Abstract
Introduction
The globally increasing prevalence of chronic kidney disease has resulted in an ever-growing demand for renal replacement therapy. Although programs are present around the world, there is a paucity of immersive educational programs that train clinicians and administrators to develop new home dialysis programs. Explore Home Dialysis (EHD) is a program created to fill this gap.
Methods
We present the results of the evaluation of the EHD program. Our team interviewed 23 clinicians and administrators who participated in the EHD program. We also assessed country-specific needs and challenges associated with home dialysis.
Results
The 4 main findings include (i) the evaluation of the effectiveness of the EHD program; (ii) the need for an educational program to train individuals on how to deploy home dialysis programs; (iii) evidence that such an educational program is beneficial to participants and for the establishment of new home dialysis programs; and (iv) the identification of barriers to the development of home dialysis programs in countries represented in this study. The data show an increased demand, with strong patient and provider interest in establishing new programs, interest in accessing resources to train clinical and administrative staff in how to run a home dialysis program, and positive feedback about the EHD program in general.
Conclusions
The data from this study were used in the next iteration of the EHD program, to inform clinicians about challenges in the deployment of new home dialysis programs, and to present educational resources that need to be developed in the future.
Keywords: chronic kidney disease, clinicians, home dialysis, program evaluation
The global increase of patients with chronic kidney disease has resulted in an increasing demand for renal replacement therapy.1 The rate of end-stage kidney disease in the developed world has plateaued, but prevalence continues to grow with a significant growth in the emerging world.2 Despite research indicating the benefits of home dialysis with respect to cost savings and improved quality of life for patients in comparison with in-center dialysis, from a patient and caregiver perspective,3 the utilization of home dialysis therapies remains considerably low for patients with end-stage kidney disease compared with in-center hemodialysis.4 According to data from the US Renal Data System, the average number of patients using in-center dialysis, peritoneal dialysis, and home hemodialysis across 42 countries in 2014 was 84.5%, 13.7%, and 1.8%, respectively.4
The dissemination and success of home dialysis programs around the world are heavily constrained by existing cultural, institutional, political, and financial characteristics of the health care system and patients.5, 6, 7 Previous studies have explored barriers to the deployment of home dialysis therapies from the perspective of patients and caregivers,3, 5, 8, 9, 10, 11, 12 identifying several common themes around patient support, technology limitations, infrastructural needs, and patient fears. Similarly, other researchers have explored patient needs and overall experience with home dialysis technologies and treatments,13, 14 both for the delivery of home dialysis and the selection of patients for treatment.
Personal perceptions related to the use of home dialysis14, 15, 16 have shown extensive support from clinicians in Australia, but apprehension from clinicians in Europe and South America. The importance of clinician support and buy-in has been widely demonstrated in Australia and New Zealand,17 revealing that clinicians are likely the main enablers for the success of home dialysis programs. However, knowledge and expertise for creating home dialysis programs is scattered, with limited availability of materials and resources to support nephrologists and nurses in this process,18, 19 and lacking patient educational content.20, 21 Rope et al.18 identified that nephrologists in training felt least prepared in the area of home hemodialysis, including both home hemodialysis and peritoneal dialysis, making it a top preference for additional instruction during fellowships.
In this setting, there was a strong need to create a program to guide the development of new home dialysis programs around the world. The Explore Home Dialysis (EHD) program was created at the University Health Network (UHN) to fill this gap and provide the necessary support for nephrologists to create home dialysis programs locally. In the program, participants are immersed in 4 core domains: clinical encounters and/or observations, core curriculum teaching, simulation and practical applications of knowledge, and concept testing and research project presentation.
This report describes (i) the results of an evaluation program to assess the effectiveness of the EHD program; (ii) the need for an educational program to train individuals on how to deploy home dialysis programs; (iii) the evidence that such an educational program is beneficial to participants and for the deployment of new home dialysis programs around the world; and (4) a brief summary of barriers (political, technological, and administrative) to the deployment of home dialysis programs in different countries from the perspective of participants from the EHD program. Through a user-centered design approach,22, 23 data from current users have been used to create the next iteration of the EHD program. User-centered design approaches leverage qualitative and quantitative data collection methods to incorporate user needs into the future design of technologies and programs.
