Abstract
The present study investigated the expression and potential influence of SHC SH2 domain-binding protein 1 (SHCBP1) in gastric cancer (GC) cells. SHCBP1 is closely related to cell proliferation and cell cycle progression, but its role in GC remains unclear. The TCGA database revealed that SHCBP1 is highly expressed in GC tissues. Furthermore, SHCBP1 was revealed to be highly expressed in GC cell lines MGC-803 and SGC-7901 cells, and downregulation of SHCBP1 significantly inhibited GC cell proliferation. Furthermore, SHCBP1 expression promoted cell cycle progression and inhibition of apoptosis. Since the CDK4, cyclin D1 and caspase family proteins play important roles in cell cycle and apoptosis regulation, it was examined whether there was an association between SHCBP1 and these signaling pathways in GC. Our results revealed that SHCBP1 promoted cell cycle progression by regulating the CDK4-cyclin D1 cascade and suppressed caspase-3, caspase PARP-dependent apoptotic pathways. Cell invasion and metastasis experiments also revealed that SHCBP1 promoted tumor growth and invasiveness. These tumor-promoting functions of SHCBP1 may provide a potential molecular basis for the diagnosis and targeted therapy of GC.
Keywords: SHCBP1, gastric cancer, cell cycle, proliferation, metastasis
Introduction
Gastric cancer (GC) is the most common malignant tumor of the digestive system, and its incidence is ranked fourth and its mortality is ranked third among malignant tumors (1). Most patients are at an advanced stage when they are diagnosed with GC. Chemotherapy is the main treatment for patients with advanced GC, however, although it can prolong the overall survival, the adverse reactions are more prominent (2). The liver is the main target organ of GC metastasis. Shitara et al compiled 12,656 patients with advanced GC, of which the incidence of liver metastasis was as high as 44% (3). Patients who developed liver metastases from GC had limited resection and the treatment was more difficult. GC patients with liver metastases have a 5-year survival rate of only ~10% (4). With the in-depth study of the molecular mechanism of the occurrence and development of GC, molecular targeted therapy of GC has gradually emerged. Therefore, it is urgent to understand the mechanisms involved in the metastasis of GC, taking effective measures for early diagnosis and targeted therapy for GC to improve their survival and life quality.
SHC encodes three sub-subunits, including p46Shc, p52Shc, and p66Shc, each of which has a carboxy-terminal Src homology domain (SH2), a phospho-serine-binding domain (PTB) with a free α-amino group, and a central proline-rich collagen-homologous region (CH1), however, p66shc contains an amino terminal region (CH2) (5,6). p46Shc and p52Shc are ubiquitous in various cells, including cancer cells, such as breast and endometrial cancer, however the amount of p66shc expression varies depending on the cell type (7). Tyrosine phosphorylation kinase receptors such as the growth factor receptors EGFR, FGFR, erbB-2 and other tyrosine phosphorylation of the intracellular domain recognize and bind to proteins in the corresponding SH2 region of the cytoplasm, with the extracellular signals passed down step by step (8).
SHC SH2 domain-binding protein 1 (SHCBP1) is an important connexin on the SH2 domain of the SHC protein, and its functional role has not been clearly established (9). The mRNA and protein of the SHCBP1 gene are expressed in proliferating cells, such as stem cells, lymphocytes and cancer cells, but are not expressed in stable cells or permanent cells, such as skeletal muscle and cardiomyocytes (10,11). SHCBP1 is an important intracellular signaling pathway protein, which has been demonstrated to mediate multiple signaling pathways such as RAS and PI3K/AKT and has a role in regulating the cell cycle and promoting cell migration and invasion (10,12). However, the exact role of SHCBP1 in GC remains unclear.
In the present study, we attempted to reveal the role of SHCBP1 in GC and its possible mechanism. SHCBP1 was revealed to be overexpressed in GC tissues compared with adjacent normal tissues from TCGA database. Downregulation of SHCBP1 inhibited proliferation and invasion and promoted apoptosis in vitro. In addition, SHCBP1 knockdown decreased the expression levels of cyclin D1 and CDK4. Hence, our study revealed that SHCBP1 may play a role in cell growth and metastasis and may be a potential diagnosis biomarker and therapeutic target for GC.
Materials and methods
Materials and reagents
MGC-803 and SGC-7901 cell lines were purchased from the American Type Culture Collection (ATCC; Manassas, VA, USA) and cultured in Dulbecco's modified Eagle's medium (DMEM) containing 10% fetal bovine serum (FBS; both from Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA). Antibodies against cleaved PARP (dilution 1:1,000; cat. no. 5625), Bax (dilution 1:1,000; cat. no. 14796), Bcl-2 (dilution 1:1,000; cat. no. 3498), CDK4 (dilution 1:1,000; cat. no. 12790), cyclin D1 (dilution 1:1,000; cat. no. 2978) and cleaved-caspase-3 (dilution 1:500; cat. no. 9664) were all purchased from Cell Signaling Technology, Inc. (Danvers, MA, USA) and SHCBP1 (dilution 1:1,000; cat. no. ab184467) and GAPDH (dilution 1:5,000; cat. no. ab181602) were purchased from Abcam (Cambridge, MA, USA).
