Introduction
Vestibular migraine (VM), a common disorder with familiar predisposition, is characterized by recurrent episode of dizziness or vertigo and accompanying symptoms of nausea, vomiting, and/or headaches. The patients with VM may require neurologic, emergency, or otorhinolaryngologic services, and the disorder is often misdiagnosed with posterior circulation ischemia (PCI) or transient ischemic attack (TIA), peripheral vestibular vertigo, Meniere's disease (MD), and multiple (lacunar) cerebral infarctions. Report from population-based study showed that the prevalence of VM was up to 1%,[1] which was one of the common disorders causing dizziness/vertigo, and the rate of misdiagnosis was up to 80%.[2] Thus, a multidisciplinary expert consensus about the definition, characteristics, related work-ups, and diagnostic criteria is needed for the accurate diagnosis and standardized management.
Development of the Concept of VM
In 1917, Boemhei first proposed the concept of “vestibular migraine.” In 1984, Kayan and Hood[3] first described the relationship of migraine and vertigo. Previously, VM was often named as migraine-associated vertigo or dizziness, migraine-related vestibulopathy, migrainous vertigo, benign recurrent vertigo, etc.[4] Different terms for the same disorder were confusing and made the management more difficult.[5] VM is actually a vestibular symptom induced by mechanism(s) related to migraine with vertigo (not migraine with aura) as the main manifestation of VM, which made the disorder less likely to be a subtype of headaches defined by the International Headache Society (IHS). VM had not been defined or studied as a disease entity as MD had been. In 1999, Dieterich and Brandt[6] proposed the concept of VM again; however, it was not accepted widely at the time. Until 2001, Neuhauser et al[7] proposed a diagnostic criteria for VM, which was more liberal than that in international classification of headache disorders (ICHD), and VM as a disease entity, was first defined. In the following 5 to 11 years of studies, the diagnostic criteria showed a positive predictive value of 85%,[8] and then VM was widely accepted. Based on the above diagnostic criteria, the Barany Society listed the diagnostic criteria of VM in the international classification of vestibular disorders (ICVD-1).[9] In 2012, the Barany Society and IHS together launched the concept and diagnostic criteria of VM,[10] and later they were adopted by the third version of diagnostic criteria of ICHD-IIIβ in 2013[11] and by ICHD-III in 2018.[12]
One study showed that the diagnostic rate of VM could be 20%.[13] About 14.5% of neurologists and 19% of ear-nose-throat (ENT) doctors never diagnose VM. The data illustrated the insufficiency of the recognition and diagnosis of VM in clinical practice.
Experts consensus 1: The VM is a common disorder with familiar predisposition, and characterized by recurrence of episodic dizziness or vertigo, which may be accompanied by nausea and vomiting, with or without headaches.
Epidemiology of VM
The VM is one of the common disorders with recurrent vertigo, and the third most common vertigo-related disorder. Due to the insufficiency of recognition, its prevalence has been underestimated.[14] VM can involve patients at any age, and male to female ratio is 1:1.5–5, with a female predominance.[15] One study demonstrated that for females with 40–54 years of age in community-based population, the annual incidence of VM was 5%.[16] Before the publication of the diagnostic criteria of ICHD-IIIβ, VM accounted for 4.2% to 29.3% of the disorders in ENT outpatient service, 6% to 25.1% of the disorders in vertigo outpatient service, and 9% to 11.9% of the disorders in headache outpatient service.[17,18] After the release of VM diagnostic criteria in 2013, a prospective multicenter study in 2016 found that for the patients who first presented in neurologic clinics, the patients with VM and the patients with possible VM accounted for 10.3% and 2.5% of the patients with migraine headaches, respectively.[19] The annual incidence was about 0.89%, and the total population prevalence was 1% [20], 5 to 10 times of that of MD, and was one of the common disorders causing vertigo. Currently, there is no epidemiologic data about VM in China, and limited data showed that it is the second most cause for vertigo, after Benign paroxysmal positional vertigo (BPPV) [2,21].
Expert consensus 2: The VM is one of the most common disorders causing vertigo, with a female preponderance. With the increase of recognition and diagnosis of VM, more of the patients with VM are going to be identified from vertigo related disorders.
Pathogenesis of VM
So far, the pathogenesis of VM is not well known. Hypotheses include cortical spreading depression, neurotransmitter abnormality, trigeminal nerve-vessel dysfunction, ion channel insufficiency, central signal integrating abnormality and genetic abnormality.[22] However, none of the above hypotheses explains all the symptoms and signs of the disorder, with some of them explaining only part of the neurologic deficits of VM. Tendency of familial aggregation has been found for VM in clinical practice, but related studies are sparse. Small studies found that in some families, VM takes autosomal dominant inherence, with penetrance significant lower in male than in female patients and the prevalence significantly higher in female than in male, and sexual hormone may have impact on the prevalence of migraine and VM.[23,24] Most of the patients with VM have a family history, thus, physicians need to carefully ask the history.
