | 2.23 (1.99–2.49) |
| High WHtR | 3.44 (3.10–3.81) | 3.01 (2.67–3.40) | 2.56 (2.24–2.93) | 2.57 (2.22–2.98) | 3.06 (2.83–3.32) | 2.82 (2.57–3.09) |
| High WC | ||||||
| ABOW | 3.55 (3.05–4.15) | 3.04 (2.55–3.63) | 1.89 (1.23–2.89) | 1.61 (1.00–2.60) | 3.26 (2.85–3.72) | 2.79 (2.40–3.24) |
| ABOB | 4.47 (3.49–5.73) | 3.95 (3.02–5.15) | 2.58 (2.00–3.34) | 2.29 (1.72–3.04) | 3.46 (2.81–4.27) | 3.05 (2.42–3.83) |
Bold text represents that ORs and 95% CI was significant at 0.05 levels. ORs were calculated after adjusting for age, regions, rural/urban areas, household economic level, and BMI groups. ABOB, abdominal obesity; ABOW, abdominal overweight; CI, confidence interval; OR, odds ratio; WC, waist circumference; WHR, waist hip rate; WHtR, waist-to-height ratio.
aReference: not breastfeeding.
bReference: vaginal delivery.
cReference: no history.
dReference: at least two serving (200 g)/day.
eReference: at least three servings (300 g)/day.
fReference: 7 days/week.
gReference: 0 time/week.
hReference: 0 time/week.
iReference: less than 2 h/day.
jReference: at least 1 h/day.
kOne serving of meat products was equivalent to 75 g.
DISCUSSION
Analyzing data from a representative sample of 50 336 children and adolescents aged 6–17 years from seven provinces in China, we found that the new CPG definition of HBP developed with a nonoverweight reference population resulted in a higher HBP prevalence, compared with that defined by the Fourth Report, which was developed with a reference population with children and youths of all body weights. The higher HBP prevalence with the CPG definition was consistently observed in boys and girls, children and adolescents, and in different BMI and height groups, but not in girls aged 13–17 years.
Prior research has confirmed that HBP increases in a graded fashion with increasing adipose tissue [25–27]. Compared with normal-weight children, the odds of HBP increases two-fold in children with obesity and four-fold in children with severe obesity [28]. A reanalysis of the United States BP reference database additionally demonstrated that exclusion of overweight and obese children resulted in HBP reference values that were on average 2–3 mmHg lower than those calculated using the whole database [10]. Given the positive association between obesity and HBP, it could be expected that the decline in HBP reference values would have a greater impact on children with adiposity than those of normal weight. In our study, the gap in HBP prevalence applying the two different HBP definitions increased with increasing BMI in both sexes, conforming to the speculations above. Further, the association between HBP and BMI was stronger in overweight and obese children applying both the CPG and the Fourth Report guidelines, and notably the strength of association with BMI did not differ remarkably between the two HBP guidelines. Thus, using the new CPG definition would draw more attention to the high risk of HBP in children with overweight and obesity, without affecting the association between HBP and obesity compared with previous results using the Fourth Report. That is, being more inclusive (lower screening value for diagnosis) did not reduce the strength of association between obesity and HBP.
A different pattern was shown for adolescent boys than girls. HBP prevalence increased gradually with age applying the CPG guideline in boys, yet steadily decreased in adolescent girls. Generally, the height of boys after puberty still increases through to adulthood with a large amplitude, which is not the case for girls [29,30]. Thus, the effect of height growth on HBP after puberty was small in girls, which could also be observed in the HBP reference values of the Fourth Report. The differential in HBP prevalence observed between the two guidelines was greater for children aged 8–11 years old than the other ages. One reason may be the difference in SBP and DBP reference values for the CPG and the Fourth Report was most pronounced for children aged 8–11 years (as illustrated in Figure S1). Also, the prevalence of overweight and obesity, as well as the sex-specific and age-specific height z-scores in children aged 8–12 years was higher than that in other age groups (as illustrated in Table S6), and the difference in HBP prevalence between the two definitions was larger in those with higher BMI or height. These findings will provide an important reference to clinicians and epidemiologists when using the updated guidelines.
