Abstract
Fruits and vegetables (FVs) are recognized as healthy constituents of diet and a sustainable solution to the existing twin burden of micronutrient deficiencies and non-communicable diseases in developing and developed countries. In general, FVs are nutrient dense foods low in energy, containing varying amounts of vitamins and minerals including carotenoids, B vitamins, vitamin C, iron, zinc, potassium, calcium, magnesium and fibre. These are abundantly rich in phytochemicals that function as antioxidants, anti-atherosclerotic and anti-inflammatory agents. This review summarizes some epidemiological, prospective cohort and intervention studies on the health benefits of FVs in relation to cardiovascular disease, obesity and diabetes. The rich varieties of FVs available, their composition, production scenario in India, dietary intake and trends over time, barriers to sufficient intake mainly sociocultural, economic and horticulture environment, policies for promotion and prevention of diseases are considered.
Keywords: Cardiovascular disease, diabetes, fruits and vegetables, micronutrients, obesity, phytonutrients
Introduction
Worldwide, today defiant chronic health issues covering a wide spectrum of diseases are encountered. The developing countries, in addition, have to confront the existing nutritional deficiency disorders, particularly micronutrient deficiencies that are extensive in the population with undesirable consequences. Dietary guidelines of several countries suggest that plant food, especially fruits and vegetable (FVs) rich in micro/phytonutrients and the much-needed fibre, are the basis for health and wellness of all age groups and prevent several disorders1. These power-packed nutrient dense colourful foods are low in calories and rich in nutrients/non-nutrients, which synergistically participate in modifying pathophysiological and metabolic aspects of diseases. These are the much-wanted component of healthy diets and are the best gift from nature to nurture the humankind.
This article describes the health benefits of FVs, the rich varieties available, their composition, production scenario in India, daily intake and trends over time, barriers to sufficient intake, how to promote FVs rich diets and the way forward to maximize the intake to proactively prevent non-communicable diseases (NCDs). The WHO and the Dietary Guidelines of India suggest 400 g of FVs per day to reduce NCDs and for overall health1,2. These enhance the diversity of diet and play a prominent role in the prevention of deficiency disorders and diet-related chronic diseases such as cardiovascular disease (CVD) including stroke, cancer, diabetes mellitus (DM), cataract, age-related maculopathy, gastrointestinal problems, chronic obstructive pulmonary disease (COPD) and bone health3. This review highlights the health benefits in relation to CVD, obesity and DM. Briefly, micronutrient deficiency is also emphasized.
Mortality & disability-Adjusted life years (DALYs)
About one per cent of disability-adjusted life years (DALYs) and 2.8 per cent of mortality globally are due to low FVs consumption4. Worldwide, 5.2 million deaths (3.4 and 1.8 million deaths for FVs, respectively) have been attributed to the inadequate intake of FVs2. To improve the FVs intake, focused approaches are required through all stages of life. There is an urgent need for policies to promote varieties and support enhanced production, processing and distribution of FVs to the public.
Micronutrients
Hidden hunger or micronutrients (MN) inadequacy is a public health problem, and worldwide about two billion people suffer from chronic deficiency impacting mortality, morbidity, growth, development, cognition, immune functions, productivity and economy5. Hidden hunger indices are high in sub-Saharan African countries, India and Afghanistan6. About a third of two billion people suffering from MN deficits are in India7. Currently, dietary patterns or food quality, a diversified diet is considered as crucial for the inadequacy of MN. In a model diet, vegetables contribute 12 per cent of iron, 80 per cent of vitamin C, 23 per cent of folates and eight per cent of zinc intakes and fruits to 6, 20 and 12 per cent (mainly greens) respectively to iron, vitamin C and folates in India8.
Nutritional classification
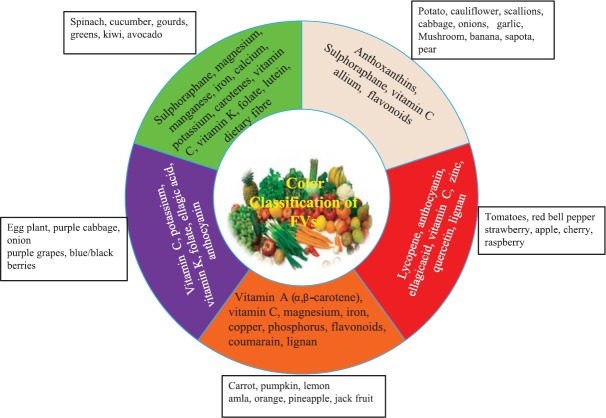
FVs are packed with several nutrients and vital sources of β-carotene (precursor for vitamin A), vitamin C, folic acid, dietary fibre, minerals (potassium, magnesium, zinc and calcium) and several other bioactive compounds including polyphenols and relatively low in calorie, fat and sodium9. These nutritional qualities highlight the importance of FVs as a component of the daily diet. The nutrient and colour classification of FVs are shown in Fig. 1.
Fig. 1.
Colour classification and nutrient composition of fruits and vegetables. Source: Refs 9, 10.
Production
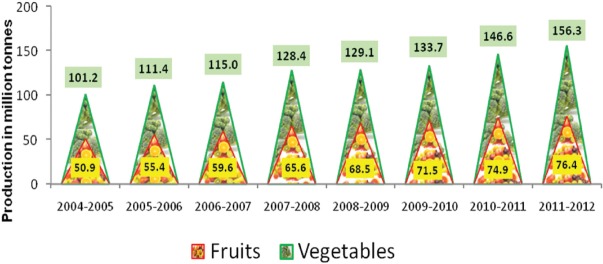
The varied agro-climatic conditions of India favour the production of an array of fresh FVs. These represent over 90 per cent of the horticulture crop production. According to the latest report from the National Horticulture Board (NHB)11, currently 6480 and 10290 million hectare land is used for the production of fruits and vegetables, respectively in India. The productivity was 14.33 (fruits) and 17.01 (vegetables) metric tonnes/hectare in 2016-2017. Next to China, India is the leading producer of FVs in the world, with a production of 92.8 MT and 175 MT of fruits and vegetables, respectively. This approximately represents 10-15 per cent of the global supply11 (Fig. 2).
Fig. 2.
Production of fruits and vegetables during 2004-2012. Source: Ref. 11.
The government of India has initiated the Horticulture Mission in several States for Integrated Development of Horticulture for enhanced production of FVs in the country11. India may develop as a foremost horticulture crops producing, exporting and consuming country in the world12.
Consumption of fruits and vegetables
In many countries, several segments of the population are consistently consuming less than the daily recommended FVs intake. More than 75 per cent of men and women consumed less than recommended servings of FVs in 52 low- and middle-income countries. In India, 74 per cent of adults consumed low amounts of FVs13.
According to the recent National Sample Survey Office (NSSO) report, there has been a slight decline in the calorie contributed by FVs as %E in both rural and urban segments14 (Fig. 3). The consumption of fruits (kg/person/annum) was 9.6 and 15.6 among rural and urban Indians respectively while the intake of vegetables was 74.3 (rural) and 79.1 in urban population14. The data from National Nutrition Monitoring Bureau (NNMB) report also suggested low consumption of FVs, 127 and 26 g/consumption unit/day for vegetables and fruits, respectively15.
Fig. 3.
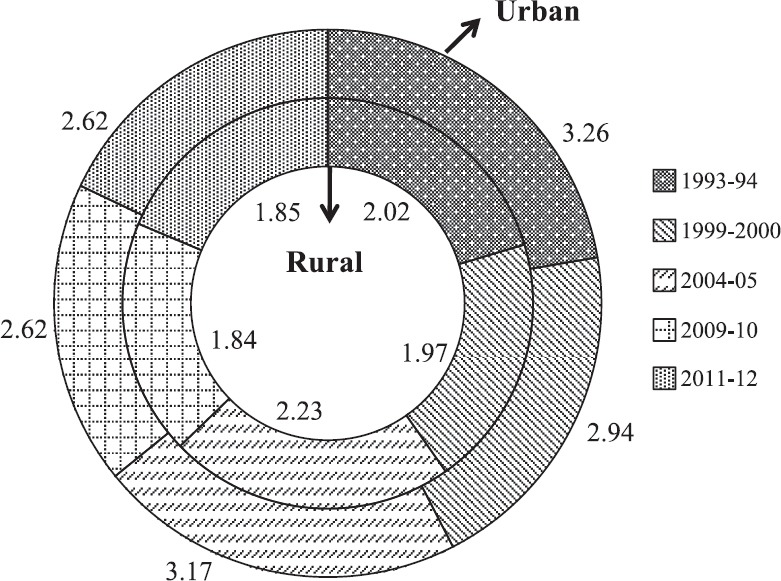
Trends in per cent calorie contribution of fruits and vegetables in urban and rural India. Source: Ref. 14.
A study in 1001 individuals ≥18 yr, fresh FVs intake across five cities of India was below the WHO recommendations (400 g or 5 servings of FVs)16. In cereal staple, Indian diet FVs contributed only nine per cent of total calories with an average intake of 3.5 servings/day (1.5 and 2 serving of FVs, respectively). The study further highlighted the intake was <3 serving/day among the younger generation (18-24 yr). There was variation from city to city with respect to intake of FVs. Chennai had the highest (4.35 servings/day) and Kolkata reported the least (2.81 servings/day)16.
FVs intake and diseases
Cardiovascular diseases (CVDs)
The global epidemiological scenario suggests that CVDs represent the most widespread and challenging health issue. Of the 17.7×106 deaths <70 yr of age, 82 per cent were in low- and middle-income countries, of which 37 per cent were due to CVD in 201517. Globally, deaths due to coronary heart disease (CHD) and stroke were 7.4 and 6.7 million, respectively4.
CVD is the primary cause of death in India and accounts for two-thirds of mortality due to NCDs. Over 50 per cent of deaths occur prematurely between ages 30 and 69 yr18. According to the Global Burden Disease Report 2017, heart disease accounts for about 2.74 million deaths in India19. The major drivers of this epidemic are demographic transition, globalization, socio-economic factors, urbanization and liberalization of markets which have impacted the food environments20. The public health consequences impact human capital, sustainable development and overload the health-care system.
The global health risk report4 identified tobacco, alcohol, high blood pressure (BP), body mass index (BMI), cholesterol, blood glucose, low intake of FVs and physical inactivity accounting for 61 per cent of cardiovascular deaths. FVs is one of the crucial food groups which impacts CVD and other NCDs. About 11 per cent of coronary artery disease (CAD) and nine per cent of stroke deaths worldwide results from unsatisfactory consumption of FVs4. DALYs attributed to low FVs intake are highest in middle-income European countries and South East Asia. The various study details and important findings are presented in Table I.
Table I.
