Abstract
Introduction:
Implantation of an osseointegrated percutaneous prosthesis provides a reconstruction alternative for thumb amputation without sacrificing donor tissues.
Methods:
Thirteen thumb amputees received osseointegrated prostheses (1990 to 2014). The treatments were started with custom-designed implants. Since 2005, standardized implant components and structured rehabilitation protocols were introduced. The median follow-up period was 9.5 years.
Results:
Six patients were lost to follow-up. Seven patients (including all six after the introduction of the standardized protocol) had good osseoperception, grip strength (Jamar) was 28.3 kg on the operated side versus 40.4 kg in the unaffected hand (70%), and key grip strength was 6 versus 9.1 kg. Hand function was 94% of the normal hand. The most common complications were mechanical failures necessitating changes of components (eight times in three patients) and superficial infections (seven times in five patients). Five patients had no complications. The refined implant design and new standardized treatment protocol achieved a 100% cumulative success rate with 9.5 years of follow-up so far.
Discussion:
Treatment of thumb amputees using bone-anchored percutaneous prostheses seems to be a safe, durable method with excellent short- and medium-long follow-up results. Severe adverse events are few except for implant loosening which occurred only in the early custom-designed group.
Thumb amputation results in devastating disability with the loss of pinch and grasp, evaluated as 40% impairment of hand function.1 Multiple reconstructive procedures to restore thumb function have been described, such as toe-to-thumb transplantation, pollicization, and osteoplastic lengthening.2 Each of the methods described earlier offers subtle benefits and downsides and maybe more applicable in certain conditions. For amputations through the metacarpophalangeal joint or distal metacarpal levels, toe transfer has long been regarded as the standard of care.3 The procedure requires microsurgical expertise combined with prolonged wound monitoring and rehabilitation process. Despite success rates of more than 95% are reported, secondary procedures such as tenolysis, bone or nerve graft, web deepening, and opponensplasty are often required.4 The extent of donor site morbidity remains controversial. Although patients could ambulate, climb stairs, and participate in certain sports,5 delayed wound healing, high callus formation rate, and decreased push-off in gait after toe transfer are known.4 From a cosmetic point of view, many patients consider that transferred toes are unappealing: the second toe had a tendency to claw and the great toe can give a cobra head appearance.6,7 Therefore, alternative methods for thumb reconstruction are needed.
Bone-anchored prostheses based on the osseointegration principle have been widely used over a half century in different parts of human body, including oral, cranial facial, and extremity reconstructions.8 The concept of osseointegration can be defined as a direct anchorage of an implant into skeleton by induction of bone healing to the implant surface.9-11 The intimate bone-implant contact without the presence of fibrous tissue can prevent penetration of bacteria from skin opening or oral environment, providing stability for long-term usage. Another advantage with osseointegrated prostheses is the ability to sense vibrations and pressure, defined as osseoperception.12 Neurophysiologic and psychophysical evidence of osseoperception have been collected, making the assumption more likely that a proper peripheral feedback pathway can be restored with development of osseointegrated implants.13 The facts mentioned earlier indicate that application of osseointegration might provide an attractive reconstruction alternative for thumb amputation without sacrificing donor tissues.
The first report on osseointegrated thumb reconstruction was published in 1996 on three posttraumatic amputees.14 All patients underwent two-stage reconstructive procedures and were followed up between 18 months and 3 years. The results were promising, ie, no implant loosening or skin complications occurred and some extent of tactile discrimination was achieved. However, the samples are small, and the short-term follow-up is not sufficient for evaluating an implant-based treatment strategy. In the present article, we summarize the long-term follow-up of 13 thumb amputees treated in our center with osseointegrated prostheses between 1990 and 2014. We present data on cumulative success rate, radiologic analysis, functional outcomes, and adverse events. To our knowledge, this is the most complete case series available for evaluating this novel thumb reconstruction method.
