See Clinical Research on Page 222
Depression is common in patients with predialysis chronic kidney disease (CKD), with prevalence rates of approximately 20% to 25%.1 In patients with CKD, depression is associated with poor medical outcomes, including a higher risk of acute kidney injury, CKD progression, and cardiovascular events.2 Although depression has been clearly associated with increased mortality in patients with end-stage renal disease (ESRD),2 the association between depression and mortality in patients with CKD is less clear. In a study of 598,153 US veterans with CKD, depression was associated with a 1.5 times higher risk of mortality over a median follow-up of 4.7 years.3 Conversely, in a study of 628 patients from the African American Study of Kidney Disease and Hypertension (AASK) cohort, depressive affect (using time-varying Beck Depression Inventory II [BDI-II] scores) was significantly associated with cardiovascular death/hospitalizations but not all-cause death.4 Only 1 large study of patients with CKD has examined the effect of depression on mortality after the development of ESRD, finding only a weak association between the two.5
In this issue of KI Reports, Tuot et al. attempt to answer the question of whether depressive symptoms are associated with all-cause mortality (both before and after ESRD initiation) in patients with CKD.6 Their retrospective study of the Chronic Renal Insufficiency Cohort (CRIC) included 3739 adults with an estimated glomerular filtration rate (eGFR) of 20 to 70 ml/min per 1.73 m2 who self-identified as black, white, or Hispanic, and were followed up for a median of 6.8 years. The authors found that 16.3% had a baseline BDI score of >14 and 18.2% reported antidepressant use. Similar to other studies, risk factors for depression included younger age, female sex, nonwhite race/ethnicity, lower household income, and comorbid conditions (including a lower eGFR and proteinuria >1 g/g). As for their primary objective, the authors found that participants with a BDI >14 had a 1.27 higher risk of all-cause mortality compared to participants with a BDI ≤14. Interestingly, antidepressant medication use did not attenuate this risk. The authors also found a differential association of depressive symptoms with mortality by race. Baseline BDI >14 was associated with higher risk of death among white participants, a trend toward higher mortality among Hispanic participants, but no association with all-cause mortality among black participants. To further examine the effect of depression on mortality by race, the authors performed a similar analysis among patients from the African American Study of Kidney Disease (AASK) study. This cohort included 611 black participants with eGFRs of 20–65 ml/min per 1.73 m2 that, similarly, did not appear to have an association of depressive symptoms with all-cause mortality.
The strengths of this study were that it included 2 large cohorts of participants with CKD and depressive symptoms. In addition, the authors included a sensitivity analysis (results were similar for a BDI >16) and a validation cohort (AASK). Finally, unlike some prior studies of CKD and depression, they focused their analysis on those with at least mild depressive symptoms (BDI >14), excluding patients with minimal symptoms where depression and distress often overlap.4 The limitations of the study are its retrospective design, which precludes any conclusions about the effects of antidepressant medication in this population, as well as the limited number of Hispanic patients. In addition, depressive symptoms were examined only at study onset due to a high number of missing surveys at follow-up. Thus, there could be a significant proportion of participants in which depression developed over time, due to the increasing burdens of CKD, that were neither identified nor included in the analysis.
This study confirms an association between depression and mortality in patients with CKD. More importantly, however, it introduces 2 additional questions about the characteristics of depression in CKD that promise to move the field further. Why is there a difference in depression mortality by race, and why is there no attenuation of mortality risk with antidepressant use? These questions highlight the dearth of research into the mechanisms of depression in CKD. The problem of depression and its effects have been defined, but the question of why this problem exists remains to be answered.