Expert consensus 3: The pathogenesis of VM is not well known. The disorder has tendency of familial aggregation. Some female patients with migraine headaches may transform to VM during their menopausal period, which may relate to sexual hormones decline.
Symptoms, Signs of and Work UPS for VM
Symptoms of VM
One study indicated that VM could occur at any age.[25] Either headache or vertigo of VM might present as the initial symptom, which did not occur in a fixed pattern. For most of the patients, headache occurs several years before vertigo, while for some other patients, headache, and vertigo always present simultaneously. A few of the patients might have vertigo earlier than headache, and very rarely patients might have recurrent vertigo or dizziness without headache. VM without aura is more common. The mean age of onset was 37.7 years for female and 42.4 years for male according to a report from other country.[15] A small scale study in China showed that mean age of onset for patients with migraine was 32.7 ± 10.5 years, and the mean age of onset for patients with VM vertigo was 36.6 ± 10.3 years.[26] A different study, however, found that the mean age of vertigo onset for patients with VM was 52.1 years.[27]
Stress, fatigue, anxiety, lack of sleep, excessive physical activities, and some specific food may trigger the attack of VM. The relationship of vestibular symptoms and migraine headache varied greatly among individuals,[10,28,29] and also with age. For example, patients with adolescent benign paroxysmal vertigo might have headache or VM with the growing of age. For some of the female patients with VM, their migraine headache might become less severe or even disappear after menopause, with frequent vertigo attacks as the main manifestation. Thus, for middle-aged and older female with vertigo attacks, history of migraine should be carefully inquired.
It should be noted the diversity of clinical manifestations in the patients with VM. The same patient may present differently at different age or in different attacks. The symptoms and signs in several close attacks may also be different. Vestibular symptoms of VM include vertigo/dizziness, nausea, vomiting, and unsteady gait.[30] Some of the patients with VM have head movement intolerance, neck uncomfortableness, mood disorder, etc. A few of the patients with VM may have transient hypacusis during the attacks. The clinical features of the VM outpatients in China are similar to those reported from other countries. Spontaneous vertigo is the primary type, and the episodes may last from seconds to days. Vertigo during initial attacks are often spontaneous, and then can be triggered by head movement or visual stimulus with the progress of the disease. The duration of vertigo attacks varies greatly among patients. A small study found that vertigo might persist minutes, hours, days, or seconds in 30%, 30%, 30%, and 10% of the patients, respectively.[1] Most of the attacks of VM lasted <72 h,[11,31] of which more were within 24 to 72 h. Visual aura or symptoms of VM may include palisade-, water wave-, zigzagging-, cloud-, or lighting-like lines. Sound and/or light stimulus might aggravate the vertigo of the patient, and the patients might have accompanying photophobia and phonophobia during attacks,[32] and prefer to stay in calm, quiet and dark rooms. In addition, it is effective for alleviating the symptoms with the patient staying in quiet room. Sound, light and head movement may make the vestibular symptoms worse. Attacks of VM may be complicated by sleep, mood, and anxiety disorders. Some VM may have comorbid vertigo of other somatic disorders.
Expert consensus 4: The patients with VM present mainly with vertigo/dizziness, and the mean age of first presentation is older than that of migraine. It should be noted the diversity of clinical manifestations of the patients with VM, and the same patient may present differently at different age or in different attacks. The diverse clinical manifestations of VM may also have comorbid vertigo of other disorders. For the middle-aged and older patients with chief complaint of vertigo/dizziness in outpatient clinics and emergency department, history of migraine headache or other types of headaches should be inquired.[33] The family history of migraine headache and VM should also be emphasized.
Signs of VM
The VM lacks specific signs. During the attack of VM, transient body imbalance, various types of nystagmus, and visual field deficits etc can occur. It is difficult to distinguish these nystagmus with those of peripheral, central, or mixed vestibular abnormalities.[32] It was reported that 70% of the patients with VM had pathologic nystagmus, including spontaneous, positional nystagmus, or gaze-evoked nystagmus, and the nystagmus could be induced by positional test. Spontaneous nystagmus occurred in 19% of the patients.[34] Central and peripheral vestibular dysfunction accounted for 50% and 15% of the patients with VM, respectively, with unclear locations involved in the remaining 35% of the patients.[32]
During the attacks of VM, vestibular dysfunction could be detected, that is, gaze-induced nystagmus, central positional nystagmus, spontaneous nystagmus, comprised unilateral vestibular function and vestibular-occular reflex inhibition failure, etc.[35,36] The abnormal neuro-oto signs are dynamic, and the opportunity for finding the abnormal eye movements increases significantly with multiple follow-ups.[37]
Expert consensus 5: VM lacks specific signs. During and in-between the VM attacks, transient signs may occur, which should be carefully examined and detected during then patients’ initial interview and follow-ups.