Patients and Methods
Patient Demography
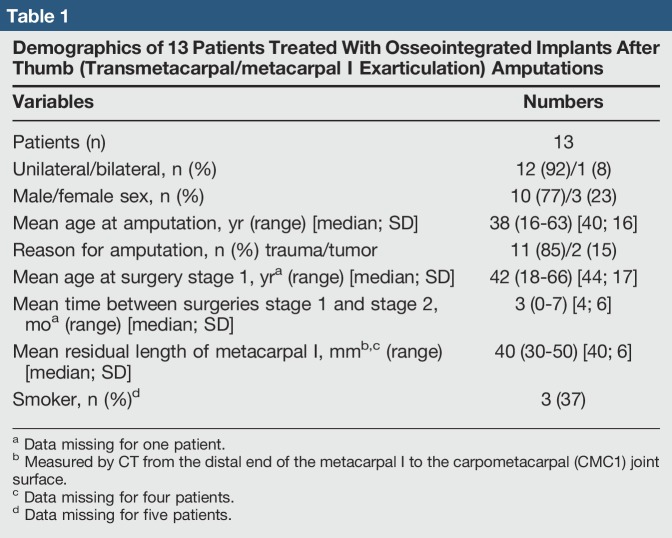
This is a retrospective single center study from 1990 to October 2017. Preoperative and postoperative data were collected from 13 thumb amputees. Ethical approval was obtained from the Medical Ethical Committee of the Local Region (no. 952-13). Removal of the implant was considered as the end point for failure. The inclusion criterion was thumb amputation at distal metacarpal or through the metacarpophalangeal joint. One patient with amputation at the proximal phalange level was included. The patients should be suitable for surgery based on physical examination and medical history and likely to comply with rehabilitation and follow-up requirements. All patients understood that other reconstructive methods are available and osseointegration procedure is so far not the standard treatment. One patient was a bilateral amputee, the left hand treated with toe-to-thumb transfer and the right hand with an osseointegrated prosthesis (Table 1).
Table 1.
Demographics of 13 Patients Treated With Osseointegrated Implants After Thumb (Transmetacarpal/metacarpal I Exarticulation) Amputations
Surgical Methods
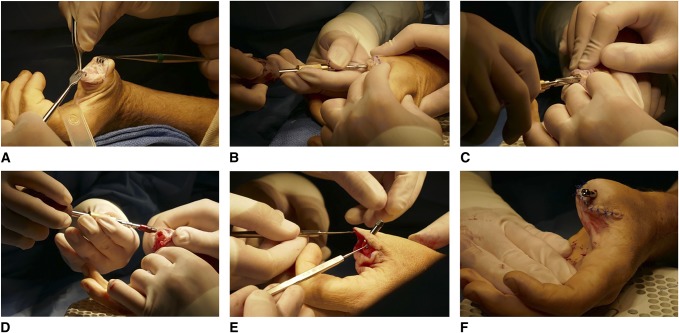
The osseointegration procedure consists of two surgeries. In the first stage (S1), a threaded titanium implant (the fixture) is inserted into the intramedullary canal of metacarpal I after gentle reaming and tapping (Figure 2). The bone marrow blood is always collected and seeded onto the fixture surface before implant insertion to assure plenty amount of osteoprogenitors in the bone-implant interface. Intimate contact of the fixture threads to the inner cortex is necessary. According to our experience, good primary stability usually indicates good future osseointegration. In the earlier cases, cancellous bone graft from the iliac crest was often added to assure a satisfied distal bone closure. At the second stage (S2), the muscle/tendon endings are sutured to the periosteum at least 0.5 cm proximal to the end of metacarpal stump. The subcutaneous fat is removed at least 1 cm from the skin opening to guarantee a thin, hair follicular-free, and immobile skin around the abutment. The direct healing of skin to bone edge without any mobile soft-tissue interface is crucial to avoid soft-tissue complications under usage. The abutment is then inserted through the skin opening to the press-fitting part of the fixture with compression applied by an abutment screw. The mean healing period between S1 and S2 surgeries was 3 months (0 to 7 months), including three recent cases in which a single-stage surgical protocol was used. In one tumor patient, a single-stage approach was used at the time of amputation. During the period 1990 to 2004, patients were treated with the custom-designed implant modified from the dental implant system. From 2005 and onward, a thumb-specific implant system was used with a standardized surgical protocol.
Figure 2.
