Abstract
Vitamin A deficiency (VAD) among 1-5 yr old children is reported to be widely prevalent in Southeast Asia and some parts of Africa. It is the leading cause of preventable blindness in young children in the low-income countries in the world. Children even with milder signs of VAD have higher risk of morbidity and mortality. Inadequate dietary intakes of vitamin A with poor bioavailability associated with frequent infections are the primary contributory factors. Currently available approaches to control VAD are ensuring adequate intakes of vitamin A in daily diets, fortification of foods consumed regularly particularly among the low-income communities and periodic administration of massive dose of vitamin A supported by public health interventions and reinforced by behaviour change communication. Under the National Programme in India, six monthly administration of mega dose of vitamin A to 6-59 month old children has been implemented since 1970, to prevent particularly blindness due to VAD and control hypovitaminosis A. Despite inadequate coverage and poor implementation of the programme, blindness due to VAD in children has almost disappeared, though subclinical VAD is still widely prevalent. Based on the results of meta-analysis of eight trials, which indicated that vitamin A supplementation to children aged 6-59 months reduced child mortality rates by about 23 per cent, the World Health Organization made a strong recommendation that in areas with VAD as a public health problem, vitamin A supplementation should be given to infants and children of 6-59 months of age as a public health intervention to reduce child morbidity and improve child survival. At present, in India, there is a need for change in policy with respect to the national programme to opt for targeted instead of universal distribution. However, NITI (National Institution for Transforming India) Aayog, which formulates policies and provides technical support to the Government of India, recommends strengthening of the National Programme for control of VAD through six monthly vitamin A supplementation along with health interventions. Eventually, the goal is to implement food based and horticulture-based interventions harmonizing with public health measures, food fortification and capacity building of functionaries for elimination of VAD.
Keywords: Biannual distribution, child mortality, child survival, mega-dose vitamin A, National Vitamin A Programme, targeted distribution, universal distribution, vitamin A supplementation
Introduction
Micronutrient deficiencies, i.e. deficiencies of vitamins and minerals, are significant contributors to the global burden of disease. In India, the most important micronutrients of public health significance are vitamin A, iron and iodine. In fact, deficiencies of vitamin A, iron and zinc together are reported to be the second largest risk factor in the global burden of diseases1. Yet, micronutrient malnutrition goes largely unrecognized and hence is also referred to as ‘hidden hunger’, the consequences of which are high morbidity and mortality among young children. As per the estimates of the World Health Organization (WHO), globally vitamin A deficiency (VAD) was affecting about a third of children aged 6-59 months, with prevalence rates as high as about 50 per cent in Southeast Asia and about 44 per cent in Africa. In Southeast Asia, it is estimated that a little over 90 million preschool children had subclinical VAD as indicated by low serum retinol levels2. The WHO recommends serum retinol levels <0.70 μmol/l as an indicator to assess the severity of VAD in communities3. The magnitude of clinical and subclinical VAD among young children in India is higher than the neighbouring countries in the Southeast Asia4. Even though the prevalence of Bitot spots in preschool children currently is low, subclinical VAD is widespread in the country. The National Nutrition Monitoring Bureau (NNMB)5 surveys revealed that about 62 per cent of preschool children had low serum retinol <0.70 μmol/l and 21.5 per cent had levels <0.35 μmol/l. Low tissue concentrations of vitamin A could also cause adverse health consequences, even in the absence of clinical signs, and therefore should be considered as of public health significance. By and large, the available data indicate slight improvement in India with respect to prevalence of VAD, since 1991, as compared to the neighbouring countries such as Sri Lanka, the Maldives and Bangladesh, which have achieved substantial reductions in VAD among children6.
