Abstract
The present research investigated wall/object punching as a form of nonsuicidal self-injury (NSSI) among 1,143 veterans seeking treatment for posttraumatic stress disorder (PTSD). Wall/object punching was remarkably common in this sample (43%), and its inclusion in the definition of NSSI increased estimated prevalence of recent NSSI by 14%. As expected, wall/object punching was strongly associated with other traditional forms of NSSI, post-NSSI relief, and suicidal ideation. Male veterans and veterans with PTSD were significantly more likely to engage in wall/object punching than female veterans and veterans without PTSD. More research on this important but under-recognized form of NSSI is needed.
Keywords: nonsuicidal self-injury, suicidal ideation, self-injurious behavior
Nonsuicidal self-injury (NSSI) refers to the act of intentionally destroying one’s own body tissue for nonsuicidal purposes that are not socially sanctioned (Klonsky, 2011). Prominent models of the function of NSSI emphasize the role of both intrapersonal and interpersonal factors, including emotion regulation, self-punishment, anti-dissociation/feeling generation, and interpersonal influence (e.g., Bentley, Nock, & Barlow, 2014; Chapman, Gratz, & Brown, 2006); however, converging evidence suggests that relief from negative emotions (i.e., emotion regulation) is the most common reason that individuals provide for engaging in NSSI (e.g., Klonsky, 2007, 2011).
While NSSI was once thought to be largely restricted to female psychiatric patients (e.g., Miller, 1994), recent research demonstrates the frequent occurrence of NSSI among males (e.g., Klonsky, 2011; Selby, Kranzler, Fehling, & Panza, 2015)—particularly male veterans with posttraumatic stress disorder (PTSD; Kimbrel et al., 2014; Sacks et al., 2008). Population-based studies of NSSI suggest that there are not significant gender differences in rates of NSSI engagement (Briere & Gil, 1998; Klonsky, 2011); however, a recent meta-analysis that included many clinical and college student samples found that women were significantly more likely to engage in NSSI than men, 33.8% vs. 26.4%; OR = 1.50, p = 0.001 (Bresin & Schoenleber, 2015), although it should be noted that the overall rate of NSSI observed among the males included in this meta-analysis was quite high (26%).
Bresin and Schoenleber’s (2015) meta-analysis also revealed that women were more likely than men to engage in several specific NSSI methods, including cutting, biting, and scratching. Unfortunately, due to a lack of available studies, these researchers were not able to examine gender differences in wall/object punching—a form of NSSI that has often been overlooked by researchers and clinicians alike (Kimbrel, Calhoun, & Beckham, 2017). Providing support for the importance of further research in this area, results of a large study of NSSI among college students (N = 14,372) revealed that wall/object punching was the most common method of NSSI reported by self-injuring college-aged men (44%; Whitlock et al., 2011). This study also found that wall/object punching was significantly more common among college-aged men than women, 44% vs. 19%, OR = 3.4, p < 0.001, suggesting that wall/object punching may be a preferred NSSI method among adult men. It should be noted, however, that a sizable proportion of self-injuring college-aged women (i.e., 19%) also reported using wall/object punching as a form of NSSI in this study. Likewise, Briere and Gil’s (1998) seminal study on the form and function of NSSI found that wall/object punching was a common NSSI method that was endorsed by 40% of a predominantly female (96%) sample of self-injurers. While these studies provide solid preliminary evidence that wall/object punching is a relatively common form of NSSI in both men and women who self-injure, the vast majority of NSSI research studies to date have overlooked wall/object punching as a possible form of NSSI (Bresin & Schoenleber, 2015; Kimbrel et al., 2017).