shRNA and RT-PCR
The shRNA sequence of SHCBP1 was: CCGGCGAGGAAGTAAGGAAGGGAATCTCGAGATTCCCTTCCACTTCTCCGTTTTTG. Total RNA was reversed to the first strand of cDNA with PrimeScript Reverse Transcriptase (cat. no. RR047A; Takara Biotechnology Co., Ltd., Dalian, China). RT-PCR was performed using a SYBR Premix Ex Taq II kit (RR420A; Takara Biotechnology Co., Ltd.) and detected by StepOnePlus (Applied Biosystems; Thermo Fisher Scientific, Inc.) using the following conditions: 95°C for 30 sec, followed by 40 cycles of 95°C for 5 sec and 60°C for 30 sec. The data were analyzed using the ∆∆Cq method (13) with GAPDH as an internal control. The SHCBP1 PCR primers were as follows: forward, 5′-GCTACCGTGATAAACCAGGTTC-3′ and reverse, 5′-AGGCTCTGAATCGCTCATAGA-3′.
Stable cell line construction
The target shRNA sequence to SHCBP1 and the negative control RNA sequence were synthesized and inserted into the lentivirus core vector expressing a GFP reporter and puromycin resistance. Recombinant lentiviruses were provided by Shanghai GeneChem Co., Ltd. (Shanghai, China). Cells were infected with the corresponding lentivirus, and after 72 h, cells were selected with puromycin (1 µg/ml) for 7 days. The expression level of SHCBP1 in the selected cells was confirmed by qRT-PCR analysis and western blot assays.
Western blotting
After cells expressing SHCBP1-shRNA (sh-SHCBP1) and the control group were lysed by RIPA lysate (Beyotime Institute of Biotechnology, Shanghai, China) and the protein concentration was determined using BCA kit (Beyotime Institute of Biotechnology), protein samples (40 µg/lane) were separated on SDS-PAGE gel (10%) and transferred to polyvinylidene difluoride (PVDF) membranes. After blocking with 5% milk for 1 h at room temperature, the membranes were incubated with a primary antibody overnight at 4°C, washed three times with TBST, and incubated with HRP-fused secondary antibody (dilution 1:5,000; cat. no. ab6721; Abcam, Cambridge, UK) for 1 h. The bands were displayed by ECL illumination (EMD Millipore, Billerica, MA, USA). The experiment was repeated three times.
Cell proliferation detection
Cell proliferation was assessed by Cell Counting Kit-8 (CCK-8) kit (cat. no. CK04; Dojindo Molecular Technologies, Inc., Kumamoto, Japan). Cells (104/100 µl)/well were cultured in 96-well plates for 24–72 h. CCK-8 solution (10 µl) was added to each well, and then the number of cells was assessed using a 450-nm absorbance on a microplate reader. Three independent experiments were performed.
Colony formation
Cells were trypsinized into single cell suspension and seeded in 6-well plates at a density of 800 cells/well. After 14 days of culture, the cells were fixed with a 4% formaldehyde solution for 30 min, stained with 0.1% crystal violet solution, rinsed with tap water and dried in air and photographed under a light microscope (Leica Microsystems, Wetzlar, Germany). Quantitative analysis was performed by counting the number of colonies stained in each well. Three independent experiments were performed.
Cell cycle
The cell cycle assay kit (cat. no. C1052) was purchased from Beyotime Institute of Biotechnology (Haimen, China). The cells were fixed with 70% ethanol at 4°C for 24 h, and then resuspended in cold phosphate-buffered saline (PBS). Then, the cells were resuspended with a staining solution containing RNase A and propidium iodide (PI), and the DNA content was assessed using a flow cytometer. The number of cells in the different phases was counted using ModFit version 3.2 (Verity Software House, Topsham, ME, USA). Three independent experiments were performed.
Cell apoptosis
The apoptosis assay kit (cat. no. C1062) was purchased from Beyotime Institute of Biotechnology. Cells were double stained with Annexin V and PI according to the manufacturer's instructions. The stained cells were analyzed by flow cytometry and the data were analyzed using FlowJo version 10.5.3 (FlowJo LLC, Ashland, OR, USA) software. Three independent experiments were performed.
Cell invasion and metastasis
The wound healing experiment was to inoculate treated GC cells in a 6-well culture plate and grow to a density of >90%. After 12 h, the wound was created by the tip and the image of moved cells was captured after 48 h. In the cell invasion assay, cells were placed in Transwell, 600 µl complete DMEM was added to the lower chamber, and cells mixed with serum-free DMEM were added to the upper chamber. After 24 h of culture, the cells that migrated to the lower chamber were fixed with 4% paraformaldehyde and stained with 0.1% crystal violet. Three independent experiments were performed.