The osseointegration procedure: The distal end of metacarpal I is exposed and opened (A). After reaming (B) and tapping (C), a threaded titanium implant is inserted into the intramedullary canal (D). The abutment is then inserted through the skin opening to the press-fitting part of the fixture with compression applied by an abutment screw (E, F).
Figure 1.
A, Schematic illustration of the implant system. B, Photograph of a patient with an osseointegrated percutaneous thumb prosthesis (the silicon sleeve has been folded to make it easier to see the implant). C, Radiograph of an osseointegrated percutaneous thumb prosthesis.
Rehabilitation and Follow-up
Approximately 4 weeks after the S2 surgery, patients were supplied with their first prosthesis and could start gentle motion. Two weeks later, the patients started full range of motion (ROM) and strengthening exercises. They were allowed to do light daily activities and gradually increased the load.15 The follow-up protocol (conducted at 3 and 6 months and at 1, 2, 3, 5, 7, 10, 15, 20, and 25 years after the S2 surgery) included a radiographic examination and a clinical examination by a specialized team composed of an orthopaedic surgeon, an occupational therapist, and a prosthetist. During the follow-up period, all adverse events, radiologic outcomes, and functional outcome measures were registered in the medical records.
Measurements for Functional Outcomes
Two questionnaires were used for patient-reported outcomes: the first relates to the symptoms and ability to perform activities, the Disability of the Arm, Shoulder, and Hand, and the second, European Quality of Life-3 Dimensions (EQ5D-3L), is a nonspecific health-related quality of life questionnaire.
The following hand function tests were used: B&L pinch gauge and Jamar dynamometers, monofilament test, and Sollerman hand function test. In these tests, the unaffected hand was compared with the affected hand. A higher score correlates with better strength of the hand.
Hand strength was measured with a hydraulic hand dynamometer (Jamar) for grip strength and B&L Engineering Mechanical Pinch Gauge for key and pinch grip.16 The Sollerman standardized hand function test (SHFT) was used to test dexterity and hand function. It consists of 20 tasks based on activities of daily living, and eight different handgrips were used. The types of grip described in the test are pulp pinch, lateral pinch, tripod pinch, five-finger pinch, diagonal volar grip, five-finger grip, spherical volar grip, and extension grip. Each subtest is scored from 0 to 4 based on the time and ability to use the right grip. The maximum score for normal hand function is 80 points.17,18 Sensibility in the thumb was measured using a standardized kit with five monofilaments (Semmes Weinstein monofilaments). The monofilament consists of a plastic rod with a nylon thread, which exerts a pressure measured in grams when applied to the skin.19,20 The affected thumb was compared with the unaffected thumb. Monofilament 2.83 g indicates normal sensation, scores over shows diminished light touch (3.61), diminished protective sensation (4.31), loss of protective sensation (4.56), and deep pressure sensation only (6.65). ROM was measured with a standardized goniometer according to HAKIR, a Swedish National Quality Register for Hand Surgery (http://hakir.se/).
Results
A total of 13 patients were followed up for a mean of 9.5 years (0.25 to 25). Two patients were withdrawn from the study for unrelated reason (death from unrelated cause, after 20 and 15 years of follow-up, respectively). There were four nonusers: Two patients had their implants removed at 6 months after S2 because of failed osseointegration and implant loosening. The patient with amputation at the proximal phalange developed deep infection between S1 and S2 surgeries, which led to extraction of implants. None of the patients with implant failure (n = 3) had a new implant installed. One patient decided not to use any prostheses 1 year after S2. The patient, however, did not want the implant to be removed. His implant is clinically and radiologically well osseointegrated. The first patient treated with an osseointegrated thumb prosthesis in 1990 had a fall in 2006 leading to a tetraplegic condition and has very limited remaining hand function. This patient could not be measured by functional tests, but he continued to wear the prosthesis daily for functional and cosmetic reasons.
For the well-osseointegrated implants, none of the patients had load-related pain. Five patients had been documented with a total of seven superficial infections/inflammations around the skin openings. The infections were treated by oral antibiotics and/or local ointments with antibiotics (Terra-Cortril with polymyxin B; Pfizer, Sweden). The symptoms were all resolved within 2 weeks. None of the local complications progressed to deep infection.