It is likely that the relative lack of systematic research on wall/object punching (compared to other forms of NSSI) may be due, in part, to the fact that many of the most commonly used instruments to assess NSSI do not specifically assess wall/object punching as a possible NSSI method (e.g., Gratz, 2001; Nock, Holmberg, Photos, & Michel, 2007), although there are several notable exceptions (e.g., Resnick & Weaver, 1994; Whitlock, Exner-Cortens, & Purington, 2014). Thus, most studies assess wall/object punching only when participants report this behavior in the “other” category (e.g., Gratz, 2001). For example, in our 2015 study of NSSI among 151 non-treatment seeking Iraq/Afghanistan-era veterans, we found that 14% (n = 21) of veterans reported a history of NSSI on the Deliberate Self-Harm Inventory (DSHI; Gratz, 2001). Of these 21 participants, 14% (n = 3) endorsed a valid form of NSSI on the final item of the measure, which asks participants if they have ever done anything else to hurt themselves intentionally. Our initial interest in wall/object punching as a form of NSSI among male veterans stemmed from our observation that all three of the responses to this item came from male veterans who voluntarily reported (i.e., without prompting) that they punched walls, doors, and/or their motor vehicles as a means of deliberately hurting themselves. These observations, coupled with the previous work of Briere and Gil (1998) and Whitlock et al. (2011) motivated the present research.
Study Rationale and Hypotheses
Previous estimates may underestimate the true prevalence of NSSI in adult men due to biased sample selection and assessment procedures (Kimbrel et al., 2017). For example, studies of NSSI are rarely conducted in clinics and hospitals that have a high percentage of male patients with psychiatric problems [e.g., Veterans Affairs (VA) medical centers], despite the fact that the limited research in this area suggests markedly elevated rates of NSSI among male veterans seeking treatment for PTSD (e.g., Kimbrel et al., 2014; Sacks et al., 2008). Failure to systematically assess wall/object punching has also likely biased previous estimates of the prevalence of NSSI among men, given Whitlock and colleagues’ (2011) finding that wall/object punching was the most common method of NSSI (44%) reported by self- injuring college-aged men. Accordingly, the aim of the present research was to further explore the construct validity of wall/object punching as a form of NSSI in a predominantly male (96%) sample of 1,143 veterans seeking treatment for PTSD in order to increase clinicians’ and researchers’ awareness of this important but under-recognized form of NSSI.
Our first hypothesis was that inclusion of wall/object punching in the operational definition of NSSI would meaningfully increase the prevalence of NSSI in this predominantly male sample of veterans. Our second hypothesis was that wall/object punching would be positively associated with other common forms of NSSI. Our third hypothesis was that veterans who only engaged in wall/object punching would experience similar levels of post-NSSI episode relief as veterans who only engaged in traditional forms of NSSI, as relief from negative emotions is posited to be one of the key functions of NSSI (e.g., Bentley et al., 2014; Chapman et al., 2006; Klonsky, 2007, 2011). Given past research linking NSSI with suicidality (Asarnow et al., 2011; Bryan et al., 2015; Klonsky & Glenn, 2013; Kimbrel et al., 2016), including suicidal ideation (Kimbrel et al., 2014, 2015), our fourth hypothesis was that wall/object punching would demonstrate incremental validity relative to age, gender, combat exposure, PTSD diagnosis, and traditional forms of NSSI in relation to suicidal ideation. Based on the work of Whitlock et al. (2011), we also expected that male veterans would be more likely to engage in wall/object punching than female veterans (Hypothesis 5). In addition, based on our clinical observations of veterans with PTSD who self-injure, we also expected that veterans who met full diagnostic criteria for PTSD would be more likely to engage in wall/object punching than veterans without PTSD (Hypothesis 6).
Method
Participants & Procedures
Participants included 1,143 veterans seeking treatment for PTSD at the Durham VA Medical Center PTSD Clinic who were assessed for NSSI as part of the clinic’s intake procedures. Consistent with the demographic make-up of the Medical Center, most participants were male (96%; n = 1,096) and either African American (52%; n = 594) or White (44%; n = 502). On average, participants were 48.7 years of age (SD = 12.3). Approval to examine the data obtained from the clinical intake procedures of the PTSD Clinic for research purposes was provided by the Durham VA Medical Center Institutional Review Board prior to data analysis. Two previous papers by our group have reported on subsets of the participants included in the present analyses (Kimbrel et al., 2014; Sacks et al., 2008).