Work-ups for VM
In approximately 10% to 20% of the patients with VM, vestibular functioning test is helpful in identifying the decrease of unilateral vestibular function. During the vertigo attacks, some of the patients may complain hypacusis subjectively; however, electro-audiogram for most of the patients does not show any hearing impairment. On the contrary, a few of the patients did suffer from mild hearing impairment.[38,39] Vestibular function test can help detect the peripheral, central, or mixed vestibular nystagmus, which indicates that VM can compromise the peripheral or central vestibular function. For some of the patients, caloric test demonstrates palsy of semicircular canal or unilateral preponderance, indicating comprised function of semicircular canal. The 11% to 15% of the patients with VM show abnormality with video-head-impulse.[40] Inner ear anatomical abnormality associated vertigo can be detected with vestibular myogenic evoked potential test; however, it is non-specific.[41,42] In 2 small studies,[25,43] images on magnetic resonance imaging (MRI) FLAIR showed multiple white matter hyperintense foci in subcortical white matter and centrum ovale (not considered as lacunae infarction), suggesting imaging changes of VM on MRI.
Expert consensus 6: The MRI and other ancillary findings for VM are non-specific; however, they are necessary for the differential diagnosis with other disorders.
Diagnosis and Differential Diagnosis Flowchart for VM
Diagnosis flowchart
Due to the “diversity” of its clinical manifestations, VM often mimics other recurrent episodic dizziness disorders; thus, the differential diagnosis is very important. In one aspect, we should master the diagnostic criteria for vertigo/dizziness disorders,[44] and in another aspect, we can make the differential diagnosis based on the recurrent features of VM. For the convenience of differential diagnosis with other vertigo/dizziness disorders, the following VM diagnosis and differential diagnosis work flow can be used as a reference [Figure 1], and the appropriate work ups and the diagnosis are done mainly based on the different clinical manifestations. It is doable and can be used by general practitioner.
Figure 1.
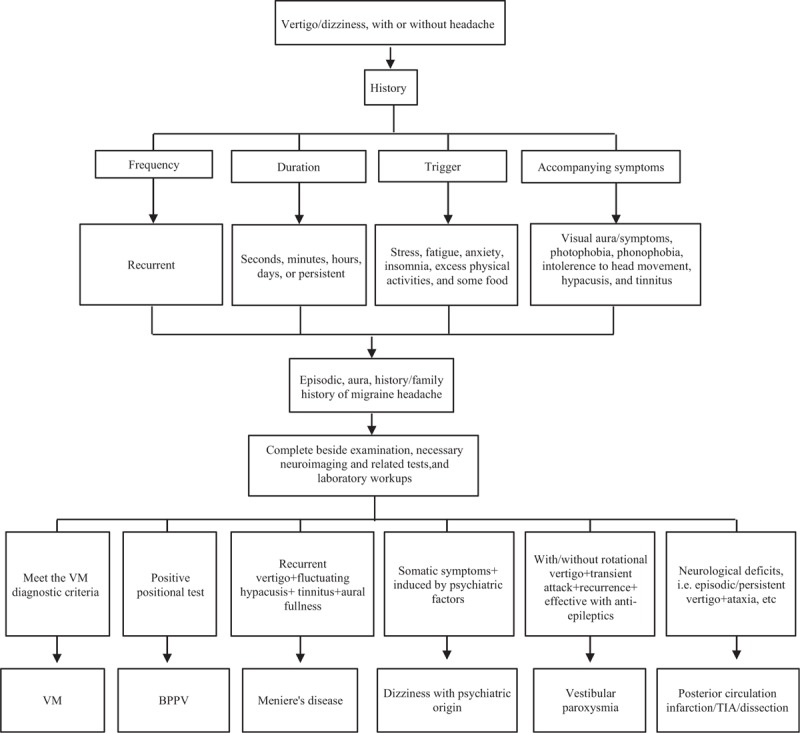
VM diagnosis and differential diagnosis work flow. VM: Vestibular migraine; BPPV: Benign paroxysmal positional vertigo.
Differential diagnosis
-
(1)
BPPV: BPPV is most common disorder with recurrent vertigo. Its diagnosis mainly rely on the Dix-Hallpike and the supine roll test.[45] Complete diagnosis also include work-ups on the involved semicircular canal and pathophysiologic studies (otolithiasis and cupulolithiasis). The diagnosis of BPPV needs positional tests, which can induce nystagmus of the tested semicircular canal. The data needed for the diagnosis include latent period, direction and duration of the nystagmus. Usually, if other inner ear diseases are suspected, vestibular and acoustic tests should be performed. For the patients with typical BPPV, imaging studies of brain and ear are not necessary. The disorder is somehow self-limiting, and manipulative reduction is an effective approach to management of BPPV attack.