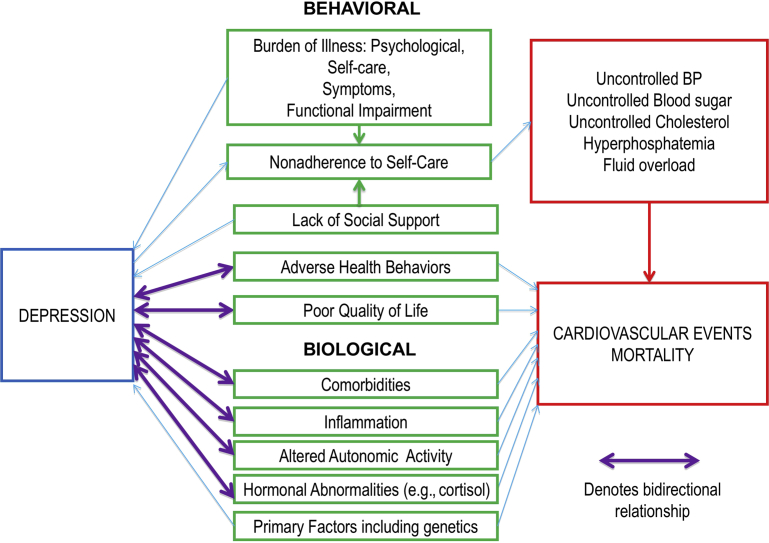
Depression in CKD likely results from a combination of behavioral and biological mechanisms that are unique for different subgroups and individuals with CKD (Figure 1).2 Potential behavioral mechanisms include burdens of illness, lack of social support, adverse health behaviors, and poor quality of life. Potential biological mechanisms include comorbidities, inflammation, altered autonomic activity, and hormonal abnormalities. The heterogeneity of CKD makes it likely that different mechanisms of depression affect different subgroups of CKD patients, explaining the differential effect of depression on mortality in black versus white versus Hispanic CKD patients. Only with further research into these subgroup-specific mechanisms can effective individualized interventions that improve outcomes be designed. A generic “one size fits all” treatment plan for patients with CKD and depression has thus far been ineffective. In a recent randomized, double-blind, placebo-controlled trial involving 201 participants with stage 3 to 5 CKD and depression, sertraline use did not show an improvement in depressive symptoms compared to placebo.7 This finding highlights the need to examine patient-specific interventions that target individualized behavioral and biological causes of depression. In patients with diabetes or coronary artery disease and depression, collaborative care models that combine medical, psychiatric, and psychological care have led to improvements in mood and medical outcomes.8 A similar model is likely needed to improve outcomes for patients with CKD and depression. Ultimately, until we understand the mechanisms of depression in CKD and design interventions that target these mechanisms, we are unlikely to meaningfully improve mood or medical outcomes in this population.
Figure 1.
Mechanisms of depression and adverse medical outcomes. BP, blood pressure. Reprinted from Shirazian S, Grant CD, Aina O, et al. Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep. 2017;2:94–107,2 with permission from Elsevier. Copyright © 2017 International Society of Nephrology.
Disclosure
The author declared no competing interests.
References
- 1.Palmer S., Vecchio M., Craig J.C. Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies. Kidney Int. 2013;84:179–191. doi: 10.1038/ki.2013.77. [DOI] [PubMed] [Google Scholar]
- 2.Shirazian S., Grant C.D., Aina O. Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep. 2017;2:94–107. doi: 10.1016/j.ekir.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balogun R.A., Abdel-Rahman E.M., Balogun S.A. Association of depression and antidepressant use with mortality in a large cohort of patients with nondialysis-dependent CKD. Clin J Am Soc Nephrol. 2012;7:1793–1800. doi: 10.2215/CJN.02650312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fischer M.J., Kimmel P.L., Greene T. Elevated depressive affect is associated with adverse cardiovascular outcomes among African Americans with chronic kidney disease. Kidney Int. 2011;80:670–678. doi: 10.1038/ki.2011.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Molnar M.Z., Streja E., Sumida K. Pre-ESRD depression and post-ESRD mortality in patients with advanced CKD transitioning to dialysis. Clin J Am Soc Nephrol. 2017;12:1428–1437. doi: 10.2215/CJN.00570117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tuot DS, Lin F, Norris K. Depressive symptoms associate with race and all-cause mortality in patients with CKD. Kidney Int Rep. 2019;4:222–230. doi: 10.1016/j.ekir.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hedayati S.S., Gregg L.P., Carmody T. Effect of sertraline on depressive symptoms in patients with chronic kidney disease without dialysis dependence: the CAST randomized clinical trial. JAMA. 2017;318:1876–1890. doi: 10.1001/jama.2017.17131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katon W.J., Lin E.H., Von Korff M. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]