Abstract
The role of vitamin D3 (VitD3) in the upregulation of osteopontin (OPN) and eNOS in the endothelium of cerebral arteries after subarachnoid hemorrhage (SAH) is investigated. The endovascular perforation SAH model in Sprague-Dawley rats (n = 103) was used. The VitD3 pretreatment (30 ng/kg) increased endogenous OPN and eNOS expression in cerebral arteries compared with naïve rats (n = 5 per group). Neurobehavioral scores were significantly improved in Pre-SAH+VitD3 group compared with the SAH group. The effects of VitD3 were attenuated by intracerebroventricular (i.c.v) injections of siRNA for the vitamin D receptor (VDR) and OPN in Pre-SAH+VitD3+VDR siRNA and Pre-SAH+VitD3+OPN siRNA rats, respectively (n = 5 per group). The significant increase of VDR, OPN and decrease of C44 splicing in the cerebral arteries of Pre-SAH+VitD3 rats lead to an increase in basilar artery lumen. The increase in VDR expression led to an upregulation and phosphorylation of AMPK and eNOS, especially dimer form, in endothelium of cerebral artery. The results provide that VitD3 pretreatment attenuates cerebral artery remodeling and vasospasm through the upregulation of OPN and phosphorylation of AMPK (p-AMPK) and eNOS (p-eNOS) at Ser1177-Dimer in the cerebral arteries. Vitamin D may be a useful new preventive and therapeutic strategy against cerebral artery remodeling in stroke patients.
Keywords: Subarachnoid hemorrhage, vitamin D, AMPK, endothelial nitric oxide synthase, artery endothelium
Introduction
Aneurysmal SAH is a devastating form of hemorrhagic stroke with significant mortality and long-term morbidity among survivors1,2 for which no effective treatments are available.3,4 Studies during past few decades concerning cerebral vascular spasm have mostly been focused on finding therapeutic strategies for aneurysmal SAH, unfortunately mortality and poor clinical outcomes after SAH remain considerably high.5,6 In recent years, researchers have focused on elucidating the mechanisms of early brain injury (EBI) after SAH7 and are working to resolve the limitations of past studies.
Vitamin D is a neuroprotective hormone that regulates a number of genomic and non-genomic pathways.8,9 VDR is a ubiquitous nuclear transcription receptor expressed in human body tissues including endothelium.10 Moreover, vitamin D regulates endothelium relaxation factors such as nitric oxide (NO), through a VDR-dependent pathway, with its insufficiency associated with a profoundly increased risk for endothelial dysfunction and hypertension.11,12 Epidemiological and basic science studies suggest that vitamin D deficiency is associated with neurological and cerebrovascular diseases, including stroke.13–15 However, while vitamin D deficiency is associated with an increased risk of stroke and adverse outcomes for post-stroke patients,16 studies are limited concerning vitamin D deficiency in vivo.17,18
Our previous studies have shown that vitamin D upregulates endogenous OPN in rat brain hemispheres and leads to blood–brain barrier integrity in the micro vessels after SAH.19 Additionally, cerebral OPN is primarily expressed in astrocytes and endothelial cells after SAH and protects vascular smooth muscle remodeling and cerebral vasospasm in EBI after SAH.20,21 However, the preventive effects of vitamin D induced upregulation of OPN in the endothelium of cerebral arteries after SAH have not been elucidated. We hypothesized that vitamin D affects the endothelium of cerebral arteries, not only micro vessels, with a pleiotropic effect of vitamin D upregulating OPN. Thus, we aimed to identify a role of vitamin D upregulated OPN on a CD44-(a receptor of OPN) dependent intracellular mechanism in the endothelium of cerebral arteries of rats after SAH.
Materials and methods
All experimental protocols and procedures were approved by the Institutional Animal Care and Use Committee of Loma Linda University, are in accordance with the ARRIVE (Animal Research: Reporting In Vivo Experiments) guidelines, and comply with the NIH Guidelines for the Use of Animals in Neuroscience Research.
Animals and treatment
Adult male Sprague-Dawley rats (n = 103, 300–350 g; Harlan Indianapolis, IN) were housed in a light-and-temperature-controlled environment and fed ad libitum. Naïve rats were pretreated a single 30 ng/kg of VitD3 (calcitriol, 71820, Cayman Chemical, MI, USA) (+VitD3) by intranasal route to study the effect of VitD3 on endogenous expression of OPN in the cerebellum, brain stem and cerebral arteries at 24 h after the pretreatment (n = 5 per group). Next, animals were divided randomly into the following groups: Sham, SAH time course at 3, 6, 12, 24, 72 h, Sham operated plus vehicle (5% ethanol) (Sham, n = 5), SAH plus vehicle (SAH, n = 5), SAH plus a single 30 ng/kg of VitD3 pretreatment 24 h before surgery (Pre-SAH+VitD3, n = 5). Lastly, to examine the molecular mechanism, 15 animals were divided randomly into the following groups: Pre-SAH+VitD3+Control siRNA (n = 5), Pre-SAH+VitD3+VDR siRNA (n = 5), Pre-SAH+ VitD3+OPN siRNA (n = 5). All animals were sacrificed 24 h after surgery.
Surgery procedures
The endovascular perforation model of SAH was performed as previously described.19,22 Briefly, rats were anesthetized and kept on a ventilator during surgery with 2–3% isoflurane in air (isoflurane was reduced to 1.5% at the moment of puncture). A sharpened 4–0 nylon suture was inserted into the left internal carotid artery though the external carotid artery and common carotid bifurcation. The 3-cm suture was advanced until resistance was felt at the bifurcation of the anterior and middle cerebral arteries. The suture was then further advanced to puncture the vessel and then immediately withdrawn after artery perforation. During sham operations, the suture was inserted into the left carotid artery; however, no perforation was performed. After removal of the suture, the skin incision was sutured and rats were housed individually in heated cages until recovery.
Neurological score evaluation
At 24 h after surgery, neurological scores were evaluated in a blinded fashion using a modification of the Garcia scoring system as previously described.23 This composite sensorimotor assessment evaluated the rodent’s spontaneous activity, spontaneous movement of all limbs, vibrissae touch, forelimbs outstretching and climbing wall of cage. Each subtest was scored from 0 (minimum) to 3 (maximum). Animals were also evaluated for walking distances on a wooden beam for 1 min and wire hanging ability for 30 s, each scored from 0 to 4.
SAH grading
The severity of SAH was blindly evaluated by the SAH grading system immediately after euthanasia as previously described.24 Briefly, after removing the brain from the skull, a photograph of the base of the brain was divided into six parts that were scored (0–3) according to amount of subarachnoid blood present, and a total score was calculated as the sum of each sections score. Operated animals received a total score ranging from 0 (no SAH) to 18 (most severe SAH), and SAH rats with a score of 7 or less were excluded from this study (Table 1).
Table 1.