Effect of fruits and vegetables consumption on cardiovascular disease- A summary
| Author | Year | Study | Study participants (n) | Outcome variable | Assessment tool | Major findings | Confounders adjusted |
|---|---|---|---|---|---|---|---|
| Joshipura et al21 | 2001 | Prospective cohort study | 126,399 individuals (84 251 women 42 148 men) 1063 cases | CHD | FFQ | 1 vs. 5 quintile: All FVs: RR 0.80 (0.69-0.93); GLV: 0.72 (0.63-0.83) ↑ 1 serving/day: FVs: RR 0.96 (0.94-0.99); GLV: 0.77 (0.64-0.93) Vitamin C-rich FVs RR 0.94 (CI, 0.88-0.99) |
Age, smoking, alcohol, family history of myocardial infarction, BMI |
| Liu et al22 | 2001 | Physician's health study | 15,220 men 1148 incident cases | CHD | Semi- quantitative FFQ | Highest (+2.5 servings/day) vs. lowest (<1 serving/day) Vegetable RR: 0.77 (0.60-0.98; P=0.03) adjusted↑1 serving vegetable/day RR: 0.83 (0.71-0.98) Results were more evident among men with higher BMI (≥25 kg/m2) Vegetable RR: 0.71 (0.55-0.99) |
Smoking, alcohol, BMI, physical activity, history of diabetes, high cholesterol, hypertension and use of multivitamins |
| Bazzano et al23 | 2002 | Prospective cohortstudy NHANESI | 9608 individuals; 888 stroke events; 1786 IHD events; 1145 CVD deaths and 2530 all-cause mortality | CVD | FFQ | ≥3 times/day compared vs. <1 time/day Stroke incidence RR: 0.73 (0.57-0.95; P for trend=0.01); ↓27% stroke mortality RR: 0.58 (0.33-1.02; P for trend=0.05); ↓42% IHD mortality RR: 0.76 (0.56-1.03; P for trend=0.07); ↓ 24% CVD mortality RR: 0.73 (0.58-0.92 P for trend=0.008); ↓ 27% All-cause mortality RR: 085 (0.72-1.00; P for trend=0.02); ↓ 15% |
Age, sex, race, history of diabetes, physical activity, education level, regular alcohol consumption, current cigarette smoking at baseline, vitamin supplement use, and total energy intake |
| Bazzano et al24 | 2002 | Prospective cohort study NHANES I | 9764 individuals; 926 stroke events; 3758 CVD events | Stroke CVD | Single 24 dietary recall | Highest (405 µg/day) vs. lowest (99 µg/day) folate intake Stroke events RR: 0.79 (0.63-0.99, P for trend 0.03) CVD events RR: 0.86 (0.78-0.95, P for trend-0.001) | Age, race, sex, systolic blood pressure, serum cholesterol, BMI, history of diabetes, physical activity, level of education, regular alcohol consumption, current cigarette smoking, saturated fat intake, and total energy intake |
| Rissanen et al25 | 2003 | Prospective KIHD study | 2641 men | CVD-related and non-CVD - related mortality | 4-day food intake record | Highest (<405 g/day) vs. lowest (<133 g/day) quintile intake of berries, FVs intake: All-cause mortality RR: 0.66 (0.50-0.88) CVD mortality RR: 0.59 (0.33-1.06) Non-CVD mortality RR: 0.68 (0.46-1.00) | Biochemical variables and other risk factors age, BMI, systolic blood pressure, diastolic blood pressure, plasma fibrinogen, serum insulin, blood glucose, serum total cholesterol, serum LDL cholesterol, serum haptoglobin, energy, alcohol, cholesterol, saturated fat, E%/day, fiber, vitamin E, vitamin C, folate, carotene, percentage of total smokers, hypertension, family history of ischaemic heart disease, diabetes, BMI |
| Yusuf et al26 | 2004 | INTERHEART case-control study | 12,461 cases and 14637 controls (52 countries) | MI | Structured questionnaire | Daily vs. lack of daily FVs intake OR: 0·70 (0·62-0·79) | Age, sex, smoking and all other risk factors for MI |
| Rastogi et al27 | 2004 | Case-control study | 350 cases 700 controls | MI | FFQ | Highest (3.5 servings/day) vs. lowest (0.8 servings/day) intake MI RR: 0.33 (0.13-0.82; P for trend 0.006) for total vegetable Highest (3.5 servings/day) vs. lowest (0.5 servings/day) GLV intake MI RR: 0.33 (0.17-0.64; P for trend 0.0001) for GLV No association with fruits were noted | Age; sex; hospital; cigarette smoking; bidi smoking; BMI, in kg/m2; waist-to-hip ratio; leisure time physical exercise; history of hypertension; history of diabetes; history of high cholesterol; family history of IHD; alcohol intake; education; household income; and Hindu religion |
| Radhika et al28 | 2008 | CURES study | 983 individuals | Cardiovascular risk | Validated semi- quantitative FFQ | SBP β=−2·6 (−5·92-1·02 mmHg; P=0·027) BMI β=−2·3 (−2·96-1·57 kg/m2; P<0·0001), waist circumference β=−2·6 (−3·69-−1·46 cm; P<0·0001) | Age, sex, smoking, alcohol and BMI adjusted |
| Total cholesterol (β=−50 (−113·9-−13·6 mg/l; P=0.017) and LDL-cholesterol β=−55 (−110·8-−11·1 mg/l; P=0·039) ↑ Higher intake of FVs elicited 48% protective effect against CVD risk factors | |||||||
| Dauchet et al29 | 2011 | Meta-analysis of cohort studies | 9 independent studies comprising 221,080 individuals and 5007 events | CHD | Literature searches | (+1) portion FVs RR: 0.96 (0.93-0.99; P=0.0027) ↓ 4%; (+1) portion fruits RR: 0.93 (0.89-0.96; P<0.0001); ↓ 7% Vegetable intake and CHD risk was heterogeneous (P=0.0043), more marked for CVD mortality RR: 0.74 (0.75-0.84, P<0.0001) Fatal and nonfatal MI RR: 0.95 (0.92-0.99, P=0.0058) | NA |
| Zhang et al30 | 2011 | Cohort study | 134,796 individuals 3442 deaths in women and 1951 deaths in men | Total and cardiovascular mortality | Validated FFQ | Quintile 1 (median-133g/d) vs. quintile 5 (median-545 g/d) for FVs intake: CVD HR: 0.78 (0.71-0.85; P<0.0001 for trend) for cruciferous vegetables HR: 0.84 (0.69-1.00; P=0.03) for total vegetables HR: 0.83 (0.76-0.92; P<0.0001 for trend) for total fruit intake | Age, education, occupation, family income, cigarette smoking, alcohol consumption, BMI, amount of regular exercise, multivitamin supplement use, intakes of total energy and saturated fat, menopausal status and hormone therapy use (for women only), and history of CHD, stroke, hypertension, or diabetes |
| Gupta et al31 | 2012 | Jaipur Heart Watch-5 | 739 individuals | Cardiovascular risk | Random sampling using house-to- house survey | Low FVs (<3 servings/day) 70 and 76% prevalence of CVD risk actors in men and women respectively | Age- and sex-adjusted |
| Shridhar et al32 | 2014 | The Indian Migration Study | 6555 individuals | Cardiovascular risk | Validated semi- quantitative- FFQ | Vegetarians vs. non-vegetarians: Total cholesterol: β - 0.1 (0.03-0.2; P=0.006) Triglyceride: β - 0.05 (0.007-0.01; P=0.02) | Age, sex, SLI, BMI, tobacco, alcohol, site, migration status, energy, physical activity and SibPair |
| LDL - cholesterol: β - 0.06 (0.050-0.1; P=0.03) HDL - Cholesterol: β - 0.01 (0.003-0.03) SBP: β - 0.9 (−0.08-1.9) DBP: β - 0.7 (0.07-1.2; P=0.02) FBS: β - 0.07 (−0.01-0.2) | |||||||
| Leenders et al33 | 2014 | EPIC and Nutrition study | >450,000 participants | Mortality | Country- specific dietary questionnaires | Highest (569 g/d) vs. lowest (249 g/d) circulatory deaths HR - 0.85 (0.770.93) | |
| Okuda et al34 | 2015 | NIPPON DATA80 prospective study | 9112 participants | CVD, stroke and CHD | 3-day weighing dietary records | Highest (290 g/1000 cal) vs. lowest quartile (130 g/1000 cal) of total FVs intake total CVD HR: 0.74 (0.61-0.91; 0.004; 0.003) Stroke HR : 0.80 (0.59-1.09; 0.105; 0.036) CHD HR: 0.57 (0.37-0.87; 0.010; 0.109) | Adjusted for age, sex, BMI, smoking habit, drinking habit, sodium intake, intakes of meat, fish and shellfish, milk and dairy products and soybeans and legumes |
| Nguyen et al35 | 2016 | Cohort study | 150,969 individuals | All-cause mortality | Validated FFQ | Highest vs. lowest Quartile: FVs combined HR: 0.90 (0.84-0.97; P for trend 0.002) Fruit intake HR: 0.83 (0.74-0.93; P for trend 0.003) Vegetable intake HR: 0.98-0.90; P for trend 1.06) | Age (categorical), sex, education level, marital status, location of residence, socio-economic status, smoking status, physical activity categories, multi-vitamin use, processed meat consumption, diabetes, and BMI |
| Aune et al36 | 2017 | Systematic review and dose-response meta-analysis | 95 studies | Cardiovascular risk | Literature searches (PubMed and Embase) | About 200 g/day FVs RR: 0.92 (0.90-0.95) for CHD; RR: 0.84 (0.76-0.92) for stroke; RR: 0.92 (95% CI: 0.90-0.95) for CVD Inverse associations were observed between the intake of apples and pears, citrus fruits, GLVs, CVs, salads and CVD and all-cause mortality | NA |
| Miller et al37 | 2017 | Prospective cohort study | 135,335 participants from 18 countries | CVD and death | Country- specific FFQ | Fruits (<3 servings/wk vs. >3 servings/day) CVD mortality HR: 0·83 (0·65-1·06; P for trend=0·0458); All-cause mortality HR: 0·81 (0·72-0·93; P for trend <0.0001) Vegetables (<1 serving vs. >2 servings/day) Major CVD events HR: 0·71 (0·58-0·87; P for trend=0.0056) hIGH FVs and legumes intake together was associated with only lower cardiovascular and total mortality | For fruits confounders adjusted include age, sex, centre (random effect), energy intake, current smoker, diabetes, urban or rural location, physical activity, education level and tertiles of white meat, red meat, and intake of breads, cereals, and vegetables. For vegetables confounders adjusted include age, sex, and centre (random effect) |
| Joshipura et al38 | 1999 | Prospective cohort study | 75,596 women and 38,683 men | Stroke | Semi quantitative FFQ | Highest vs. Lowest quintile: FVs RR: 0.69 (0.52-0.92) Cruciferous vegetables, +1 serving RR: 0.68 (0.49-0.94) GLVs RR: 0.79 (0.62-0.99) citrus fruit+juice RR: 0.81 (0.68-0.96) Citrus fruit juice RR: 0.75 (0.61-0.93) 6% reduction in stroke for (1+) serving of FVs RR: 0.94; (0.90-0.99; P for trend=0.01) | |
| Sauvaget et al39 | 2003 | Lifespan study | 40,349 Japanese men and women 1926 Stroke events | Stroke | Food- frequency questionnaires | Daily vs. lack of daily intake. Green yellow vegetables: Men HR: 0.77 (0.62-0.95; P=0.01); Women HR: 0.81 (0.68-0.96; P=0.012); 26% ↓ Fruit: Men HR: 0.65 (0.53-0.80; P<0.0001) Women HR: 0.75 (0.64-0.88; P<0.0001) 35% men and 25% women ↓ | Age-stratified, and adjusted for radiation dose, city, BMI, smoking status, alcohol habits, education level, medical history of hypertension, myocardial infarction, diabetes, and consumption of animal products (egg, dairy, fish) |
| Johnsen et al40 | 2003 | Prospective study | 54,506 men and women 266 cases | Stroke | Semi- quantitative FFQ | Highest vs. lowest quintile (673 vs. 147 g/d): FVs RR: 0.72 (0.47-1.12, P for trend=0.04) Fruits RR: 0.60 (0.38-0.95; P for trend=0.02) | Sex, total energy intake, smoking status, systolic blood pressure, diastolic blood pressure, total serum cholesterol, history of diabetes, BMI, alcohol intake, intake of red meat, intake of n-3 polyunsaturated fatty acids, physical activity, and education |
| Dauchet et al41 | 2005 | Meta-analysis of cohort studies | 7 studies; 232049 individuals and 2955 events | Stroke | Literature searches | (+1) portion fruit RR: 0.89 (0.85 to 0.93) ↓ 11%; (+1) portion FVs RR: 0.95 (0.92 to 0.97)↓ 5%; (+1) portion vegetable RR: 0.97 (0.92 to 1.02) ↓ 3% | NA |
| He et al42 | 2006 | Meta-analysis of cohort studies | 8 studies; 257,551 individuals and 4917 events | Stroke | Literature searches | 3-5 portions vs. >5 portions Fruits RR: 0·89 (0·82-0·98) vs. 0·74 (0·66-0·79) Vegetables RR: 0·93 (0·82-1·06) vs. 0·81 (0·72-0·90) | NA |
| Oude Griep et al43 | 2011 | Population- based cohort study | 20,069 participants | Stroke | Food- frequency questionnaires | Highest vs. lowest quartile: Total FVs (475 vs. 241g/d): HR-0.66 (0.45-0.99) Raw FVs (>262 vs. <92) HR: 0.70; 95% CI: 0.47-1.04) for CHD; HR: 0.70 (0.47-1.03) for stroke Deep orange vegetables: 0.74 (0.55-1.00) for CHD White FVs: 0.48 (0.29-0.77) for stroke | Age, gender, alcohol, energy intake, smoking, educational level, dietary supplement use, BMI, intake of fish, whole grain foods and processed meat |
| Sharma et al44 | 2013 | Cohort study | >215,000 individuals | Stroke | Validated FFQ | ↑ vegetable RR: 0.60 (CI: 0.36-0.99) ↓ risk 40% in African women; ↑Fruit RR: 0.43 (0.22-0.85)↓ risk 57% in Japanese American women | Adjusted for ethnicity, time on study, years of education, energy intake, smoking, BMI, physical activity, history of diabetes, and alcohol intake. The models for women were additionally adjusted for history of hormone replacement therapy |