Consequences
VAD is the leading cause of preventable blindness in young children in the low-income countries in the world. In addition, it can impair growth, weaken the immune system and thus increase susceptibility to infection. Children suffering from measles are at a higher risk of death in the presence of VAD7. Higher risk of respiratory infection and diarrhoea has been demonstrated among Indonesian children with mild VAD8. The children with mild xerophthalmia also had increased risk of mortality9. Pregnant women having serum retinol level <20 μg/dl (<0.70 μmol/l), which is indicative of VAD, during the third trimester of pregnancy had higher risk of preterm delivery and maternal anaemia10. A study in Nepal also showed that night blindness in pregnant women increased the mortality risk among women11.
Contributory factors
An understanding of the possible contributory factors for the widespread occurrence of VAD in India would help in the formulation of programmes for its prevention. Poverty and ignorance, mainly due to low literacy particularly among women, are the important underlying factors for the extensive prevalence of VAD in India and the neighbouring developing countries. Inadequate intakes of vitamin A in women during pregnancy and lactation, increase the chances of VAD in the offspring12. The primary reason for the widespread VAD in India is consumption of inadequate amounts of the vitamin in diets among all the age groups. On the average, diets of young children in the rural areas are woefully inadequate in foods providing β-carotene/retinol. The consumption of animal sources such as milk and eggs that provide preformed vitamin A is very low (Table). As a result, the mean daily consumption of vitamin A is less than half of the recommended dietary allowance (RDA), and more than a third of the children of 1-6 yr of age consume much below 25 per cent RDA of vitamin A13.
Table.
Mean dietary intake of β-carotene/retinol foods - rural preschool children
| Age group (yr) | Carotene/retinol foods (g) | Retinol equivalents (µg) | RDA (μg) | |
|---|---|---|---|---|
| Vegetables | Milk and milk products | |||
| 1-3 | 41 | 86 | 151 | 400 |
| 4-6 | 70 | 67 | 177 | 400 |
Source: Ref. 13
The intestinal conversion ratio of dietary carotenoids to retinol is currently reported to be 12:114. In other words, the efficiency of conversion of β-carotene to retinol is only about a half as compared to that thought so far. Hence, the diets which are primarily based on β-carotene providing vegetables and fruits are unlikely to provide the required amounts of vitamin A in communities, subsisting on inadequate diets. Repeat surveys of NNMB13 indicate very negligible improvement in vitamin A intakes over the past three decades (Figure).
Figure.
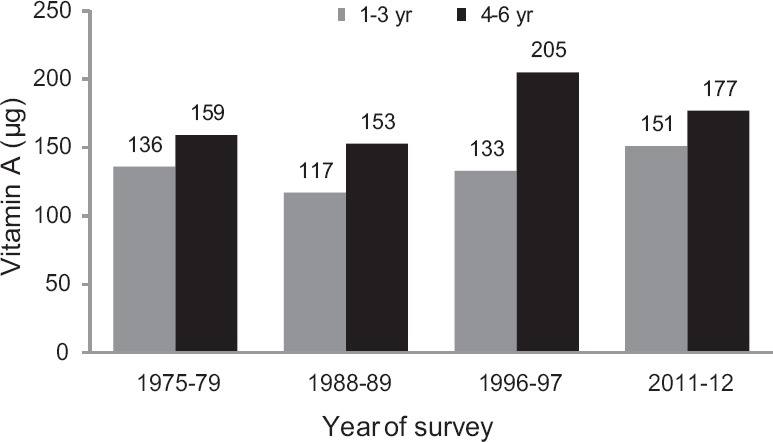
Time trends in vitamin A intakes in preschool children. Source: Ref. 13.
Avoidance of foods rich in β-carotene such as papaya during pregnancy and discarding colostrum immediately after childbirth, due to superstitions and general lack of awareness in the community about the nutritional needs also contribute to poor vitamin A status from very young age. In addition, Indian preschool children are exposed to frequent respiratory infections and diarrhoea and parasitic infestations. Repeated infections reduce the absorption of vitamin A, aggravating further the already poor nutritional status of the children in rural communities15.