We found that the impact of the CPG guideline on HBP prevalence was greater for children of taller stature. Height is an identified important factor in the process of establishing pediatric HBP references worldwide [5,8–10,31]. A previous study found that a childhood HBP reference that did not consider the impact of extreme height yielded a small number of false positives and a very high rate of false negatives [32]. On the whole, the CPG guideline with a lower screening threshold tended to yield a higher prevalence of HBP in taller youth. This is because the gap of reference values between the two HBP guidelines increased with height percentiles in the comparable population. However, an almost undifferentiated effect of height on HBP occurred in adolescent girls aged 13–17 years applying the two HBP guidelines. The likely reason was that the range of SBP and DBP levels in adolescent girls aged 13–17 years with average height was 124–129 and 81–84 mmHg in the Fourth Report BP reference tables, respectively, which offsets the gap of systolic HBP and diastolic HBP prevalence using the CPG guideline with a constant threshold of 130/80 mmHg. In total, children of tall stature may be more likely to be hypertensive based upon the updated CPG and will warrant more attention from clinicians, especially in boys and young girls.
Early life factors, dietary behavior, physical activity, and other factors play an important role on influencing HBP mechanisms in youth. We found that using two different HBP definitions, preterm delivery, cesarean delivery, and family hypertension history were risk factors for HBP in children, which was consistent with previous studies [33,34]. In the previous review, the relationship between high birth weight and HBP in children and adolescents was inconsistent, with studies reporting positive, inverse, or no associations [35]. The present study found that high birth weight was negatively associated with HBP in children and adolescents with similar odds ratios using THE two definitions after adjusting for current BMI. These findings were inline with Steinthorsdottir's study [36], and current weight could be a potential causal pathway between high birth weight and HBP [15]. In addition, a positive association of cesarean delivery with HBP was found only using the CPG guideline. Prior studies found that children delivered by cesarean had a 52% higher risk of being overweight throughout childhood, which in turn was associated with a higher levels of blood pressure [34].
We also assessed the association of HBP with behavioral factors (i.e. diet and activity), which form the basis of the lifestyle interventions for children with HBP. The updated CPG guideline suggests that the recommendation of diet and physical activity in childhood is similar to that in adults [9]. Although the literature indicates a high intake of fruits and vegetables is associated with lower BP [9], we observed no significant association between fruits, vegetables, and breakfast with HBP risk in the current study applying either HBP definitions. Yet, we found significant associations between HBP and other behavioral factors, such as consumption of fried food, western fast food, meat products and eating speed, screen time, and, for boys only, engagement in regular physical activity. The findings support the influence of lifestyle factors on HBP in children and the need for behavioral interventions.
Our study has several potential implications. First, as the updated CPG definition has lower HBP reference values, more youth will be identified as hypertensive and the threshold for HBP intervention in early life will be lowered, which may lead to a declined risk of target organ damage in childhood [37], and reduced risk of HBP and CVD in adulthood [38–41]. Second, with more youth likely to be identified with HBP, the transition to the new CPG offers an opportunity for improving HBP awareness among healthcare providers of children. Few large surveys have studied HBP awareness in children and adolescents. The SEARCH for Diabetes in Youth study found that only 31.9% of youth aged 3–17 years with type 2 diabetes and 7.4% of youth with type 1 diabetes were aware of their HBP status [42]. Further, a recent survey revealed that only 44.7% of Chinese adults with hypertension were aware of their diagnosis [43]. An even lower HBP awareness is speculated in Chinese young people without comorbid health conditions. Hence, increasing pediatric awareness would be a primary task for regular BP measurement and HBP screening to motivate subsequent intervention and treatment in those with pediatric hypertension [44]. Third, although the updated CPG definition will increase the HBP prevalence, highly consistent associations between HBP and obesity, early life factors, and behavioral factors were detected for both definitions, even after adjusting for several confounding factors. The strong and consistent associations point to relevant targets for prevention and treatment of pediatric hypertension. That more children and adolescents will be identified as hypertensive will result in increased use of pharmacological treatments and costs, especially in children with resistant HBP. However, lifestyle modifications in diet, physical activity, weight, and stress should remain the key approaches according to CPG recommendations.