Differential expression analysis of SHCBP1 using UALCAN
Based on The Cancer Genome Atlas (TCGA; http://cancergenome.nih.gov/), level 3 RNA-seq and clinical data from stomach adenocarcinomas, the expression data of SHCBP1 in GC and normal samples were retrieved and analyzed using the online web portal UALCAN (http://ualcan.path.uab.edu).
Statistical analysis
Data analysis and statistics were performed by SPSS 17.0 software (SPSS, Inc., Chicago, IL, USA). T-tests and one-way analysis of variance (ANOVA) followed by the Fishers' least significant difference test (LSD) were used to determine differences between groups. A P-value <0.05 was considered to indicate a statistically significant result.
Results
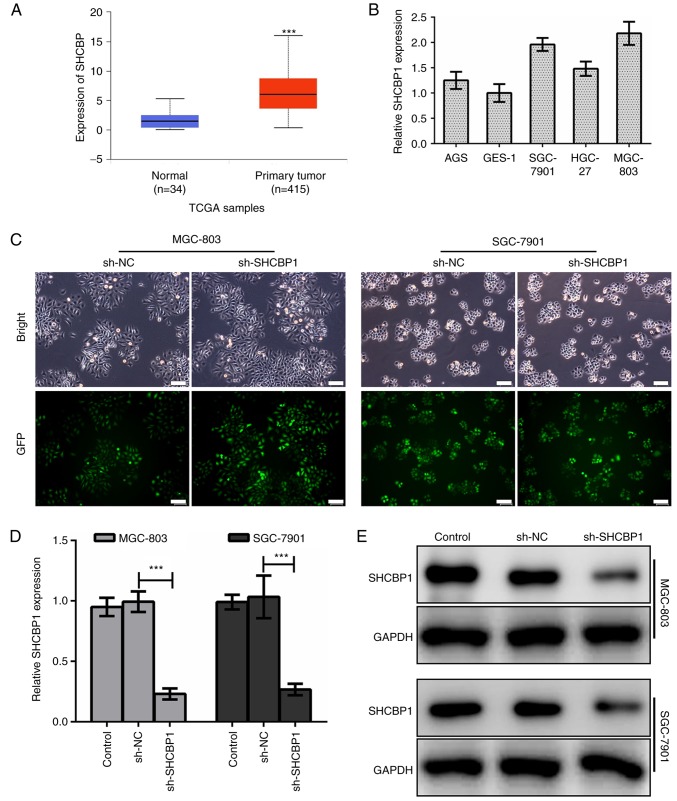
High expression of SHCBP1 in GC tissues and cell lines
The results in TCGA database (https://cancergenome.nih.gov/) confirmed that the expression of SHCBP1 in GC tissues was significantly higher than that in normal tissues (Fig. 1A). In various GC cell lines, we found that the expression of SHCBP1 was higher in MGC-803 and SGC-7901 cells (Fig. 1B), thus, these two cell lines were used as research models. First, we established a human GC cell line model with stable SHCBP1 knockdown. We constructed a green fluorescent protein (GFP) fusion expression vector of negative control-shRNA (sh-NC) and SHCBP1-shRNA (sh-SHCBP1), and introduced shRNA into human GC cell lines MGC-803 and SGC-7901 by lentiviral transfection (Fig. 1C). By RT-PCR, we examined the knockdown efficiency of SHCBP1 mRNA in the MGC-803 and SGC-7901 cell lines expressing sh-SHCBP1 (Fig. 1D). Western blotting was used to detect the expression of SHCBP1 protein in MGC-803 and SGC-7901 cells expressing sh-SHCBP1 (Fig. 1E). The results revealed that the expression of SHCBP1 was successfully knocked down in the GC cell lines MGC-803 and SGC-7901.
Figure 1.
SHCBP1 was effectively knocked down in MGC-803 and SGC-7901 cells. (A) Differences in the expression of SHCBP1 in GC and normal tissues from the TCGA database using the online web portal UALCAN (http://ualcan.path.uab.edu). ***P<0.001. (B) Differential expression of SHCBP1 mRNA in several GC cell lines. (C) MGC-803 and SGC-7901 cells transfected with GFP-fused negative control lentivirus (NC) and SHCBP1 knockdown lentivirus (sh-SHCBP1) were photographed under a fluorescence microscope at a magnification of ×100. (D) RT-PCR detection revealed SHCBP1 knockdown efficiency. ***P<0.001. (E) Western blot analysis revealed SHCBP1 protein expression after transfection of sh-NC and sh-SHCBP1 lentivirus. SHCBP1, SHC SH2 domain-binding protein 1; GC, gastric cancer; sh-NC, negative control-shRNA; sh-SHCBP1, SHCBP1-shRNA.