Methods
Recruitment and Demographics
A convenience sampling method was used, recruiting clinicians and administrators who participated in the EHD program at UHN between 2014 and 2016. A total of 23 participants agreed to participate in this study; a group consisting of clinical nephrologists, nephrology educators, fellows, nurses, administrators, and marketing leads, as those were who attended the EHD program. All study participants were recruited by the program’s clinical coordinator as part of an internal improvement initiative for the EHD program and forwarded to our data collection team at Healthcare Human Factors. A sample of countries represented in the EHD client population is provided in Table 1.
Table 1.
Global representation in our participant sample
| Country | Roles |
Number of participants | Percentage (n = 23) | |||
|---|---|---|---|---|---|---|
| Nephrologist | Nurse | Nephrology fellow | Administrator | |||
| Australia | 1 | 1 | 4.3 | |||
| Brazil | 3 | 3 | 13.0 | |||
| Canada | 1 | 1 | 4.3 | |||
| Colombia | 1 | 1 | 4.3 | |||
| Germany | 1 | 1 | 4.3 | |||
| Hong Kong | 4 | 5 | 9 | 39.1 | ||
| Hungary | 1 | 1 | 4.3 | |||
| Iran | 2 | 2 | 8.7 | |||
| Jordan | 1 | 1 | 4.3 | |||
| Singapore | 1 | 1 | 2 | 8.7 | ||
| Thailand | 1 | 1 | 4.3 | |||
| Total | 11 | 7 | 4 | 1 | 23 | 100 |
Data Collection
A mixed-methods approach,24, 25 combining quantitative metrics (surveys) with qualitative data collection (semi-structured interviews and open-ended survey questions), was used to develop a comprehensive picture of the needs and barriers when creating new home dialysis programs around the world and to support the deployment of new home dialysis programs. This combination of methods was selected to combine the strength of quantitative feedback with the richness of qualitative data. The 1-hour-long interviews were conducted by the authors; participants were interviewed at Healthcare Human Factors at a private interviewing room where only the participants and researchers were present, and direct representatives from EHD were not present during the interview to avoid biasing the results. The researchers responsible for the data collection and analysis were a Research Lead and Research Assistant at Healthcare Human Factors located at the Centre for Global eHealth Innovation, with extensive experience in qualitative methods, human factors engineering, user experience, and data collection. Field notes were the main data collection mechanism, and video and audio recording were not used in this study. Before the interview, the researchers described their affiliation with Healthcare Human Factors, that they were at arm’s length from EHD, and that our goal was to understand the global landscape and evaluate the EHD program.
EHD program observers and fellows were asked to complete a questionnaire before their arrival at UHN to start the program, a postdeparture questionnaire once they completed their observership/fellowship, and 1 interview during their tenure in the program. The pre-arrival questionnaire focused on (i) observers’ motivations for joining the program, (ii) their learning expectations, and (iii) an opportunity for our team to investigate global trends and resources available with in-home dialysis around the world. The postdeparture questionnaire collected quantitative feedback on various aspects of the EHD experience and opportunities for improvement. In particular, participants were asked to rate their satisfaction in the following areas of the EHD program: clinical encounters/observations of patients, curriculum of the program, simulation facilities and resources, practical application of their knowledge, workshops and lectures, orientation by the clinical team, administrative support, and overall experience in the program. Regarding feedback on how to improve the EHD program, the questionnaire encouraged suggestions for workshops and potential additional resources that could benefit EHD observers while at UHN or after returning to their home institutions. EHD clients were interviewed while they were at UHN during their observerships, providing additional insights about the challenges and barriers faced in their home countries when deploying a home dialysis program. The semi-structured interview questions were chosen in advance to further explore participants’ answers to the pre-arrival questionnaire, allowing them to elaborate on their answers and provide additional details and clarifications when necessary.24, 25
Data analysis was performed using grounded theory,26 with data evaluated and coded by the authors. Themes were extracted from the data following grounded theory principles,26 and defined after the codes were evaluated.
Results
The main participants of the EHD program are clinicians (nephrologists, nurses, and fellows) who work in nephrology, renal care, and in-clinic dialysis facilities (Table 1). Our sample included representatives from South America, Europe, Asia, and Oceania. The sample represented in Table 1 corresponds to clinicians and administrators who have registered for EHD, have been accepted, and self-funded their attendance to the EHD program. Data saturation was achieved for most of the areas being explored.