Experimental design and number of animals used per group.
| Part | Groups | Neuro test WB | Histology IHC | Mortality (%) | Exclusion | Sum |
|---|---|---|---|---|---|---|
| 1 | VitD3 pretreatment study: | |||||
| Naïve | 5 | 2 | – | – | 7 | |
| +VitD3 | 5 | 2 | – | – | 7 | |
| 2 | Time course study (n = 5 per group): | |||||
| Sham | 5 | – | – | – | 5 | |
| SAH (3, 6, 12, 24, 72 h) | 25 | – | 6 (18%) | 3 | 34 | |
| 3 | Outcome study: | |||||
| Sham | 5 | 3 | – | – | 8 | |
| SAH | 5 | 3 | 3 (23%) | 2 | 13 | |
| Pre-SAH+VitD3 | 5 | 3 | 2 (18 %) | 1 | 11 | |
| 4 | Molecular mechanism study: | |||||
| Pre-SAH+VitD3+VDR siRNA | 5 | – | 1 (17%) | – | 6 | |
| Pre-SAH+VitD3+OPN siRNA | 5 | – | 1 (17%) | – | 6 | |
| Pre-SAH+VitD3+Control siRNA | 5 | – | – | 1 | 6 | |
| Total | 70 | 13 | 13 (17%) | 7 | 103 |
Note: Sprague-Dawley male rats with 300–350 g body weights were used. +VitD3, a single intranasal treated 30 ng/kg of calcitriol 24 h before.
SAH: subarachnoid hemorrhage; Pre-SAH+VitD3: VitD3 treated 24 h before SAH induction; VDR: vitamin D receptor; OPN: osteopontin; siRNA: small interfering ribonucleic acid; WB: Western blot; IHC: immunohistochemistry.
Intracerebroventricular administration
Intracerebroventricular (i.c.v) administration was performed as previously described.19 Briefly, rats were placed in a stereotaxic apparatus under 2.5% isoflurane anesthesia. The needle of a 10 ml Hamilton syringe (Microliter 701; Hamilton Company, Reno, NV) was inserted, through a burr hole, into the right lateral ventricle at the following coordinates relative to the bregma: 0.92 mm posterior, 1.5 mm lateral, and 3.3 mm below the horizontal plane of the skull. VDR small interfering ribonucleic acid (siRNA) (SR508804, OriGene Technologies, Inc., MD, USA), OPN siRNA Sigma-Aldrich, MO, USA), and a scrambled negative control siRNA were prepared at 1000 pMol each in RNAse free resuspension buffer and was injected 48 h before SAH induction surgery at a rate of 2 µl/min with a total volume of 10 µL.
Western blot
Western blot analyses of samples from the cerebellum and brain stem were performed as previously described.19,25 Artery samples including the Wills circle and basilar artery were collected from the basal cisterns and snap frozen in liquid nitrogen. Artery samples were homogenized using a polypropylene pestle in 200 mL of RIPA Lysis Buffer System (sc-24948, Santa Crus, CA, USA). Equal amounts of sample protein (30 mg) were loaded onto an SDS-PAGE gel. After electrophoresis and transfer of the samples to a nitrocellulose membrane, the membrane was blocked for 1 h at 21℃ then incubated overnight at 4℃ with the following primary antibodies: VDR (1:500, sc-13133), OPN (1:1000, sc-21742), β-Actin (1:5000, I-19), endothelial nitric oxide synthase (eNOS, 1:1000, sc-653), p-eNOS-Ser1177 (1:1000, sc-12972), p-eNOS-Thr495 (1:1000, sc-136519) (Santa Cruz Biotechnology Inc., Texas, USA), and adenosine monophosphate-activated protein kinase (AMPK, 1:2000, #5832), p-AMPK (1:2000, #2535) (Cell Signaling, MA, USA). Next, the membranes were incubated at room temperature for 1 h with the appropriate secondary antibodies (1:5000, Santa Cruz Biotechnology Inc.). Immunoblots were then probed with ECL Amersham Western blotting detection reagents (Amersham Biosciences UK Ltd, PA, USA). Blot bands were quantified by densitometry using image J software (Image J 1.4, NIH, USA). β-Actin was used as the loading control.
Morphometric analysis
The brain sections encompassing the BA were stained with hematoxylin and eosin according to the routine protocol as previously described.21 Histological photographs were serially captured in LASX software with a Leica DMi8 microscope (Leica Microsystems, Germany). At the level of the pons-cerebellum and midbrain, the cross-sectional areas of BA were measured using Image J software (Image J 1.4, NIH, USA).
Immunofluorescence staining
Deeply anesthetized rats were perfused transcardially with 60 mL of PBS followed by 60 mL of 10% paraformaldehyde through the upper part of the body. The brains were removed, fixed for 24 h in 10% paraformaldehyde followed by 30% sucrose for three days, then embedded into OCT compound (Scigen Scientific Gardena, CA, USA) and frozen at −80°. The tissues were cut on a cryostat (LM3050S; Leica Microsystems, Bannockburn, III, Germany) into 10 µm thick slices of basilar artery located between the pons-cerebellum and midbrain and mounted on poly-L-lysine-coated glass slides. Double-fluorescence labeling was performed as described previously.26 Anti-CD34 (1:500, 250591, Abbiotec, San Diego, CA), anti-CD31 (1:500, ab119339, abcam, Cambridge, MA), anti-OPN (1:100, sc-21742), VDR (1:500, sc-13133), and p-eNOS-Ser1177 (1:500, sc-12972), (Santa Cruz Biotechnology Inc., Dallas, TX), antibodies were applied and incubated overnight at 4℃, followed by incubation for 1 h at room temperature with secondary antibodies at a dilution of 1:500. Slide pictures were taken in LASX software with a Leica DMi8 fluorescence microscope (Leica Microsystems, Germany).
Statistical analysis
Data analysis was performed using IBM SPSS Statistics software version 21 (IBM, Armonk, New York, USA). Data are shown as mean ± SD and analyzed by one-way ANOVA followed by LSD post hoc analysis for comparison among all groups. Independent Samples T-Test was used to compare two groups. A P value of < 0.05 was considered statistically significant.