| Larsson et al45 | 2013 | Prospective study | 74961 individuals 4089 cases | Stroke | Food- frequency questionnaires | Highest vs. lowest Total FVs RR: 0.87 (0.78-0.97; P for trend=0.01) | Adjusted for age, sex, smoking status and pack-years of smoking, education, |
| Apple and pears RR: 0.89 (0.80-0.98; P for trend=0.02) GLV RR: 0.92 (0.81-1.04; P for trend=0.03) | BMI, total physical activity, aspirin use, history of hypertension, diabetes, family history of myocardial infarction, and intakes of total energy, alcohol, coffee, fresh red meat, processed meat, and fish. Total fruit and total vegetable consumption was mutually adjusted by including both variables in the same multivariable model | ||||||
| Wang et al46 | 2014 | Meta-analysis of cohort studies | 16 studies; 833,234 individuals | Cardiovascular risk | Literature searches | (+1) portion FVs HR: 0.96 (0.92-0.99; P=0.001); (+1) portion Fruits HR: 0.95 (0.91-1.00; P=0.002); (+1) portion. Vegetable HR: 0.96 (0.93-0.99; P=0.006) | |
| Alonso et al47 | 2004 | SUN study | 4393 individuals | Blood pressure | Food- frequency questionnaires | Highest vs. lowest quintile: Prevalence of undiagnosed hypertension (OR) combined FVs, OR: 0·23 (0·10-0·55; P for trend 0·001) Vegetables OR: 0·58 (0·36-0·91; P for trend 0·01) Fruits OR: 0·68 (0·43-1·09; P for trend 0·10) | Adjusted for age, sex, BMI, energy-adjusted alcohol consumption, Na consumption, hypercholesterolaemia and physical activity during leisure time |
| Chan et al48 | 2014 | INTERMAP study | 2195 individuals | Blood pressure | Four standardized multi-pass 24 h dietary recalls and eight BP measurements | Average systolic blood pressure difference: Raw vegetable (68 g/1000 cal): −1.3 mm Hg (−2.4-0.2; P=0.02) Cooked vegetable (92 g/1000cal): −0.9 mm Hg (−2.0-0.2; P=0.1) | Adjusted for BMI age, gender, sample, education, physical activity, smoking status, history of CVD or diabetes mellitus, family history of high BP, use of special diet, use of dietary supplement, urinary sodium, and alcohol, polyunsaturated fatty acids, saturated fatty acids, and cholesterol, total fruit |
| Li et al49 | 2016 | Review article | 25 studies with 334,468 individuals; 41,713 events | Hypertension | Literature search | Highest vs. lowest consumption (RR): Combined FVs RR: 0.81 (0.74-0.89; P heterogeneity=0.000); Fruits RR: 0.73 (0.62-0.86; P heterogeneity=0.002); Vegetable RR: 0.97 (0.91-1.02) Significantly inverse association between fruit consumption and hypertension risk was found in studies carried out in Asia RR: 0.70; (0.61-0.79; P heterogeneity=0.000) | NA |
FVs, fruits and vegetables; RR, response rate; CI, confidence interval; GLVs, green leafy vegetables; BMI, body mass index; CHD, coronary heart disease; CVD, cardiovascular disease; KIHD, Kuopio Ischaemic Heart Disease Risk Factor; LDL, low-density lipoprotein; MI, myocardial infraction; IHD, ischaemic heart disease; SUN, Seguimiento Universidad de Navarra; NA, not available; FFQ, food frequency questionnaire; SLI, standard of living index; HR, hazard ratio; ↓, decrease; ↑, increase
In a pooled analysis, 2190 incident cases of CAD from the Health Professionals’ Follow Up Study and Nurses’ Health Study, the highest quintile of FVs intake (5.1 for men and 5.8 serving/day for women) had a lower risk ratio (RR) of CAD 0.80 and a four per cent reduction was observed for one extra serving of FVs (P for trend=0.01). Green leafy vegetables (GLVs) and citrus fruits (CFs) accounted for the protective effect21. In Physicians’ Health Study, the role of aspirin and beta-carotene was assessed in a randomized trial, for primary prevention of CVD among male doctors, considering vegetables as a continuous variable, an RR of 0.83 was recorded, the protection being more evident in men with BMI ≥25kg/m2 comparing highest and lowest intake (>2.5 vs. <1 servings/day)22.
Prospective cohorts, metabolic and intervention studies from 147 original publications concerning diet and CHD strongly suggest that apart from quantity and quality of fat and protein in diets, plenty of colourful FVs rich in phytomicronutrients/antioxidants will offer protection and prevent CVD50. In the first National Health survey of US, after 19 years an inverse association was documented with FVs intake and CVD. Higher intake of FVs (≥3 vs. <1 times/day), a lower stroke incidence and reduction in mortality due to stroke, ischaemic heart disease (IHD), CVD and total mortality were recorded23. In the same group, dietary intake of folate protected against the incidence of stroke and CVD24.
It has been documented that plant-based foods such as FVs, nuts and whole grains decrease the risk of CVD and strokes. The antioxidants in the various types of FVs and a prudent dietary pattern may be the right prescription for lifestyle-related disorders51. In Kuopio Ischaemic Heart Disease Risk Factor study in Finland mean higher intake (408 g/day) of fruits, berries and vegetables, jams, juices and nectars was associated with lower risk of mortality (total, non-CVD and CVD)25.
The INTERHEART study recorded several risk factors of acute myocardial infarction (MI) in 52 countries. For daily consumption of FVs, an odds ratio 0.70 (30% protection) and in those who did not consume FVs daily, population attributable risk factor was 13.7 per cent. The results were significant in both men and women in adjusted models26. A case-control study of acute MI in India indicated a dose-dependent inverse association between consumption of vegetables and IHD risk which was stronger for GLVs intake. In a multivariate analysis, the median intake of 3.5 servings/week vs. 0.5 servings/week of GLVs had a 67 per cent lower risk of IHD27.
In an exhaustive analysis in relation to risk of CVD and DM protective effect of FVs was observed52. The author has quoted previous case-control, prospective and country-specific information documenting beneficial effects of FVs intake both for stroke and CAD, though in some due to inadequate sample size, the results tended towards significance particularly after adjustments. However, the conclusions are that larger sample size, high quality (high power) prospective studies are essential on the types of FVs to detect better association and causation.
Cardiovascular risk factors such as obesity, hypertension, fasting plasma glucose and dyslipidaemia were explored in a cross-sectional study in Chennai28. When confounding factors were adjusted, the highest quartile of FVs intake (418 g/day) showed significant inverse association with systolic blood pressure; BMI, waist circumference, total and low-density lipoprotein (LDL) cholesterol concentration when compared with the lowest quartile (141 g/day). A higher consumption explained 48 per cent protective effect against the well-known risks of CVD28.
A meta-analysis using quantitative approaches29 assessed the extent of the relation between FVs consumption and CAD. In all nine independent studies, 5007 events occurred between 5 and 19 yr. The results demonstrated that for one additional portion/day of FVs protective effect for CHD varied between 21 and three per cent and for fruits an increment of one portion/day varied from 19 to five per cent. For one extra portion of FVs/day, the risk of CHD reduced by four per cent for vegetables and seven per cent for fruits. In Chinese adults from Shanghai Women's Health Study and Men's health study identified 3442 and 1950 deaths in women and men, respectively in 10.2 yr. Overall FVs intake (P<0.03) was inversely related with risk of deaths due to CVD with a dose-dependent effect for cruciferous vegetables (CV) (P<0.0001)30.
In Jaipur heart watch study in India31 in an urban middle-class community, 68.7 per cent had low FVs intake, <3 helpings/day in addition to usual risk factors. In univariate analysis, low FVs was a determining factor for metabolic syndrome. The Indian migration study32 assessed the vegetarian diets and risk of CVD, in individuals who migrated to the urban area, their rural counterparts and permanent urban residents, from four regions and 18 States of India. The mean age was 40.9 yr, of which one-third were vegetarians, better educated, less likely to smoke and drink alcohol. Vegetarians had lower cardiometabolic risk factors including fasting glucose. The authors concluded the relative magnitude of these benefits was small from a clinical perspective. In the European Prospective Investigation into Cancer and Nutrition (EPIC) study33, 13 yr hazard ratios (HRs) indicated that individuals who had more than 569 g/day of FVs had lower death risk from circulatory, respiratory and digestive disorders as compared to those consuming 249 g/day. Inverse associations were observed with consumption of vegetables in the raw form than cooked varieties with no association reported for fruit intake33. A 24 yr study in Japan also elicited a 25 per cent reduction in total CVD mortality with highest intake (median intake 290 g/1000 kcal) of FVs34.
Prospective cohorts study in Australia recorded that a higher consumption of FVs (≥7 servings/day) together accounted for 10 per cent reduced deaths due to all causes. Both raw and cooked vegetables also reduced mortality in minimally adjusted models35. The strength and dose-response effects were assessed in a systematic review and meta-analysis for CVD, cancer and total mortality36. The summary of results demonstrated reduced risk of CVD (CHD and stroke) and mortality due to all-causes were observed on an intake of 800 g/day for FVs combined. Premature deaths estimated were 5.6 million for <500 g and 7.8 million for <800 g/day. Apples/pears, CFs, GLVs salads and CVs were inversely related with CVD and mortality36.
A prospective urban-rural epidemiological study (PURE)37 was conducted in 18 countries in seven geographical regions. The populations at baseline were without CVD. In this 10 years study, the impact of various food groups on the clinical endpoints was reported (median follow up of 7.4 yr). One serving was defined as 125 g of FVs. Higher fruits intake (age and sex adjusted) reduced the risk of major CVD, stroke, cardiovascular, non-cardiovascular and total deaths. However, vegetable intake was inversely associated with only cardiovascular, non-cardiovascular and total mortality, while in adjusted models no significant association was seen in most geographical regions. The trend towards benefit for CVD mortality was also reported. However, fruit, vegetables and legumes consumption considered together were inversely related only to non-cardiovascular and total mortality37.
Strokes
Strokes are as common as CAD with serious outcomes and several investigators have shown an inverse association of FVs intake with the disease and its outcome. An investigation among men with ischaemic stroke patients, comparing highest quintile of FVs intake (median 5.1 and 5.8 servings/day in men and women, respectively) with the lowest quintile (median 2.6 and 2.9 servings/day in men and women respectively) observed 31 per cent risk reduction38. An additional serving of FVs per day elicited six per cent lower risk of ischaemic stroke. The protective effect was attributed to CVs, GLVs, CF and the juice.
A prospective cohort study in Japanese men and women followed up for 18 yr, 1926 deaths from all types of stroke were registered. More frequent consumption of green-yellow vegetables and fruits reduced the risk of death (32% in men and 30% in women) from stroke. Regular fruit intake daily was associated with a significant 35 per cent reduction in all types of strokes risk in men and a 25 per cent reduction in women. The association was strong for both types of stroke39.