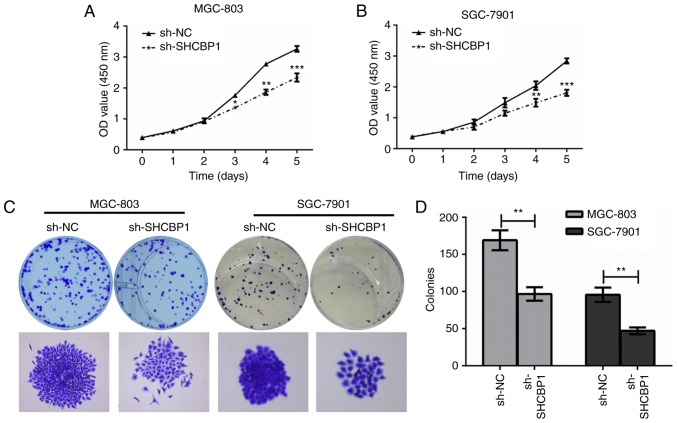
High expression of SHCBP1 promotes proliferation of GC cells
Next, the effect of SHCBP1 on the proliferation of GC cells was examined. MGC-803 and SGC-7901 cells expressing sh-NC and sh-SHCBP1 were cultured in 96-well plates, and cell proliferation was assessed by CCK-8 assay. It was found that GC cells expressing sh-SHCBP1 significantly inhibited cell proliferation (Fig. 2A and B). Cell colony assays of MGC-803 and SGC-7901 cells expressing control, sh-NC and sh-SHCBP1 were determined (Fig. 2C), and the number of colonies formed in each group was counted (Fig. 2D). The results revealed that the proliferation of MGC-803 and SGC-7901 cells by shHCBP1 knockdown was significantly inhibited, thus, SHCBP1 promoted the proliferation of GC cells.
Figure 2.
SHCBP1 promotes proliferation of GC cells. (A and B) The CCK-8 assays revealed cell proliferation of sh-NC and sh-SHCBP1 in MGC-803 and SGC-7901 cells. *P<0.05, **P<0.01, ***P<0.001. (C) Colony formation assays revealed the proliferation effect of sh-SHCBP1 compared to sh-NC in MGC-803 and SGC-7901 cells. (D) The number of colonies in C were analyzed. SHCBP1, SHC SH2 domain-binding protein 1; GC, gastric cancer; CCK-8, Cell Counting Kit-8; sh-SHCBP1, sh-NC, negative control-shRNA; SHCBP1-shRNA.
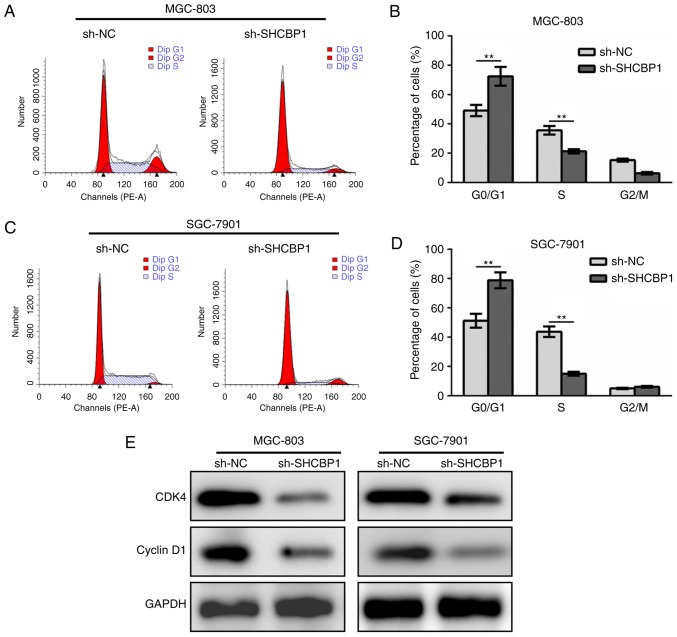
SHCBP1 promotes cell cycle progression of GC cells via CDK4-cyclin D1 cascade
The GC cell lines MGC-803 (Fig. 3A and B) and SGC-7901 (Fig. 3C and D) expressing sh-NC and sh-SHCBP1 were stained with PI, followed by cell cycle analysis by flow cytometry. After SHCBP1 knockdown, the proportion of cells in the G1 phase in the cell cycle increased while the cells in the S phase decreased significantly, while the G2/M phase was not altered (Fig. 3B and D). By detecting the levels of key regulatory proteins in the cell cycle, it was found that SHCBP1 knockdown resulted in downregulation of CDK4 and cyclin D1 (Fig. 3E). These data indicated that SHCBP1 promoted cell cycle progression in GC cells.
Figure 3.
SHCBP1 promotes cell cycle progression of GC cells via CDK4-cyclin D1. (A and C) Flow cytometry was used to detect the cell cycle in sh-SHCBP1-treated MGC-803 and SGC-7901 cells, with sh-NC and untreated cells as controls. (B and D) Analysis of the percentage of each phase in A and C **P<0.01. (E) Western blotting showed expression of CDK4 and cyclin D1 after SHCBP1 knockdown in MGC-803 and SGC-7901 cells. SHCBP1, SHC SH2 domain-binding protein 1; GC, gastric cancer; sh-SHCBP1, SHCBP1-shRNA; sh-NC, negative control-shRNA.