-
(2)
Meniere's disease: MD is a disease of inner ear with unclear etiology, and its pathology is endolymphatic hydrops within membranous labyrinth. Clinical manifestations include episodic vertigo, fluctuating hypacusis, tinnitus, and/or aural fullness.[46] The diagnosis of MD mainly relies on history taking and physical examination, and the above 4 typical symptoms may occur in sequence or overlapping. However, in the early stage of the disease these symptoms do not occur simultaneously, which makes the differential diagnosis with VM difficulty.[46] In addition, approximately 13% of patients with MD may have comorbid VM.[47]
-
(3)
PCI: PCI includes infarction and TIA, which can be caused by easily overlooked etiologies such as arterial dissection. Vertigo in these settings is life threatening and severely disabling, thus it is called malignant vertigo. Typical PCI is characterized by episodic or persistent dizziness and imbalance, and the symptoms mostly last minutes to hours, or even persistently. Dysarthria, diplopia, deficit of visual field, and other neurologic deficits may occur simultaneously or with the progress of the disease. When isolated vertigo occurs as the initial symptom of the disorder, it is difficult to distinguish PCI from VM and other benign inner ear disorders. Thus, for middle-aged and older patients with cardiovascular risk factors, PCI should be considered when dizziness or vertigo is persistent,[48,49] avoiding mutual misdiagnosis. Assessment of the cerebral blood vessels with magnetic resonance angiography, digital substract angiography, and MRI perfusion imaging are necessary for the evaluation of PCI.
-
(4)
Non-structural dizziness disorders: This disorder consists of functional dizziness and psychiatric dizziness, manifesting as subjective dizziness or vertigo exacerbated by active motion or postural challenges, and actually this feeling is illusional. Clinical features of non-structural dizziness are persistent dizziness/vertigo on a daily basis and may be accompanied by panic attack and other somatic symptoms such as palpitation, choking, and shortness of breath, as well as sleep disorder and dyspepsia. Dizziness/vertigo is not obvious when distracted or during exercise, but obvious when resting. Disease course is usually ≥3 months, and is often induced by other diseases, mood swings, and the symptoms fluctuate with mood.
-
(5)
Other rare episodic vertigo: such as epileptic vertigo, migraine with brain stem aura, vestibular neuritis, multiple sclerosis, vestibular paroxysm, etc. The diagnoses of these disorders also need careful history inquiring, physical examinations, and appropriate work-ups for direct or indirect evidence.
Expert consensus 7: The diagnostic criteria for VM require 5 or more episodes of moderate to severe symptomatic vestibular attacks, emphasizing the multiple and recurrent attacks of vestibular symptoms Five or more episodes lack statistical evidence. For patients with definite family history of migraine headache or previous migraine headache attacks, who present with the first episode of vestibular vertigo, VM should be considered. The diagnosis and differential diagnosis flowchart is helpful for identifying the etiology of recurrent dizziness/vertigo.
Management of VM
Although the prevalence of VM is high, there is no good quality clinical trial for this disorder because its concept and diagnostic criteria have not been released until recently. Up to now, the management of VM mainly still follows the guidelines for migraine headache, and is classified as symptomatic (ictal phase) and preventive (interictal phase). To prevent VM attacks, we emphasize a comprehensive approach, avoiding inducible factors, modifying life style and abiding by a regular work and resting style, such as making sure to get enough sleep and avoiding food that can trigger the attacks (food containing tyrosine, glutamate, and red wine).[10] Vestibular system rehabilitation can be conducted when necessary, which is helpful to improve the insight and objective balance of the patients with VM with comorbid anxiety and depression.[50,51] Patient education helps the patients understand the disorder, and reduces the anxious mood toward the disorder, which is useful for the patients to handle the symptoms.[52,53]
-
(1)
Pharmacotherapy of the symptoms: the goal of the management is to control symptoms such as vertigo and nausea, with triptans and vestibular inhibitors. Sedatives may also be used as needed. Vestibular inhibitors, such as promethazine and dimenhydrinate, can alleviate vertigo and vomiting during acute attacks.
-
(2)
Preventive medications: the management of VM in this phase is consistent with the principles for migraine headache. Preventive medications should be considered based on the frequency, duration, severity of the attacks, and their impact on the quality of life. Options of medications include β-blocker (propranolol, metoprolol), calcium channel antagonist, antiepileptics (valproic acid, topiramate), and medications for symptoms management, that is, Gastrodin (Tian Xuan Qing),[54] Nicergoline,[55] etc. Some of the patients may have anxiety or depressive disorder due to recurrent attacks and unsatisfied management of VM, and some of the patients may have somatic transformation, presenting somatic symptom of dizziness.[56] Anxiety and depression need clinical assessment and management with appropriate medications.