Results
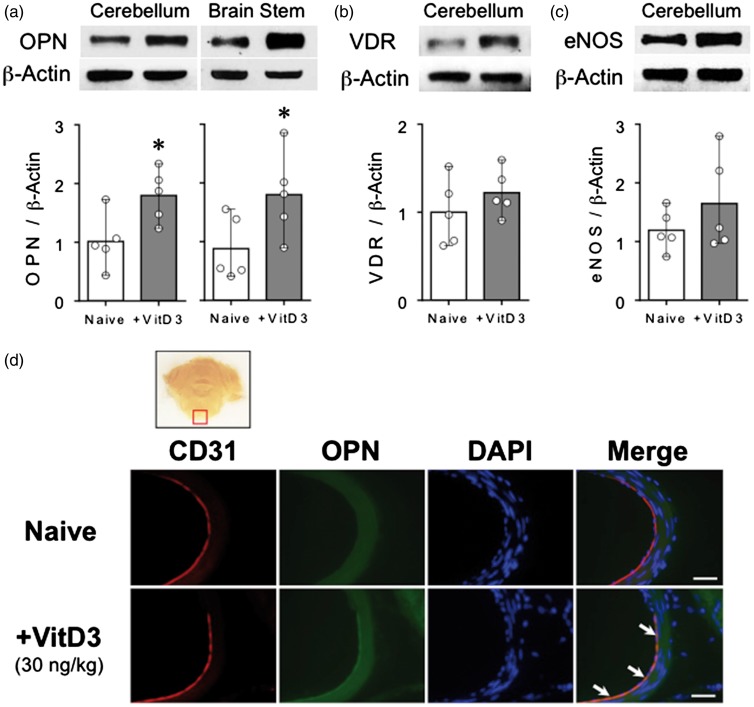
Pretreatment of VitD3 increases endogenous OPN expression in the hindbrain and cerebral arteries
Western blot analysis showed that a single pretreatment of VitD3 (30 ng/kg) significantly increased OPN expression in the cerebellum and brain stem (Figure 1(a)). Additionally, VDR (Figure 1(b)) and eNOS (Figure 1(c)) expression were increased in the cerebellum after 24 h in naïve rats. OPN expression was increased in the arterial layers of the basilar artery including the endothelium after pretreatment with VitD3 (Figure 1(d)).
Figure 1.
A single pretreatment of vitamin D3 (VitD3) upregulates endogenous osteopontin (OPN) in hindbrain and cerebral vascular endothelium. (a) Representative Western blots of VitD3-induced (30 ng/kg) expression of OPN (upper panel) and quantitative analysis (lower panel) 24 h after pretreatment in the cerebellum and brain stem of VitD3 pretreated (+VitD3) and naïve rats. (b) Vitamin D receptor (VDR) and (c) endothelial nitric oxide synthase (eNOS) representative western blots (upper panel) and quantitative analysis (lower panel) after pretreatment in the cerebellum of +VitD3 and naïve rats. *P < 0.05 vs. naïve rats. n = 5 per group. (d) Immunohistochemical staining of OPN (green) and endothelium (CD31, red) of basilar artery. Nuclei are stained with DAPI (blue). Top panel indicates the location of staining (small red box). Arrows indicate colocalization of OPN and CD31. n = 2 per group. Bar = 50 µm.
Mortality and SAH severity
After SAH, blood clots were present around the basal cistern with a significant difference in SAH grade between Sham and SAH animals, but no difference was observed between all SAH groups at 24 h post-ictus as described our previous study.19 Of the 103 total animals used, 75 were subjected to SAH, of which 13 (17%) died within 24 h after SAH induction (Table 1).
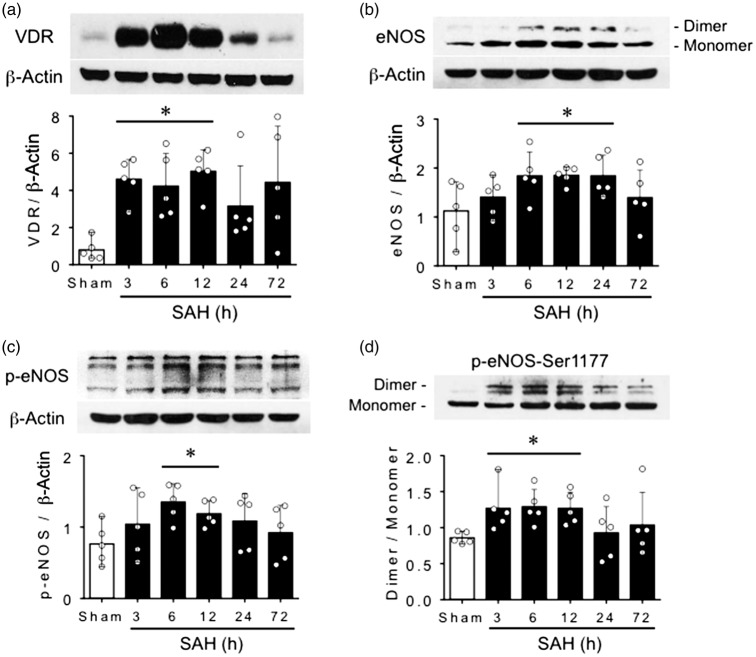
Expression changes of VDR and eNOS in the brain after SAH
Western blot results showed that expression of VDR dramatically increased from 3 to 12 h and declined from 24 h to 72 h in the left hemisphere of the brain after SAH induction (Figure 2(a)). Total expression of eNOS, including monomer and dimer forms, increased significantly at 6, 12 and 24 h and decreased at 72 h (Figure 2(b)). However, total expressions of p-eNOS and ratio of dimer to monomer of the p-eNOS at Ser1177 (p-eNOS-Ser1177) increased significantly at 3, 6 and 12 h and declined at 24 h, specifically the dimer form of p-eNOS-Ser1177 which is the most active form of eNOS (Figure 2(c) and (d)).
Figure 2.
Expression changes of vitamin D receptor (VDR) and endothelial nitric oxide synthase (eNOS) after SAH in the brain. Time dependent changes of representative Western blots (upper panel) and quantitative analysis (lower panel) of VDR (a) in left hemisphere of the brain after SAH induction. Time dependent changes of representative Western blots including monomer and dimer bands (upper panel) and quantitative total analysis (lower panel) of eNOS (b) and phosphorylated eNOS-Ser1177 (p-eNOS-Ser1177) (c–d) in left hemisphere of the brain after SAH induction. *P < 0.05 vs. Sham. n = 5 per group.
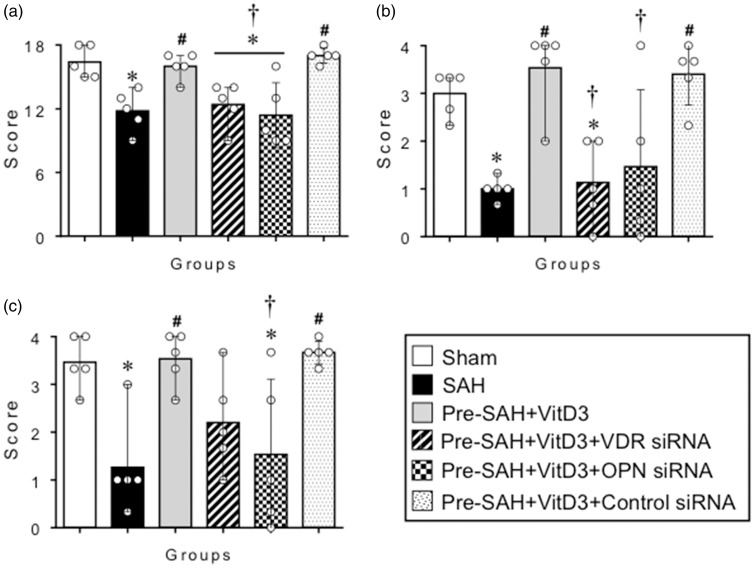
Pretreatment of VitD3 attenuates neurological deficits after SAH
A single pretreatment of 30 ng/kg of VitD3 significantly increased the neurological score on modified Garcia (Figure 3(a)), beam balance (Figure 3(b)) and wire hanging (Figure 3(c)) tests at 24 h in Pre-SAH+VitD3 rats compared with SAH. The preventive effects of Pre-SAH+VitD3 were reversed by siRNAs for VDR and OPN (Figure 3).
