Abstract
Purpose:
There is an emerging standard to provide patients rapid electronic access to elements of their medical records. Although surveys of patients generally support it, this practice is controversial among oncologists, because few empiric data are available for scenarios of potentially life-threatening conditions like cancer. We report the views of oncologists about patient electronic access to radiology and pathology results that could potentially indicate disease progression.
Methods:
Four months before oncologists were surveyed, final results of radiology/pathology reports were routinely made available to patients online through a secure portal after a 7-day, hold to provide clinicians time to review and communicate results with the patients. Mixed methods were used to assess physician attitudes and experiences toward this change.
Results:
One hundred twenty-nine oncologists were surveyed, and 82 (64%) responded. A small majority (54%) responded that the release of reports was somewhat or very beneficial for patients who received normal radiology/pathology results before discussion with a physician, but 87% said it was somewhat or very harmful for patients to receive abnormal results before discussion. Forty-nine percent reported that release of reports had a somewhat or very negative impact on communication with their patients.
Conclusion:
Almost half of oncologists reported that sharing digital radiology and pathology records had a negative impact on their communication with patients. Patient surveys in similar cancer populations would complement the physician perspective. Efforts are needed to improve consensus among oncologists and patients on how to best communicate such results in a timely fashion.
INTRODUCTION
The 21st century has seen a strong move toward engagement of patients in their own health care.1-5 Shared decision making is a well-accepted patient-centric standard and has been accompanied by efforts to share information previously relatively inaccessible to patients. The Health Insurance Portability and Accountability Act (HIPAA), for instance, entitles patients to obtain their medical records on request.6 Supporters believed that better access to their own data would improve patient engagement, which itself had been associated with improved outcomes.7 At the time HIPAA was enacted in 1996, most health records were in paper form, which made sharing tedious and often impractical. The advent of electronic health records, spurred by the meaningful use standards of the American Reinvestment Act of 2009, has much reduced those concerns. Instead, concerns have arisen that real-time access to results without mediating physician input might harm patients, especially those with serious diseases.8 Given the asymmetry of skills, patients might misunderstand results that physicians could explain, which could result in undue anxiety and even reduced adherence.
Previous studies have primarily examined patient access to physician notes and laboratory tests in the context of primary care, in which serious conditions are relatively uncommon.9-12 A few studies extended to the context of the emergency room13 or specialty care setting.14 This study seeks to extend the existing literature by exploring oncologist perspectives and experiences at a single academic cancer center approximately 4 months after implementation of a system that allowed release of finalized radiology and pathology results to patients with cancer via a secure patient portal. Specifically, we investigated attitudes, experiences, and opinions about the release of normal versus abnormal results, the timing of the release to patients relative to communication with the physician, and the impact of electronic release of reports to patients on oncologist behaviors and/or communications with patients.
METHODS
As part of a large digital health initiative aimed at improvement of patient engagement, Stanford Cancer Center enabled release of finalized radiology and pathology results to patients with cancer via their secure patient portals in late April 2015. Patients who had had an imaging test or biopsy received an e-mail to let them know that their results were available in their electronic health records upon physician review and approval of results or 7 days after the report was finalized, whichever came first.
As part of a quality improvement initiative, we developed a brief questionnaire to obtain the opinions and experiences of practicing oncologists approximately 4 months after the system had been implemented. The questionnaire was developed with input from evaluation experts (M.W., F.H.-S., S.M.A.), oncologists (E.L.R., M.K.B.), the Cancer Medical Director (E.L.R.), and the Chief Medical Information Officer (C.S.) of Stanford Hospitals and Clinics. The questionnaire included six Likert-scale questions—four about oncologist opinions and two about their experiences with release of radiology and pathology results to patients—plus one open-ended additional comment field. The opinion questions asked about the following: (1) physician opinion in patient receipt of radiology/pathology results before discussion with a physician; (2) effect on patient if normal results are received before discussion with a physician; (3) effect on patient if abnormal results are received before discussion with a physician; and (4) the minimum amount of elapsed time needed for oncologists before they talk with the patient. The experience questions asked about the following: (1) whether they had changed their process for review of radiology/pathology reports upon implementation of patient access to reports and (2) the impact that the release of reports had on their communication with their patients.