Prevention strategies
As the major contributory factor for the extensive prevalence of VAD is consumption of diets providing low amounts of vitamin A because of food insecurity and lack of awareness, fundamental aim, therefore, should be to ensure regular intakes of vitamin A among the vulnerable groups through horticultural intervention to produce foods rich in the micronutrient, thus improving availability, access and utilization of locally available vitamin A/β-carotene-rich foods including non-conventional leafy vegetables with high β-carotene content. Horticultural strategy coupled with behaviour change communication will therefore be a sustainable approach to control VAD. A three-year study at the National Institute of Nutrition (NIN) demonstrated that home gardening along with effective nutrition communication in villages in backward districts of Andhra Pradesh increased availability and consumption of vegetables rich in β-carotene at household level, pointing out the need for incorporating nutrition component to the horticultural policy in India16. Conventional approaches to nutrition education have not been successful in changing the diet practices essential to prevent and control VAD among rural Indian communities. A study conducted at NIN in rural areas of Andhra Pradesh demonstrated that adopting social marketing strategy was effective in communicating nutrition messages to prevent VAD and, thus, emphasizing the need for adopting innovative strategies for communicating nutrition messages17. Behavioural change communication strategy practices are essential to prevent and control VAD among rural Indian communities. Innovative strategies adopting marketing principles for conveying appropriate messages for changing nutrition behaviour are, therefore, advocated. Behavioural change communication strategy requires substantial financial and human resources and has very large gestation period. Effective communication should be an essential component of all interventions.
As a medium-term strategy, fortification of one or more commonly consumed foods with vitamin A may be a cost-effective strategy for preventing VAD, particularly in countries where improvement of dietary intakes among rural communities in the conceivable future is not possible. In the case of fortification, essential nutrients that are deficient in the diets and leading to nutrition deficiencies are added to increase their consumption regularly and also to improve the quality of the diet so as to provide nutritional benefit without any risk to the health of the individuals. Iodized salt programme is, perhaps, the earliest and the most successful food fortification strategy adopted to control iodine deficiency disorders in India. With respect to vitamin A, mandatory fortification of hydrogenated fats with vitamin A was perhaps the first such an approach in India. Elsewhere in Central and South America, VAD was effectively controlled through fortification of sugar as early as 40 years back. In several Central American countries, sugar was fortified with vitamin A successfully for reducing VAD significantly18. Success stories of sugar fortification in Guatemala and Honduras showed the possibility to control this public health problem through adopting strategies appropriate for the regions with wise planning19. In the Philippines and Indonesia, fortification of monosodium glutamate with vitamin A was adopted extensively. Evaluation of the programme revealed that there was improvement in breast milk and serum retinol concentrations and improvement in growth and survival of preschool children20. In Brazil, it has been demonstrated that it is feasible to fortify soybean oil with vitamin A21. Caution, however, should be exercised in promoting fortified foods with vitamin A, especially in a population which is illiterate and ignorant, because of the possibility of overdose of vitamin A.
As a short-term strategy, in situations requiring immediate intervention, the most conventional and extensively adopted strategy is supplementation with one or more micronutrients. The Government of India initiated in 1970 the National Prophylaxis Programme against VAD. The programme's objective was mainly to prevent nutritional blindness. The scientific rationale behind the approach was that vitamin A, being fat soluble, when administered in large dose orally in oil miscible form is stored in the liver for utilization by the human body as required during the period. The national programme was the result of extensive clinical and field trials at the NIN, Hyderabad, carried out about half a century back22. Under the programme, preschool children, particularly in the rural and tribal