In Denmark, cancer and health prospective study, 266 cases of hospitalized ischaemic strokes were analyzed. After adjustments for potential confounders, persons in the highest quintile of FVs intake (median consumption 673 g/day), 28 per cent protection was noted compared to persons in the bottom quintile intake (median-147g/day; P for trend=0.02). The protection was higher for fruits (40%-P for trend=0.02), the risk being significant for CF in unadjusted model (P<0.01)40.
In a meta-analysis of seven cohort studies, five from the US, one each from Europe and Japan investigated the intake of FVs in relation to stroke. A total of 2955 stroke event occurred within 3-20 yr. The results showed the risk reduction in stroke as 11 per cent and for each extra portion of fruits a five per cent and for one combined FVs intake a three per cent reduction was documented. A linear relationship was observed between the intake of FVs and strokes suggesting dose response effects41. Another meta-analysis of 4917 stroke events was performed during 13 yr follow up. Comparing persons with <3 servings of FVs compared to that of >3-5 servings/day an RR of 0.89 and with >5 servings/day an RR of 0.74 were observed42. Diets with plenty of FVs, whole grains, fibre from cereals, folate and fatty fish, similar to Mediterranean dietary patterns are likely to reduce stroke risk53.
Processed and raw fruits and vegetables consumption and protection from stroke were assessed in a population-based cohort study in the Netherlands43. In 233 newly diagnosed strokes cases, HR for total, ischaemic and haemorrhagic stroke were calculated for a mean follow up of 10.3 yr. Strokes reduced by 30 per cent (HR): 0.70 in those with high intake of raw FVs (262 g/day) compared with low intakes (92 g/day; P for trend=0.07). Processed FVs was not related probably due to loss of heat sensitive nutrients and non-nutrients.
DALYs due to the effects of 67 independent risk factors and clusters for 21 regions over a period of 20 yr (1990-2010) were calculated. Low fruits and high sodium intake combined with other dietary risk factors and physical inactivity accounted for 10 per cent (UI 9·2-10·8) of global DALYs. Globally, shifts in DALYs and current risks varied across regions. The minimum risk for IHD, different forms of strokes and cancers at several sites with fruits was for a consumption of 300±30 g/day and for vegetables 125±12.5 g/day. DALYs attributed to diets with low fruits and vegetables were 30 and 12 per cent, respectively. The % increase in fruits and vegetables rank order was 29 and 22 per cent for FVs respectively from 199054.
The association between food groups and stroke mortality was examined in five ethnic minorities groups in the US between 1993 and 1996. Total deaths due to stroke were 860. A significant risk reduction in fatal stroke with high vegetable intake was seen in African women (40%), while in Japanese American women high fruit intake reduced the risk of stroke by 57 per cent, while in men no impact was observed44. In a prospective study of 4089 with stroke incidences, in 10.2 yr45 observations indicated 13 per cent stroke reduction (P for trend=0.01) in non-hypertensives. Consumption of apples, pears and GLVs was inversely associated with stroke.
A total of 16 prospective cohort studies in a meta-analysis quantified the dose-response relation between FVs consumption and deaths due to CVD, cancer and all-cause mortality45. Confounding factors were adjusted in most cohorts. The data supported the current recommendation for 400 g/day of FVs intake46. The average risk reduction for CVD mortality was four per cent for each additional serving of FVs, while fruits alone reduced mortality by five per cent and vegetables by four per cent.
Hypertension
Hypertension is a risk factor for CVD and strokes. It is well known that DASH diet (dietary approaches to stop hypertension) is not only low in total fat, saturated fat (low in dairy fat) and sodium but is rich in FVs55 and reduces blood pressure. FVs are full of vitamins, minerals, fibre and potassium, which help to balance out the negative effects of salt. A project in Spain, in age- and sex-adjusted models, documented an inverse linear relationship for FVs intake and prevalence of undiagnosed hypertension47. The adjusted risk for undiagnosed hypertension (upper vs. lowest quintile for intakes) was 42 and 32 per cent lower for vegetable (957 vs. 240 g/day) and (726 vs. 114 g/day) fruits, respectively. A high FVs intake in Mediterranean population was inversely associated with BP levels despite high fat in the diet47 and in a meta-analysis Mediterranean diets (MD) with high FVs intake had similar results56.
In the INTERMAP (International Population Study on Macronutrients and BP) study48 both raw (68 g/1000 calories) and cooked (92 g/1000 calories) vegetables, in multivariate-adjusted models showed a significant reduction in systolic and diastolic blood pressures. Raw carrot, cooked peas and celery, tomatoes and scallions in both forms were significantly inversely related to BP. A meta-analysis of 25 studies (2 from the US, 13 from Asia 5 each from Europe and Africa) in hypertensives49 comparing the highest and lowest intake the pooled RR for hypertension was 0.81 for FVs, 0.73 for fruit and 0.97 for vegetables.
The protective effect of apples which contains fibre, polyphenols, vitamins C, E and potassium, on CVD risk, risk for total and cancer mortality, aortic calcification and forearm blood flow responses has been documented57. Apples also reduced cholesterol due to pectin, but the juice had no effect, probably due to fructose. The synergistic effects of polyphenols and fibre modify risk factors for CVD.
CVDs are primary cause of death and disability in India which occur a decade earlier both in urban and rural areas and has serious economic impacts58. The challenge ahead is enormous, and it would be best to invest in enhancing FVs intake for protective effect.
Diabetes & obesity
Globally, diabetes is the fastest growing disease affecting over 451 million people and resulting in >5 million deaths. Global data suggested that approximately 673 billion dollars were spent for treating diabetes during 2015-201659. Recent ICMR-INDIAB estimates 7·3 per cent prevalence of diabetes across 15 States of India60. Diabetes not only enhances the risk for CVD but is an important cause of morbidity and mortality61. Obesity is another independent risk factor contributing to chronic diseases such as type 2 diabetes. According to Global nutrition report (2017), two billion adults are overweight or obese and 16 per cent of men and 22 per cent of women in India are overweight62.
The ICMR-INDIAB (India Diabetes Study)- study reported the prevalence of generalized and abdominal obesity as 21 and 24.8 per cent, respectively while together prevalence was 28.6 per cent (199 million people) in India63. ‘Diabesity’ is a new medical term linking obesity with diabetes and refers to increased insulin resistance64. Altered lifestyles particularly dietary transitions (high intake of calorie-dense refined and fatty foods coupled with low intake of whole grains, FVs) and sedentary behaviours lead to the growing epidemic of obesity and DM65.
FVs are known to promote satiety and reduce energy intake. However, not much is known about the role of different elements of FVs responsible for regulation of hunger, satiety and body weight66. A few studies and meta-analysis have shown that increased intake of FVs may aid in the prevention of obesity and decrease body weight over time (Table II).
Table II.
Effect of fruits and vegetables on obesity and diabetes-summary
| Author | Year | Study | Study participants (n) | Outcome variable | Assessment tool | Major findings | Confounders adjusted |
|---|---|---|---|---|---|---|---|
| He et al67 | 2004 | Nurse's Health Study, Prospective cohort | 74,063 Women | Obesity and weight gain | Validated FFQ | Increased (3.99) vs. decreased (−2.36) FVs intake obesity RR: 0.76 (0.69-0.86); P for trend <0.0001 weight gain RR: 0.72 (0.55-0.93); P for trend=0.01 Increased (1.86) vs. decreased (−1.27) Fruit intake Obesity RR: 0.76 (0.68-0.84); P for trend=0.0007 weight gain RR: 0.73 (0.56-0.95) P for trend=0.03 Increased (2.80) vs. decreased (−1.82) Vegetable intake obesity RR: 0.84 (0.75-0.93); P for trend=0.0002; weight gain RR: 0.76 (0.59-0.99); P for trend=0.03 | Age, year of follow up, change in physical activity, change in cigarette smoking status, changes in alcohol consumption and caffeine intake, change in use of hormone replacement therapy, and changes in energy-adjusted intakes of saturated fat, polyunsaturated fat, monounsaturated fat, trans-unsaturated fatty acid, protein, and total energy and baseline BMI |
| Vergnaud et al68 | 2013 | EPIC - cohort | 373803 participants | Weight change | Country- specific validated questionnaires | Weight change in men for 100g increase in FVs β: −5 (−8-−1; P=0.006) Total vegetables β: −10 (−17-−3; P=0.007) Weight change was drastic among men who quit smoking Vegetables β:-32 (−58-−6; P=0.02); Fruits β: −26 (−46-−7; P=0.007) Fruits were found to be protective among women β: −6 (−11-−1; P=0.009) | Age, indicator of vegetable (or fruit) consumption, educational level, physical activity level, change in smoking status, BMI at baseline, follow up time, total energy intake, and energy coming from alcohol and fruit (for vegetable analysis) or vegetable (for fruit analysis) intake |
| Schwingshackl et al69 | 2015 | Meta- analysis | 563277 participants | Anthropometric measures | Literature search | Highest intake of fruits (per 100-g increment): ↓ in weight β: −13.68 g/year (−22.97-−4.40; P=0.001) | NA |
| Highest intake of FVs: ↓ adiposity, OR: 0.91 (0.84-−0.99) Highest intake of Fruits: ↓ adiposity, OR: 0.83 (0.71-0.99) Highest intake of vegetables: ↓ adiposity, OR: 0.83 (0.70-0.99) | |||||||
| Rautiainen et al70 | 2015 | Women's Health Study | 18,146, women | Weight change and risk of overweight and obesity | FFQ | Highest (>3.1 serving/day) vs. lowest quintile (<3.1 serving/day) of fruit intake HR overweight/obesity: 0.87 (0.80-0.94; P-trend: 0.01) Highest (≥1.3 serving/day) vs. lowest quintile (<0.2 serving/day) for citrus fruit intake 0.84 (0.78-0.90); P-trend: <0.0001 No association with total fruits and vegetables, vegetables and dietary fibre was observed | Age, randomization treatment assignment, physical activity, history of hypercholesterolaemia or hypertension, smoking status, post-menopausal status, post-menopausal hormone use, alcohol use, multivitamin use, and energy intake |
| Liu et al71 | 2004 | Prospective cohort study | 39,876 women | Diabetes | Semi- quantitative FFQ | Q1 (0.14 serving/day) vs. Q5 (1.42 serving/day) GLV RR for T2DM: 0.96 (0.81-1.13) Q1 (0.13 serving/day) vs. Q5 (1 serving/d) CV RR for T2DM: 0.95 (0.80-1.12) Q1 (0.07 serving/day) vs. Q5 (1 serving/d) dark yellow vegetables RR for T2DM: 0.81 (0.67-0.98) | Age, smoking, total calories, alcohol use, BMI, exercise, history of hypertension, history of high cholesterol, and family history of diabetes |
| Villegas et al72 | 2008 | Prospective cohort study | 64,191 women | Diabetes | Validated FFQ | Q1 (121.5 g/day) vs. Q5 (428 g/day) vegetable | Age, daily energy intake, meat intake, BMI, WHR, smoking, |
| HR: 0.72 (95% CI: 0.61-0.85, P for trend <0.0001) Q1 (5 g/day) vs. Q5 (45.2 g/day) CVs HR: 0.72 (0.61-0.83, P for trend<0.001) Q1 (28 g/day) vs. Q5 (136.1 g/day) GLVs HR: 0.82 (0.71-0.95, P for trend <0.001) Q1 (0.04 g/day) vs. Q5 (17.3 g/day) yellow vegetables HR: 0.55 (0.47-0.64, P for trend <0.001) Q1 (2.2 g/day) vs. Q5 (17.9 g/day) Allium HR: 0.69 (0.59-0.81, P for trend <0.001) Q1 (40.7 g/day) vs. Q5 (181 g/day) other vegetables HR: 0.76 (0.64-0.89, P for trend <0.01) | alcohol consumption, physical activity, income level, education level, occupational status, and hypertension | ||||||
| Bazzano et al73 | 2008 | Nurse's Health Study, Prospective cohort | 71,346 women | Diabetes | Semi- quantitative FFQ | HR for diabetes Q1 (0.46) vs. Q5 (2.64) Fruits: 0.90 (0.80-1.00; P for trend <0.008) +3 servings of fruits: 0.82 (0.72-0.94) Q1 (0.25) vs. Q5 (1.48) GLVs: 0.90 (0.82-1.00; P for trend <0.010) +1 serving of GLVs: 0.91 (0.84-0.98) | BMI, physical activity, family history of diabetes, post-menopausal hormone use, alcohol use, smoking, and total energy intake, whole grains, nuts, processed meats, coffee, potatoes, and sugar-sweetened soft drinks |