The Research Electronic Data Capture tools15 hosted at Stanford University were used to send the questionnaire to oncologists via automated emails; to monitor response rates; and to collect, store, and manage the data. All practicing oncologists at Stanford Cancer Center were sent an automated e-mail with a personalized message from the medical director that requested their input via completion of the questionnaire to help inform policy decisions about the release of radiology/pathology reports to patients. Confidentiality of any responses and comments was ensured. Two reminder emails were sent, each 1 week apart, to individuals who had not already completed the survey. The survey was available for completion from September 21, 2015, through October 7, 2015 (Data Supplement).
Descriptive statistics were calculated for responses to each question, and the response rate was calculated. Data analysis was performed with the statistical software R studio version 0.98.501. Two coders, experts in health systems (M.W.) and qualitative health research (C.B.-J.), respectively, developed coding schemas and independently identified key themes from the open-ended comments (n = 35).16-18 Through iterative meetings, coders achieved consensus with high agreement. Of the 47 items coded initially, only three items were subsequently modified on the basis of the second coder. The questionnaire was reviewed and deemed exempt by the local institutional review board as quality improvement.
RESULTS
Surveys were sent to 129 oncologists and were completed by 82 (63.5%), and 35 respondents wrote a comment. Fifty-one percent of respondents were medical oncologists, 35% were surgical oncologists, and 14% were radiation oncologists. Specialists from teams that treated all major tumor sites, including, breast, gynecology, genitourinary, gastrointestinal, thoracic, head and neck, neurologic, cutaneous, sarcoma, lymphoma, hematologic, and bone marrow transfer, were included.
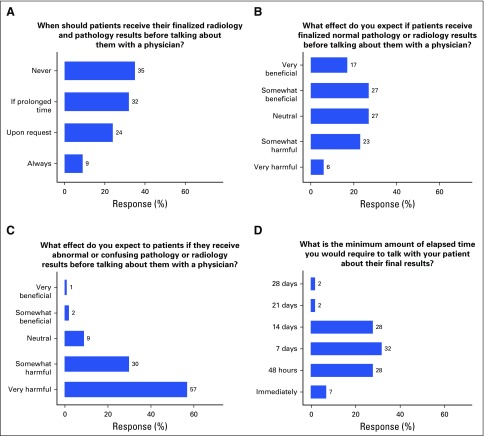
Figure 1 shows the distribution of responses for the opinion questions. Thirty-five percent of oncologists responded that patients should never see results of radiology/pathology reports before consultation with their physicians, and a similar percentage (32%) reported that release should take place only if time to discussion with doctor is prolonged (Fig 1A). When asked about expected effects on patients who receive normal reports before consultation, 44% responded this would be somewhat or very beneficial (Fig 1B). In contrast, 87% responded that the expected effect on patients who receive abnormal or confusing reports before consultation would be somewhat or very harmful (Fig 1C). If results were to be released, a 14-day or shorter review period was supported by most oncologists (Fig 1D).
FIG 1.
Oncologists’ opinions about patient access to radiology and pathology results via an online secure portal.
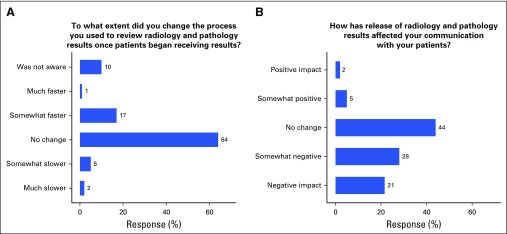
Figure 2 shows the distribution of responses to the two experience questions. Most respondents (90%) were aware of the changes made in patient access to radiology/pathology reports; however, 64% of respondents had not changed their results review and communication process (Fig 2A). Almost 50% reported that release of radiology/pathology reports had a somewhat negative or negative impact on communication with their patients (Fig 2B). Oncologists who reported a negative impact on communication (n = 40) were less likely than those who reported no change or a positive impact in their communication with their patients to view release of normal results to patients as beneficial (25% v 61%; P = .001). Similarly, oncologists who reported a negative impact on communication were more likely than their counterparts to view release of abnormal results to patients as harmful (100% v 76%; P = .002).