Symptomatically, VM equals to “wind vertigo,” “intermittent headache,” or “migraine” in traditional Chinese medicine. The disease is located in the head orifices, and the etiology involves exogenous and endogenous factors. Endogenous factors, such as Yang wind, phlegm-turbid, blood stasis, blood-insufficiency, kidney weakness etc, are the main causes of the disorder, which is induced by exogenous 6 evils of wind, coldness, summer hotness, humidity, dryness, and fire, or fatigue, excessive food intake, and emotional stressors. The treatment should abide by syndrome differentiation, and management of symptoms in acute phase and of causes in chronic phase. Studies in China[57-59] showed that based on the frequency of attacks and disability in acute and chronic phases, sequential or oral tianshu capsule alone is effective, which dispel and eliminate wind, resolve sputum, facilitate the circulation of blood and enrich consumption, etc, to relieve pain and vertigo.
Expert consensus 8: In acute phase of VM, the treatment of VM is mainly symptomatic management. For patients with frequent attacks and severe symptoms which comprise the patients’ daily living, preventive treatment is necessary and the management should follow the approaches to the management of migraine headache. At the same time, associated psychiatric disorders should be taken seriously, which need assessment and treatment.
Committee of specialists
Li-Yi Wang (Department of Otolaryngology, Beijing Hospital); Xin Ma (Department of Otolaryngology, Peking University People's Hospital); Jun-Ru Tian (Department of Neurology, University Of California Los Angeles); Jian-Hua Zhuang (Department of Neurology, Changzheng Hospital of Second Military Medical University); Bo Liu (Department of Otolaryngology Head and Neck Surgery, Beijing Tongren Hospital of Capital Medical University); Ming Ren (Clinical Research Center, Xuanwu Hospital of Capital Medical University); Feng Qiu (Department of Neurology, the Sixth Medical Center, Chinese PLA General Hospital); Zhi-Gang Chen (Dongfang Hospital of Beijing University of Chinese Medicine); Xing-Quan Zhao (Department of Neurology, Tiantan Hospital of Capital Medical University); Xiao-Kun Qi (Department of Neurology, the Sixth Medical Center, Chinese PLA General Hospital); Zi-Dong Jiang (Department of Otolaryngology, Peking Union Medical College Hospital); Jun-Liang Han (Department of Neurology, Xijing Hospital of Air Force Medical University); Yi Ju (Department of Neurology, Tiantan Hospital of Capital Medical University); Kai Wang (Department of Neurology, PLA 305 Hospital); Wei Wang (Department of Otolaryngology Head and Neck Surgery, Tianjin First Center Hospital of Nankai University); Wu-Qing Wang (Department of Otolaryngology, Eye and ENT Hospital of Fudan University); Jin Fu (Department of Neurology, the Second Affiliated Hospital of Harbin Medical University); Qing Sun (Department of Otolaryngology Head and Neck Surgery, the Third Medical Center, Chinese PLA General Hospital); Xin-Yu Sun (Department of Psychiatry, Peking University Sixth Hospital); Zhong-Shi Li (Department of Orthopaedic, China-Japan Friendship Hospital); Xin-Yi Li (Department of Neurology, Shanxi Dayi Hospital of Shanxi Academy of Medical Sciences); Xiao-Hong Li (Department of Neurology, Dalian Municipal Friendship Hospital of Dalian Medical University); Jun Wu (Department of Neurology, the First Affiliated Hospital of Zhengzhou University); Yong-Bin Song (Department of Neurology, Xinjiang General Hospital of PLA); Tai-Sheng Chen (Department of Otolaryngology Head and Neck Surgery, Tianjin First Center Hospital of Nankai University); Yu-Hua Chen (Department of Neurology, Wuhan Brain Hospital); Xu Yang (Department of Neurology, Aerospace Center Hospital); Zhi-Wei Wang (Department of Neurology, the Sixth Medical Center, Chinese PLA General Hospital); Qi-Feng Guo (Department of Neurology, the Sixth Medical Center, Chinese PLA General Hospital); Xue-Wen Fan (Department of Neurology, General Hospital of Ningxia Medical University); Gui-Ping Zhao (Department of Neurology, Peking University First Hospital); Chun-Li Zhao (Department of Otolaryngology, Hospital of Tsinghua University); Chi Zhong (Department of Neurology, Weifang People's Hospital); Li-An Huang (Department of Neurology, the First Affiliated Hospital of Jinan University); Yong-Hui Pan (Department of Neurology, the First Affiliated Hospital of Harbin Medical University).
Funding
This study was supported by a grant from New technology and New Business Fund (No. HZXJS[2016]-8) from the Sixth Medical Center, Chinese PLA General Hospital (Formerly known as Navy General Hospital).
Conflicts of interest
None.