| Cooper et al74 | 2012 | CASE-cohort study | 3704 participants | Diabetes | 7-day prospective food diaries | HR for incident diabetes. Quantity: T1 (2.1) vs. T3 (5.7) portions/day: FVs: HR 0.79 (0.62-1.00; P for trend=0.04) | Sex, BMI, waist circumference, education level, Townsend Deprivation Index, occupational social class, smoking status, physical |
| T1 (1.1) vs. T3 (2.6) portions/day: Vegetables: 0.76 (0.60-0.97; P for trend=0.03) Variety: T1 (8) vs. T3 (16.3) items/wk: FVs: HR 0.61 (0.48-0.78; P for trend <0.001) T1 (5.5) vs. T3 (11.4) items/wk: Vegetables: 0.77 (0.61-0.98; P for trend=0.03) T1 (2) vs. T3 (6.9) items/wk: Fruits: 0.70 (0.53-0.91; P for trend=0.002) | activity, family history of diabetes, energy intake, and season, fruit variety for fruit quantity, vegetable variety for vegetable quantity, or combined FVs variety for combined FVs quantity | ||||||
| Wang et al75 | 2016 | Meta-analysis | 22 studies | Diabetes | Literature search | Highest vs. lowest intake Total fruits RR: 0.91 (0.87-0.96) Berries RR: 0.75 (0.66-0.84) GLVs RR: 0.87 (0.81-0.93) Yellow vegetables RR: 0.72 (0.57-0.90) CVs: 0.82 (CI 0.67-0.99) Fruit fibre RR: 0.93 (0.88-0.99) Vegetable fibre RR: 0.87 (0.80-0.94)- in ≥10 yr follow up period | NA |
| Jia et al76 | 2016 | Meta- analysis | 306,723 participants | Diabetes | Literature search | Highest vs. lowest intake CVs RR=0.84 (0.73-0.96; P heterogeneity =0.09); Citrus fruits had no effects | NA |
| Mamluk et al77 | 2017 | *Consortium on health and ageing network of cohorts in Europe and the United States (CHANCES) | 422,538 participants | Diabetes | FFQ and records of intake over seven or 14 days | OR for T2DM Highest (7.73) vs. lowest (0.82) intake (portions/day)-NIH AARP Study: Fruits: 0.95 (0.91-0.99; P=0.04) Highest (8.06) vs. lowest (0.65) | Age, sex, BMI, physical activity, energy intake, alcohol consumption, education and smoking |
| intake (portions/day)-GLVs: 0.87 (0.84-0.90; P for trend <0.01). No significant effect was noted in combined EPIC elderly and NIHAARP study as well as EPIC-elderly study individually | |||||||
| Du et al78 | 2017 | China Kadoorie Biobank study | 482,591 participants | Diabetes | FFQ | HR for Diabetes: Daily vs. non-consumers FVs: 0.88 (0.83-0.93; P<0.001) HR for macrovascular complications: FVs 0.87 (0.82-0.93; P<0.001) | Age at risk, sex, and region and were adjusted for education, income, alcohol intake, smoking, physical activity, survey season, BMI, family history of diabetes, and intakes of dairy products, meat, and preserved vegetables |
EPIC, European Prospective Investigation into Cancer and nutrition; FVs, fruits and vegetables; RR, response rate; CI, confidence interval; BMI, body mass index, GLVs, green leafy vegetables; NA: not available; FFQ, food frequency questionnaire; OR, odds ratio; NIH-AARP, National Institute of Health-American Association of Retired Persons; HR, hazard ratio; WHR, waist hip ratio; CV, cruciferous vegetables; T2DM, type 2 diabetes mellitus
In Nurses’ Health Study, risk of obesity in Women (74,063) was compared with respect to intake of FVs during 12 years follow up. The RR of becoming obese was reduced by 24 per cent on high intake (P-trend: <0.0001)67. The intake of FVs and weight change in participants aged 25 and 70 yr from the EPIC cohort indicted no changes in weight for five years (follow up). However, high fruit intake at baseline was negatively associated with weight gain among women and in men and women who discontinued smoking68.
A meta-analysis of 17 cohort studies assessed the consumption of FVs with respect to changes in anthropometry. Fruits but not vegetables, total FVs combined was associated with decrease in body weight and waist circumference. The highest combined category of total FVs elicited nine per cent and vegetable and fruits as discrete groups elicited 17 per cent (each) reduced risk of fat deposits69. The data from Women's Health Study70 showed that high ingestion of fruits at baseline was linked with reduced risk of becoming overweight and obese in women with normal BMI. However, total FVs, vegetables and dietary fibre were not associated with the long-term changes in body weight70.
Epidemiological and prospective cohort studies have shown an inverse association between intake of selected fruits, GLVs and risk of DM (Table II). High intake of green leafy and dark yellow vegetable was inversely associated with lower incidence of diabetes among overweight women while fruits had no effects71.
A prospective study among Chinese women reported an inverse association between highest quintile (428 g/day) of vegetable intake vs. lowest quintile (121.5 g/day) with 28 per cent reduction in the incidence of DM (P =0.01)72. The intake of different classes of vegetables including CV, GLVs, allium, tomatoes and other vegetables recorded a significant reduction in the incidence of DM. However, fruits had no significant association72. The Nurse's health study with 18 years follow up had the lowest risk of DM. With one serving increase in GLV intake, nine per cent reduction was observed73.
A prospective study examined the incidence of DM in relation to amount and variety of fruit, vegetables and combined FVs intake in men and women from the Norfolk component of the EPIC (EPIC-Norfolk) study. Both the quantity and variety of FVs and total FVs intake were independently protective for risk reduction of DM. After adjusting for potential confounders, the incidence of DM decreased by eight per cent for multiple varieties and quantity of FVs74.
The highest intake of total FVs and fruits elicited a greater risk reduction (25% for FVs and 28% for fruits alone) for type 2 DM (T2DM) in a meta-analysis of 23 prospective studies (1992-2014)75. Another meta-analysis of seven prospective studies explored the association of CVs and CFs on the incidence of T2DM and reported a 16 per cent reduction with CVs intake. No such association was evident with CFs76.
The association between T2DM and FVs intake using data from the National Institutes of Health-American Association of Retired Persons (NIH-AARP) study and the EPIC-elderly study recorded that pooled data had no effect of FVs diabetes risk reduction. However, the NIH-AARP study independently demonstrated reduced diabetes risk with fruit (5%) and GLVs (13%) in elderly77.
The China Kadoorie Biobank-seven-year prospective study among 0.5 million Chinese adults showed that fresh fruit consumption reduced the risk of diabetes including mortality and major vascular hospitalizations in known diabetes patients at baseline. Individuals without diabetes initially, who regularly consumed high amounts of fruits had a significant lower risk of developing diabetes as compared to non-consumers participants with known diabetes, higher fruit consumption was associated with lower risks, total mortality from all causes and macro-vascular complications78.
Higher intake of sugars is often associated with negative impacts of health including increase in body weight and risk of diabetes and CVD. On the contrary fruits rich in sugar elicit lower glycaemic response (GR) and are in general recommended as a part of healthy diet. This may be due to the cell wall and fiber content of fruits that may perhaps restrict absorption of sugar. Low GI fruits diets are associated with lower glycated haemoglobin (HbA1c), blood pressure and CHD risk79. A study from India made an attempt to evaluate the GR of mango against white bread as reference food, among Indians with DM. The findings showed that mango elicited lower GR than reference bread. This may be attributed to the high moisture content in mangoes80.
In general, fruits appear to be better for weight reduction while in addition to fruits, CV and GLVs were found to be protective for DM. Significant valid data from clinical trials are scarce. Well-designed intervention trial and large prospective studies are needed to assess the effectiveness of total and individual FVs for risk of obesity and T2DM.
Interventions
Food-based interventions are difficult to conduct and at best can measure only the intake. Very few clinical endpoints can be targeted. The DASH diet trial with high FVs, fish and low saturated fat and salt decreased blood pressure in hypertensives55. The Lyon heart study with dietary advice similar to DASH diet in MI patients following MD reduced cardiovascular morbidity within 12 months and extended survival after five years81.
In a randomized trial in a general population, the intervention group was advised to enhance FVs consumption. This group significantly enhanced their FVs intake by 1.4 serving and had greater increase in plasma concentrations of carotenes, phytonutrients, vitamins A, E and C than controls. Both systolic and diastolic blood pressure (SBP and DBP) reduced in intervention group82. The WHO83 in a review identified interventions and programmes promoting FVs intake worldwide among children in school settings, adults in general population, worksite, healthcare settings, low-income population, churches, supermarkets, other retail settings and individuals with CVD and cancer. A large number of interventions showed improvement in FVs intake post-intervention particularly in CVD and Cancer patients83.
In a study dose-response effects were seen with increasing servings of FVs for two months. Further, forearm blood flow responses enhanced by 6.2 per cent84. In a Cochrane review of 10 trials with one ongoing, provision of FVs in six trials, and advice to enhance the intake of FVs in four trials, directed at high-risk adults of CVD or healthy adults showed favourable effects on SBP (−3 mmHg) and LDL-cholesterol but not on DBP85. Variations were noted in types of FVs provided (one each of FVs) and advice for number of servings ranging from 2 to 9. The trials were too short (three months to one year) to impact clinical endpoints.
Consumption of FVs improved when habit-based intervention message through electronic media was delivered to undergraduates86. In a systematic review of trials promoting FVs among 1026 individuals, mean difference of 133 g of FVs between intervention and non-intervention group resulted in weight reduction of 0.68 kg (P=0.01)87. A systematic review of 55 trials on child feeding practices examined 11,108 participants. Small differences (4.3 g/day) were observed between those with interventions versus no interventions88.
An updated systematic review and meta-analysis highlighted the health effects of adherence to the MD which is rich in FVs. Increased adherence to MD showed significant reductions in overall mortality, both CVD and cancer incidence and mortality, and neurodegenerative diseases89.
Interventions with FVs and their implications particularly the clinical endpoints are difficult to interpret because of extended durations, fluctuating intakes, available varieties, permutations and combinations of bioactives/nutrients, their bioavailability and finally in vivo blood levels and their synergistic activity.
Mechanisms of action of fruits and vegetable
FVs through several mechanisms can modify risk of CVD, diabetes, cancer and obesity and other NCDs52,69,90,91,92,93. The various mechanisms of action of FVs are summarized in Table III.
Table III.
Mechanism of action for fruits and vegetables
| Nutrients | Mechanism of action |
|---|---|
| Fibre and low energy | Body weight and adiposity↓ Delayed gastric emptying ↓ Satiety through gut hormones ↑ Insulin sensitivity, ↓ insulin resistance and blood glucose ↓Blood lipids (total and LDL-cholesterol) |
| Polyphenols/bioactives, vitamins C, E, β-carotenes and selenium, manganese | ↓ Oxidant damage by scavenging oxygen radicals- anti-atherosclerotic Vasodilatation through nitric oxide synthase |
| Bioactives and vitamins | Anti-inflammatory/platelet aggregation ↓ Lipogenesis and↑lipolysis |
| Vitamin, folate, B6 | ↓ Homocysteine |
| Potassium, magnesium | Stabilizes heart rate and blood pressure Improves endothelial dysfunction |
| Phytonutrients | Microbiome is altered for better health Potentiates immune mechanisms Detoxification by modifying xenobiotic metabolizing enzymes |
LDL, low-density lipoprotein; ↓ decrease; ↑ increase
Source: Refs 52, 69, 90-93.
Barriers to consumption
It is a great challenge to encourage better lifestyles and promote FVs intake in the population. These are the best substitutes for high energy foods due to their volume and nutrient density. Knowledge, attitudes and practices survey and focus group discussions are the best way to judge the existing barriers for consumption of FVs94.