FIG 2.
Oncologists’ experiences with change in process (A) and change in communication with patients (B) as a result of patient access to radiology and pathology results via an online secure portal.
Four main themes emerged from the theme-based analysis of the 35 open-ended written comments: patient ability to interpret reports, quality of care, support of (extra) work, and expectation setting. Respondents who provided a negative response to question 2, depicted in Figure 1B, were just as likely as those who provided a neutral or positive response to write a comment (P = .83), which suggested that comments were not biased toward any particular opinion group. Furthermore, comments were made by those who had both negative and positive opinions on each of the four main themes.
Table 1 lists three to four representative opinion comments in each theme. Sixteen comments related to the patient ability to interpret reports. Key points were that (1) patients are not able to properly interpret results as currently written, because reports are written for clinicians, not patients, and (2) patient research of clinical terminology and/or diagnoses in reports often leads to additional misunderstanding and anxiety. Consistent with the survey, opinions about whether normal results were reasonable to release to patients differed. Some respondents expressed only concern for equivocal or abnormal results, whereas others gave examples of patients who had misunderstood normal or benign results, largely because of the terminology used. Some also expressed concerns that radiologists, pathologists, and attending physicians may differ in their interpretation of radiology or (more rarely) pathology because of differences in knowledge in the patient history and/or context for the test, which can lead to confusion and anxiety for the patient and, potentially, to errors.
Table 1.
Representative Opinions of Each Theme Expressed by Oncologists in Comment Field
| Theme | Opinion |
|---|---|
| Patients' abilities to interpret reports | Patients won't understand what normal pathology is, making physician and staff review imperative prior to release to the patient. |
| Currently, the language of these reports contains code that informs us physicians but confuses the patients. | |
| Radiologists need to stop using vague terminology that alarms patients. | |
| The release of results has led to frequent misinterpretation by patients, who may not understand the medical terminology within the reports. | |
| Quality of care | I have had multiple patients call to not come in because they want results online…. It’s bad care to never see patients on whom you order tests. |
| Our medical decision making is informed by subtle clues and it is important for physicians to formulate a plan and a response before discussing it with the patient. | |
| I had a medical oncologist misread the pathology report and felt pressured to call the patient before I had a chance to review. He told the patient that all of her margins were positive and that she needed further surgery. In fact, all of her margins were widely negative and she needed no further therapy. | |
| Extra work | I think we just need to have systems to support us. I do believe that release of results is important, but we need to work with patients to get appointments coordinated in a timely fashion for discussion, or we need to have credit for time spent on the phone in discussion. |
| This system of releasing laboratory results would be tenable if physicians universally had qualified support in the form of NC or APP. We don't. | |
| I encourage my nurse and/or PA to discuss normal results, but I tend to discuss abnormal results with patients. The former can often happen sooner if my RN/PA help. | |
| Release adds substantially to time, because I try to avoid having results of these studies released automatically in the absence of a note that puts the result in context, or I try to anticipate and explain potentially confusing or threatening results. This requires a significant expenditure of time and might be better accomplished face to face. | |
| Expectations | I believe I set the right expectations with patients. We are always available to discuss results comprehensively during their next visit or briefly through myHealth between visits. |
| I explain to all of my patients at the time I order a test that I will do the best I can to get the results to them in a timely manner. And I explain to them what the spectrum of results may be, so if they hear them first, they will understand the implications. | |
| The issue is when they get a result they didn't expect or there is something that sounds concerning and they don't understand what it means.... Are they going to need a long phone call that would otherwise take place during a clinic visit? Although immediate access to results may have its benefits, I think that the physician should approve the release of every result before the patient can access it. |
Abbreviations: APP, advanced practice provider; NC, nurse coordinator; PA, physician’s assistant; RN, registered nurse.