areas, received a large oral dose of 200,000 IU of vitamin A concentrate every six months23. In addition, all children with clinical signs of xerophthalmia, those suffering from measles (if not received megadose for one month) and children suffering from severe PEM were administered an additional massive dose by the health functionaries. The National Prophylaxis Programme against nutritional blindness is sponsored by the Union Ministry of Health and Family Welfare (MoHFW) and administered by the State Governments through the auxiliary health functionaries of the Primary Health Centres. A large five-year longitudinal covering over 60,000 children, demonstrated categorically that biannual distribution of massive oral dose of vitamin A reduced the incidence of corneal xerophthalmia by 80 per cent24. An evaluation of the programme, carried out after about 10 years of implementation in different States, however, indicated that the outreach of the programme was poor due either to irregular or inadequate supplies or poor appreciation of the programme by the implementing health staff and absence of effective supervision. Therefore, the reduction in clinical signs was observed only where it was implemented satisfactorily by the health centres25. Periodic large dosing, though conceptually simple, is thus beset with several operational problems, particularly in a large country like India. NFHS (National Family Health Survey)-3 revealed that the proportion of children in 12-35 months of age receiving a vitamin A dose during the previous six months in the rural areas during 2005-2006 was a mere 24 per cent26. In order to improve the coverage, especially of the children most vulnerable to nutritional blindness and to optimally utilize the limited supplies of vitamin A, the Union Health Ministry decided to link vitamin A administration to the ongoing immunization programme. Under the revised regimen, all infants at nine months of age received a dose of 100,000 IU of vitamin A along with measles vaccine and a second dose of 200,000 IU was administered at 18 months of age along with booster dose of diphtheria-pertussis-tetanus (DPT) and oral polio vaccine (OPV). Subsequently, the children received three biannual doses of 200,000 IU of vitamin A until 36 months of age. Integrated Child Development Services (ICDS) functionaries also were involved in vitamin A distribution. NNMB surveys in eight States during 2011-2012 revealed that less than a half of 12-59 months old children had received the expected two doses, while 36.5 per cent had received only one dose13. The approach of different States to implementation of the programme was, however, not uniform and thus the coverage varied considerably among the States. Nevertheless, in the States of Bihar and Odisha, six monthly vitamin A supplementation programme for 1-5 yr old children was reported to have achieved consistently high coverage of over 80 per cent over a five-year period by ensuring adequate supplies through better planning and effective monitoring27.
In Assam State, the vitamin A administration was linked with pulse polio immunization campaign with an aim to further improve the coverage. During the campaign, a few deaths of children who had received the vitamin A concentrate were attributed to mega dose of vitamin A causing considerable concern among the public and contributing to extensive adverse publicity which almost derailed the national programme28. It is relevant to know that under the Indian National Vitamin A Prophylaxis Programme, since its inception in 1970, vitamin A concentrate is administered in syrup form and dispensed with a 2 ml spoon, unlike vitamin A capsule distribution in most other countries. For the Assam programme, the sponsoring agency had replaced the 2 ml spoons with 5 ml cups29. Thus, the workers, who were, perhaps, not adequately trained, might have administered more than 2 ml of vitamin A to such children. High-potency vitamin A has been known to cause transient side effects such as nausea, vomiting and headache in a small proportion of 1-4 yr old children30. The deaths may also have been chance occurrences when vitamin A concentrate was administered to sick children, who should have been excluded as well and, thus, not related to the programme per se. Considering the importance of the vitamin A supplementation programme and taking into cognisance the experience in the State of Assam, it was reiterated by the Union government that in future, the administration should adhere to the guidelines on vitamin A supplementation, and focus on quality control, particularly avoiding distribution to very sick and ailing children and use only time-tested 2 ml spoons as dispensers.