Attitudes
Individual's idiosyncrasies reflect food choices with little concern for nutritional/functional benefits95,96. IEC is a time-tested method to impart nutrition education. In addition, a favourable environment is essential for the community to practice what they have learnt97 (Fig. 4).
Fig. 4.
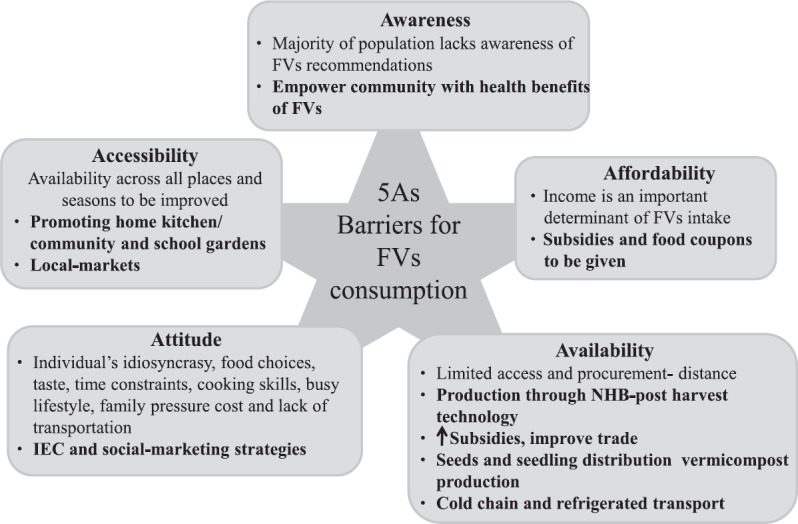
Barriers for fruits and vegetable consumption. FVs, fruits and vegetables; NHB, National Horticulture Board.Source: Refs 95-100.
Awareness
Changing food habits is difficult in the absence of overt adverse effects. Inculcating food habits from early life might influence the adult behaviours. Social marketing strategies have been used to enhance GLVs and fruits intake to overcome vitamin A deficiency using change agents in India98. It is always good to use the local administration and promote through the community particularly women, schools, worksites and deliver information, education and communicate for behavioural modifications.
Availability & accessibility
FVs must be made available throughout all places and seasons and at distances, which people can access easily. Promoting local production and periodic inputs from agricultural extension workers can enhance accessibility. In rural centres, donating land for growing FVs and giving illustrative fact sheets will be of immense benefit. Creating marketing channels, cold chain and refrigerated transport are essential for sustained production and distribution. The government of India has set up a National Horticulture Board (NHB), which has several schemes and subsidies, to cover production, primary processing, cold chain facility and distribution including expert consultancy facilities99. A recent review elaborates on marketing and production problems such as natural calamities, weather vagaries, demographic pressures, use of pesticides, demand for organic produce and migration that are linked to production12. Horticulture is economically productive, and there is scope for further strengthening trade-related preservation, processing and infrastructure strengthening.
Affordability
A study across 18 countries highlighted that affordability was the prime determinant of FVs intake (PURE)36. The qualitative method identified ‘that FVs were expensive and were a relatively intractable barrier’ for those with ‘inflexible food budget’100. In urban India, affordability is a strong barrier to FVs intake101. India being one of the largest producers of variety FVs, if the supply chain management is streamlined almost 25-30 per cent wastage can be avoided, improving affordability.
A recent survey conducted in India across four metros in 1001 individuals clearly brought out the impediments for consumption of FVs16. Lifestyle issues (52%) followed by seasonal availability (26%), higher cost and dislike (20%) were reported by majority of participants as inability to meet the WHO recommended intake.
Trade (domestic and international) can unmask unexploited potentials in developing or Asian countries to drive production, distribution and enhance availability and provide economic opportunity for farmers. Health sectors can be the advocates for policy inputs into horticulture initiatives. ‘Aid for Trade’102 by governments and donor agencies can invest in infrastructure, technical inputs to impact quality, production, processing, supply chain and export.
Policy initiatives
Policies should essentially promote and support dietary diversification with FVs. The availability of FVs has increased slightly in most countries but is still well below the recommended level both in developed and developing countries.
Chronic diseases needs priority attention from policymakers, health personnel/consumers and agriculturalists and industries to emphasize on natural foods that are both innately healthy and minimally processed. The overall dietary patterns and the food matrix determine the health outcome, and hence foods and food-based approaches, not nutrients should be the focus of attention. Energy intake and output and the quality of diet ultimately influence body weight, composition, metabolic health, microbiome and health and disease profiles in the community103.
In order to have an optimistic impact on chronic diseases and MN deficiencies, the Global Burden of Diseases Collaborative Network19 and global health risk factors4 can help policymakers to have a dedicated approach and achieve global health targets for the double burden of diseases. It is important to understand the risks to formulate policy and effective approaches and implement environment-specific strategies at national levels. The barriers for adequate intake have to be broken to enhance the consumption of FVs in all age groups. The Indian scenario, barriers, policy issues and the current mission mode approaches to enhance the consumer consumption have been highlighted104. Enhancing the production and consumption proactively in required amounts of FVs will prevent the disease from affecting the population and reduce healthcare expenditures and demands on health systems. The five As (attitude, awareness, availability, accessibility and affordability) require concerted efforts. High-risk individuals and the population at large need to be targeted through dietary guidelines and disease counselling and management. The strategies and actions are indicated in Table IV to promote healthy and mindful intakes in the community. The healthy eating pattern should be wide-ranging, steady, sustainable and economically viable in all segments of the population.
Table IV.
Policy initiatives (multi-sectoral, multi-pronged/multi-faceted and cohesive approaches in unison with stakeholders for common vision and objectives)
| National government | ||
|---|---|---|
| Strategies | Actions | |
| Advocacy for national policy, goals and programmes | Partnership with allied agencies (stakeholders) | |
| Promote surveys/research/IEC | Coordination between academy and university | |
| Harness support of horticulture/agriculture and PPP | Production, preservation, and processing, packaging/distribution/prevent onfarm losses | |
| Health and nutritional services | IEC, DG, skill development and mass media education | |
| Fiscal policies | Pricing and public distribution, food coupon and subsidies for FVs, incentives for farmers | |
| Urbanrural planning | Transport, farmers and rural markets, infrastructure for cold storage | |
| Food labels, laws and advertisement | To empower community, women in particular | |
| Create advisory council | Decisionmaking/create cohesive environment/advertisement | |
| Monitoring and surveillance | Human resources/financial support/measures of outcome | |
| Proper trade policies | For export facilities | |
| Civic bodies and private sectors | ||
| Civic bodies | Private sectors | |
| To promote IEC's in worksites, clubs, and community in general | Innovative food technology for healthy alternatives/avoid FVs wastage | |
| Help in skill development | Primary and secondary processing | |
| Bridgebetween government and private industries and community | Creating enabling environment from farm to fork | |
| School health programme, workplace interventions | Help the government and civic bodies through CSR | |
| Information, education and communication | Funding for educational programmes | |
Civic bodies, municipal corporations, municipality, panchayat, city councils; NGO, private associations; IEC, Information, education, communication; DG, dietary guidelines; CSR, corporate social responsibility; PPP, publicprivate partnerships; FVs, fruits and vegetables.
Source: Refs 20, 104-106
Healthcare professionals such as peripheral workers from diverse backgrounds especially in developing countries can serve as motivators at all levels. Public-private partnerships can create a healthy environment and healthy alternatives for consumption. Public health interventions should be tailored to the health needs of the population and address the socio-economic, cultural, environmental and behavioural determinants of food habits. The Alliance for Food and health (2017) has explicitly set out a multistakeholder approach for better health, in track with sustainable goals of UN particularly, ‘Good Health and Well-Being’105. The Government of India has initiated an NCD prevention strategy with several action-oriented programmes which includes both primary and secondary prevention covering all risk behaviours107.
Conclusions
This review described studies conducted to explore the health benefits of FVs, which in myriad ways impact deficiency and cardiometabolic problems. Nutrient approaches are currently replaced by food-based approaches. Literature is replete with evidence that FVs are the corner stones for enhancing the quality of diet to impact the twin burden of diseases particularly in developing countries. Plentiful FVs (half the plate) are promoted as healthy foods and as a viable sustainable solution. Raw vegetables appear to be better than cooked, and fruits better than fruit juices for health impacts. However, consensus on the optimal intake, which reduces chronic disease death and disability, is varying widely, including global estimates. FVs vary in their nutrients, bioactive and availability from a highly complex food matrix. Cultural practices and variety of cuisines may either augment or mitigate the beneficial role. Non-starchy vegetables, green and orange coloured vegetables, cruciferous variety, allium veggies, citrus and non-CFs may have pleotropic effects. Overall dietary patterns and choices are influenced by individual, socio-cultural and environmental factors. Although hedonistic attributes are important, availability/affordability particularly influence consumer choices. Barriers can be overcome by modern horticulture creativities, appropriate public health measures, their outreach and policies with cooperation from all stakeholders. Conscientious eating habits pave the way for healthy habits and wholesome life.