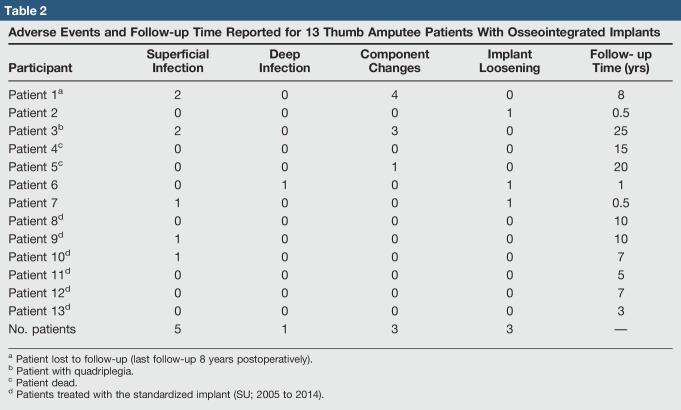
A total of eight mechanical complications were documented in the three patients who were treated with the custom-designed experimental implant before 2004. The complications included abutments or abutment screw bending or fractures, which were treated with component changes. No fractures of the fixtures were seen. Notably, no mechanical complications were documented for patients who received the standardized thumb implants (Table 2).
Table 2.
Adverse Events and Follow-up Time Reported for 13 Thumb Amputee Patients With Osseointegrated Implants
The success rates for the custom-designed implants is 57% while for the standardized implants is 100%. For both implant systems, no late implant failures were seen after the first year, with the longest follow-up of 25 years.
Radiologic Assessment
The radiological evaluation of osseointegration regarding the phenomenon of distal and near-implant bone resorption, buttressing and loosening has previously been described.21,22 The patient's latest performed radiograms on AP and lateral views were evaluated; signs of loosening, as well as distal and near-implant bone resorption, were noted. Nine of the 13 patients had assessable radiograms. Only one patient (patient 3) had noticeable bone resorption (Table 3). This patient had near-implant bone resorption on the radial and palmar side (six threads). A minimal insignificant distal bone resorption (0.7 mm) was observed in one patient, but it did not expose the threads of the fixture. Buttressing (ie, formation of cortical bone around the proximal end of the fixture) was not a prominent feature in any of the patients.
Table 3.
Radiologic Evaluation of Osseointegration Around the Implant in 13 Patients
Outcome Measures
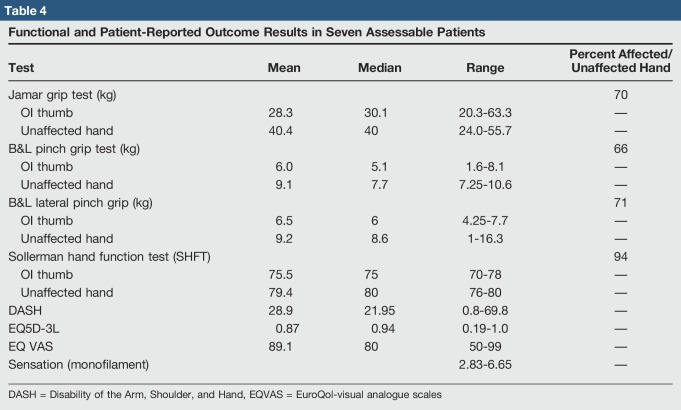
For the seven patients who could be measured with functional tests, the average usage time (1991 to October 2017) was 9.5 years (range, 0.25 to 25 years; median, 8 years), and all seven patients used their prostheses 7 d/wk, 8 to 24 hr/d. The functional outcome of these patients was evaluated.
Hand strength test outcomes: in the Jamar grip test, patients had 70% of grip strength compared with the unaffected hand. Two patients had better strength with the affected hand compared with the unaffected hand. One patient had only 38% of grip strength compared with his unaffected hand, but his digits I to IV are partially amputated.
Measured pinch strength was 66% and lateral pinch 71% compared with the unaffected hand. Two patients showed better strength in the affected hand compared with the unaffected hand when measuring the pinch grip. With the lateral grip, one patient had better grip with the affected hand.