Demand for Home Dialysis Programs
Clinicians described a strong need for new home dialysis programs in their home countries to manage the increasing numbers of hospital-based dialysis patients. Another aspect highlighted by clinicians was the specific need for home hemodialysis programs for patients who are not suitable for peritoneal dialysis (in countries where only peritoneal dialysis was available). The overall perception is that (i) home dialysis programs will promote a better quality of life for patients by allowing less disturbance to the patient’s work and social life, and (ii) reduce clinicians’ workload related to delivering in-clinic dialysis care, allowing them to provide higher quality of care for their patients.
Motivations and Learning Objectives in the EHD Program
The next phase of this study explored why clinicians and administrators attended the EHD program, along with the skills that they were expecting to gain. These data were compiled from the pre-arrival surveys and the semi-structured interviews.
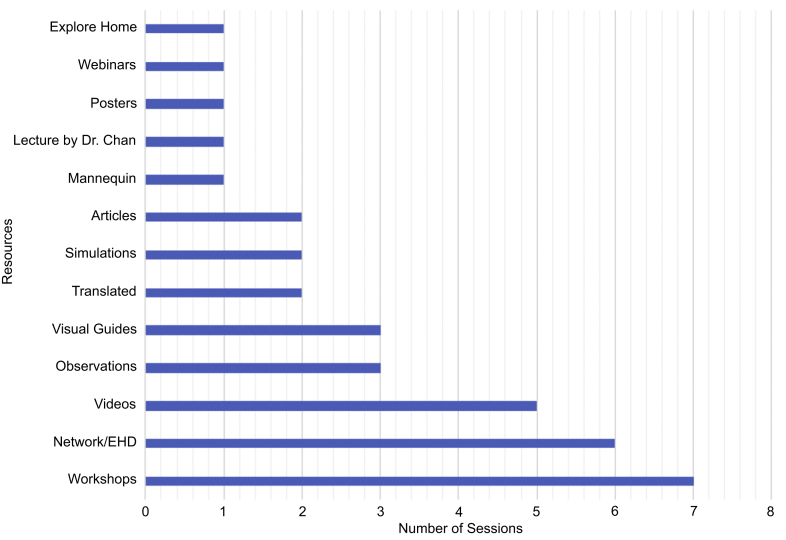
The primary motivation for participating in the EHD program was to use the new knowledge gained from the EHD program to implement new home dialysis programs in their home institutions. Other motivations for joining the program were as follows: (i) to improve patient care, training models, or accessibility of specialized patient care in an existing home dialysis program; (ii) to support home therapy initiatives; (iii) to uphold professional nursing practice standards in home dialysis; (iv) to establish connections and network opportunities with the Canadian health care system; and (v) to gain exposure to different practices and perspectives with respect to home dialysis. Figure 1 describes the resources participants thought were or would be effective in helping them achieve their learning objectives in the EHD program, with more details provided in Table 2.
Figure 1.
Number of interview sessions in which each resource was identified as beneficial to Explore Home Dialysis (EHD) clients.
Table 2.
Detailed description of suggested resources for EHD alumni
| Format | Materials |
|---|---|
| Online resources | Web portal with additional content Helpdesk for EHD alumni Web resources/webinars |
| Presentation and talks | PowerPoints Recorded lectures and talks to support meetings to sell idea to others in the institution Demonstrations |
| Printed and visual material | Posters Brochures Videos (modules) Articles Manuals Home dialysis information packages Leaflets Diagrams Photo guides Models Translated booklets Books Program book Short written documents Printouts |
| Workshops, discussions, and hands-on activities | Workshops about different types of home dialysis Educational meetings Simulators: cannulators, equipment simulators, patient simulators demonstrating problems that patients may have at home Tutorials Peer sessions/Small group discussions |
| Existing UHN resources | UHN protocols UHN training manual Copy of UHN’s patient agreement forms for nocturnal center |
EHD, Explore Home Dialysis; UHN, University Health Network.
EHD clients had well-established goals and learning objectives related to the EHD program, indicating a clear need for home dialysis training programs such as EHD.
Selling the Concept of Home Dialysis
EHD clients wanted to learn how to “pitch” or sell the idea of novel home dialysis treatments, such as home hemodialysis, to their colleagues and management teams in their home institutions. Clients also wanted to learn more about the benefits, importance, adequacy, and efficacy of home dialysis; information to be used when discussing the advantages of a home dialysis program in their home institutions.