Footnotes
How to cite this article: Stroke and Vertigo Association of Chinese Stroke Association. Multidisciplinary experts consensus for assessment and management of vestibular migraine. Chin Med J 2019;132:00–00. doi: 10.1097/CM9.0000000000000064
Contributor Information
Collaborators: Stroke and Vertigo Association of Chinese Stroke Association and Stroke and Vertigo Association of Chinese Stroke Association
References
- 1.Stolte B, Holle D, Naegel S, Diener HC, Obermann M. Vestibular migraine. Cephalalgia 2015;35:262–270. doi: 10.1177/0333102414535113. [DOI] [PubMed] [Google Scholar]
- 2.Dieterich M, Obermann M, Celebisoy N. Vestibular migraine: the most frequent entity of episodic vertigo. J Neurol 2016;263:S82–S89. doi: 10.1007/s00415-015-7905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain 1984;107:1123–1142. doi: 10.1093/brain/107.4.1123. [DOI] [PubMed] [Google Scholar]
- 4.Jiang ZD. Interpret the diagnostic criteria for vestibular migraine (in Chinese). Chin J Neurol 2013;46:567–568. doi: 10.3760/cma.j.issn.1006-7876.2013.08.019. [Google Scholar]
- 5.Jiang ZD. Revisiting issues associated with vestibular migraine (in Chinese). Chin J Otol 2016;14:486–489. doi: 10.3969/j.issn.1672-2922.2016.04.011. [Google Scholar]
- 6.Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol 1999;246:883–892. doi: 10.1007/s004150050478. [DOI] [PubMed] [Google Scholar]
- 7.Neuhauser H, Leopold M, von Brevern M, Arnold G, Lempert T. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology 2001;56:436–441. doi: 10.1212/WNL.56.4.436. [DOI] [PubMed] [Google Scholar]
- 8.Radtke A, Neuhauser H, von Brevern M, Hottenrott T, Lempert T. Vestibular migraine–validity of clinical diagnostic criteria. Cephalalgia 2011;31:906–913. doi: 10.1177/0333102411405228. [DOI] [PubMed] [Google Scholar]
- 9.Bisdorff A, Von Brevern M, Lempert T, Newman-Toker DE. Classification of vestibular symptoms: towards an international classification of vestibular disorders. J Vestib Res 2009;19:1–13. doi: 10.3233/VES-2009-0343. [DOI] [PubMed] [Google Scholar]
- 10.Lempert T, Olesen J, Furman J, Waterston J, Seemungal B, Carey J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res 2012;22:167–172. doi: 10.3233/VES-2012-0453. [DOI] [PubMed] [Google Scholar]
- 11.Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 12.Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia 2018;38:1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 13.Millen SJ, Schnurr CM, Schnurr BB. Vestibular migraine: perspectives of otology versus neurology. Otol Neurotol 2011;32:330–337. doi: 10.1097/MAO.0b013e3182040b21. [DOI] [PubMed] [Google Scholar]
- 14.Yollu U, Uluduz DU, Yilmaz M, et al. Vestibular migraine screening in a migraine-diagnosed patient population, and assessment of vestibulocochlear function. Clin Otolaryngol 2017;42:225–233. doi: 10.1111/coa.12699. [DOI] [PubMed] [Google Scholar]
- 15.Sohn JH. Recent advances in the understanding of vestibular migraine. Behav Neurol 2016;2016:1801845 doi: 10.1155/2016/1801845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hsu LC, Wang SJ, Fuh JL. Prevalence and impact of migrainous vertigo in mid-life women: a community-based study. Cephalalgia 2011;31:77–83. doi: 10.1177/0333102410373152. [DOI] [PubMed] [Google Scholar]
- 17.Geser R, Straumann D. Referral and final diagnoses of patients assessed in an academic vertigo center. Front Neurol 2012;3:169 doi: 10.3389/fneur.2012.00169. eCollection 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vuković V, Plavec D, Galinović I, Lovrencić-Huzjan A, Budisić M, Demarin V. Prevalence of vertigo, dizziness, and migrainous vertigo in patients with migraine. Headache 2007;47:1427–1435. doi: 10.1111/j.1526-4610.2007.00939.x. [DOI] [PubMed] [Google Scholar]
- 19.Cho SJ, Kim BK, Kim BS, Kim JM, Kim SK, Moon HS, et al. Vestibular migraine in multicenter neurology clinics according to the appendix criteria in the third beta edition of the international classification of headache disorders. Cephalalgia 2016;36:454–462. doi: 10.1177/0333102415597890. [DOI] [PubMed] [Google Scholar]