The mean value of all scores from the SHFT was 75.5 points of a maximum of 80 points. Hence, the results show that the patients have 94% of a normal hand function. All patients had some difficulties picking up coins, handling bolts/knots, and doing buttons up. One patient with four digits partially amputated had additional complications using a knife/fork, unscrewing large lids, folding letters, and pouring milk from a package.
All patients were able to feel tactile sensation in their osseointegrated prosthesis. One patient could detect normal sensation, one diminished protective sensation, two had loss of protective sensation, and three could feel deep pressure. Table 4 presents all functional and patient-rated outcome measures.
Table 4.
Functional and Patient-Reported Outcome Results in Seven Assessable Patients
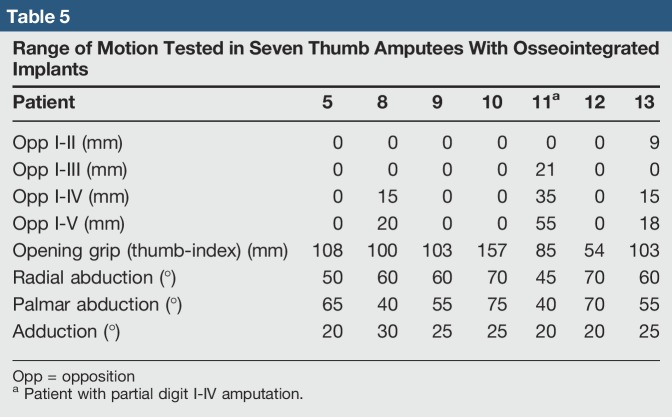
ROM outcomes: the opposition of the thumb to the index finger was normal in 6 cases (Table 5).
Table 5.
Range of Motion Tested in Seven Thumb Amputees With Osseointegrated Implants
Discussion
Although replantation is typically indicated after thumb amputation, the rate of primary replantation for instance in the United States remains low and many patients need secondary reconstruction procedures to restore their hand functions.23 To our knowledge, the present article provides the most comprehensive data for thumb reconstruction treated with osseointegrated percutaneous prostheses.
Our data show that active users of the osseointegrated prostheses can achieve hand function with 66% grip strength and 71% lateral pinch strength compared with the unaffected side. The results are comparable to the great toe-to-thumb transfers, as described previously, with grip strength 77% and pinch strength 67% of the uninjured side.24 Strikingly, all osseointegrated prosthetic users were able to feel tactile sensation from their prosthesis. With the monofilament test, one patient could detect normal sensation, one diminished protective sensation, two had loss of protective sensation, and three could feel deep pressure. The regained sensibility by an osseointegrated prosthesis for thumb amputees provides further evidence on osseoperception, a phenomenon known for decades and is thought to correlate with the functional achievement for patients receiving dental or extremity osseointegrated prostheses.12,13 The underlying mechanism(s) of osseoperception remains a matter of debate.25 Vibrations are known to be received and transmitted by Pacinian corpuscles, which are particularly dense in the fingertips, hand, and foot soles.26,27 They were also identified to be spread on the periosteum covering the bones, supporting the idea of bony sensitivity to vibration as proposed by Egger more than a century ago.28 Of interest, the latest research conducted by Ortiz-Catalan et al indicates that a multisensory perception mechanism might be involved in osseoperception including touch and hearing.29 We suppose that the sensibility of an osseointegrated thumb prosthesis makes up the closed-loop tactile feedback system, which explained the high scores for patients performing the SHFT. The sensibility also presents a major advantage of osseointegrated prostheses over ordinary hand prostheses, by which the users are forced to rely primarily on visual feedback to ensure their prosthetic hand behaving appropriately. Relying primarily on visual feedback with no tactile input can be rather burdensome when it comes to picking up, holding, or manipulating objects.30
Since the introduction in 1966, the vascularized toe transfers were quickly introduced in reconstructive hand surgery for patients with devastating trauma or congenital digit absence.31 However, the markedly improved hand function tends to overshadow the resulted impairment in foot function because of digit donation. According to a recent review of Sosin et al,32 the overall rate of developing a wound healing complication in the donor site after toe-to-hand transfer was 20.2% (162 of 802 digit transfers), with donor site reoperative intervention occurring in 11.8% of cases (95 digits). For great toe transfers, changes or alterations of the normal gait cycle were reported in many studies.33,34 Specifically, the push-off phase of gait was altered, as was the load distribution during gait, center of gravity during standing, and peak pressure on the foot.6,28 Evaluation by piezoelectric analysis indicated that the impact load was transitioned to the remaining metatarsal heads and digits, with the potential for increased aberrant loading, callus formation, and eventual plantar pad erosion.32 With the osseointegrated thumb reconstruction procedure, no donor organ is sacrificed. Therefore, the patients and the reconstruction team no longer have the concern of donor site morbidity.