Study limitations are noted. Firstly, BP levels in our study were obtained at a single visit, which may overestimate the HBP prevalence [45]. Secondly, the reference values of both the Fourth Report and the CPG were based on American children, which may influence its use in the Chinese population. However, the Fourth Report was widely used in previous studies conducted in China, and it is expected that the updated CPG definition will be widely used in Chinese children as well. Data were obtained from seven Chinese provinces geographically located in the north, northeast, central, south, east, northwest, and southwest of China. The participants were recruited to be largely representative of Chinese children and adolescents. The prevalence of overweight and obesity in children (15.6%) and adolescents (6.9%) in the current study was close to that reported nationally (12.1 and 7.3%, respectively) in 2014 [46]. Thirdly, indicators of target organ damage, which were not collected here, warrant investigation in future studies. Finally, measures of early life factors and dietary behavioral factors were self-reported.
In conclusion, on the basis of our comparison analysis using the 2004 Fourth Report and 2017 AAP CPG in a Chinese population, the CPG definition will result in a higher HBP prevalence, especially in boys, children with adiposity, and those of a tall stature. Additionally, the strength of association between HBP and obesity, height, early life factors, and behavioral factors using the CPG definition did not change significantly compared with the results using the Fourth Report. Researchers and clinical practitioners should understand the differences between the two pediatric guidelines for HBP classification and refresh their routine practice. Consistent and strong associations between HBP with BMI, hip and waist circumference, and behavioral factors support the importance of these features as prevention and intervention targets for pediatric hypertension. Future study is warranted to understand the rationality of the updated HBP definition, especially its association with target organ damage and other health consequences in adulthood.
ACKNOWLEDGEMENTS
The authors acknowledge the efforts of the research team members and the participating students, teachers, parents, and local education and health staff.
Information about previous presentations: Neither whole nor part of the work presented in this manuscript was presented in previous articles.
Source of Funding: The present study was supported by the National Natural Science Foundation (81673192) awarded to J.M. and the Excellent Talents Fund Program of Peking University Health Science Center (BMU2017YJ002) awarded to B.D. J.P.'s time was supported by the National Heart, Lung and Blood Institute (R01HL117736).
Author contributors: Y.D. conceptualized and designed the study, completed the statistical analyses, drafted the initial manuscript, and reviewed and revised the manuscript; J.M. and B.D. contributed to the conceptualization and design of the study, supervised the data collection, the statistical analyses and initial drafting of the manuscript, and reviewed and revised the manuscript; Y.S. and Z.Z. assisted with the statistical analyses and reviewed the manuscript; J.J.P. assisted with the statistical analyses and critically reviewed and revised the manuscript; All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Footnotes
Abbreviations: AAP, American Academy of Pediatrics; CPG, Clinical Practice Guideline; FBG, fasting blood-glucose; HBP, high blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; OR, odds ratios; TC, total cholesterol; TC/HDL, total cholesterol/high-density lipoprotein cholesterol ratio
REFERENCES
- 1.Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation 2011; 124:1673–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ingelfinger JR. The child or adolescent with elevated blood pressure. N Engl J Med 2014; 370:2316–2325. [DOI] [PubMed] [Google Scholar]