The eleven comments in the theme of quality of care related to quality in the context of communication, coordination, and/or patient safety. Several comments expressed the importance of meeting with patients face to face to relay bad news or sensitive information, with the perspective that relay of such information deserves in-person counseling. Two comments also relayed the importance of time to prepare a plan prior to speaking with the patient and before the patient sees his or her results, if the results indicate action is needed (eg, “I prefer to have a plan in place”). Two comments also relayed concerns and/or instances of errors in communications with patients that had occurred because of differences in the interpretation of results in the medical team combined with feelings of urgency to communicate results quickly to the patient before the attending physician could review the results.
Ten comments fell into the theme of support for (extra) work, which expressed the need for appropriate staff support to enable timely response to patients about report results, whether by phone calls or by face-to-face visits. Some expressed frustration because of the lack of support, whereas others expressed that use of medical support staff has allowed them to be successful in timely communication of normal results to patients before results are released online. There was universal messaging, explicit and implied, that abnormal results are or should always be relayed first to patients by the primary physician or covering physician. There were five comments that indicated that release of results to patients has created extra work for physicians that is not billable (ie, emails and phone calls, as well as time spent writing a note about the results to put them in context before the patient discussion).
Six comments were categorized as expectations, because they focused on efforts the physicians made to ensure that patients knew what to expect in terms of both possible results of tests and when they could expect to receive the results. One suggestion recommended that it be made physically clearer in the electronic medical record when results would be released to patients, so that physicians had clearer expectations of timelines: “There should be a note in bold (possibly red) stating that this report will be automatically released to the patient on....”
DISCUSSION
Oncologists agreed that patient online access to abnormal radiology/pathology results has negative consequences (87%), whereas opinions were more mixed for normal results. Almost half of oncologists, however, reported that sharing online results had worsened their communications with patients, and these oncologists were most worried about abnormal results. Written comments supported these findings; concern over patient abilities to properly understand reports was the most frequent comment theme. Although a strong majority of respondents wanted, at most, 14 days to communicate results to patients, only 27% wanted > 7 days (the current embargo), which suggests that discomfort with the release went beyond the current allotted time and likely reflected concern about patient abilities to understand reports. Written comments also suggested that better success with online release of radiology/pathology results to patients could be obtained with appropriate medical staff support. It is possible that such support would allow more timely contact with patients and could decrease anxiety for both physicians and patients.
There have not been any other studies that have focused on the opinions of oncologists with respect to the timing of release of radiology/pathology reports. A recent survey of primary care physicians and specialists from Australia and the United States reported that 77% of physicians were uncomfortable with the release of abnormal test results to patients online before discussion for chest x-ray, HIV tests, and cancer screening tests, whereas 65% believed that patients should have online access to results that were normal.13 Another study assessed oncologist opinions of immediate release of laboratory reports to patients with cancer before and after implementation of online release via a secure patient portal.19 Although there was a significant increase in oncologist approval of online patient access to laboratory results (25% before and 40% after), only 35% were comfortable with immediate access by patients, and only 13% thought that patients could reasonably interpret their results.