Acknowledgment
Authors thank Ms Sudha, Sr. Scientist, Madras Diabetes Research Foundation for her valuable suggestions, and acknowledge Ms Anjana Ramalingam and Ms Kalpana for helping in formatting the Tables and References.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1.Dietary guidelines for Indians: A manual. Hyderabad: NIN; 2011. National Institute of Nutrition, Indian Council of Medical Research. [Google Scholar]
- 2.Increasing fruit and vegetable consumption to reduce the risk of non-communicable diseases. e-Library of Evidence for Nutrition Actions (eLENA) Geneva: WHO; 2018. [accessed on June 5, 2018]. World Health Organization. Available from: https://www.who.int/elena/titles/fruit_vegetables_ncds/en/ [Google Scholar]
- 3.Krishnaswamy K. Newer roles of vegetables in the prevention and control of problems of over nutrition and chronic degenerative diseases. In: Nath P, Gaddagimath PB, Dutta OP, editors. Food security and vegetables - A global perspective. Banglore, India: Dr Prem Nath Agricultural Science Foundation; 2004. pp. 162–80. [Google Scholar]
- 4.Global Health Risks. Mortality and burden of disease attributable to selected major risks. Geneva: WHO; 2009. World Health Organization. [Google Scholar]
- 5.Investing in the future: A united call to action on vitamin and mineral deficiencies. Ottawa, Canada: Micronutrient Initiative; 2009. Micronutrient Initiative. [Google Scholar]
- 6.Muthayya S, Rah JH, Sugimoto JD, Roos FF, Kraemer K, Black RE, et al. The global hidden hunger indices and maps: An advocacy tool for action. PLoS One. 2013;8:e67860. doi: 10.1371/journal.pone.0067860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kotecha PV. Micronutrient malnutrition in India: Let us say “No” to it now. Indian J Community Med. 2008;33:9–10. doi: 10.4103/0970-0218.39235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nair MK, Augustine LF, Konapur A. Food-based interventions to modify diet quality and diversity to address multiple micronutrient deficiency. Front Public Health. 2015;3:277. doi: 10.3389/fpubh.2015.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Department of Agriculture. Composition of foods raw, processed, prepared. USDA National Nutrient Database for Standard Reference, Release 23. 2010 [Google Scholar]
- 10.Steele M, Weatherspoon D. Agricultural & Applied Economics Association Annual Meeting; 2016 July 31-August 2. Boston: Massachusetts; Demand for fruit and Vegetable Colors. (No. 235912) [Google Scholar]
- 11.National Horticultural Board. Horticultural statistics at a glance. Horticulture Statistics Division Department of Agriculture, Cooperation & Farmers Welfare. Ministry of Agriculture & Farmers Welfare, Government of India. 2017 [Google Scholar]
- 12.Chittora NA, Bisht V, Johar V. Marketing and production of fruits and vegetables in India. Int J Curr Microbiol App Sci. 2017;6:2896–907. [Google Scholar]
- 13.Hall JN, Moore S, Harper SB, Lynch JW. Global variability in fruit and vegetable consumption. Am J Prev Med. 2009;36:402–9. doi: 10.1016/j.amepre.2009.01.029. [DOI] [PubMed] [Google Scholar]
- 14.Nutritional intake in India, 2011-12. NSS, 68th Round. New Delhi: Government of India; 2014. National Sample Survey Office. Report No. 560. [Google Scholar]
- 15.Diet and nutritional status of rural population, prevalence of hypertension & diabetes among adults and infant & young child feeding practices - Report of third repeat survey. Hyderabad: National Institute of Nutrition; 2012. National Nutrition Monitoring Bureau. Technical report No. 26. [Google Scholar]
- 16.Mukherjee A, Dutta S, Goyal MT. New Delhi: Academic Foundation; 2016. India's phytonutrient report: A snapshot of fruits and vegetables consumption availability and implications for phytonutrient intake. [Google Scholar]
- 17.World Health Organization. Fact Sheet: Cardiovascular diseases (CVDs) 2017. May 17, [accessed on July 28, 2018]. Available from: http://www.who.int/news-room/fact-sheets/detail/cardiovasculardiseases-(cvds)
- 18.Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: Current epidemiology and future directions. Circulation. 2016;133:1605–20. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 19.Global burden of disease study 2016 (GBD 2016) results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME); 2017. [accessed on August 26, 2018]. Global Burden of Disease Collaborative Network. Available from: http://ghdx.healthdata.org/gbd-results-tool . [Google Scholar]
- 20.Krishnaswamy K, Vaidya R, Gayathri R, Sudha V. Diet and nutrition in the prevention of non-communicable diseases. Proc Indian Nat Sci Acad. 2016;82:1477–94. [Google Scholar]
- 21.Joshipura KJ, Hu FB, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, et al. The effect of fruit and vegetable intake on risk for coronary heart disease. Ann Intern Med. 2001;134:1106–14. doi: 10.7326/0003-4819-134-12-200106190-00010. [DOI] [PubMed] [Google Scholar]
- 22.Liu S, Lee IM, Ajani U, Cole SR, Buring JE, Manson JE, et al. Intake of vegetables rich in carotenoids and risk of coronary heart disease in men: The physicians’ health study. Int J Epidemiol. 2001;30:130–5. doi: 10.1093/ije/30.1.130. [DOI] [PubMed] [Google Scholar]
- 23.Bazzano LA, He J, Ogden LG, Loria CM, Vupputuri S, Myers L, et al. Fruit and vegetable intake and risk of cardiovascular disease in US adults: The first national health and nutrition examination survey epidemiologic follow-up study. Am J Clin Nutr. 2002;76:93–9. doi: 10.1093/ajcn/76.1.93. [DOI] [PubMed] [Google Scholar]
- 24.Bazzano LA, He J, Ogden LG, Loria C, Vupputuri S, Myers L, et al. Dietary intake of folate and risk of stroke in US men and women: NHANES I epidemiologic follow-up study. National Health and Nutrition Examination Survey. Stroke. 2002;33:1183–8. doi: 10.1161/01.str.0000014607.90464.88. [DOI] [PubMed] [Google Scholar]
- 25.Rissanen TH, Voutilainen S, Virtanen JK, Venho B, Vanharanta M, Mursu J, et al. Low intake of fruits, berries and vegetables is associated with excess mortality in men: The Kuopio Ischaemic Heart Disease Risk Factor (KIHD) study. J Nutr. 2003;133:199–204. doi: 10.1093/jn/133.1.199. [DOI] [PubMed] [Google Scholar]
- 26.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 27.Rastogi T, Reddy KS, Vaz M, Spiegelman D, Prabhakaran D, Willett WC, et al. Diet and risk of ischemic heart disease in India. Am J Clin Nutr. 2004;79:582–92. doi: 10.1093/ajcn/79.4.582. [DOI] [PubMed] [Google Scholar]
- 28.Radhika G, Sudha V, Mohan Sathya R, Ganesan A, Mohan V. Association of fruit and vegetable intake with cardiovascular risk factors in Urban South Indians. Br J Nutr. 2008;99:398–405. doi: 10.1017/S0007114507803965. [DOI] [PubMed] [Google Scholar]
- 29.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: A meta-analysis of cohort studies. J Nutr. 2006;136:2588–93. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X, Shu XO, Xiang YB, Yang G, Li H, Gao J, et al. Cruciferous vegetable consumption is associated with a reduced risk of total and cardiovascular disease mortality. Am J Clin Nutr. 2011;94:240–6. doi: 10.3945/ajcn.110.009340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gupta R, Sharma KK, Gupta A, Agrawal A, Mohan I, Gupta VP, et al. Persistent high prevalence of cardiovascular risk factors in the urban middle class in India: Jaipur heart watch-5. J Assoc Physicians India. 2012;60:11–6. [PubMed] [Google Scholar]
- 32.Shridhar K, Dhillon PK, Bowen L, Kinra S, Bharathi AV, Prabhakaran D, et al. The association between a vegetarian diet and cardiovascular disease (CVD) risk factors in India: The Indian Migration Study. PLoS One. 2014;9:e110586. doi: 10.1371/journal.pone.0110586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leenders M, Boshuizen HC, Ferrari P, Siersema PD, Overvad K, Tjønneland A, et al. Fruit and vegetable intake and cause-specific mortality in the EPIC study. Eur J Epidemiol. 2014;29:639–52. doi: 10.1007/s10654-014-9945-9. [DOI] [PubMed] [Google Scholar]
- 34.Okuda N, Miura K, Okayama A, Okamura T, Abbott RD, Nishi N, et al. Fruit and vegetable intake and mortality from cardiovascular disease in Japan: A 24-year follow-up of the NIPPON DATA80 study. Eur J Clin Nutr. 2015;69:482–8. doi: 10.1038/ejcn.2014.276. [DOI] [PubMed] [Google Scholar]
- 35.Nguyen B, Bauman A, Gale J, Banks E, Kritharides L, Ding D, et al. Fruit and vegetable consumption and all-cause mortality: Evidence from a large Australian cohort study. Int J Behav Nutr Phys Act. 2016;13:9. doi: 10.1186/s12966-016-0334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality – A systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017;46:1029–56. doi: 10.1093/ije/dyw319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller V, Mente A, Dehghan M, Rangarajan S, Zhang X, Swaminathan S, et al. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): A prospective cohort study. Lancet. 2017;390:2037–49. doi: 10.1016/S0140-6736(17)32253-5. [DOI] [PubMed] [Google Scholar]
- 38.Joshipura KJ, Ascherio A, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, et al. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA. 1999;282:1233–9. doi: 10.1001/jama.282.13.1233. [DOI] [PubMed] [Google Scholar]
- 39.Sauvaget C, Nagano J, Allen N, Kodama K. Vegetable and fruit intake and stroke mortality in the hiroshima/Nagasaki life span study. Stroke. 2003;34:2355–60. doi: 10.1161/01.STR.0000089293.29739.97. [DOI] [PubMed] [Google Scholar]
- 40.Johnsen SP, Overvad K, Stripp C, Tjønneland A, Husted SE, Sørensen HT, et al. Intake of fruit and vegetables and the risk of ischemic stroke in a cohort of Danish men and women. Am J Clin Nutr. 2003;78:57–64. doi: 10.1093/ajcn/78.1.57. [DOI] [PubMed] [Google Scholar]
- 41.Dauchet L, Amouyel P, Dallongeville J. Fruit and vegetable consumption and risk of stroke: A meta-analysis of cohort studies. Neurology. 2005;65:1193–7. doi: 10.1212/01.wnl.0000180600.09719.53. [DOI] [PubMed] [Google Scholar]
- 42.He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: Meta-analysis of cohort studies. Lancet. 2006;367:320–6. doi: 10.1016/S0140-6736(06)68069-0. [DOI] [PubMed] [Google Scholar]
- 43.Oude Griep LM, Verschuren WM, Kromhout D, Ocké MC, Geleijnse JM. Raw and processed fruit and vegetable consumption and 10-year stroke incidence in a population-based cohort study in the Netherlands. Eur J Clin Nutr. 2011;65:791–9. doi: 10.1038/ejcn.2011.36. [DOI] [PubMed] [Google Scholar]
- 44.Sharma S, Cruickshank JK, Green DM, Vik S, Tome A, Kolonel LN, et al. Impact of diet on mortality from stroke: Results from the U.S. multiethnic cohort study. J Am Coll Nutr. 2013;32:151–9. doi: 10.1080/07315724.2013.791798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Larsson SC, Virtamo J, Wolk A. Total and specific fruit and vegetable consumption and risk of stroke: A prospective study. Atherosclerosis. 2013;227:147–52. doi: 10.1016/j.atherosclerosis.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 46.Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2014;349:g4490. doi: 10.1136/bmj.g4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alonso A, de la Fuente C, Martín-Arnau AM, de Irala J, Martínez JA, Martínez-González MA, et al. Fruit and vegetable consumption is inversely associated with blood pressure in a Mediterranean population with a high vegetable-fat intake: The Seguimiento Universidad de Navarra (SUN) study. Br J Nutr. 2004;92:311–9. doi: 10.1079/BJN20041196. [DOI] [PubMed] [Google Scholar]
- 48.Chan Q, Stamler J, Brown IJ, Daviglus ML, Van Horn L, Dyer AR, et al. Relation of raw and cooked vegetable consumption to blood pressure: The INTERMAP study. J Hum Hypertens. 2014;28:353–9. doi: 10.1038/jhh.2013.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li B, Li F, Wang L, Zhang D. Fruit and vegetables consumption and risk of hypertension: A meta-analysis. J Clin Hypertens (Greenwich) 2016;18:468–76. doi: 10.1111/jch.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA. 2002;288:2569–78. doi: 10.1001/jama.288.20.2569. [DOI] [PubMed] [Google Scholar]
- 51.Hu FB. Plant-based foods and prevention of cardiovascular disease: An overview. Am J Clin Nutr. 2003;78:544S–51S. doi: 10.1093/ajcn/78.3.544S. [DOI] [PubMed] [Google Scholar]
- 52.Bazzano LA. Dietary intake of fruit and vegetables and risk of diabetes mellitus and cardiovascular diseases. Geneva: World Health Organization; 2005. [Google Scholar]
- 53.Ding EL, Mozaffarian D. Optimal dietary habits for the prevention of stroke. Semin Neurol. 2006;26:11–23. doi: 10.1055/s-2006-933305. [DOI] [PubMed] [Google Scholar]
- 54.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH collaborative research group. N Engl J Med. 1997;336:1117–24. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 56.Rees K, Hartley L, Flowers N, Clarke A, Hooper L, Thorogood M, et al. ‘Mediterranean’ dietary pattern for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;((8)):CD009825. doi: 10.1002/14651858.CD009825.pub2. [DOI] [PubMed] [Google Scholar]