Measures
The Structured Clinical Interview for DSM-IV (SCID-IV; (First, Spitzer, Gibbon, & Williams, 1994) was used to assess PTSD. Because this assessment was conducted as part of standard clinical procedures, no reliability estimates were obtained; however, all interviews were conducted by trained clinicians with expertise in the assessment and treatment of PTSD among veterans. Eighty percent (n = 913) of the sample met criteria for a current diagnosis of PTSD at the time of the intake assessment. Analyses included veterans with and without PTSD so that the association between PTSD diagnosis and wall/object punching (i.e., Hypothesis 6) could be examined. The Combat Exposure Scale (CES; Keane et al., 1989) is a widely-used 7-item self-report measure that was used to assess veterans’ combat experiences. Item nine from the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) was used to assess suicidal ideation. Following the procedures of Kimbrel et al. (2014), participants endorsing a “1” or higher on this item (53.1%) were classified as having current suicidal ideation.
NSSI was assessed with the Habit Questionnaire (HQ; Resnick & Weaver, 1994), which assesses for scratching at one’s skin until it leaves a mark, cutting oneself, hitting oneself, burning oneself, and punching walls or objects. If participants endorsed any of these forms of NSSI during their lifetime, they were asked how often they had engaged in that behavior during the past two weeks using the following scale: not at all = 0; once = 1; 2–4 times = 2; 5+ times = 3. Participants endorsing a history of NSSI were also asked to report the specific forms of NSSI they had engaged in during their most recent episode and whether or not their most recent NSSI episode had resulted in relief.
Results
Descriptive Statistics
Approximately 62% (n = 705) of participants reported a lifetime history of one or more traditional forms of NSSI (i.e., scratching, cutting, burning, or hitting oneself), with 50% (n = 570) reporting engaging in traditional forms of NSSI during the past two weeks. Likewise, 69% (n = 793) of participants reported a lifetime history of wall/object punching, with 43% (n = 492) reporting wall/object punching during the past two weeks. Notably, wall/object punching was the most common form of NSSI reported during the past two weeks and over the course of participants’ lifetimes. Furthermore, consistent with Hypothesis 1, when wall/object punching was included in the operational definition of NSSI, lifetime prevalence of NSSI increased by 20% (n = 904) and the current (i.e., past two weeks) prevalence of NSSI increased by 14% (n = 734), resulting in lifetime and current rates of 82% and 64%, respectively.
Association between Wall/Object Punching and Other Forms of NSSI
Consistent with Hypothesis 2, a chi-square analysis revealed that veterans who engaged in traditional forms of NSSI were more likely to have engaged in wall/object punching than veterans who had not engaged in traditional forms of NSSI, 57.5% vs. 28.6%, χ2(1) = 97.500, p < 0.0001. In addition, the number of traditional NSSI methods veterans had engaged in during the past two weeks (coded 0–4, where 0 = no traditional NSSI during the past two weeks and 4 = engaged in all four traditional NSSI methods during the past 2 weeks) had a strong linear association with wall/object punching, χ2(4) = 173.666, p < 0.0001 (Figure 1). Notably, 100% of veterans who had engaged in all 4 traditional forms of NSSI during the past two weeks had engaged in wall/object punching during this same period of time.
Figure 1.
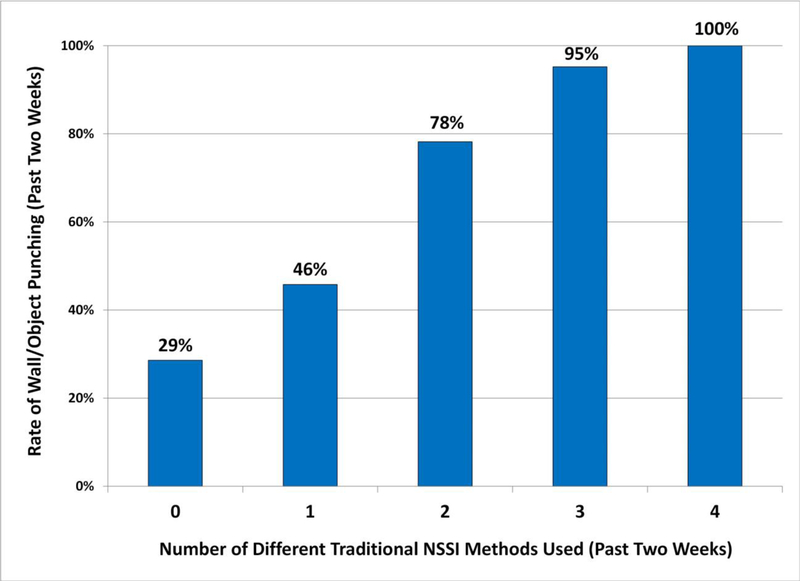
Association Between Number of Traditional NSSI Methods Used and Rate of Wall/Object Punching
Wall/Object Punching and Post-NSSI Relief