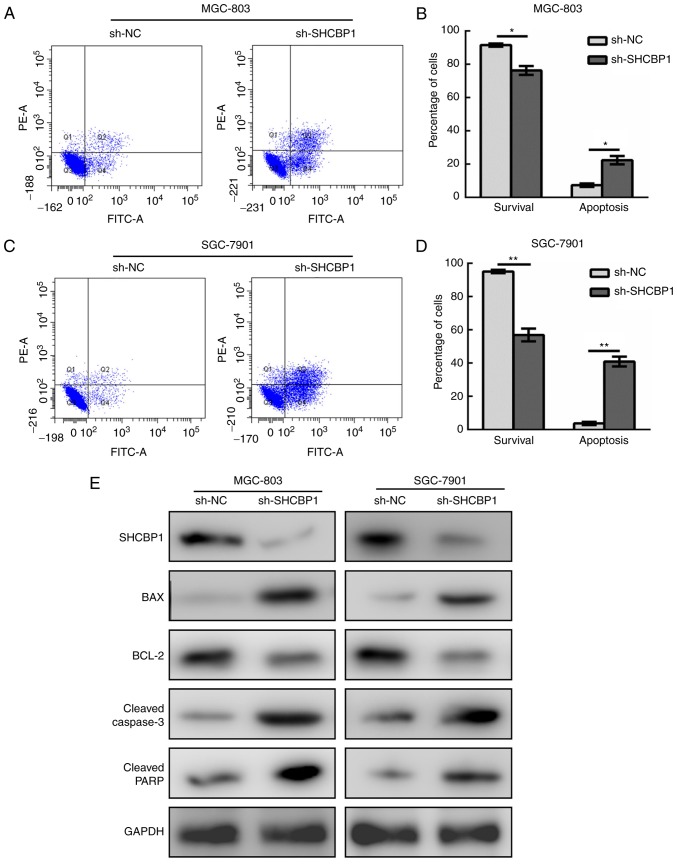
SHCBP1 alters the apoptosis pathway and inhibits apoptosis of GC cells
In a similar manner, GC cell lines MGC-803 (Fig. 4A and B) and SGC-7901 (Fig. 4C and D) expressing sh-NC and sh-SHCBP1 were subjected to apoptosis analysis by flow cytometry. It was found that the percentage of apoptotic GC cells increased after SHCBP1 knockdown, and the proportion of surviving cells decreased. The results of apoptosis-related markers revealed that the levels of Bax, cleaved caspase-3 and cleaved PARP increased with SHCBP1 knockdown (Fig. 4E). Therefore, the role of SHCBP1 in GC cells was to inhibit apoptosis.
Figure 4.
SHCBP1 inhibits apoptosis of GC cells by regulating the caspase-dependent pathway. (A and C) Flow cytometry was used to detect apoptosis in MGC-803 and SGC-7901 cells expressing sh-SHCBP1, with sh-NC used as a control. (B and D) Analysis of the percentage of survival and apoptotic cells in A and C *P<0.05, **P<0.01. (E) Western blot analysis revealed the levels of apoptosis-related proteins after knockdown of SHCBP1 in MGC-803 and SGC-7901 cells. SHCBP1, SHC SH2 domain-binding protein 1; GC, gastric cancer; sh-SHCBP1, SHCBP1-shRNA; sh-NC, negative control-shRNA.
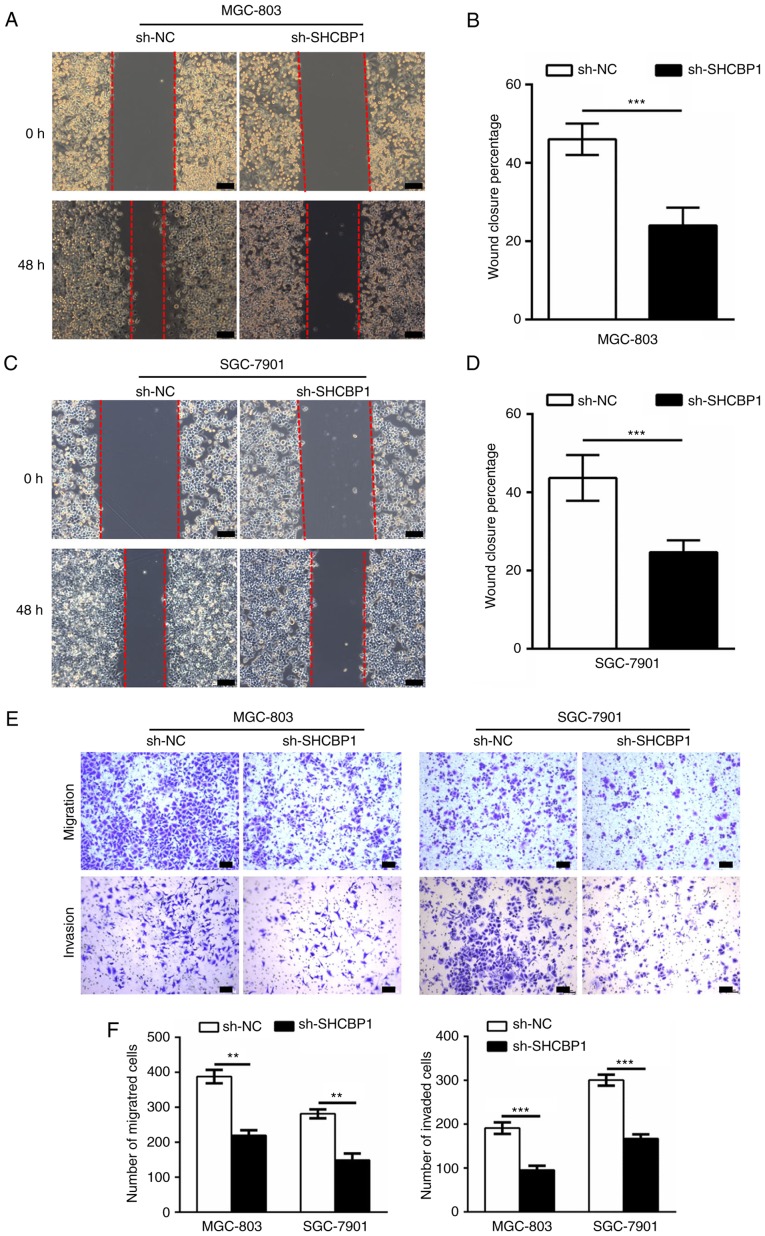
SHCBP1 promotes invasion and metastasis of GC cells
The role of SHCBP1 in the invasion and metastasis of GC cells was then investigated. The wound healing assays examined the effect of knockdown of SHCBP1 on migration ability, and the migration distance of sh-SHCBP1 MGC-803 (Fig. 5A and B) and SGC-7901 (Fig. 5C and D) cells was significantly reduced compared to the control and sh-NC cells. In the invasion and metastasis assays, we assessed the invasion and migration abilities of treated MGC-803 and SGC-7901 cells by Transwell. The number of invading and migrating cells in sh-SHCBP1 cells was significantly reduced compared to control and sh-NC cells (Fig. 5E and F). These data indicated that expression of SHCBP1 enhanced the ability of GC cells to invade and metastasize.
Figure 5.
SHCBP1 enhances the invasion and metastasis of GC cells. (A and C) Wound healing assay revealed the mobility of MGC-803 and SGC-7901 cells after sh-SHCBP1 knockdown, with sh-NC used as a control. (B and D) Percentage statistics of wound healing in A and C. ***P<0.001. (E) Transwell assays examined the effect of SHCBP1 knockdown on cell migration (top panel) and invasion (bottom panel). (F) Statistical graph of the number of migrated and invaded cells. **P<0.01, ***P<0.001. SHCBP1, SHC SH2 domain-binding protein 1; GC, gastric cancer; sh-SHCBP1, SHCBP1-shRNA; sh-NC, negative control-shRNA.
Discussion