- 20.Neuhauser HK, Radtke A, von Brevern M, Feldmann M, Lezius F, Ziese T, et al. Migrainous vertigo: prevalence and impact on quality of life. Neurology 2006;67:1028–1033. doi: 10.1212/01.wnl.0000237539.09942.06. [DOI] [PubMed] [Google Scholar]
- 21.Muelleman T, Shew M, Subbarayan R, Shum A, Sykes K, Staecker H, et al. Epidemiology of dizzy patient population in a neurotology clinic and predictors of peripheral etiology. Otol Neurotol 2017;38:870–875. doi: 10.1097/MAO.0000000000001429. [DOI] [PubMed] [Google Scholar]
- 22.Sun SF, Si NN, Su LM. Advances in genetic studies on the pathogenesis of vestibular migraine [in Chinese]. Chin J Otol 2018;16:307–311. doi: 10.3969/j.issn.1672-2922.2018.03.010. [Google Scholar]
- 23.Teggi R, Colombo B, Albera R, Asprella Libonati G, Balzanelli C, Batuecas Caletrio A, et al. Clinical features, familial history, and migraine precursors in patients with definite vestibular migraine: the VM-phenotypes projects. Headache 2018;58:534–544. doi: 10.1111/head.13240. [DOI] [PubMed] [Google Scholar]
- 24.Frejo L, Giegling I, Teggi R, Lopez-Escamez JA, Rujescu D. Genetics of vestibular disorders: pathophysiological insights. J Neurol 2016;263:45–53. doi: 10.1007/s00415-015-7988-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiu F, Song DD, Guo QF, Wang QQ, Wang ZW, Liu JG, et al. Analysis of clinical features for vestibular migraine with imaging abnormalities on brain MRI [in Chinese]. Chin J Med 2017;97:1049–1053. doi: 10.3760/cma.j.issn.0376-2491.2017.14.004. [DOI] [PubMed] [Google Scholar]
- 26.Zhang YX, Kong QT, He ZL, Dong LZ, Tan G. Clinical features of vestibular migraine in a neurological clinic [in Chinese]. J Chongq Med Univ 2015;50:708–710. doi: 10.13406/j.cnki.cyxb.000616. [Google Scholar]
- 27.Qiu F, Qi XK. An etiological analysis of 367 neurological outpatients with complaint of vertigo [in Chinese]. Chin J Med 2012;51:350–352. doi: 10.3760/cma.j.issn.0578-1426.2012.05.006. [PubMed] [Google Scholar]
- 28.Furman JM, Marcus DA, Balaban CD. Vestibular migraine: clinical aspects and pathophysiology. Lancet Neurol 2013;12:706–715. doi: 10.1016/S1474-4422 (13)70107-8. [DOI] [PubMed] [Google Scholar]
- 29.von Brevern M, Lempert T. Vestibular migraine. Handb Clin Neurol 2016;137:301–316. doi: 10.1016/B978-0-444-63437-5.00022-4. [DOI] [PubMed] [Google Scholar]
- 30.Ashish G, Augustine AM, Tyagi AK, Lepcha A, Balraj A. Subjective visual vertical and horizontal in vestibular migraine. J Int Adv Otol 2017;13:254–258. doi: 10.5152/iao.2017.4056. [DOI] [PubMed] [Google Scholar]
- 31.Bisdorff A. Migraine and dizziness. Curr Opin Neurol 2014;27:105–110. doi: 10.1097/WCO.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 32.von Brevern M, Zeise D, Neuhauser H, Clarke AH, Lempert T. Acute migrainous vertigo: clinical and oculographic findings. Brain 2005;128:365–374. doi: 10.1093/brain/awh351. [DOI] [PubMed] [Google Scholar]
- 33.Zhao XQ. More clinical thoughts for diagnosis and treatment of vertigo/dizziness [in Chinese]. Chin J Med 2016;55:745 doi: 10.3760/cma.j.issn.0578-1426.2016.10.001. [Google Scholar]
- 34.Polensek SH, Tusa RJ. Nystagmus during attacks of vestibular migraine: an aid in diagnosis. Audiol Neurotol 2010;15:241–246. doi: 10.1159/000255440. [DOI] [PubMed] [Google Scholar]
- 35.Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain 1984;107:1123–1142. doi: 10.1007/978-3-642-71642-3_15. [DOI] [PubMed] [Google Scholar]
- 36.Battista RA. Audiometric findings of patients with migraine-associated dizziness. Otol neurotol 2004;25:987–992. doi: 10.1097/00129492-200411000-00021. [DOI] [PubMed] [Google Scholar]
- 37.Radtke A, von Brevern M, Neuhauser H, Hottenrott T, Lempert T. Vestibular migraine: long-term follow-up of clinical symptoms and vestibulo-cochlear findings. Neurology 2012;79:1607–1614. doi: 10.1212/WNL.0b013e31826e264f. [DOI] [PubMed] [Google Scholar]
- 38.Jiang ZD. Focus on vestibular migraine [in Chinese]. Chin J Med 2016;96:321–323. doi: 10.3760/cma.j.issn.0376-2491.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 39.Huppert D, Brandt T. Descriptions of vestibular migraine and Menière's disease in Greek and Chinese antiquity. Cephalalgia 2016;37:385–390. doi: 10.1177/0333102416646755. [DOI] [PubMed] [Google Scholar]