Chi-square analyses were also used to assess the association between the different forms of NSSI used during participants’ most recent NSSI episode and the presence or absence of post-NSSI relief. These analyses were limited to participants who reported engaging in NSSI during the past two weeks and provided information about their most recent NSSI episode (n = 413). Participants were placed into three groups for the purposes of these analyses including: (a) those who reported their most recent NSSI episode included traditional forms of NSSI only (n = 230); (b) those who reported their most recent NSSI episode consisted of wall/object punching only (n = 63); and (c) those who reported their most recent NSSI episode included both wall/object punching and one or more traditional forms of NSSI (n = 120). As can be seen in Figure 2, the overall chi-square test revealed significant group differences in rates of post-NSSI episode relief, χ2(2) = 15.360, p < 0.0001. Follow-up bivariate comparisons revealed that the two groups of participants who reported wall/object punching during their most recent episode did not differ significantly from each other with respect to post-NSSI episode relief, χ2(1) = 0.61, p = 0.43; however, participants who reported only engaging in traditional forms of NSSI during their most recent episode were significantly less likely to report post-NSSI episode relief than those who engaged in wall/object punching only, χ2(1) = 11.291, p = 0.001, and those who engaged in both wall/object punching and traditional NSSI methods, χ2(1) = 9.250, p = 0.002, providing support for Hypothesis 3.
Figure 2.

Association between Different Forms of NSSI and Post-NSSI Episode Relief
Wall/Object Punching and Suicidal Ideation
Hierarchical logistic regression was used to assess the incremental validity of recent wall/object punching (coded as absent vs. present) in the prediction of current suicidal ideation (a well-established and clinically meaningful correlate of traditional forms of NSSI), relative to gender, age, combat exposure, current PTSD, and recent engagement in traditional NSSI (coded as absent vs. present). As shown in Table 1, age, current PTSD, and recent engagement in traditional forms of NSSI reliably predicted suicidal ideation in the first step of the model. Consistent with Hypothesis 4, recent engagement in wall/object punching emerged as a statistically significant predictor of current suicidal ideation in the second step of the model after accounting for the effects of gender, age, combat exposure, current PTSD, and recent engagement in traditional forms of NSSI.
Table 1.
Summary of Hierarchical Logistic Regression Model Predicting Current Suicidal Ideation
| Suicidal Ideation | ||
|---|---|---|
| Step 1 | Odds Ratio | 95% Confidence Intervals |
| Age | 1.01* | 1.00 – 1.03 |
| Male Gender | 1.48 | 0.75 – 2.90 |
| Combat Exposure | 0.99 | 0.98 – 1.00 |
| Current PTSD Diagnosis | 2.13*** | 1.43 – 3.18 |
| Traditional NSSI | 2.12*** | 1.65 – 2.74 |
| Step 2 | ||
| Age | 1.02** | 1.00 – 1.03 |
| Male Gender | 1.20 | 0.60 – 2.40 |
| Combat Exposure | 0.99 | 0.98 – 1.00 |
| Current PTSD Diagnosis | 1.85** | 1.23 – 2.78 |
| Traditional NSSI | 1.67*** | 1.28 – 2.19 |
| Wall/Object Punching | 2.65*** | 2.00 – 3.49 |
Note: Gender coded as 0 = female, 1 = male.
p < 0.05
p < 0.01
p < 0.001.
Gender, PTSD, and Wall/Object Punching
Consistent with Hypothesis 5, male veterans were twice as likely as female veterans (44.0% vs. 21.7%) to have engaged in wall/object punching during the past two weeks, χ2(1) = 8.904, p = 0.003. In contrast, engagement in one or more of the four traditional forms of NSSI in the past two weeks did not differ significantly between men (49.8%) and women (52.2%), χ2(1) = 0.098, p = 0.75.