Unlike toe transfers, which require advanced microsurgical techniques and sophisticated postoperative wound monitoring, the osseointegrated thumb reconstruction is a relative simple procedure that could be performed by surgeons with proper training. The surgery is approximately 60 minutes for a combined S1 + S2 procedure, and the patients are usually discharged 1 day after S1 or S2 surgery, or could be done as an outpatient procedure. However, the osseointegrated reconstructed thumb requires certain maintenance, such as changing of silicon outer prosthetic sheath due to abrasion or changing of the abutments/abutment screws due to fatigue fractures. In this study, three patients received abutment and/or abutment screw changes because of fatigue fractures of the components (all of them were treated with the early custom-designed experimental implant components). So far, there have not been any reports of mechanical complaints with the standardized implant used since 2005. This result indicates that the mechanical strength has been sufficiently improved during the standardization of the implant system. The authors recommend that a multidisciplinary osseointegration team with effective collaboration with orthopaedic, hand/plastic surgeons, occupational therapists, prosthetics, and nurses is needed to guarantee optimal functional outcomes of this type of prosthesis users.
Like all other percutaneous implant systems, infections are of concern also for osseointegrated thumb reconstructions. In the present study, we report on one case with a deep infection between S1 and S2 surgeries, which led to loosening of the implant 1 year after the second-stage surgery. This was one of the early patients treated with a custom-made design. Monitoring for early signs of infections before the second-stage surgery is thus of importance to make the patients aware of prophylactic caution and avoiding loosening. According to this study, five patients had been documented with a total of seven superficial infections/inflammations around the skin openings. With antibiotic treatment, the symptoms were all resolved within 2 weeks. None of the patients developed deep infections with implant loosening. Notably, the bilateral thumb amputee patient in our series was not satisfied with the toe-to-thumb transfer on his left amputated thumb and decided to reconstruct his right thumb with an osseointegrated thumb prosthesis instead. At his last visit at the clinic (25 years of follow-up), despite a superficial infection, the patient was satisfied with his choice of an osseointegrated thumb reconstruction.
In studies on osseointegrated prostheses for transhumeral amputees, there is an 85% cumulative success rate at 2 years.21 In transfemoral amputees, the corresponding figure is 92%.9 The cumulative success rate in this study regarding patients with early custom-designed implants was 77% (at 1-year follow-up), but after introducing standardized implant components and a strict rehabilitation program in 2005, there is now a 100% cumulative success rate for those six patients who have been followed for up to 10 years (mean, 7 years). Compared with all other osseointegrated prostheses in an orthopaedic setting, the thumb amputees seem to have the possibility to have the highest cumulative success rate.
There are several limitations to the present study. First of all, the number of patients (13) is low, but it includes all treated patients since the treatment was introduced in 1990. Data are missing or unattainable for some patients regarding adverse events (1 of 13), outcome measures (6 of 13), and radiographic assessments (4 of 13). This phenomenon is partly due to limited, old, and archived medical records. More importantly, all records from the later treatment period are intact. Another limitation is that not every patient with a thumb amputation is suitable for using an osseointegrated prosthesis. Immature skeleton and recent radiation therapy and/or chemotherapy treatment are relative contraindications to using the technique.
In conclusion, treatment of thumb amputees using bone-anchored percutaneous prostheses with the osseointegration technique seems to be a safe, durable method with excellent short- and medium-long follow-up results. Using the latest design (after 2005), there is a 100% cumulative success rate, up to 10 years of follow-up. Although the patient population is limited, the osseointegrated reconstruction of thumbs is shown to offer a valuable psychological, functional, and rehabilitative potential in daily life activities for patients.