At present, the prognosis of GC still relies on traditional pathological indicators such as tumor size and histological grade (14,15). Therefore, it is imperative to study the relevant molecular mechanisms in the development of GC. The development of GC involves a series of oncogenes and tumor suppressors. Screening for new oncogenes and studying their mechanisms of action have important clinical diagnostic value for the early diagnosis of biomarkers and potential molecular therapeutic targets for GC. The metastasis of GC is a multi-step pathological process involving a loss of epithelial properties, such as reduced expression of E-cadherin, and a gain in mesenchymal phenotypes, such as enhanced expression of N-cadherin and vimentin (16). On one hand, tumor cells regulate the changes of their own molecules, so that they can develop in the direction of metastasis; on the other hand, they interact with other cells to form a special metastatic microenvironment and promote liver metastasis of GC (17). At present, there are still many molecular mechanisms to be studied in the process of GC metastasis. Although GC is easily transferred to the liver mainly due to the function of the liver and intestine, numerous studies have shown that tumor cells do not tend to metastasize to the nearest organ, and different tumors have the specificity of organ metastasis (18). The intrinsic determinants of GC-specific metastasis are still unclear. Finding specific genes important for GC liver metastasis is a priority for future research. The development of targeted therapeutic drugs for these specific molecules has important clinical application value. Each process of GC liver metastasis is inseparable from the interaction with the microenvironment, and the tumor microenvironment plays an important role in promoting the metastatic process (19). Considering the invasion-promoting ability of SHCBP1 in various cancers and in GC, it is of high significance to further examine the relationship between SHCBP1 expression and liver metastasis. Additionally, enlarged human tissues are required to assess the potential of SHCBP1 to serve as an early diagnostic marker.
Research on the transfer microenvironment has gradually become the main research direction in the field of cancer, however research on the microenvironment of liver metastasis of GC is still in its preliminary stage, and in-depth research is required to have a clearer understanding of liver metastasis of GC (20). In recent years, tumor treatment strategies targeting the tumor microenvironment have rapidly developed, and drugs targeting the tumor extracellular matrix, endothelial cells or immune cells have been increasingly developed and utilized (21). However, in GC, particularly liver metastasis, there is still a lack of effective targeted therapies. Since many patients with liver metastases have been unable to undergo surgery, accurate targeted therapy and emerging immunotherapy may be the main way to treat liver metastasis of GC in the future.