Figure 3.
A single pretreatment of vitamin D3 (VitD3) improves neurological deficits after subarachnoid hemorrhage (SAH). A single pretreatment of VitD3 (30 ng/kg) significantly increased the modified Garcia (a), beam balance (b) and wire hanging test (c) scores 24 h in Pre-SAH+VD3 group (n = 5 per group) and reversed by small interfering ribonucleic acid (siRNA) for vitamin D receptor (VDR) and osteopontin (OPN). Pre-SAH+VitD3, pretreatment (30 ng/kg) VitD3 24 h before SAH; *P < 0.05 vs. Sham. #P < 0.05 vs. SAH. †P < 0.05 vs. Pre-SAH + VitD3+Control siRNA.
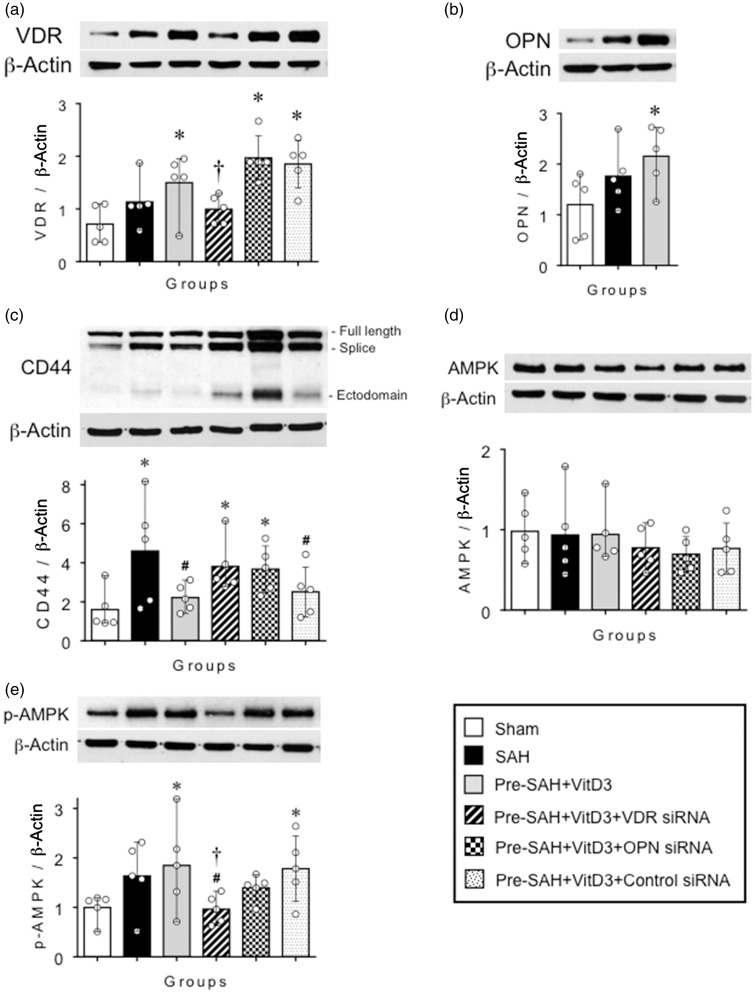
VitD3 upregulates AMPK and eNOS through a VDR dependent mechanism in cerebral arteries
At 24 h after SAH induction, VDR expression was higher in the cerebral arteries of SAH rats compared with Sham group and reached a significantly higher level by VitD3 pretreatment. Moreover, i.c.v injection of siRNA for VDR significantly inhibited VDR expression in the cerebral arteries of Pre-SAH+VitD3+VDR siRNA rats compared with Pre-SAH+VitD3+Control siRNA rats (Figure 4(a)). Expression of OPN in the basilar artery was significantly increased in Pre-SAH+VitD3 rats compared with SAH rats (Figure 4(b)). Total expression of CD44 was significantly higher in the SAH group compared with that of Sham rats and was decreased mainly dependent on degradation of CD44 splice and ectodomain variants in Pre-SAH+VitD3 group. These changes were reversed by intervention of siRNA for both VDR and OPN in the Pre-SAH+VitD3+VDR siRNA and Pre-SAH+VitD3+OPN siRNA rats, respectively, compared with that Pre-SAH+VitD3+Control siRNA rats (Figure 4(c)). Total expression of AMPK did not change significantly among groups (Figure 4(d)). However, the p-AMPK increased in the SAH group (P = 0.097) and it was reached significantly higher in the Pre-SAH+VitD3 group compared with that of the Sham rats and was reversed by VDR siRNA, but not OPN siRNA, these effects compared with that Pre-SAH+VitD3+Control siRNA rats (Figure 4(e)).
Figure 4.
Vitamin D3 (VitD3) upregulates vitamin D receptor (VDR), osteopontin (OPN), decreases CD44 splicing and improves phosphorylation of adenosine monophosphate-activated protein kinase (AMPK) in cerebral arteries after SAH. Representative Western blots (upper panel) and quantitative analysis (lower panel) of VDR (a), OPN (b), CD44 (c), AMPK (d) and phosphorylated AMPK (p-AMPK) (e) in cerebral arteries after SAH induction. Pre-SAH+VitD3, pretreatment (30 ng/kg) VitD3 24 h before SAH induction; siRNA, small interfering ribonucleic acid; *P < 0.05 vs. Sham. †P < 0.05 vs. Pre-SAH + VitD3+Control siRNA. n = 5 per group.