Footnotes
Supported by the ALF foundation Västra Götaland Region (ALFGBG-449381), the Swedish Research Council (VR 521-2014-2664), and the CIMED collaboration foundation (H93041113).
Dr. Li or an immediate family member serves as an unpaid consultant to Integrum AB. Ms. Kulbacka-Ortiz or an immediate family member is an employee of Integrum AB and has stock or stock options held in Integrum AB. Dr. Brånemark or an immediate family member is an employee of Integrum AB and Integrum; serves as a paid consultant to Integrum AB; has stock or stock options held in Integrum; and serves as a board member, owner, officer, or committee member of the Orthopaedic Surgical Osseointegration Society. Neither Ms. Caine-Winterberger nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article.
References
- 1.Rondinelli RD: AMA Guides to the Evaluation of Permanent Impairment. American Medical Association, 2008. [Google Scholar]
- 2.Graham DJ, Venkatramani H, Sabapathy SR: Current reconstruction options for traumatic thumb loss. J Hand Surg Am 2016;41:1159-1169. [DOI] [PubMed] [Google Scholar]
- 3.Pet MA, Ko JH, Vedder NB: Reconstruction of the traumatized thumb. Plast Reconstr Surg 2014;134:1235-1245. [DOI] [PubMed] [Google Scholar]
- 4.Lin PY, Sebastin SJ, Ono S, Bellfi LT, Chang KW, Chung KC: A systematic review of outcomes of toe-to-thumb transfers for isolated traumatic thumb amputation. Hand (N Y) 2011;6:235-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipton HA, May JW, Jr, Simon SR: Preoperative and postoperative gait analyses of patients undergoing great toe-to-thumb transfer. J Hand Surg Am 1987;12:66-69. [DOI] [PubMed] [Google Scholar]
- 6.Sabapathy SR, Venkatramani H, Bharathi RR: Functional evaluation of a great toe transfer and the osteoplastic technique for thumb reconstruction in the same individual. J Hand Surg Br 2003;28:405-408. [DOI] [PubMed] [Google Scholar]
- 7.Kumta SM: Unfavourable results in thumb reconstruction. Indian J Plast Surg 2013;46:294-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Branemark PI, Adell R, Breine U, Hansson BO, Lindstrom J, Ohlsson A: Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg 1969;3:81-100. [DOI] [PubMed] [Google Scholar]
- 9.Branemark R, Berlin O, Hagberg K, Bergh P, Gunterberg B, Rydevik B: A novel osseointegrated percutaneous prosthetic system for the treatment of patients with transfemoral amputation: A prospective study of 51 patients. Bone Joint J 2014;96-B:106-113. [DOI] [PubMed] [Google Scholar]
- 10.Eriksson E, Branemark PI: Osseointegration from the perspective of the plastic surgeon. Plast Reconstr Surg 1994;93:626-637. [PubMed] [Google Scholar]
- 11.Branemark PI: Osseointegration and its experimental background. J Prosthet Dent 1983;50:399-410. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs R, Branemark R, Olmarker K, Rydevik B, Van Steenberghe D, Branemark PI: Evaluation of the psychophysical detection threshold level for vibrotactile and pressure stimulation of prosthetic limbs using bone anchorage or soft tissue support. Prosthet Orthot Int 2000;24:133-142. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs R, Van Steenberghe D: From osseoperception to implant-mediated sensory-motor interactions and related clinical implications. J Oral Rehabil 2006;33:282-292. [DOI] [PubMed] [Google Scholar]
- 14.Lundborg G, Branemark PI, Rosen B: Osseointegrated thumb prostheses: A concept for fixation of digit prosthetic devices. J Hand Surg Am 1996;21:216-221. [DOI] [PubMed] [Google Scholar]
- 15.Jonsson S, Caine-Winterberger K, Branemark R: Osseointegration amputation prostheses on the upper limbs: Methods, prosthetics and rehabilitation. Prosthet Orthot Int 2011;35:190-200. [DOI] [PubMed] [Google Scholar]