Vitamin A Supplementation Programme and child survival
In 1986, a study conducted in Indonesia reported that the mortality rate in children between 12 and 71 months of age, who had received vitamin A supplements, reduced by about 34 per cent as compared to a control group31. The results of another study in Madurai, south India, revealed that in areas where VAD and undernutrition are public health problems, there was 54 per cent reduction in mortality rate in children (12 and 71 months of age) as compared to a control group32. However, in another placebo-controlled randomized field trial that was conducted at the NIN, Hyderabad, no significant mortality reduction was observed among under-five children in a backward rural area after biannual mega-dose vitamin A supplementation33. In 1990, based on the proposal by the Advisory Group on Nutrition, the United Nation Subcommittee on Nutrition (UN-SCN) approved a study, for critically analyzing the available scientific evidence on the effect of vitamin A supplementation on mortality and morbidity in children in the developing countries. Results of a meta-analysis of eight mortality trials indicated that vitamin A supplementation to children aged six months to five years brought down mortality rates by about 23 per cent in populations with at least low prevalence of clinical signs of vitamin A deficiency. There were no differences in the effects by age and sex34. The WHO, taking into consideration the results of the meta-analysis, made a strong recommendation that, in areas where VAD is a public health problem, vitamin A supplementation should be provided to infants and children (6-59 months of age) as a public health intervention to reduce child morbidity and mortality35. The UN-SCN also issued a statement that young child mortality reduction might be an additional reason for increasing efforts to control VAD34. On the other hand, deworming and enhanced vitamin A (DEVTA) study - a cluster-randomized trial - carried out on about one million children in the north Indian State of Uttar Pradesh contradicted the results of the meta-analysis and observed only a small reduction of four per cent among children who had received six monthly vitamin A supplementation36. Subsequently, Cochrane review published a detailed analysis of 47 studies covering around 1,223,856 children from 19 countries in Asia, Africa, Latin America and Australia, with the main objective of determining whether vitamin A supplementation prevented morbidity and mortality in children in the age group of 6-59 months. The results indicated about 12 per cent reduction in risk of death in general and due particularly to diarrhoea after vitamin A supplementation. The review recommended continuing with the policy of universal supplementation for children under five years of age in populations at risk of VAD. The authors also felt that there was no need for further placebo-controlled trials on vitamin A supplementation and morbidity and mortality in children37. In view of the fact that there is no controversy about the benefits of vitamin A supplementation either on clinical or subclinical VAD in areas where it is a public health problem, any additional benefits on child mortality could be considered as a ‘bonus’.
Need for policy change
With these observations on the benefits of vitamin A supplementation on child mortality, vitamin A supplementation was emphasized more for child survival than control of VAD per se particularly by the international agencies. UNICEF considered that Millennium Development Goal-4 (MDG-4) could be achieved by including young children with a package of conventional child survival interventions along with vitamin A supplementation and it recommends vitamin A supplementation in all the countries with high Under-Five Mortality Rate (U5MR). On this basis, 61 countries with high U5MR (>70/1000 childbirths) are considered as priority countries for vitamin A supplementation38. In India, there has been considerable criticism about the continuation of universal vitamin A supplementation as a permanent solution to VAD and more specifically for improvement primarily of child survival. The biannual administration of vitamin A was envisaged as only an interim measure and the medicinal vitamin A supplementation was to be used as no more than a ‘crutch’39. There has been an anxiety that the continuation of biannual vitamin A supplementation programme created a culture of everlasting dependence on the health infrastructure and is operated as prescribed by donors through the international agencies40. There has been a criticism that obsession with vitamin A supplementation programme has caused a policy barrier that has ignored and perhaps hindered other sustainable approaches to prevent and eliminate VAD41. There is a strong demand for abandoning universal approach of prophylactic mega-dose vitamin A supplementation to preschool children and giving preference to targeted approach on the ground that currently there is conclusive evidence supporting almost complete elimination of keratomalacia and reduction in the prevalence of VAD. It is contended that such an approach would help to optimize the available scarce resources better42. It should be appreciated, however, that for identification of communities with VAD, for targeted approach, data should be available on the extent of VAD in the populations in different parts of the country, absence of which, at present, is one of the critical limitations for identifying vulnerable communities/areas for monitoring the programme. Whether any ethical considerations are required, in view of limited availability of proper data, is also to be deliberated before making a decision on targeted approach as it would mean withdrawing the benefits of the existing programme to the really needy, particularly in the absence of surveillance system in communities which lack awareness of the consequences of the deficiency due to illiteracy and ignorance, and more so in view of the evidence-based claims on the beneficial effects on survival. There is, therefore, a need for conducting surveys which include assessment of clinical/subclinical VAD at least once in five years before such decision. The National Nutrition Strategy evolved by NITI (National Institution for Transforming India) Aayog nonetheless envisages strengthening of the programme for control of VAD through vitamin A supplementation as per the MoHFW guidelines, which encourage young child feeding practices, call for improving dietary intake of vitamin A and increasing production and consumption of vitamin A-rich foods and public health Interventions43. As the MoHFW guidelines involve biannual mega dose of vitamin A to children between 6 and 11 months and 12-59 months involving both health and ICDS functionaries, it appears that the government's policy is to continue universal programme of six monthly vitamin A supplementation at least until 20225. Eventually, the proposal to adopt a broader approach to controlling VAD in line with the long-standing policy recommendations should be deliberated and shift the focus from the stand-alone programme of periodic vitamin A supplementation to tackling the basic causes by increasing regular intakes among all segments, including pregnant women, with an effective monitoring of changes in VAD among young children44. This demands harmonious strategies that encourage community acceptable and locally appropriate food-based strategy and horticulture-based interventions, capacity-building of functionaries, public health interventions and food fortification.