Managing Home Dialysis Programs
Clients wanted to learn to successfully manage home dialysis programs by observing how these programs are managed at UHN. More specifically, participants were interested in understanding the administrative details of home dialysis, how the program is financed, how much it costs, and how the program manages and handles insurance coverage and government reimbursements. Participants also expressed an interest in learning about the business aspects of the program, as well as the equipment and nephrology delivery models currently in place at UHN.
Getting a Complete Picture of Home Dialysis at UHN
EHD clients were interested in observing and understanding how the home dialysis program operates at UHN and adapting the knowledge to help support the building or improvement of the home dialysis program(s) in their home institutions. Topics of interest included the following: (i) what daily operations in home dialysis look like; (ii) how patients perform home dialysis independently at home; (iii) what are some of the challenges experienced in home dialysis; (iv) details regarding vascular access and other clinical aspects of home hemodialysis; (v) how to select, follow-up, and support patients at home; (vi) how to manage patient safety concerns and complications; (vii) how to troubleshoot and manage issues; (viii) how to train clinicians and patients in home dialysis; and (ix) what are the staffing, equipment, and technical resources required to successfully place patients in the various types of home dialysis. Some clients wanted to better understand how different members of a multidisciplinary team interact and work with others in home dialysis.
Personal Development
Some clients were interested in using this opportunity to learn or develop transferable skills in interviewing, negotiation, and leadership, as well as teamwork and collaboration. Others wanted to learn how to personally set up home hemodialysis technology and learn about technical support and maintenance of the home hemodialysis machines. Participants wanted to learn how to effectively coordinate and communicate in inpatient and community settings.
Training at Home Institution
Participants described various topics in which they wanted to train patients, caregivers, and clinicians in their home country or home institution. These included the following: (i) topics related to the dialysis machine, connections, safety mechanisms, backups, and monitoring devices; (ii) fundamentals of business; (iii) how to deal with medical complications; (iv) how to manage change in their organization; (v) teamwork and collaboration; and (vi) how to communicate effectively with technicians. Participants explained that certain tools such as online resources, presentations and talks, printed and visual material, workshops, discussions, and existing UHN home dialysis resources would be useful once back at their home institution (see Table 2).
Evaluation of the EHD Program
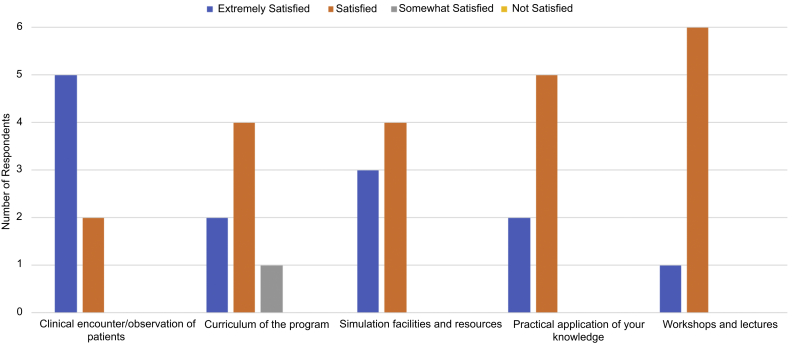
The second phase our study focused on the evaluation of the EHD program. Seven of the 23 participants filled out the postdeparture questionnaire. Participants primarily indicated they were satisfied or extremely satisfied with various aspects of the EHD program. Figure 2 presents a summary of participants’ responses about their overall experiences in the EHD program, with respect to clinical encounters and observations of patients, the curriculum of the program, the simulation facilities and resources, practical application of knowledge, and workshops and lectures.
Figure 2.
Summary of the postdeparture questionnaire.
Participants also indicated areas of improvement that would have better ensured the program fit their needs. These included (i) more workshops, (ii) more practical activities, (iii) more observations, and (iv) greater availability of educational documents that participants could bring back to nurses and physicians.
Barriers to Home Dialysis Deployment from the Perspective of EHD Clients
We have identified that within our participant sample, the current demand for home dialysis programs is not being met, as several barriers are still preventing these innovators from establishing new home dialysis programs in their home countries. The 6 major categories of barriers identified by our participants were as follows: (i) financial, (ii) technological, (iii) infrastructural, (iv) governance and political, (v) institutional and cultural, and (vi) patient barriers. Table 3 provides information about incidence and Table 4 provides detailed descriptions of each barrier category.
Table 3.