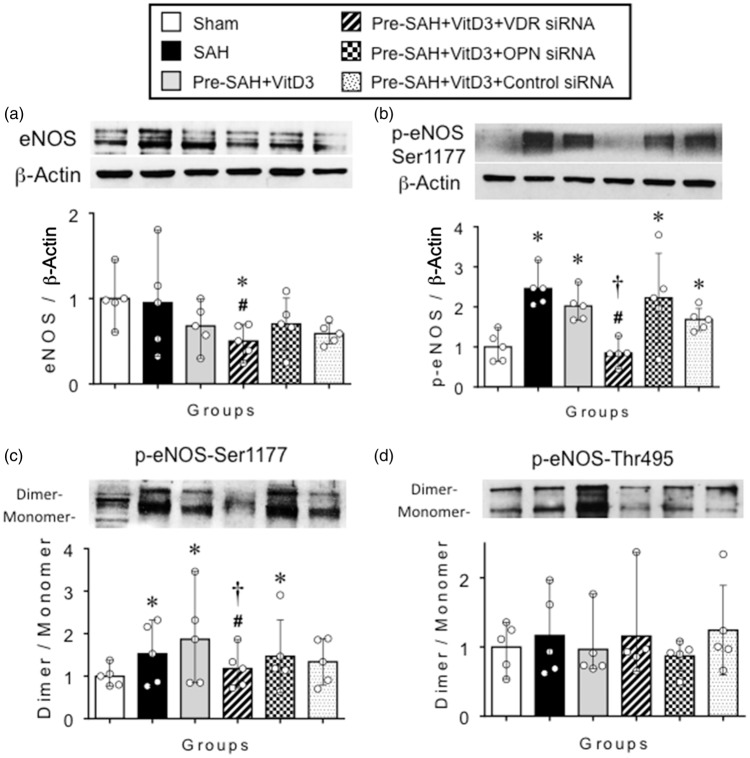
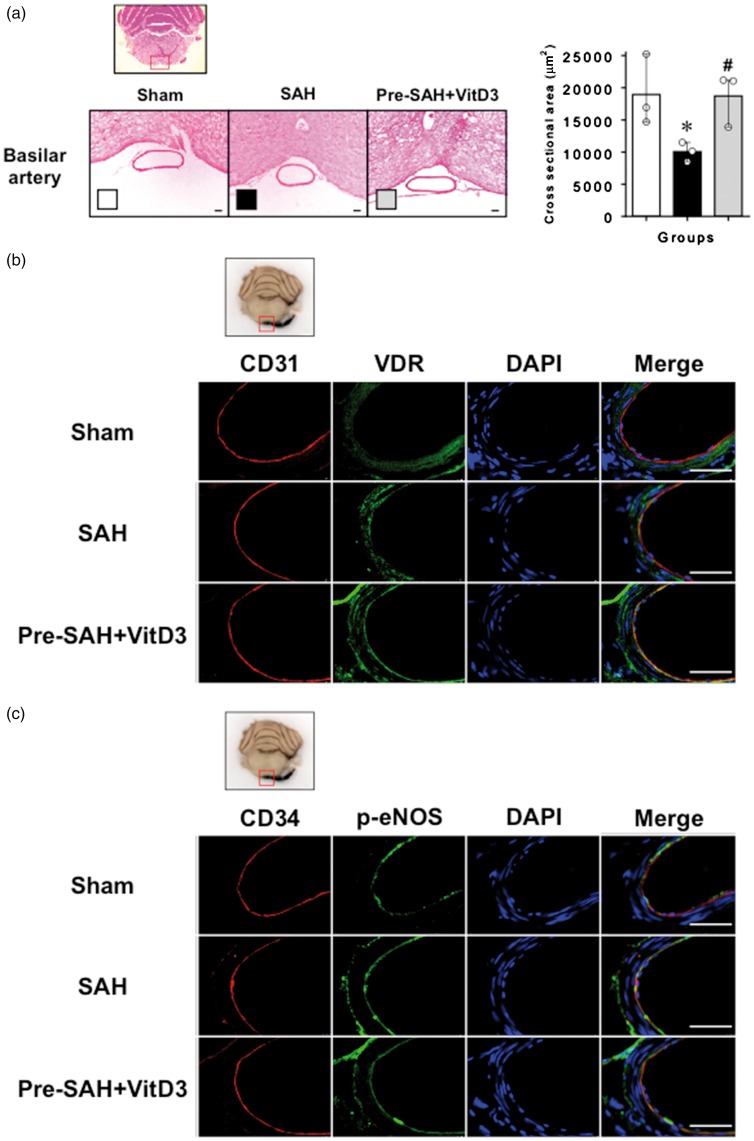
Moreover, total expression of eNOS was significantly lower in Pre-SAH+VitD3+VDR siRNA rats compared with that of the Sham and SAH rats (Figure 5(a)). Moreover, the total and ratio of dimer to monomer p-eNOS-Ser1177 were significantly upregulated and stayed significantly higher in the SAH group as well as in pretreatment SAH groups compared with that of the Sham rats. Compared with Pre-SAH+VitD3+Control siRNA rats, these effects were reversed by VDR siRNA, but not OPN siRNA (Figure 5(b) and (c)). Expression of the p-eNOS-Thr495-Dimer was affected in an inverse manner with the p-eNOS-Ser1177-Dimer changes, but it did not reach significant differences between the groups (Figure 5(d)). Hematoxylin–eosin-stained histology images of the basilar artery between the pons-cerebellum and midbrain showed that the diameter (left panel) and cross-sectional area (right panel) of the basilar artery decreased after SAH compared with Sham rats and was reversed by pretreatment with VitD3 (Figure 6(a)). Immunohistochemistry staining of the basilar artery showed that VDR is highly expressed in the artery layers of Sham rats and was increased in SAH rats as well as Pre-SAH+VitD3 rats (Figure 6(b)). Moreover, p-eNOS, which is primarily expressed in the basilar artery endothelium of Sham rats, was increased in SAH and Pre-SAH+VitD3 rats (Figure 6(c)).
Figure 5.
Vitamin D3 (VitD3) pretreatment regulates Ser1177-Dimer phosphorylation of endothelial nitric oxide synthase (p-eNOS) in cerebral arteries after SAH. Representative Western blots (upper panel) and quantitative analysis (lower panel) of total eNOS (a), total phosphorylated eNOS (p-eNOS-Ser1177) (b), p-eNOS-Ser1177-Dimer/Monomer (c) and p-eNOS-Thr495-Dimer/Monomer (d) in cerebral arteries after SAH induction. Pre-SAH+VitD3, pretreatment (30 ng/kg) VitD3 24 h before SAH induction; VDR, vitamin D receptor; OPN, osteopontin; siRNA, small interfering ribonucleic acid; *P < 0.05 vs. Sham. #P < 0.05 vs. SAH. †P < 0.05 vs. Pre-SAH+VitD3+Control siRNA. n = 5 per group.
Figure 6.
Vitamin D3 (VitD3) pretreatment improves phosphorylated endothelial nitric oxide synthase (p-eNOS) expression in the endothelium of basilar arteries after subarachnoid hemorrhage (SAH). (a) Hematoxylin–eosin-stained basilar artery lumen image (left panel) and quantitative analysis of the cross-sectional area (right panel) at level between midbrain and pons-cerebellum. *P < 0.05 vs. Sham. #P < 0.05 vs. SAH. (b) Immunohistochemistry images of VDR (green) and the endothelium (CD31, red) in the basilar artery. (c) Immunohistochemistry images of p-eNOS (green) at Ser1177 and the endothelium (CD34, red) in the basilar artery. Nuclei are stained with DAPI (blue). Top panel indicates the location of staining (small red box). Pre-SAH+VitD3, pretreatment (30 ng/kg) VitD3 24 h before SAH induction; n = 3 per group; Bar = 50 µm.