It will be a fitting tribute to the NIN, to make nutrition fundamental to the nation's development policies, when it is completing 100 years of its constant and unending endeavour to identify sustainable solutions to the widespread problems of malnutrition in the country.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1.Kotecha PV. Micronutrient malnutrition in India: Let us say “No” to it now. Indian J Community Med. 2008;33:9–10. doi: 10.4103/0970-0218.39235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global prevalence of vitamin A deficiency in populations at risk 1995-2005. Geneva: WHO; 2009. World Health Organization. [Google Scholar]
- 3.Micronutrients indicators - Serum retinol concentrations for determining the prevalence of vitamin A deficiency in populations. Geneva: WHO; 1998. World Health Organization. [Google Scholar]
- 4.Gragnolati M, Bredenkamp C, Shekar M, Das Gupta M, Lee Y. Health, Nutrition and population series. Washington, DC: The World Bank; 2006. India's undernourished children: A call for reform and action. [Google Scholar]
- 5.National Nutrition Monitoring Bureau, Prevalence of vitamin A deficiency among preschool children in rural areas, technical report 23. Hyderabad: NIN; 2006. National Institute of Nutrition. [Google Scholar]
- 6.Harding KL, Aguayo VM, Webb P. Hidden hunger in South Asia: A review of recent trends and persistent challenges. Public Health Nutr. 2017;21:1–11. doi: 10.1017/S1368980017003202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barclay AJ, Foster A, Sommer A. Vitamin A supplements and mortality related to measles: A randomised clinical trial. Br Med J (Clin Res Ed) 1987;294:294–6. doi: 10.1136/bmj.294.6567.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sommer A, Tarwotjo I, Hussaini G, Susanto D. Increased mortality in children with mild vitamin A deficiency. Lancet. 1983;2:585–8. doi: 10.1016/s0140-6736(83)90677-3. [DOI] [PubMed] [Google Scholar]
- 9.Sommer A, Katz J, Tarwotjo I. Increased risk of respiratory disease and diarrhea in children with preexisting mild vitamin A deficiency. Am J Clin Nutr. 1984;40:1090–5. doi: 10.1093/ajcn/40.5.1090. [DOI] [PubMed] [Google Scholar]
- 10.Radhika MS, Bhaskaram P, Balakrishna N, Ramalakshmi BA, Devi S, Kumar BS, et al. Effects of vitamin A deficiency during pregnancy on maternal and child health. BJOG. 2002;109:689–93. doi: 10.1111/j.1471-0528.2002.01010.x. [DOI] [PubMed] [Google Scholar]
- 11.Christian P, West KP, Jr, Khatry SK, Kimbrough-Pradhan E, LeClerq SC, Katz J. Night blindness during pregnancy and subsequent mortality among women in Nepal: Effects of vitamin A and beta-carotene supplementation. Am J Epidemiol. 2000;152:542–7. doi: 10.1093/aje/152.6.542. [DOI] [PubMed] [Google Scholar]
- 12.Vijayaraghavan K. Fat soluble vitamins deficiency - vitamins A and D. In: Bamji MS, Reddy V, Pralhad Rao PN, editors. Text Book on Human Nutrition. 4th ed. New Delhi: Oxford Publishing House; 2016. [Google Scholar]
- 13.Hypertension & diabetes among adults and infant & young child feeding practices - report of third repeat survey, NNMB technical report no.26. Hyderabad: National Institute of Nutrition; 2012. National Nutrition Monitoring Bureau. [Google Scholar]