Summary of barriers to the deployment of home dialysis around the world
| Category | Percentage of countries (n = 11) | List of countries | Percentage of interview sessions (n = 16) |
|---|---|---|---|
| Financial barriers | 100 | Australia, Brazil, Canada, Colombia, Germany, Hong Kong, Hungary, Iran, Jordan, Singapore, Thailand | 94 |
| Technological barriers | 36 | Australia, Hong Kong, Iran, Singapore | 31 |
| Infrastructural barriers | 91 | Australia, Brazil, Canada, Germany, Hong Kong, Hungary, Iran, Jordan, Singapore, Thailand | 63 |
| Governance and political barriers | 27 | Singapore, Hong Kong, Iran | 19 |
| Institutional and cultural barriers | 91 | Australia, Brazil, Canada, Germany, Hong Kong, Hungary, Iran, Jordan, Singapore, Thailand | 88 |
| Patient barriers | 91 | Australia, Brazil, Canada, Germany, Hong Kong, Hungary, Iran, Jordan, Singapore, Thailand | 88 |
Table 4.
Description of each of the barrier categories
| Barrier | Barrier description |
|---|---|
| Financial | Patients in home dialysis require a personal dialysis machine (either home hemodialysis or peritoneal dialysis) and a constant supply of clean water (mainly for home hemodialysis), energy, and various machine consumables. Because the practice of home dialysis is new in many countries, many current health care financing and reimbursement models do not enable or support home therapies of this nature. Thus, many patients currently cannot afford the costs associated with setting up, running, and maintaining dialysis equipment in their homes. |
| Technological | Home hemodialysis machines and peritoneal dialysis machines are complex to set up and operate. Patients often struggle with self-cannulation and lack support in setting up, operating, and/or troubleshooting problems encountered during dialysis. The complex nature of home dialysis technology, in combination with poor technical support, often results in challenges when implementing home dialysis on a wide scale. |
| Infrastructural | Home dialysis requires patients to have dedicated space in their homes in addition to appropriate water, sewage, and electrical infrastructure. Several countries covered in this project do not provide the necessary infrastructure, requiring patients to cover the costs to establish the minimum requirements for home dialysis. Clinicians require dedicated clinical space to educate and train patients on operating the equipment and performing dialysis on their own. Limited resources in some of these hospitals prevents the establishment of home dialysis programs. |
| Governance and political | Government and policies largely influence the success of home dialysis programs. The availability of government funding support, regulations, and standards in home dialysis care can greatly encourage or discourage patients and clinicians to consider home dialysis. Unfortunately, some governing bodies regard home dialysis as a luxury and prioritize other treatment methods, discouraging the implementation of home dialysis programs. |
| Institutional and cultural | Home dialysis requires the collaboration of a diverse team of clinicians, patients, and their families. Because of some deeply rooted cultural views and practices, some home dialysis programs around the world experience difficulties recruiting and/or training patients to independently perform self-dialysis. Some examples include staff being skeptical of prescribing home dialysis to patients and skeptical letting patients take a more active role in their therapy. The cultural norm of the sick having to be taken care of may introduce cultural barriers to home dialysis, as home dialysis requires the patient to play a more active role in the therapy. A successful home dialysis program must consider the influence of patient, institutional, and societal culture during development and implementation. |
| Patient | Because home dialysis relies on patients and caregivers to independently operate and troubleshoot dialysis equipment, the success and uptake of home dialysis heavily depends on how comfortable patients are with the procedures and technology. Patients may be uncomfortable or afraid of having problems at home while performing home dialysis and not having a clinician available to help. The age and education level of the patient population may vary from country to country, which will influence how open patients are to home dialysis. Patients’ families may or may not be supportive of home dialysis due to the added load on the family as caregivers. Consequently, negative patient and caregiver perceptions toward home dialysis can greatly discourage patients from transferring into home dialysis programs. |
Discussion
The data collected in this evaluation showcase an increased demand for home dialysis in the countries surveyed, with strong interest for establishing new programs and increased patient and provider interest. The limited availability of in-center dialysis in these countries drives an interest to expand the reach of dialysis services through home dialysis. However, this demand is not met because many countries do not currently have home dialysis available to their patients and the ones that do, offer only peritoneal dialysis. For example, participants from Iran, Singapore, Brazil, Thailand, Hungary, and Colombia were interested in establishing new home hemodialysis programs in their institutions due to the lack of availability of this treatment option in their institutions at the time of our data collection (2014–2016).