Consistent with Hypothesis 6, veterans who met full criteria for current PTSD were more likely to have engaged in wall/object punching during the past two weeks than those without PTSD, 46.3% vs. 24.8%, χ2(1) = 22.430, p < 0.0001. Veterans who met full diagnostic criteria for PTSD were also more likely to have engaged in one or more of the four traditional forms of NSSI during the past two weeks than veterans without PTSD, 51.2% vs. 41.6%, χ2(1) = 4.341, p = 0.037.
To further assess the relationship between gender, PTSD, and wall/object punching, two additional logistic regressions were conducted. Recent engagement in traditional forms of NSSI served as the dependent variable in the first model, and age, gender, combat exposure, PTSD, and recent history of wall/object punching served as predictors. Recent engagement in wall/object punching served as the dependent variable in the second model, and age, gender, combat exposure, current PTSD diagnosis, and recent history of traditional NSSI served as predictors. Consistent with Hypotheses 5 and 6, we expected that PTSD and male gender would be associated with wall/object punching in the second model.
The only reliable predictor of engagement in traditional NSSI was wall/object punching, OR = 3.32, 95% CI: 2.55–4.33, p < 0.0001. Age, gender, combat exposure, and PTSD were not reliable predictors in this model; however, consistent with Hypotheses 5 and 6—both current PTSD, OR = 2.37, 95% CI: 1.51–3.72, p < 0.0001, and male gender, OR = 3.13, 95% CI: 1.37–7.17, p = 0.007, were significant predictors of wall/object punching in the second logistic regression model along with recent engagement in traditional NSSI, OR = 3.31, 95% CI: 2.54–4.32, p < 0.0001 (Table 2).
Table 2.
Summary of Logistic Regression Models Predicting Engagement in Different Forms of NSSI
| Traditional NSSI | ||
|---|---|---|
| Odds Ratio | 95% Confidence Intervals | |
| Age | 1.00 | 0.99 – 1.02 |
| Male Gender | 0.72 | 0.37 – 1.40 |
| Combat Exposure | 1.00 | 0.99 – 1.01 |
| Current PTSD Diagnosis | 1.23 | 0.82 – 1.84 |
| Wall/Object Punching | 3.32*** | 2.55 – 4.33 |
| Wall/Object Punching | ||
| Odds Ratio | 95% Confidence Intervals | |
| Age | 1.00 | 0.98 – 1.01 |
| Male Gender | 3.13** | 1.37 – 7.17 |
| Combat Exposure | 1.01 | 1.00 – 1.02 |
| Current PTSD Diagnosis | 2.37*** | 1.51 – 3.72 |
| Traditional NSSI | 3.31*** | 2.54 – 4.32 |
Note: Gender coded as 0 = female, 1 = male.
p< 0.05
p < 0.01
p < 0.001.
Discussion
To our knowledge, the present study represents the most systematic evaluation of wall/object punching as a form of NSSI to date. As expected, we found that inclusion of wall/object punching in the operational definition of NSSI meaningfully increased the prevalence of NSSI among male veterans with PTSD (Hypothesis 1). In addition, wall/object punching was robustly associated with traditional forms of NSSI in a clear linear fashion, such that the greater number of traditional methods of NSSI used by participants, the more likely they were to also engage in wall/object punching (Hypothesis 2). Consistent with Hypothesis 3, wall/object punching was strongly associated with post-NSSI episode relief (one of the most common motives for NSSI; Gratz et al., 2015). In fact, participants who engaged in wall/object punching-only during their most recent NSSI episode were more likely to report post-NSSI episode relief than those who only engaged in traditional forms of NSSI. Support for the incremental validity of wall/object punching was provided by the finding that wall/object punching was uniquely related to current suicidal ideation, above and beyond age, gender, combat exposure, current PTSD diagnosis, and recent engagement in traditional forms of NSSI (Hypothesis 4). In addition, as expected, male veterans and veterans with PTSD were significantly more likely to engage in wall/object punching than female veterans and veterans without PTSD (Hypotheses 5 and 6). Taken together, these findings provide strong support for the construct validity of wall/object punching as a form of NSSI and highlight the need for further research on this important but under-recognized NSSI behavior.