Discussion
The novel finding of our present study was that pretreatment with VitD3 upregulates the expression of p-AMPK and the p-eNOS-Ser1177-Dimer in cerebral arteries leading to protection against cerebral artery remodeling and spasm in EBI after SAH in rats. Pretreatment with VitD3 (calcitriol), the most active form of vitamin D improved neurological impairment and attenuated artery remodeling and spasm. VitD3 pretreatment was also associated with upregulation of OPN and eNOS in the hindbrain, and decrease of CD44 splicing and upregulation of p-AMPK-Thr172 and the p-eNOS-Ser1177-Dimer in the cerebral artery within 24 h after SAH. Blockage of VDR and OPN exacerbated neurologic impairment and was associated with a decrease of eNOS and AMPK in the arteries.
The VDR association with both genomic and non-genomic pathways8,9 with a number of vitamin D-induced neuroprotective effects having been studied in neuroscience.27 Interestingly, because stroke is a significant cause of mortality for patients with vitamin D deficiency, prolonged vitamin D therapy could reduce the risk and mortality of stroke.13,16,28 However, a precise mechanism of the effect is still lacking. Studies have shown that long-term vitamin D therapy is protective against ischemic stroke through GDNF and NR3A/CREB pathways in neurons.17,18 Our recent study showed that vitamin D upregulates OPN expression and inhibits blood–brain barrier disruption through an OPN/CD44/P-gp glycosylation mechanism in the endothelial cells of cerebral micro vessels.19 However, the molecular mechanism of vitamin D has not been studied in cerebral arteries after SAH. For the first time, we have demonstrated that pretreatment with VitD3 prevents cerebral artery remodeling and spasm after SAH in rats and that the molecular mechanism of VitD3 was associated with upregulation of OPN and VDR-dependent AMPK and eNOS phosphorylation in cerebral arteries.
OPN is an extracellular glycoprotein associated with neuroprotection29,30 and can be upregulated by vitamin D in vitro and in vivo.31–33 Our previous studies have shown that recombinant OPN treatment attenuates neuronal apoptosis through the FAK/PI3K/Akt pathway after SAH in rats.34 The integrin receptor-dependent effects of OPN protect against vasospasm and BBB disruption after SAH through the activation of MKP-1 and MAPK phosphatase in VSMC, astrocytes and endothelial cells.20,35 Our studies have also shown that OPN preserves the cerebral artery phenotype through Rac-1 in VSMC.21 Studies from other labs have shown that OPN protects against ischemic brain injury via Akt/p42/p44/MAPK phosphorylation and GDNF upregulation.18,29 In our present study, the mechanism for upregulation and activation of eNOS in cerebral artery endothelium is involved mostly with VDR-dependent pathways. However, the beneficial effect of pretreatment with VitD3 could also be involved in ways alternative to cerebral OPN upregulation and decrease of CD44 splicing, as reported in our previous studies.19–21,34,35
AMPK is a multisubstrate serine/threonine protein kinase involved in a number of downstream pathways is ubiquitously expressed in all human tissues.36,37 AMPK consists of a catalytic subunit α, and two regulatory subunits β and γ,36 that are differentially expressed in various tissues and subcellular locations.38 Previous studies have demonstrated that the predominant isoform expressed in vascular endothelial cells is α1.39,40 Interestingly, AMPK is the only kinase that can phosphorylate eNOS on multiple sites including Ser1177 as well as activating sites in the reductase domain and the Thr495 residue located in the inhibitory site of the calmodulin-binding domain. Endothelial AMPK is one of the main regulators of NO-dependent and -independent relaxation in arteries of mice which are different in conduit and resistance arteries, respectively.26 Current study results have shown that pretreatment with vitamin D improves AMPKα-Thr172 phosphorylation in the cerebral artery through a VDR-dependent pathway and supports eNOS-Ser1177-Dimer phosphorylation and the p-eNOS-Thr495-Dimer dephosphorylation after SAH. Osuka et al.25 have shown that p-eNOS-Ser1177 and p-AMPKα-Thr172 increased significantly in endothelial cells of the basilar artery 24 h after SAH induction in rats and was consistent with our results. Moreover, our current results showed that vitamin D improves the phosphorylation and dimerization of potential factors against eNOS dysfunction after SAH.
eNOS is a well-known member of NOS enzyme family and is highly expressed in the endothelium. The functional ability of NOS to release NO is dependent on phosphorylation (i.e p-NOS). NO, a potent vasorelaxant, is an essential factor in the endothelium that relaxes underlying VSMC. Vitamin D has been shown to upregulate eNOS through a VDR-dependent pathway in the aorta of VDR mutant mice,41 normalizes NO production in the renal artery of estrogen-deficient rats,42 and improves the dimer to monomer ratio of total eNOS in the femoral artery of diabetic rats.43 The dimerization of eNOS indicates activity of the enzyme in endothelial cells.44 However, most studies have focused on the expressional changes of total eNOS after SAH, but not on the regulatory mechanism of eNOS dimerization in the cerebral artery after SAH. Previous studies showed that total eNOS expression is significantly decreased at 3, 6 and 12 h in the brain cortex,45 increases within 24 h46 then decreases again at 48 h in the full ipsilateral hemisphere47 which is consistent with present results. Present results showed that VitD3 pretreatment increased phosphorylated eNOS in the cerebral artery after SAH through VDR-dependent signaling of the eNOS dimerization ratio in the endothelium. Because the primary role of eNOS is to dilate vessels via NO and hyperpolarization,26 understanding the role of eNOS in cerebral artery resistance48 is an important issue for effective stroke treatment. The activity of NOS having phasic changes in the brain after SAH with each subtype having different effects on specific cell types, helps to explain these findings. To this end, the current results shed new light on the role of vitamin D in stimulating the dimer phosphorylation ratio of p-eNOS-Ser1177 through VDR and AMPK-dependent pathways. Our results also provide a functional link between eNOS activity and cerebral artery circulation after SAH. The precise signaling mechanism of vitamin D, regarding the role of p-AMPK in the eNOS dimer/monomer modification and role of OPN in the endothelium of brain resistance arteries after stroke remains to be elucidated in further studies.