However, establishing and running new home dialysis programs is not an easy endeavour as there was an absence of well-established guidelines and protocols to support the development of new programs by these clinicians. In the absence of this material, many have sought the opportunity to come to the UHN to join the EHD program. This was an opportunity to experience how the UHN team designed and implemented a program, selects patients, provides training to patients and family members, as well as choosing the ideal treatment type for each patient. The major motivation to attend the EHD program in Toronto was the opportunity to learn how to create and operate a home dialysis program in their home countries. The positive feedback provided by EHD clients indicated the overall perceived benefit of the program, with clear opportunities for improvement. Establishment of more extensive documentation and guidelines to support the creation of new home dialysis programs was a high priority, along with educational material that could be used to train local staff on home dialysis procedures and program characteristics. Examples of the types of materials that the EHD clients were interested in leveraging are presented in Table 2, with emphasis on (i) materials that could be used to train their staff back in their home institution, (ii) access to UHN protocols and training manuals as a printed material to be available after returning to their home institution, (iii) opportunities to connect to their peers and EHD mentors after the end of their tenure at the EHD program, and (iv) support material to demonstrate the financial viability and benefit of home dialysis programs.
The participants who described several barriers to the deployment of home dialysis have limited the expansion and uptake of home dialysis as a treatment option, with financial, institutional, infrastructural, and patient barriers being the major issues. These results are an indication of the complexity of deploying home dialysis in these countries, as simple infrastructural needs, such as clean water and stable electricity, which are necessary for home hemodialysis, may not be available.
As a limitation of our study, we would like to acknowledge the small sample used in this evaluation and the limited diversity in terms of the origin and background of the participants. The use of a convenience sample including individuals who participated in the program has resulted in a potentially biased cohort that has already shown interest for new home dialysis programs. Ultimately, the results presented herein showcase the absence of supporting materials available to guide the establishment of new home dialysis programs. The EHD program is a great opportunity to support the establishment of these new programs and to support the expansion of home dialysis around the world.
Disclosure
CTMC has consulted for Baxter, NxStage, and Medtronic Inc. JMB has consulted for Baxter Canada, Baxter Global, NxStage, and Cook Medical. All the other authors declared no competing interests.
Acknowledgments
The authors acknowledge the support of Baxter for the development of this project by providing seed funding for the initial development of the EHD Program.
References
- 1.Nahas A.M.E., Bello A.K. Chronic kidney disease: the global challenge. Lancet. 2010;365:331–340. doi: 10.1016/S0140-6736(05)17789-7. [DOI] [PubMed] [Google Scholar]
- 2.Liyanage T., Ninomiya T., Jha V. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 3.Walker R.C., Hanson C.S., Palmer S.C. Patient and caregiver perspectives on home hemodialysis: a systematic review. Am J Kidney Dis. 2015;65:451–463. doi: 10.1053/j.ajkd.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 4.United States Renal Data System. United States renal data system 2016 annual data report. Available at: https://www.usrds.org/adr.aspx. Accessed December 1, 2016.
- 5.Hope J. A patient perspective on the barriers to home dialysis. J Ren Care. 2013;39:3–8. doi: 10.1111/j.1755-6686.2013.00333.x. [DOI] [PubMed] [Google Scholar]
- 6.Nissenson A.R. Restructuring the ESRD payment system in the United States. Kidney Int. 2004;66:466–476. doi: 10.1111/j.1523-1755.2004.00753.x. [DOI] [PubMed] [Google Scholar]
- 7.Zacharias J., Komenda P., Olson J. Home hemodialysis in the remote Canadian north: treatment in manitoba fly-in communities. Semin Dial. 2011;24:653–657. doi: 10.1111/j.1525-139X.2011.01004.x. [DOI] [PubMed] [Google Scholar]