- 14.Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington, DC: National Academy Press (US); 2001. [accessed on September 24, 2018]. Institute of Medicine (US) Panel on Micronutrients. Available from: https://www.ncbi.nlm.nih.gov/books/NBK222310/ [PubMed] [Google Scholar]
- 15.Sivakumar B, Reddy V. Absorption of labelled vitamin A in children during infection. Br J Nutr. 1972;27:299–304. doi: 10.1079/bjn19720094. [DOI] [PubMed] [Google Scholar]
- 16.Vijayaraghavan K, Uma Nayak M, Bamji MS, Ramana GNV, Reddy V. Home gardening for combating vitamin A deficiency in rural India. Food Nutr Bull. 1997;18:337–43. [Google Scholar]
- 17.Nayak U, Vazir S, Vijayaraghavan K, Chandralekha K. Nutrition communication using social marketing techniques to combat vitamin A deficiency: Results of summative evaluation. Food Nutr Bull. 2001;22:454–65. [Google Scholar]
- 18.Arroyave G, Mejia LA. Five decades of vitamin A studies in the region of Central America and Panama. Food Nutr Bull. 2010;31:118–29. doi: 10.1177/156482651003100112. [DOI] [PubMed] [Google Scholar]
- 19.Mora JO, Dar O, Chinchilla D, Arroyave, G . Arlington: MOST - USAID Micronutrient Programme; 2000. Vitamin A sugar fortification in Central America - Experience and lessons learned. [Google Scholar]
- 20.Muhilal, Murdiana A, Azis I, Saidin S, Jahari AB, Karyadi D, et al. vitamin A-fortified monosodium glutamate and vitamin A status: A controlled field trial. Am J Clin Nutr. 1988;48:1265–70. doi: 10.1093/ajcn/48.5.1265. [DOI] [PubMed] [Google Scholar]
- 21.Favaro RMD. Evaluation of the effect of heat treatment on the biological value of vitamin A fortified soybean oil. Nutr Res. 1992;12:1357–63. [Google Scholar]
- 22.Swaminathan MC, Susheela TP, Thimmayamma BVS. Field prophylactic trial with a single annual oral massive dose of vitamin A. Am J Clin Nutr. 1970;23:119–22. doi: 10.1093/ajcn/23.1.119. [DOI] [PubMed] [Google Scholar]
- 23.Kapil U, Sachdev HPS. Massive dose vitamin A programme in India - Need for a targeted approach. Indian J Med Res. 2013;138:411–7. [PMC free article] [PubMed] [Google Scholar]
- 24.Vijayaraghavan K, Sarma KV, Rao NP, Reddy V. Impact of massive doses of vitamin A on incidence of nutritional blindness. Lancet. 1984;2:149–51. doi: 10.1016/s0140-6736(84)91058-4. [DOI] [PubMed] [Google Scholar]
- 25.Vijayaraghavan K, Rao NP. An evaluation of the national prophylaxis programme against blindness due to vitamin A deficiency. Nutr Rep Int. 1982;25:431–41. [Google Scholar]
- 26.National Family Health Survey, Report of NFHS-3. Mumbai: IIPS; 2007. International Institute for Population Sciences, Ministry of Health and Family Welfare, Government of India. [Google Scholar]
- 27.Rah JH, Houston R, Mohapatra BD, Kumar SS, Saiyed F, Bhattacharjee S, et al. A review of the vitamin A supplementation program in India: Reasons for success in the states of Bihar and Odisha. Food Nutr Bull. 2014;35:203–10. doi: 10.1177/156482651403500207. [DOI] [PubMed] [Google Scholar]
- 28.Sharma DC. UN vitamin A campaign in under fire. Lancet. 2001;358:1791. [Google Scholar]
- 29.Kapil U. Deaths in Assam during vitamin A pulse distribution: The needle of suspicion is on the new measuring cup. Indian Pediatr. 2002;39:114–5. [PubMed] [Google Scholar]