Vitamin D deficiency is strongly correlated with incidences of cancer, diabetes, and cardiovascular diseases13–15 as well as stroke.16 Moreover, the incidence of SAH is highly prevalent in non-Caucasian populations,49 of which a worse prognosis is remarkably increased during winter months.50 Based on this and the vitamin D regulatory mechanism of AMPK and eNOS, it suggests that vitamin D is critical to reducing both SAH sequelae and the occurrence of SAH. For the first time, the beneficial effect of VitD3 was shown to be involved in an increased dimerization ratio of p-eNOS in the endothelium of the cerebral artery and upregulation of VDR and p-AMPK in endothelial cells, thereby attenuating cerebral artery spasm in EBI after SAH. Our previous study confirmed that vitamin D upregulates endogenous OPN expression in brain hemispheres of an in vivo model of SAH.19 Our current results also demonstrated that pretreatment with VitD3 leads to increased expression of endogenous OPN in the cerebellum and brain stem, specifically in cerebral artery endothelium. Thus, pretreatment with vitamin D would be an inexpensive and easy safe way to upregulate eNOS and OPN-dependent protective factors in the cerebral arteries in SAH patients.
In conclusion, we demonstrated that pretreatment with VitD3 attenuated cerebral artery remodeling and spasm in EBI after SAH in rats through a VDR-dependent OPN upregulation in the cerebral artery and AMPK/eNOS-Ser1177-Dimer phosphorylation mechanism in endothelial cells. Vitamin D may be a useful new preventive and therapeutic strategy against cerebral artery remodeling in stroke patients via upregulation of OPN and manipulation of eNOS.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was partially supported by grants NS081740 and NS082184 from the National Institutes of Health to J.H.Z.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ contributions
For this paper, the conception and design were made by BE, JT, and JHZ. Drafting the article was done by BE and JM. BE and WMH performed most of the experiments. WJ, WW and GW conducted experiments. Manuscript reviews and revisions were made by all authors. Approval of the final manuscript was made by JHZ.
References
- 1.Linn FH, Rinkel GJ, Algra A, et al. Incidence of subarachnoid hemorrhage: role of region, year, and rate of computed tomography: a meta-analysis. Stroke 1996; 27: 625–629. [DOI] [PubMed] [Google Scholar]
- 2.van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid haemorrhage. Lancet 2007; 369: 306–318. [DOI] [PubMed] [Google Scholar]
- 3.Athar MK, Levine JM. Treatment options for cerebral vasospasm in aneurysmal subarachnoid hemorrhage. Neurotherapeutics 2012; 9: 37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Velat GJ, Kimball MM, Mocco JD, et al. Vasospasm after aneurysmal subarachnoid hemorrhage: review of randomized controlled trials and meta-analyses in the literature. World Neurosurg 2011; 76: 446–454. [DOI] [PubMed] [Google Scholar]
- 5.Ingall T, Asplund K, Mahonen M, et al. A multinational comparison of subarachnoid hemorrhage epidemiology in the who monica stroke study. Stroke 2000; 31: 1054–1061. [DOI] [PubMed] [Google Scholar]
- 6.Schievink WI, Riedinger M, Jhutty TK, et al. Racial disparities in subarachnoid hemorrhage mortality: Los Angeles County, California, 1985-1998. Neuroepidemiology 2004; 23: 299–305. [DOI] [PubMed] [Google Scholar]
- 7.Cahill J, Zhang JH. Subarachnoid hemorrhage: is it time for a new direction? Stroke 2009; 40: S86–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harms LR, Burne TH, Eyles DW, et al. Vitamin d and the brain. Best Pract Res Clin Endocrinol Metab 2011; 25: 657–669. [DOI] [PubMed] [Google Scholar]
- 9.Haussler MR, Whitfield GK, Kaneko I, et al. Molecular mechanisms of vitamin d action. Calcif Tissue Int 2013; 92: 77–98. [DOI] [PubMed] [Google Scholar]
- 10.Molinari C, Uberti F, Grossini E, et al. 1alpha,25-dihydroxycholecalciferol induces nitric oxide production in cultured endothelial cells. Cell Physiol Biochem 2011; 27: 661–668. [DOI] [PubMed] [Google Scholar]
- 11.Ni W, Watts SW, Ng M, et al. Elimination of vitamin d receptor in vascular endothelial cells alters vascular function. Hypertension 2014; 64: 1290–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodnar LM, Catov JM, Simhan HN, et al. Maternal vitamin d deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab 2007; 92: 3517–3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daubail B, Jacquin A, Guilland JC, et al. Association between serum concentration of vitamin d and 1-year mortality in stroke patients. Cerebrovasc Dis 2014; 37: 364–367. [DOI] [PubMed] [Google Scholar]
- 14.Teng M, Wolf M, Lowrie E, et al. Survival of patients undergoing hemodialysis with paricalcitol or calcitriol therapy. N Engl J Med 2003; 349: 446–456. [DOI] [PubMed] [Google Scholar]
- 15.Tunon J, Cristobal C, Tarin N, et al. Coexistence of low vitamin d and high fibroblast growth factor-23 plasma levels predicts an adverse outcome in patients with coronary artery disease. PloS One 2014; 9: e95402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pilz S, Tomaschitz A, Drechsler C, et al. Vitamin d supplementation: a promising approach for the prevention and treatment of strokes. Curr Drug Targets 2011; 12: 88–96. [DOI] [PubMed] [Google Scholar]
- 17.Fu J, Xue R, Gu J, et al. Neuroprotective effect of calcitriol on ischemic/reperfusion injury through the nr3a/creb pathways in the rat hippocampus. Mol Med Rep 2013; 8: 1708–1714. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Chiang YH, Su TP, et al. Vitamin d(3) attenuates cortical infarction induced by middle cerebral arterial ligation in rats. Neuropharmacology 2000; 39: 873–880. [DOI] [PubMed] [Google Scholar]
- 19.Enkhjargal B, McBride DW, Manaenko A, et al. Intranasal administration of vitamin d attenuates blood-brain barrier disruption through endogenous upregulation of osteopontin and activation of cd44/p-gp glycosylation signaling after subarachnoid hemorrhage in rats. J CerebBlood Flow Metab 2017; 37: 2555–2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suzuki H, Hasegawa Y, Chen W, Kanamaru K, Zhang JH. Recombinant osteopontin in cerebral vasospasm after subarachnoid hemorrhage. Ann Neurol 2010; 68: 650–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu J, Zhang Y, Yang P, et al. Recombinant osteopontin stabilizes smooth muscle cell phenotype via integrin receptor/integrin-linked kinase/rac-1 pathway after subarachnoid hemorrhage in rats. Stroke 2016; 47: 1319–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bederson JB, Germano IM, Guarino L. Cortical blood flow and cerebral perfusion pressure in a new noncraniotomy model of subarachnoid hemorrhage in the rat. Stroke 1995; 26: 1086–1091. discussion 1091–1082. [DOI] [PubMed] [Google Scholar]