- 16.Mathiowetz V, Weber K, Volland G, Kashman N: Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am 1984;9:222-226. [DOI] [PubMed] [Google Scholar]
- 17.Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S: Grip and pinch strength: Normative data for adults. Arch Phys Med Rehabil 1985;66:69-74. [PubMed] [Google Scholar]
- 18.Sollerman C, Sperling L: Evaluation of adl-function—Especially hand function. Scand J Rehabil Med Suppl 1978;6:139-143. [PubMed] [Google Scholar]
- 19.Sollerman C, Ejeskar A: Sollerman hand function test. A standardised method and its use in tetraplegic patients. Scand J Plast Reconstr Surg Hand Surg 1995;29:167-76. [DOI] [PubMed] [Google Scholar]
- 20.Bell Krotoski J: Sensibility Testing: Hand and Upper Extremity Rehabilitation. ed 3 Elsevier Inc; Churchill Livingstone: 2005. [Google Scholar]
- 21.Tsikandylakis G, Berlin O, Branemark R: Implant survival, adverse events, and bone remodeling of osseointegrated percutaneous implants for transhumeral amputees. Clin Orthop Relat Res 2014;472:2947-2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nebergall A, Bragdon C, Antonellis A, Karrholm J, Branemark R, Malchau H: Stable fixation of an osseointegated implant system for above-the-knee amputees: Titel RSA and radiographic evaluation of migration and bone remodeling in 55 cases. Acta Orthop 2012;83:121-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Conn JM, Annest JL, Ryan GW, Budnitz DS: Non-work-related finger amputations in the United States, 2001-2002. Ann Emerg Med 2005;45:630-635. [DOI] [PubMed] [Google Scholar]
- 24.Buncke GM, Buncke HJ, Lee CK: Great toe-to-thumb microvascular transplantation after traumatic amputation. Hand Clin 2007;23:105-115. [DOI] [PubMed] [Google Scholar]
- 25.Lundborg G, Waites A, Bjorkman A, Rosen B, Larsson EM: Functional magnetic resonance imaging shows cortical activation on sensory stimulation of an osseointegrated prosthetic thumb. Scand J Plast Reconstr Surg Hand Surg 2006;40:234-239. [DOI] [PubMed] [Google Scholar]
- 26.Verrillo RT: Effect of spatial parameters on the vibrotactile threshold. J Exp Psychol 1966;71:570-575. [DOI] [PubMed] [Google Scholar]
- 27.Sato M: Response of Pacinian corpuscles to sinusoidal vibration. J Physiol 1961;159:391-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greening J, Lynn B: Vibration sense in the upper limb in patients with repetitive strain injury and a group of at-risk office workers. Int Arch Occup Environ Health 1998;71:29-34. [DOI] [PubMed] [Google Scholar]
- 29.Clemente F, Hakansson B, Cipriani C, et al. : Touch and hearing mediate osseoperception. Sci Rep 2017;7:45363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Osborn L, Kaliki R, Soares A, Thakor N: Neuromimetic event-based detection for closed-loop tactile feedback control of upper limb prostheses. IEEE Trans Haptics 2016;9:196-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buncke HJ, Jr, Buncke CM, Schulz WP: Immediate Nicoladoni procedure in the Rhesus monkey, or hallux-to-hand transplantation, utilising microminiature vascular anastomoses. Br J Plast Surg 1966;19:332-337. [DOI] [PubMed] [Google Scholar]
- 32.Sosin M, Lin CH, Steinberg J, et al. : Functional donor site morbidity after vascularized toe transfer procedures: A review of the literature and biomechanical consideration for surgical site selection. Ann Plast Surg 2016;76:735-742. [DOI] [PubMed] [Google Scholar]
- 33.Barca F, Santi A, Tartoni PL, Landi A: Gait analysis of the donor foot in microsurgical reconstruction of the thumb. Foot Ankle Int 1995;16:201-206. [DOI] [PubMed] [Google Scholar]
- 34.Tiamfook T, Sartoris DJ, Goldberg J: Radiographic alterations in the foot following toe-to-thumb free transfer. J Foot Ankle Surg 1994;33:283-289. [PubMed] [Google Scholar]