The best assessments conducted in seriously ill patients to date are simulation studies. Johnson et al20 assessed patient preference for method and timing of receipt of imaging results and included patients with both serious and nonserious diseases who had recently had a computed tomography scan or MRI. Patients responded to clinical simulations that included results that were normal, seriously abnormal, and indeterminate. Regardless of the scenarios, > 80% of patients wanted to receive results within 3 days and preferred receipt via an online secure portal compared with any other method, including a return visit, call from physician or nurse, e-mail, or letter. Furthermore, only 15% wanted to postpone receipt of their results until after discussion about them with their physicians. Seventy-one percent said they would want to talk with their doctor, however, to understand the results, although the study did not ask patients how long they were willing to wait to do so. Although the Johnson study included only 53 patients, a small minority of whom may have had cancer, it is unlikely that patients with cancer, diagnosed or undiagnosed, would want to wait > 7 days for important test results. The profound difference between results from this study and ours suggests that perceptions and experiences of patients and physicians differ in important ways. Patients waiting for the outcome of a sensitive and possibly life-changing test are likely to be all-consumed in the wait for the result. Physicians, conversely, balance the care of multiple patients in similar situations and want to make sure they have had time to carefully assess results and develop an action plan, if needed, before discussion with a patient. As a result, although timeliness and nuanced discussion are important to both patients and physicians, they disagree on how and how soon results should be released.10
There are limitations to this study. First, we did not have enough power to assess whether responses varied by patient tumor site or severity of disease. Although the response rate was quite good for physician surveys, the study was relatively small and was conducted at a single cancer center. Four months may not have been enough time to fully evaluate the impact of the policy change and may not be reflective of future opinions. Another limitation is that we do not know the reasons for the negative impact on communication with patients reported by almost half of the oncologists and, therefore, are not able to estimate the degree to which negative outcomes were preventable through expectation setting or other means. A study of patients in Kaiser health plans10 found that patients whose expectations were set by their doctors before laboratory tests were less likely to e-mail or telephone their doctors or schedule additional appointments after receipt of the test results online and experienced significantly more satisfaction and less anxiety than those who did not speak with their doctors before they viewed their results. It is clear by the comments that several respondents consider expectation setting an important part of their practice. We are planning to conduct a more formal qualitative study that includes focus groups of oncologists to broaden our understanding of facilitators and barriers to online release of radiology/pathology results to patients to address several of the current limitations. The biggest limitation, of course, is that we did not speak with patients with cancer directly about their experiences; our next step is to survey current patients about their experiences with respect to this policy.
In summary, this is the first report that attempts to evaluate the impact of the release of reports directly to patients with cancer. Our results raise concerns that there could be significant negative impacts on both provider and patient wellness. Clearer understanding of physician and patient experiences with release of potentially sensitive results could lead to better recommendations for how to share complex results with critically ill patients in a patient-centered manner. Additional study is needed to understand how the release of complex medical reports should be performed to create a patient-centric and transparent health care system without compromising its compassion.
Acknowledgment
This study was funded by Stanford Health Care. C.B.-J. was supported by Grants No. T32HL007034-39 from the National Heart, Blood and Lung Institute and 21BT-0018 from the California Tobacco-Related Disease Research Program. Presented in part as a poster at the ASCO Quality Care Symposium, Phoenix, AZ, February 26-27, 2016.