- 57.Bondonno NP, Bondonno CP, Ward NC, Hodgson JM, Croft KD. The cardiovascular health benefits of apples: Whole fruit vs.isolated compounds. Trends Food Sci Technol. 2017;69:243–56. [Google Scholar]
- 58.Chauhan S, Aeri BT. Prevalence of cardiovascular disease in India and its economic impact – A review. Int J Sci Res Publ. 2013;3:1–5. [Google Scholar]
- 59.Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 60.Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, et al. Prevalence of diabetes and prediabetes in 15 states of India: Results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5:585–96. doi: 10.1016/S2213-8587(17)30174-2. [DOI] [PubMed] [Google Scholar]
- 61.Leon BM, Maddox TM. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015;6:1246–58. doi: 10.4239/wjd.v6.i13.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hawkes C, Fanzo J. Bristol: Development Initiatives Poverty Research Ltd; 2017. [accessed on July 6, 2018]. Nourishing the SDGs: Global nutrition report 2017. Available from: http://openaccess.city.ac.uk/id/eprint/19322 . [Google Scholar]
- 63.Pradeepa R, Anjana RM, Joshi SR, Bhansali A, Deepa M, Joshi PP, et al. Prevalence of generalized & abdominal obesity in urban & rural India - the ICMR-INDIAB study (Phase-I) [ICMR- INDIAB-3] Indian J Med Res. 2015;142:139–50. doi: 10.4103/0971-5916.164234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kumar N, Puri N, Marotta F, Dhewa T, Calabrò S, Puniya M, et al. Diabesity: An epidemic with its causes, prevention and control with special focus on dietary regime. Funct Foods Health Dis. 2017;7:1–6. [Google Scholar]
- 65.Mohan V, Ruchi V, Gayathri R, Bai MR, Sudha V, Anjana RM, et al. Slowing the diabetes epidemic in the World Health Organization South-East Asia region: The role of diet and physical activity. WHO South East Asia J Public Health. 2016;5:5–16. doi: 10.4103/2224-3151.206554. [DOI] [PubMed] [Google Scholar]
- 66.Prentice AM, Jebb SA. Fast foods, energy density and obesity: A possible mechanistic link. Obes Rev. 2003;4:187–94. doi: 10.1046/j.1467-789x.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- 67.He K, Hu FB, Colditz GA, Manson JE, Willett WC, Liu S, et al. Changes in intake of fruits and vegetables in relation to risk of obesity and weight gain among middle-aged women. Int J Obes Relat Metab Disord. 2004;28:1569–74. doi: 10.1038/sj.ijo.0802795. [DOI] [PubMed] [Google Scholar]
- 68.Vergnaud AC, Norat T, Mouw T, Romaguera D, May AM, Bueno-de-Mesquita HB, et al. Macronutrient composition of the diet and prospective weight change in participants of the EPIC-PANACEA study. PLoS One. 2013;8:e57300. doi: 10.1371/journal.pone.0057300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schwingshackl L, Hoffmann G, Kalle-Uhlmann T, Arregui M, Buijsse B, Boeing H, et al. Fruit and vegetable consumption and changes in anthropometric variables in adult populations: A systematic review and meta-analysis of prospective cohort studies. PLoS One. 2015;10:e0140846. doi: 10.1371/journal.pone.0140846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rautiainen S, Wang L, Lee IM, Manson JE, Buring JE, Sesso HD, et al. Higher intake of fruit, but not vegetables or fiber, at baseline is associated with lower risk of becoming overweight or obese in middle-aged and older women of normal BMI at baseline. J Nutr. 2015;145:960–8. doi: 10.3945/jn.114.199158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu S, Serdula M, Janket SJ, Cook NR, Sesso HD, Willett WC, et al. A prospective study of fruit and vegetable intake and the risk of type 2 diabetes in women. Diabetes Care. 2004;27:2993–6. doi: 10.2337/diacare.27.12.2993. [DOI] [PubMed] [Google Scholar]
- 72.Villegas R, Shu XO, Gao YT, Yang G, Elasy T, Li H, et al. Vegetable but not fruit consumption reduces the risk of type 2 diabetes in Chinese women. J Nutr. 2008;138:574–80. doi: 10.1093/jn/138.3.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bazzano LA, Li TY, Joshipura KJ, Hu FB. Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care. 2008;31:1311–7. doi: 10.2337/dc08-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cooper AJ, Sharp SJ, Lentjes MA, Luben RN, Khaw KT, Wareham NJ, et al. A prospective study of the association between quantity and variety of fruit and vegetable intake and incident type 2 diabetes. Diabetes Care. 2012;35:1293–300. doi: 10.2337/dc11-2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang PY, Fang JC, Gao ZH, Zhang C, Xie SY. Higher intake of fruits, vegetables or their fiber reduces the risk of type 2 diabetes: A meta-analysis. J Diabetes Investig. 2016;7:56–69. doi: 10.1111/jdi.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jia X, Zhong L, Song Y, Hu Y, Wang G, Sun S, et al. Consumption of citrus and cruciferous vegetables with incident type 2 diabetes mellitus based on a meta-analysis of prospective study. Prim Care Diabetes. 2016;10:272–80. doi: 10.1016/j.pcd.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 77.Mamluk L, O’Doherty MG, Orfanos P, Saitakis G, Woodside JV, Liao LM, et al. Fruit and vegetable intake and risk of incident of type 2 diabetes: Results from the consortium on health and ageing network of cohorts in Europe and the United States (CHANCES) Eur J Clin Nutr. 2017;71:83–91. doi: 10.1038/ejcn.2016.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Du H, Li L, Bennett D, Guo Y, Turnbull I, Yang L, et al. Fresh fruit consumption in relation to incident diabetes and diabetic vascular complications: A 7-y prospective study of 0.5 million Chinese adults. PLoS Med. 2017;14:e1002279. doi: 10.1371/journal.pmed.1002279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jenkins DJ, Srichaikul K, Kendall CW, Sievenpiper JL, Abdulnour S, Mirrahimi A, et al. The relation of low glycaemic index fruit consumption to glycaemic control and risk factors for coronary heart disease in type 2 diabetes. Diabetologia. 2011;54:271–9. doi: 10.1007/s00125-010-1927-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ray KS, Paharia NV, Singhania PS. Mango: Yes or no for individuals with diabetes. Endocrinol Diabetes Clin Med Res. 2017;1:103. [Google Scholar]
- 81.de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454–9. doi: 10.1016/s0140-6736(94)92580-1. [DOI] [PubMed] [Google Scholar]
- 82.John JH, Ziebland S, Yudkin P, Roe LS, Neil HA Oxford Fruit and Vegetable Study Group. Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: A randomised controlled trial. Lancet. 2002;359:1969–74. doi: 10.1016/s0140-6736(02)98858-6. [DOI] [PubMed] [Google Scholar]
- 83.Fruit and vegetables for health: report of the joint FAO/WHO workshop on fruit and vegetables for health, 1-3 September, 2004 Kobe, Japan. Geneva: WHO; 2005. [accessed on August 18, 2018]. WHO. Available from: http://www.who.int/iris/handle/10665/43143 . [Google Scholar]
- 84.McCall DO, McGartland CP, McKinley MC, Patterson CC, Sharpe P, McCance DR, et al. Dietary intake of fruits and vegetables improves microvascular function in hypertensive subjects in a dose-dependent manner. Circulation. 2009;119:2153–60. doi: 10.1161/CIRCULATIONAHA.108.831297. [DOI] [PubMed] [Google Scholar]
- 85.Hartley L, Igbinedion E, Holmes J, Flowers N, Thorogood M, Clarke A, et al. Increased consumption of fruit and vegetables for the primary prevention of cardiovascular diseases. Cochrane Database Syst Rev. 2013;((6)):CD009874. doi: 10.1002/14651858.CD009874.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rompotis CJ, Grove JR, Byrne SM. Benefits of habit-based informational interventions: A randomised controlled trial of fruit and vegetable consumption. Aust N Z J Public Health. 2014;38:247–52. doi: 10.1111/1753-6405.12232. [DOI] [PubMed] [Google Scholar]
- 87.Mytton OT, Nnoaham K, Eyles H, Scarborough P, Ni Mhurchu C. Systematic review and meta-analysis of the effect of increased vegetable and fruit consumption on body weight and energy intake. BMC Public Health. 2014;14:886. doi: 10.1186/1471-2458-14-886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hodder RK, O’Brien KM, Stacey FG, Wyse RJ, Clinton-McHarg T, Tzelepis F, et al. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database Syst Rev. 2018;5:CD008552. doi: 10.1002/14651858.CD008552.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis. BMJ. 2008;337:a1344. doi: 10.1136/bmj.a1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sharma SP, Chung HJ, Kim HJ, Hong ST. Paradoxical effects of fruit on obesity. Nutrients. 2016;8 doi: 10.3390/nu8100633. pii: E633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cheng YC, Sheen JM, Hu WL, Hung YC. Polyphenols and oxidative stress in atherosclerosis-related ischemic heart disease and stroke. Oxid Med Cell Longev. 2017;2017:8526438. doi: 10.1155/2017/8526438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.WHO technical staff: Increasing fruit and vegetable consumption to reduce the risk of non communicable diseases. Biological, behavioural and contextual rationale. e-Library of Evidence for Nutrition Actions. Geneva: WHO; 2014. Sep, [accessed on June 20, 2018]. World Health Organization. Available from: www.who.int/elena/bbc/fruit_vegetables_ncds/en . [Google Scholar]
- 93.Tang GY, Meng X, Li Y, Zhao CN, Liu Q, Li HB, et al. Effects of vegetables on cardiovascular diseases and related mechanisms. Nutrients. 2017;9 doi: 10.3390/nu9080857. pii: E857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Marías YF, Glasauer P. Romel: Food and Agriculture Organization of the United Nations; 2014. Guidelines for assessing nutrition-related knowledge, attitudes and practices. [Google Scholar]
- 95.Haynes-Maslow L, Parsons SE, Wheeler SB, Leone LA. A qualitative study of perceived barriers to fruit and vegetable consumption among low-income populations, North Carolina, 2011. Prev Chronic Dis. 2013;10:E34. doi: 10.5888/pcd10.120206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pinho MGM, Mackenbach JD, Charreire H, Oppert JM, Bárdos H, Glonti K, et al. Exploring the relationship between perceived barriers to healthy eating and dietary behaviours in European adults. Eur J Nutr. 2018;57:1761–70. doi: 10.1007/s00394-017-1458-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Brug J. Determinants of healthy eating: Motivation, abilities and environmental opportunities. Fam Pract. 2008;25((Suppl 1)):i50–5. doi: 10.1093/fampra/cmn063. [DOI] [PubMed] [Google Scholar]
- 98.Nayak MU, Vazir S, Vijayaraghavan K, Chandralekha K. Nutrition communication using social-marketing techniques to combat Vitamin A deficiency: Results of summative evaluation. Food Nutr Bull. 2001;22:454–65. [Google Scholar]
- 99.National Horticulture Board. Operational Guidelines; Schemes of Horticulture Board. National Horticulture Board. Ministry of Agriculture Government of India. 2015. Feb, [accessed on July 15, 2018]. Available from: http://nhb.gov.in/schemes.aspx?enc=3ZOO8K5CzcdC/Yq6HcdIxOVZI61DUqgouJqJXNMGlcc=
- 100.John JH, Ziebland S. Reported barriers to eating more fruit and vegetables before and after participation in a randomized controlled trial: A qualitative study. Health Educ Res. 2004;19:165–74. doi: 10.1093/her/cyg016. [DOI] [PubMed] [Google Scholar]
- 101.Finzer LE, Ajay VS, Ali MK, Shivashankar R, Goenka S, Sharma P, et al. Fruit and vegetable purchasing patterns and preferences in South Delhi. Ecol Food Nutr. 2013;52:1–20. doi: 10.1080/03670244.2012.705757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Thow AM, Priyadarshi S. Aid for trade: An opportunity to increase fruit and vegetable supply. Bull World Health Organ. 2013;91:57–63. doi: 10.2471/BLT.12.106955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: A comprehensive review. Circulation. 2016;133:187–225. doi: 10.1161/CIRCULATIONAHA.115.018585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sachdeva S, Sachdev TR, Sachdeva R. Increasing fruit and vegetable consumption: Challenges and opportunities. Indian J Community Med. 2013;38:192–7. doi: 10.4103/0970-0218.120146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rakotoniaina ALH. How to increase fruit and vegetable consumption: A Multistakeholder approach for improved health outcomes - A report from the alliance for food & health. J Am Coll Nutr. 2018;37:251–66. doi: 10.1080/07315724.2017.1376298. [DOI] [PubMed] [Google Scholar]
- 106.Krishnaswamy K, Laxmaiah A. Nutrition related non-communicable chronic disorders. In: Vir SC, editor. Public health nutirition in developing countries part II. Delhi: Woodhead Publishing India Pvt Ltd; 2011. pp. 956–81. [Google Scholar]
- 107.Ministry of Health & Family Welfare. National programme for prevention and control of cancer, diabetes, cardiovascular disease and stroke. Ministry of Health and Family Welfare. 2013. [accessed on June 28, 2018]. Available from: https://mohfw.gov.in/about-us/departments/departments-health-and-familywelfare/national-programme-prevention-and-control-cancerdiabetes-cardiovascular-disease-and .