To further clarify whether SHCBP1 can act on the proliferation and invasion of GC cells, we first detected the expression of SHCBP1 in different GC cells, and selected the cell lines with higher relative expression. Then, shRNA interfered with SHCBP1 expression, and subsequently an MTT assay, flow cytometry and cell invasion assay were used to evaluate the effect of interference with the expression of SHCBP1 on proliferation, apoptosis and invasion of GC cells. At last, the effect of SHCBP1 on the downstream signal factors of proliferation was detected by western blotting. The possible molecular mechanism of SHCBP1 in the proliferation and invasion of GC cells was explored, which provided a theoretical basis for the mechanism of SHCBP1 in the development of GC.
The clinical treatment of tumors is gradually shifting to individualization, and the discovery of new biomarkers can be used for early diagnosis of tumors, prediction of the probability of metastatic spread and recurrence and evaluation of treatment effects. The SHCBP1 signaling pathway has been revealed to be involved in the pathogenesis of a variety of malignant tumors, promoting tumor proliferation, migration and invasion, and inhibiting apoptosis and differentiation (11,22,23). Therefore, the application of SHCBP1 and its signaling pathway in the diagnosis and treatment of tumors may have a high significance. Currently SHCBP1 is being used as follows: i) SHCBP1-specific inhibitors are being used to antagonize binding to SHCBP1 and inhibit tumor cell proliferation and migration; ii) siRNAs to silence the SHCBP1 gene are being applied, thereby changing the expression and function of SHCBP1, consequently preventing and inhibiting the autocrine pathway and its mediated tumor cell activity; iii) blocking the anti-apoptotic effect of the SHCBP1 downstream signaling pathway is being used; iv) intervention to regulate the upstream signaling pathway of SHCBP1 is also being utilized, thereby indirectly regulating the SHCBP1 signaling pathway; v) in addition, radiolabels and drugs are being designed to bind to SHCBP1 inhibitors, and transport radioactive markers or drugs to tumor cells expressing SHCBP1 for imaging diagnosis and targeted therapy of tumors. In summary, SHCBP1 plays an important role in the development of GC and is expected to become an important biomarker and therapeutic target for the early diagnosis of tumors.
Acknowledgements
Not applicable.
Funding
The present study was supported in part by a grant from the Health and Family Planning Commission of Henan Province (no. 182102310205).
Availability of data and materials
The datasets used during the present study are available from the corresponding author upon reasonable request.
Authors' contributions
DYL supervised and directed this study. YDD and YLY performed most of the experiments. DYL, YDD and YLY contributed to the project design. HBY, GJT and YDD performed the western blot analysis and the Traswell assays. HBY and GJT contributed to the RNA extraction. DYL, YDD and YLY analyzed the data and wrote the manuscript. All authors read and approved the manuscript and agree to be accountable for all aspects of the research in ensuring that the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors state that they have no competing interests.
References
- 1.Whiting J, Sano T, Saka M, Fukagawa T, Katai H, Sasako M. Follow-up of gastric cancer: A review. Gastric Cancer. 2006;9:74–81. doi: 10.1007/s10120-006-0360-0. [DOI] [PubMed] [Google Scholar]
- 2.Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R, Pallares C, Sanchez JM, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncolog. 2012;13:239–246. doi: 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- 3.Shitara K, Kondo C, Takahari D, Ura T, Muro K, Matsuo K. Reporting patient characteristics and stratification factors in randomized trials of systemic chemotherapy for advanced gastric cancer. Gastric Cancer. 2012;15:137–143. doi: 10.1007/s10120-011-0083-8. [DOI] [PubMed] [Google Scholar]