- 40.Mahringer A, Rambold HA. Caloric test and video-head-impulse: a study of vertigo/dizziness patients in a community hospital. Eur Arch Otorhi 2014;271:463–472. doi: 10.1007/s00405-013-2376-5. [DOI] [PubMed] [Google Scholar]
- 41.Vesligaj T, Maslovara S. Can a finding of cervical vestibular evoked myogenic potentials contribute to vestibular migraine diagnostics? Med Glas 2016;13:36–43. doi: 10.17392/834-16. [DOI] [PubMed] [Google Scholar]
- 42.Murofushi T. Clinical application of vestibular evoked myogenic potential (VEMP). Auris Nasus Larynx 2016;43:367–376. doi: 10.1016/j.anl.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 43.Yu HX, Li YJ, Wu XL, Wang SZ. Clinical features for 90 patients with vestibular migraine with imaging abnormalities on brain MRI [in Chinese]. Acad J Sec Med Univ 2018;39:695–697. doi: 10.16781/j.0258-879x.2018.06.0695. [Google Scholar]
- 44.Qi XK, Wang XF. Understanding concept, classification and diagnostic flow of dizziness [in Chinese]. Transl Med J 2016;5:1–4. doi: 10.3969/j.issn.2095-3097.2016.01.001. [Google Scholar]
- 45.von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res 2015;25:105–107. doi: 10.3233/VES-150553. [DOI] [PubMed] [Google Scholar]
- 46.Lopez-Escamez JA, Carey J, Chung WH, Goebel JA, Magnusson M, Mandalà M, et al. Diagnostic criteria for Meniere's disease. J Vestib Res 2015;25:1–7. doi: 10.3233/VES-150549. [DOI] [PubMed] [Google Scholar]
- 47.Dieterich M, Obermann M, Celebisoy N. Vestibular migraine: the most frequent entity of episodic vertigo. J Neurol 2016;263:82–89. doi: 10.1007/s00415-015-7905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Markus HS, van der Worp HB, Rothwell PM. Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. Lancet Neurol 2013;12:989–998. doi: 10.1016/S1474-4422 (13)70211-4. [DOI] [PubMed] [Google Scholar]
- 49.Zhao XQ. Identifying cerebral vascular disorders with dizziness/vertigo [in Chinese]. Beij Med J 2017;39:758–759. 10.15932/j.0253-9713.2017.08.002. [Google Scholar]
- 50.Whitney SL, Alghwiri A, Alghadir A. Physical therapy for persons with vestibular disorders. Curr Opin Neurol 2015;28:61–68. doi: 10.1097/WCO.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 51.Cha Y. Migraine-associated vertigo: diagnosis and treatment. Semin Neurol 2010;30:167–174. doi: 10.1055/s-0030-1249225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salviz M, Yuce T, Acar H, Taylan I, Yuceant GA, Karatas A, et al. Diagnostic value of vestibular-evoked myogenic potentials in Ménière's disease and vestibular migraine. J Vestib Res 2016;25:261–266. doi: 10.3233/VES-160567. [DOI] [PubMed] [Google Scholar]
- 53.O’Connell Ferster AP, Priesol AJ, Isildak H. The clinical manifestations of vestibular migraine: a review. Auris Nasus Larynx 2017;44:249–252. doi: 10.1016/j.anl.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 54.Chen J, Liu SX, Hu GH, Zhang XY, Xia Y. Gastrodin injection in the treatment of vertigo: a multi-center single-blind randomized controlled trial [in Chinese]. Chin J Evid Based Med 2004;4:864–870. doi: 10.3969/j.issn.1672-2531.2004.12.009. [Google Scholar]
- 55.Felisati G, Pignataro O, Di Girolamo A, Bruno E, Alessandrini M, Guidetti G, et al. Nicergoline in the treatment of dizziness in elderly patients. A review. Arch Gerontol Geriatr Suppl 2004;9:163–170. doi: 10.1016/j.archger.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 56.Kutay Ö, Akdal G, Keskinoğlu P, Balci BD, Alkin T, et al. Vestibular migraine patients are more anxious than migraine patients without vestibular symptoms. J Neurol 2017;264:37–41. doi: 10.1007/s00415-017-8439-6. [DOI] [PubMed] [Google Scholar]
- 57.Wang Q, Yu M, Zhang XL, Zhu Y, Qing DQ, Cai ZR, et al. Clinical observation of Tianshu capsule for treatment of migraine vertigo [in Chinese]. Guid J Trad Chin Med 2016;22:69–70. doi: 10.13862/j.cnki.cn43-1446/r.2016.03.024. [Google Scholar]
- 58.Liu YJ, Xiao W, Liu FY, Guo JK, Fang ZL, Wang J. Clinical research of prophylactic treatment of mirgraine on Tianshu capsule [in Chinese]. Chin J Exp Pharmacol 2013;19:311–315. doi: 10.11653/syfj2013100311. [Google Scholar]
- 59.Zhu WL, Yu M, Han W, He Y, Yang Y. Meta-analysis of Tianshu capsule in treatment of migraine [in Chinese]. J Clin Neurol 2016;29:282–285. [Google Scholar]