- 30.West KP, Jr, Sommer A. Vitamin A programme in Assam probably caused hysteria. Br Med J (Clin Res Ed) 2002;324:791. doi: 10.1136/bmj.324.7340.791/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sommer A, Tarwotjo I, Djunaedi E, West KP, Jr, Loeden AA, Tilden R. Impact of vitamin A supplementation on childhood mortality. A randomised controlled community trial. Lancet. 1986;1:1169–73. doi: 10.1016/s0140-6736(86)91157-8. [DOI] [PubMed] [Google Scholar]
- 32.Rahmathullah L, Underwood BA, Thulasiraj RD, Milton RC, Ramaswamy K, Rahmathullah R, et al. Reduced mortality among children in Southern India receiving a small weekly dose of vitamin A. N Engl J Med. 1990;323:929–35. doi: 10.1056/NEJM199010043231401. [DOI] [PubMed] [Google Scholar]
- 33.Vijayaraghavan K, Radhaiah G, Prakasam BS, Sarma KV, Reddy V. Effect of massive dose of vitamin A on morbidity and mortality A double blind trial in Indian children. Lancet. 1990;336:1342–5. doi: 10.1016/0140-6736(90)92895-o. [DOI] [PubMed] [Google Scholar]
- 34.Effectiveness of vitamin A supplementation in the control of young child morbidity and mortality in developing countries. Nutrition policy discussion paper No. 13. United Nations ACC/SCN State-of-the-Art Series. Geneva: United Nations, ACC/SCN; 1993. United Nations, Administrative Committee on Coordination, Subcommittee on Nutrition (ACC/SCN) [Google Scholar]
- 35.Guidelines: Vitamin A supplementation in infants and children 6-59 months of age. Geneva: WHO; 2011. World Health Organization. [PubMed] [Google Scholar]
- 36.Awasthi S, Peto R, Read S, Clark S, Pande V, Bundy D, et al. Vitamin A supplementation every 6 months with retinol in 1 million pre-school children in North India: DEVTA, a cluster-randomised trial. Lancet. 2013;381:1469–77. doi: 10.1016/S0140-6736(12)62125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Imdad A, Mayo-Wilson E, Herzer K, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst Rev. 2017;3:CD008524. doi: 10.1002/14651858.CD008524.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vitamin A supplementation: A decade of progress. New York: UNICEF; 2007. [accessed on September 24, 2018]. UNICEF. Available from: https://www.unicef.org/publications/files/Vitamin_A_Supplementation.pdf . [Google Scholar]
- 39.Gopalan C. Vitamin A and child mortality. Bull Nutr Foundation India. 1990;11:1–3. [Google Scholar]
- 40.Kapil U, Sharma AL. Paradox of vitamin A supplementation to children in India. Indian J Public Health. 2018;49:204–24. [PubMed] [Google Scholar]
- 41.Latham MC. The great vitamin A fiasco. World Nutr. 2010;1:12–45. [Google Scholar]
- 42.Kapil U, Sachdev HP. Massive dose vitamin A programme in India – Need for a targeted approach. Indian J Med Res. 2013;138:411–7. [PMC free article] [PubMed] [Google Scholar]
- 43.NITI Ayog, Nourishing India, National nutrition strategy. New Delhi: Government of India; 2013. Government of India. [Google Scholar]
- 44.Mason J, Greiner T, Shrimpton R, Sanders D, Yukich J. Vitamin A policies need rethinking. Int J Epidemiol. 2015;44:283–92. doi: 10.1093/ije/dyu194. [DOI] [PubMed] [Google Scholar]