- 8.Cafazzo J.A., Leonard K., Easty A.C. Patient perceptions of remote monitoring for nocturnal home hemodialysis. Hemodial. Int. 2010;14:471–477. doi: 10.1111/j.1542-4758.2010.00473.x. [DOI] [PubMed] [Google Scholar]
- 9.Wong J., Eakin J., Migram P. Patients’ experiences with learning a complex medical device for the self-administration of nocturnal home hemodialysis. Nephrol Nurs J. 2009;36:27–32. [PubMed] [Google Scholar]
- 10.Tong A., Palmer S., Manns B. The beliefs and expectations of patients and caregivers about home haemodialysis: an interview study. BMJ Open. 2013;3:e002148. doi: 10.1136/bmjopen-2012-002148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cafazzo J.A., Leonard K., Easty A.C. Patient-perceived barriers to the adoption of nocturnal home hemodialysis. Clin J Am Soc Nephrol. 2009;4:784–789. doi: 10.2215/CJN.05501008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oliver M.J., Garg A.X., Blake P.G. Impact of contraindications, barriers to self-care and support on incident peritoneal dialysis utilization. Nephrol Dial Transplant. 2010;25:2737–2744. doi: 10.1093/ndt/gfq085. [DOI] [PubMed] [Google Scholar]
- 13.Walker R.C., Howard K., Morton R.L. Patient and caregiver values, beliefs and experiences when considering home dialysis as a treatment option: a semi-structured interview study. Nephrol Dial Transplant. 2016;31:133–141. doi: 10.1093/ndt/gfv330. [DOI] [PubMed] [Google Scholar]
- 14.Baillie J., Lankshear A. Patient and family perspectives on peritoneal dialysis at home: findings from an ethnographic study. J Clin Nurs. 2015;24:222–234. doi: 10.1111/jocn.12663. [DOI] [PubMed] [Google Scholar]
- 15.Ludlow M.J., George C.R., Hawley C.M. How Australian nephrologists view home dialysis: results of a national survey. Nephrology. 2011;16:446–452. doi: 10.1111/j.1440-1797.2010.01403.x. [DOI] [PubMed] [Google Scholar]
- 16.Osterlund K., Mendelssohn D., Clase C. Identification of facilitators and barriers to home dialysis selection by Canadian adults with ESRD. Semin Dial. 2014;27:160–172. doi: 10.1111/sdi.12183. [DOI] [PubMed] [Google Scholar]
- 17.Agar J.W.M., Hawley C.M., Kerr P.G. Home hemodialysis in Australia and New Zealand: how and why it has been successful. Semin Dial. 2011;24:658–663. doi: 10.1111/j.1525-139X.2011.00992.x. [DOI] [PubMed] [Google Scholar]
- 18.Rope R.W., Pivert K.A., Parker M.G. Education in nephrology fellowship: a survey-based needs assessment. J. Am. Soc. Nephrol. 2017;28:1983–1990. doi: 10.1681/ASN.2016101061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergjan M., Schaepe C. Educational strategies and challenges in peritoneal dialysis: a qualitative study of renal nurses’ experiences. J Clin Nurs. 2016;25:1729–1739. doi: 10.1111/jocn.13191. [DOI] [PubMed] [Google Scholar]
- 20.Golper T.A., Mehrotra R., Schreiber M.S. Is Dorothy correct? The role of patient education in promoting home dialysis. Semin Dial. 2013;26:138–142. doi: 10.1111/sdi.12086. [DOI] [PubMed] [Google Scholar]
- 21.Hutchison A.J., Courthold J.J. Enabling self-management: selecting patients for home dialysis? NDT Plus. 2011;4:7–10. doi: 10.1093/ndtplus/sfr151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morita P.P., Cafazzo J.A. Challenges and paradoxes of human factors in health technology design. JMIR Hum Factors. 2015;3:1–7. doi: 10.2196/humanfactors.4653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrett J. The elements of user experience: user-centered design for the Web and beyond. Available at: http://books.google.com/books?hl=en&lr=&id=9QC6r5OzCpUC&oi=fnd&pg=PT4&dq=Elements+of+User+Experience,The:+User-Centered+Design+for+the+Web+and+Beyond&ots=mG_8Mna8Vu&sig=JSups1ou7_jhTG4fOseHpGsdwF0. Accessed July 15, 2014.
- 24.Johnson R.B., Onwuegbuzie A.J. Mixed methods research: a research paradigm whose time has come. Educ Res. 2004;33:14–26. [Google Scholar]
- 25.Denzin N.K., Lincoln Y.S. 4th ed. SAGE Publications; Thousand Oaks, CA: 2005. The SAGE Handbook of Qualitative Research.https://books.google.co.uk/books/about/The_SAGE_Handbook_of_Qualitative_Researc.html?id=X85J8ipMpZEC&redir_esc=y Available at: Accessed. [Google Scholar]
- 26.Glasber B.G., Strauss A. Routledge; New York: 1999. Discovery of Grounded Theory, Strategies for Qualitative Research. [Google Scholar]