AUTHOR CONTRIBUTIONS
Conception and design: Marcy Winget, Farnoosh Haji-Sheikhi, Eben L. Rosenthal, Christopher Sharp, Mark K. Buyyounouski, Steven M. Asch
Administrative support: Marcy Winget, Farnoosh Haji-Sheikhi
Collection and assembly of data: Marcy Winget, Eben L. Rosenthal
Data analysis and interpretation: Marcy Winget, Farnoosh Haji-Sheikhi, Cati Brown-Johnson, Steven M. Asch
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Electronic Release of Pathology and Radiology Results to Patients: Opinions and Experiences of Oncologists
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Marcy Winget
No relationship to disclose
Farnoosh Haji-Sheikhi
No relationship to disclose
Cati Brown-Johnson
Other Relationship: HealthTap
Eben L. Rosenthal
Consulting or Advisory Role: Aspyrian Therapeutics
Research Funding: Novadaq Technologies (Inst), Li-Cor Biosciences (Inst)
Christopher Sharp
No relationship to disclose
Mark K. Buyyounouski
No relationship to disclose
Steven M. Asch
No relationship to disclose
References
- 1.Ross SE, Lin CT: The effects of promoting patient access to medical records: A review J Am Med Inform Assoc 10:129–138,2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gruman J Rovner MH French ME, etal: From patient education to patient engagement: Implications for the field of patient education Patient Educ Couns 78:350–356,2010 [DOI] [PubMed] [Google Scholar]
- 3.Thompson AGH: The meaning of patient involvement and participation in health care consultations: A taxonomy Soc Sci Med 64:1297–1310,2007 [DOI] [PubMed] [Google Scholar]
- 4.Entwistle VA, Watt IS: Patient involvement in treatment decision-making: The case for a broader conceptual framework Patient Educ Couns 63:268–278,2006 [DOI] [PubMed] [Google Scholar]
- 5.Forbat L Cayless S Knighting K, etal: Engaging patients in health care: An empirical study of the role of engagement on attitudes and action Patient Educ Couns 74:84–90,2009 [DOI] [PubMed] [Google Scholar]
- 6. US Department of Health and Human Services: Health information privacy. http://www.hhs.gov/ocr/privacy/
- 7.Mosen DM Schmittdiel J Hibbard J, etal: Is patient activation associated with outcomes of care for adults with chronic conditions? J Ambul Care Manage 30:21–29,2007 [DOI] [PubMed] [Google Scholar]
- 8. US Department of Health and Human Services: The The Health Information Technology for Economic and Clinical Health Act. http://www.hhs.gov/ocr/privacy/hipaa/administrative/enforcementrule/hitechenforcementifr.html.
- 9.Delbanco T Walker J Bell SK., etal: Inviting patients to read their doctors’ notes: A quasi-experimental study and a look ahead Ann Intern Med 157:461–470,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christensen K, Sue VM: Viewing laboratory test results online: Patients’ actions and reactions J Participat Med 5:e38,2013 [Google Scholar]
- 11. Sue VM, Griffin MT, Allen JY: Individual Characteristics Associated with PHR Use in an Integrated Care Organization. 44th Hawaii International Conference on System Sciences, Kauai, HI, January 4-7, 2011 (abstr 1-9)
- 12.Davis Giardina T Menon S Parrish DE, etal: Patient access to medical records and healthcare outcomes: A systematic review J Am Med Inform Assoc 21:737–741,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Callen J Giardina TD Singh H, etal: Emergency physicians’ views of direct notification of laboratory and radiology results to patients using the Internet: A multisite survey J Med Internet Res 17:e60,2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giardina TD Callen J Georgiou A, etal: Releasing test results directly to patients: A multisite survey of physician perspectives Patient Educ Couns 98:788–796,2015 [DOI] [PubMed] [Google Scholar]
- 15.Harris PA Taylor R Thielke R, etal: Research electronic data capture (REDCap): A metadata–driven methodology and workflow process for providing translational research informatics support J Biomed Inform 42:377–381,2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dey I: Qualitative Data Analysis: A User-Friendly Guide for Social Scientists. New York, NY, Routledge, 1993. [Google Scholar]
- 17.Bradley EH, Curry LA, Devers KJ: Qualitative data analysis for health services research: Developing taxonomy, themes, and theory Health Serv Res 42:1758–1772,2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pope C, Mays N (eds): Qualitative Research in Health Care. London, United Kingdom, John Wiley & Sons, 2013. [Google Scholar]
- 19.Rodriguez ES, Thom B, Schneider SM: Nurse and physician perspectives on patients with cancer having online access to their laboratory results Oncol Nurs Forum 38:476–482,2011 [DOI] [PubMed] [Google Scholar]
- 20.Johnson AJ Easterling D Nelson R, etal: Access to radiologic reports via a patient portal: Clinical simulations to investigate patient preferences J Am Coll Radiol 9:256–263,2012 [DOI] [PubMed] [Google Scholar]