- 23.Garcia JH, Wagner S, Liu KF, et al. Neurological deficit and extent of neuronal necrosis attributable to middle cerebral artery occlusion in rats. Statistical validation. Stroke 1995; 26: 627–634. discussion 635. [DOI] [PubMed] [Google Scholar]
- 24.Sugawara T, Ayer R, Jadhav V, et al. A new grading system evaluating bleeding scale in filament perforation subarachnoid hemorrhage rat model. J Neurosci Methods 2008; 167: 327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osuka K, Watanabe Y, Usuda N, et al. Modification of endothelial nitric oxide synthase through ampk after experimental subarachnoid hemorrhage. J Neurotrauma 2009; 26: 1157–1165. [DOI] [PubMed] [Google Scholar]
- 26.Enkhjargal B, Godo S, Sawada A, et al. Endothelial amp-activated protein kinase regulates blood pressure and coronary flow responses through hyperpolarization mechanism in mice. Arterioscler Thromb Vasc Biol 2014; 34: 1505–1513. [DOI] [PubMed] [Google Scholar]
- 27.Garcion E, Wion-Barbot N, Montero-Menei CN, et al. New clues about vitamin d functions in the nervous system. Trends Endocrinol Metab 2002; 13: 100–105. [DOI] [PubMed] [Google Scholar]
- 28.Brewer LC, Michos ED, Reis JP. Vitamin d in atherosclerosis, vascular disease, and endothelial function. Curr Drug Targets 2011; 12: 54–60. [DOI] [PubMed] [Google Scholar]
- 29.Meller R, Stevens SL, Minami M, et al. Neuroprotection by osteopontin in stroke. J Cereb Blood Flow Metab 2005; 25: 217–225. [DOI] [PubMed] [Google Scholar]
- 30.Schroeter M, Zickler P, Denhardt DT, et al. Increased thalamic neurodegeneration following ischaemic cortical stroke in osteopontin-deficient mice. Brain 2006; 129: 1426–1437. [DOI] [PubMed] [Google Scholar]
- 31.Chang PL, Ridall AL, Prince CW. Calcitriol regulation of osteopontin expression in mouse epidermal cells. Endocrinology 1994; 135: 863–869. [DOI] [PubMed] [Google Scholar]
- 32.Lau WL, Leaf EM, Hu MC, et al. Vitamin d receptor agonists increase klotho and osteopontin while decreasing aortic calcification in mice with chronic kidney disease fed a high phosphate diet. Kidney Int 2012; 82: 1261–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noda M, Vogel RL, Craig AM, et al. Identification of a DNA sequence responsible for binding of the 1,25-dihydroxyvitamin d3 receptor and 1,25-dihydroxyvitamin d3 enhancement of mouse secreted phosphoprotein 1 (spp-1 or osteopontin) gene expression. Proc Natl Acad Sci USA 1990; 87: 9995–9999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Topkoru BC, Altay O, Duris K, et al. Nasal administration of recombinant osteopontin attenuates early brain injury after subarachnoid hemorrhage. Stroke 2013; 44: 3189–3194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Suzuki H, Hasegawa Y, Kanamaru K, et al. Mechanisms of osteopontin-induced stabilization of blood-brain barrier disruption after subarachnoid hemorrhage in rats. Stroke 2010; 41: 1783–1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kahn BB, Alquier T, Carling D, et al. Amp-activated protein kinase: ancient energy gauge provides clues to modern understanding of metabolism. Cell Metab 2005; 1: 15–25. [DOI] [PubMed] [Google Scholar]
- 37.Lamia KA, Sachdeva UM, DiTacchio L, et al. Ampk regulates the circadian clock by cryptochrome phosphorylation and degradation. Science 2009; 326: 437–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ewart MA, Kennedy S. Ampk and vasculoprotection. Pharmacol Ther 2011; 131: 242–253. [DOI] [PubMed] [Google Scholar]
- 39.Davis BJ, Xie Z, Viollet B, et al. Activation of the amp-activated kinase by antidiabetes drug metformin stimulates nitric oxide synthesis in vivo by promoting the association of heat shock protein 90 and endothelial nitric oxide synthase. Diabetes 2006; 55: 496–505. [DOI] [PubMed] [Google Scholar]
- 40.Zou MH, Kirkpatrick SS, Davis BJ, Nelson JS, Wiles WGt, Schlattner U, Neumann D, Brownlee M, Freeman MB, Goldman MH. Activation of the amp-activated protein kinase by the anti-diabetic drug metformin in vivo. Role of mitochondrial reactive nitrogen species. J Biol Chem 2004; 279: 43940–43951. [DOI] [PubMed] [Google Scholar]
- 41.Andrukhova O, Slavic S, Zeitz U, et al. Vitamin d is a regulator of endothelial nitric oxide synthase and arterial stiffness in mice. Mol Endocrinol 2014; 28: 53–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dong J, Wong SL, Lau CW, et al. Calcitriol restores renovascular function in estrogen-deficient rats through downregulation of cyclooxygenase-2 and the thromboxane-prostanoid receptor. Kidney Int 2013; 84: 54–63. [DOI] [PubMed] [Google Scholar]
- 43.Hirata M, Serizawa K, Aizawa K, et al. 22-oxacalcitriol prevents progression of endothelial dysfunction through antioxidative effects in rats with type 2 diabetes and early-stage nephropathy. Nephrol Dial Transplant 2013; 28: 1166–1174. [DOI] [PubMed] [Google Scholar]
- 44.Chen W, Xiao H, Rizzo AN, et al. Endothelial nitric oxide synthase dimerization is regulated by heat shock protein 90 rather than by phosphorylation. PloS One 2014; 9: e105479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li Q, Chen Y, Li B, et al. Hemoglobin induced no/cgmp suppression deteriorate microcirculation via pericyte phenotype transformation after subarachnoid hemorrhage in rats. Sci Rep 2016; 6: 22070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sugawara T, Ayer R, Jadhav V, et al. Simvastatin attenuation of cerebral vasospasm after subarachnoid hemorrhage in rats via increased phosphorylation of akt and endothelial nitric oxide synthase. J Neurosci Res 2008; 86: 3635–3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li Q, Chen Y, Zhang X, et al. Scutellarin attenuates vasospasm through the erk5-klf2-enos pathway after subarachnoid hemorrhage in rats. J Clin Neurosci 2016; 34: 264–270. [DOI] [PubMed] [Google Scholar]
- 48.Enkhjargal B, Hashimoto M, Sakai Y, et al. Characterization of vasoconstrictor-induced relaxation in the cerebral basilar artery. Euro J Pharmacol 2010; 637: 118–123. [DOI] [PubMed] [Google Scholar]
- 49.Ayala C, Greenlund KJ, Croft JB, et al. Racial/ethnic disparities in mortality by stroke subtype in the united states, 1995-1998. Am J Epidemiol 2001; 154: 1057–1063. [DOI] [PubMed] [Google Scholar]
- 50.de Steenhuijsen Piters WA, Algra A, van den Broek MF, et al. Seasonal and meteorological determinants of aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Neurol 2013; 260: 614–619. [DOI] [PubMed] [Google Scholar]