- 3.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 2008; 117:3171–3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tirosh A, Afek A, Rudich A, Percik R, Gordon B, Ayalon N, et al. Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension 2010; 56:203–209. [DOI] [PubMed] [Google Scholar]
- 5.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114:555–576. [PubMed] [Google Scholar]
- 6.Dionne JM, Harris KC, Benoit G, Feber J, Poirier L, Cloutier L, et al. Hypertension Canada's 2017 guidelines for the diagnosis, assessment, prevention, and treatment of pediatric hypertension. Can J Cardiol 2017; 33:577–585. [DOI] [PubMed] [Google Scholar]
- 7.Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens 2016; 34:1887–1920. [DOI] [PubMed] [Google Scholar]
- 8.Dong Y, Ma J, Song Y, Dong B, Wang Z, Yang Z, et al. National blood pressure reference for Chinese Han children and adolescents aged 7 to 17 years. Hypertension 2017; 70:897–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 2017; 140:e20171904. [DOI] [PubMed] [Google Scholar]
- 10.Rosner B, Cook N, Portman R, Daniels S, Falkner B. Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am J Epidemiol 2008; 167:653–666. [DOI] [PubMed] [Google Scholar]
- 11.Flynn JT, Falkner BE. New Clinical Practice Guideline for the Management of High Blood Pressure in Children and Adolescents. Hypertension 2017; 70:683–686. [DOI] [PubMed] [Google Scholar]
- 12.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 13.Regnault N, Kleinman KP, Rifas-Shiman SL, Langenberg C, Lipshultz SE, Gillman MW. Components of height and blood pressure in childhood. Int J Epidemiol 2014; 43:149–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y, Ma L, Ma Y, Wang H, Luo J, Zhang X< ET-AL>. A national school-based health lifestyles interventions among Chinese children and adolescents against obesity: rationale, design and methodology of a randomized controlled trial in China. BMC Public Health 2015; 15:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dong YH, Zou ZY, Yang ZP, Wang ZH, Jing J, Luo JY< ET-AL>. Association between high birth weight and hypertension in children and adolescents: a cross-sectional study in China. J Hum Hypertens 2017; 31:737–743. [DOI] [PubMed] [Google Scholar]
- 16.Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 2007; 335:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320:1240–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002; 246:1–190. [PubMed] [Google Scholar]
- 19.Zhang YX, Wang SR, Zhou JY, Zhao JS, Chu ZH. Percentiles of waist-hip ratio and the relationship with blood pressure among children and adolescents in Shandong, China. Ann Hum Biol 2014; 41:383–388. [DOI] [PubMed] [Google Scholar]
- 20.Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev 2010; 23:247–269. [DOI] [PubMed] [Google Scholar]
- 21.Fryar CD, Gu Q, Ogden CL. Anthropometric reference data for children and adults: United States, 2007–2010. Vital Health Stat 2012; 11:1–48. [PubMed] [Google Scholar]
- 22.Chinese Society of Nutrition. The dietary guidelines of Chinese school-age children. House PsMP, editor. Beijing: People's Medical Publishing House; 2016. [Google Scholar]
- 23.American Academy of Pediatrics. Committee on Public Education. American Academy of Pediatrics: Children, adolescents, and television. Pediatrics 2001; 107:423–426. [DOI] [PubMed] [Google Scholar]
- 24.Fan M, Lyu J, He P. Chinese guidelines for data processing and analysis concerning the International Physical Activity Questionnaire. Zhonghua Liu Xing Bing Xue Za Zhi 2014; 35:961–964. [PubMed] [Google Scholar]
- 25.Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med 2015; 373:1307–1317. [DOI] [PubMed] [Google Scholar]
- 26.Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. The relationship of body mass index and blood pressure in primary care pediatric patients. J Pediatr 2006; 148:195–200. [DOI] [PubMed] [Google Scholar]
- 27.Lurbe E, Invitti C, Torro I, Maronati A, Aguilar F, Sartorio A, et al. The impact of the degree of obesity on the discrepancies between office and ambulatory blood pressure values in youth. J Hypertens 2006; 24:1557–1564. [DOI] [PubMed] [Google Scholar]