- 4.Baek HU, Sang BK, Cho EH, Jin SH, Yu HJ, Lee JI, Bang HY, Lim CS. Hepatic resection for hepatic metastases from gastric adenocarcinoma. J Gastric Cancer. 2013;13:86–92. doi: 10.5230/jgc.2013.13.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heinrich JN, Kwak SP, Howland DS, Chen J, Sturner S, Sullivan K, Lipinski K, Cheng KY, She Y, Lo F, et al. Disruption of ShcA signaling halts cell proliferation-Characterization of ShcC residues that influence signaling pathways using yeast. Cell Signal. 2006;18:795–806. doi: 10.1016/j.cellsig.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Ferro M, Savino MT, Ortensi B, Finetti F, Genovese L, Masi G, Ulivieri C, Benati D, Pelicci G, Baldari CT. The shc family protein adaptor, rai, negatively regulates T cell antigen receptor signaling by inhibiting ZAP-70 recruitment and activation. PLoS One. 2011;6:e29899. doi: 10.1371/journal.pone.0029899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shih HJ, Chen HH, Chen YA, Wu MH, Liou GG, Chang WW, Chen L, Wang LH, Hsu HL. Targeting MCT-1 oncogene inhibits Shc pathway and xenograft tumorigenicity. Oncotarget. 2012;3:1401–1415. doi: 10.18632/oncotarget.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Francia P, Cosentino F, Schiavoni M, Huang Y, Perna E, Camici GG, Lüscher TF, Volpe M. p66Shc protein, oxidative stress, and cardiovascular complications of diabetes: The missing link. J Mol Med. 2009;87:885–891. doi: 10.1007/s00109-009-0499-3. [DOI] [PubMed] [Google Scholar]
- 9.Asano E, Hasegawa H, Hyodo T, Ito S, Maeda M, Chen D, Takahashi M, Hamaguchi M, Senga T. SHCBP1 is required for midbody organization and cytokinesis completion. Cell Cycle. 2014;13:2744–2751. doi: 10.4161/15384101.2015.945840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tao HC, Wang HX, Dai M, Gu CY, Wang Q, Han ZG, Cai B. Targeting SHCBP1 inhibits cell proliferation in human hepatocellular carcinoma cells. Asian Pac J Cancer Prev. 2013;14:5645–5650. doi: 10.7314/APJCP.2013.14.10.5645. [DOI] [PubMed] [Google Scholar]
- 11.Asano E, Hasegawa H, Hyodo T, Ito S, Maeda M, Takahashi M, Hamaguchi M, Senga T. The Aurora-B-mediated phosphorylation of SHCBP1 regulates cytokinetic furrow ingression. J Cell Sci. 2013;126:3263–3270. doi: 10.1242/jcs.124875. [DOI] [PubMed] [Google Scholar]
- 12.Peng C, Zhao H, Chen W, Song Y, Wang X, Li J, Qiao Y, Wu D, Ma S, Wang X, et al. Identification of SHCBP1 as a novel downstream target gene of SS18-SSX1 and its functional analysis in progression of synovial sarcoma. Oncotarget. 2016;7:66822–66834. doi: 10.18632/oncotarget.11651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2ΔΔCT method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 14.Van CE. The treatment of advanced gastric cancer: New findings on the activity of the taxanes. Oncologist. 2004;2:9–15. doi: 10.1634/theoncologist.9-suppl_2-9. [DOI] [PubMed] [Google Scholar]
- 15.Aoyama T, Maezawa Y, Sawazaki S. Evaluation of clinic pathological characteristics and prognosis of gastric cancer in elderly patients. Ann Cancer Res Ther. 2018;26:31–32. doi: 10.4993/acrt.26.31. [DOI] [Google Scholar]
- 16.Deng X, Liu P, Zhao Y, Wang Q. Expression profiling of CEACAM6 associated with the tumorigenesis and progression in gastric adenocarcinoma. Genet Mol Res. 2014;13:7686–7697. doi: 10.4238/2014.September.26.6. [DOI] [PubMed] [Google Scholar]
- 17.Ren G, Tian Q, An Y, Feng B, Lu Y, Liang J, Li K, Shang Y, Nie Y, Wang X, Fan D. Coronin 3 promotes gastric cancer metastasis via the up-regulation of MMP-9 and cathepsin K. Mol Cancer. 2012;11:67. doi: 10.1186/1476-4598-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Obenauf AC, Massagué J. Surviving at a distance: Organ specific metastasis. Trends Cancer. 2015;1:76–91. doi: 10.1016/j.trecan.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Romano F, Garancini M, Uggeri F, Degrate L, Nespoli L, Gianotti L, Nespoli A, Uggeri F. Surgical treatment of liver metastases of gastric cancer: State of the art. World J Surg Oncol. 2012;10:157. doi: 10.1186/1477-7819-10-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsuboi K, Kodera Y, Nakanishi H, Ito S, Mochizuki Y, Nakayama G, Koike M, Fujiwara M, Yamamura Y, Nakao A. Expression of CXCL12 and CXCR4 in pT3-stage gastric cancer does not correlate with peritoneal metastasis. Oncol Rep. 2008;20:1117–1123. [PubMed] [Google Scholar]
- 21.Patra C, Boccaccini AR, Engel FB. Vascularisation for cardiac tissue engineering: The extracellular matrix. Thromb Haemost. 2015;113:532–547. doi: 10.1160/TH14-05-0480. [DOI] [PubMed] [Google Scholar]
- 22.Peng C, Zhao H, Song Y, Chen W, Wang X, Liu X, Zhang C, Zhao J, Li J, Cheng G, et al. SHCBP1 promotes synovial sarcoma cell metastasis via targeting TGF-β1/Smad signaling pathway and is associated with poor prognosis. J Exp Clini Cancer Res. 2017;36:141. doi: 10.1186/s13046-017-0616-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng W, Li HC, Xu K, Chen YF, Pan LY, Mei Y, Cai H, Jiang YM, Chen T, Feng DX. SHCBP1 is over-expressed in breast cancer and is important in the proliferation and apoptosis of the human malignant breast cancer cell line. Gene. 2016;587:91–97. doi: 10.1016/j.gene.2016.04.046. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the present study are available from the corresponding author upon reasonable request.