- 28.Parker ED, Sinaiko AR, Kharbanda EO, Margolis KL, Daley MF, Trower NK, et al. Change in weight status and development of hypertension. Pediatrics 2016; 137:e20151662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bonthuis M, van Stralen KJ, Verrina E, Edefonti A, Molchanova EA, Hokken-Koelega ACS, et al. Use of national and international growth charts for studying height in European children: development of up-to-date European height-for-age charts. PLoS One 2012; 7:e42506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zong XN, Li H. Physical growth of children and adolescents in China over the past 35 years. Bull World Health Organ 2014; 92:555–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, et al. 2016 European Society of Hypertension Guidelines for the management of high blood pressure in children and adolescents. J Hypertens 2016; 34:1887–1920. [DOI] [PubMed] [Google Scholar]
- 32.Parker ED, Sinaiko AR, O’Connor PJ, Ekstrom H, Appana D, Amundson J, Kharbanda EO. Potential misclassification of blood pressure status in children and adolescents with short or tall stature. Am J Epidemiol 2016; 183:79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pocobelli G, Dublin S, Enquobahrie DA, Mueller BA. Birth weight and birth weight for gestational age in relation to risk of hospitalization with primary hypertension in children and young adults. Matern Child Health J 2016; 20:1415–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pluymen LP, Smit HA, Wijga AH, Gehring U, De Jongste JC, Van Rossem L. Cesarean delivery, overweight throughout childhood, and blood pressure in adolescence. J Pediatr 2016; 179:111.e3–117.e3. [DOI] [PubMed] [Google Scholar]
- 35.Huxley RR, Shiell AW, Law CM. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J Hypertens 2000; 18:815–831. [DOI] [PubMed] [Google Scholar]
- 36.Steinthorsdottir SD, Eliasdottir SB, Indridason OS, Palsson R, Edvardsson VO. The relationship between birth weight and blood pressure in childhood: a population-based study. Am J Hypertens 2013; 26:76–82. [DOI] [PubMed] [Google Scholar]
- 37.Urbina EM, Khoury PR, McCoy C, Daniels SR, Kimball TR, Dolan LM. Cardiac and vascular consequences of prehypertension in youth. J Clin Hypertens (Greenwich) 2011; 13:332–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387:957–967. [DOI] [PubMed] [Google Scholar]
- 39.Niemirska A, Litwin M, Feber J, Jurkiewicz E. Blood pressure rhythmicity and visceral fat in children with hypertension. Hypertension 2013; 62:782–788. [DOI] [PubMed] [Google Scholar]
- 40.Hao G, Wang X, Treiber FA, Harshfield G, Kapuku G, Su S. Blood pressure trajectories from childhood to young adulthood associated with cardiovascular risk: results from the 23-Year Longitudinal Georgia Stress and Heart Study. Hypertension 2017; 69:435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, et al. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA 2014; 311:490–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rodriguez BL, Dabelea D, Liese AD, Fujimoto W, Waitzfelder B, Liu L, et al. SEARCH Study Group. Prevalence and correlates of elevated blood pressure in youth with diabetes mellitus: the SEARCH for diabetes in youth study. J Pediatr 2010; 157:245.e1–251.e1. [DOI] [PubMed] [Google Scholar]
- 43.Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 2017; 390:2549–2558. [DOI] [PubMed] [Google Scholar]
- 44.Gooding HC, McGinty S, Richmond TK, Gillman MW, Field AE. Hypertension awareness and control among young adults in the national longitudinal study of adolescent health. J Gen Intern Med 2014; 29:1098–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sun J, Steffen LM, Ma C, Liang Y, Xi B. Definition of pediatric hypertension: are blood pressure measurements on three separate occasions necessary? Hypertens Res 2017; 40:496–503. [DOI] [PubMed] [Google Scholar]
- 46.Wang S, Dong YH, Wang ZH, Zou ZY, Ma J. Trends in overweight and obesity among Chinese children of 7–18 years old during 1985–2014. Zhonghua Yu Fang Yi Xue Za Zhi 2017; 51:300–305. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