Clinical Implications
As noted previously, one reason for past findings of lower rates of NSSI among men in clinical settings may be that wall/object punching is not systematically assessed by most available NSSI measures. Indeed, failure to assess wall/object punching in the present study would have resulted in 14% of current self-injurers in our sample not being identified correctly—a concerning oversight given emerging evidence linking NSSI to functional impairment and suicide risk (e.g., Asarnow et al., 2011; Bryan et al., 2015; Gratz et al., 2015; Selby et al., 2015). For instance, multiple studies suggest that NSSI is more strongly associated with suicide attempts than other forms of psychopathology (e.g., Klonsky & Glenn, 2013; Kimbrel et al., 2016) and is a better prospective predictor of suicide attempts than history of suicide attempts (Asarnow et al., 2011; Bryan et al., 2015). Accordingly, we strongly recommend that clinicians and researchers systematically assess wall/object punching when evaluating participants’ potential risk for suicidal and nonsuicidal self-injury. Our findings further suggest that assessment of wall/object punching is especially important when evaluating NSSI among men, as men were significantly more likely than women to engage in wall/object punching in the present study. This is not to say, however, that wall/object punching should only be assessed when working with males. Indeed, the present study found that 1 out of 5 (22%) female veterans seeking treatment for PTSD had engaged in wall/object punching during the previous two weeks, a finding that is consistent with prior research demonstrating that substantial proportions of women use wall/object punching as a means of injuring themselves (e.g., Briere & Gil, 1998; Whitlock et al., 2011).
Evidence for a strong relationship between current PTSD and wall/object punching also has important clinical implications. Currently, none of the leading evidence-based psychosocial treatments for PTSD include systematic monitoring or treatment of NSSI, and many trials of these treatments have explicitly excluded individuals with significant NSSI. Given that wall/object punching and other forms of NSSI occurs so frequently among men with PTSD, interventions that are explicitly focused on reducing NSSI among individuals with PTSD are likely to have particular clinical utility. Indeed, incorporating such interventions into standard treatments for PTSD would not only assist patients in reducing NSSI and related suicide risk, but might also increase their overall capacity for emotion regulation (see Gratz et al., 2014, 2016), which could, in turn, improve their ability to successfully cope with PTSD symptoms.
Finally, the finding that wall/object punching was more likely to result in relief than traditional forms of NSSI highlights the particular clinical relevance that this specific form of NSSI may have for treatment outcome. In particular, given literature implicating negative reinforcement in the form of emotional relief as a key maintenance factor for NSSI (Chapman et al., 2006; Gratz et al., 2016), our findings suggest that wall/object punching may be a particularly reinforcing and intractable form of NSSI to treat. The substantial risk for significant tissue and bone damage due to wall/object punching also makes careful monitoring of this form of NSSI especially warranted.
Limitations
The present findings must be interpreted within the context of several limitations. First, these findings are cross-sectional and based on self-report. Future research would benefit from longitudinal approaches and the use of clinical interviews and laboratory assessments of NSSI and its consequences (e.g., Gratz et al., 2015, 2016). Second, our sample was a predominantly male, treatment-seeking sample of veterans. Thus, the degree to which the present findings might generalize to other clinical populations or the general population is unclear. In addition, epidemiological work is still needed to determine the prevalence of wall/object punching among youth and adults in general. Finally, our diagnostic and assessment battery was fairly limited in the present research, so we were unable to determine the influence that other relevant psychiatric diagnoses (e.g., borderline personality disorder diagnosis) and psychological constructs (e.g., impulsivity) may have had on the present findings.
Conclusion
The current findings support the construct validity of wall/object punching as a form of NSSI by demonstrating that wall/object punching is strongly associated with traditional forms of NSSI, reported relief from negative affect, and current suicidal ideation. Wall/object punching also appears to be particularly common among male veterans with PTSD—a population that has not traditionally been studied by NSSI researchers. Taken together, these findings suggest the need for both clinicians and researchers to systematically assess for wall/object punching and other forms of NSSI as a part of a comprehensive approach to risk assessment and management, even when working with groups of patients who are not traditionally viewed as being at elevated risk for NSSI.
Acknowledgements
Support for this research was provided by Award #I01CX001486 and Award #IK2CX000525 to Dr. Kimbrel from the Clinical Science Research and Development (CSR&D) Service of the Department of Veterans Affairs Office of Research and Development (VA ORD) as well as a VA VISN 17 New Investigator Award to Dr. Kimbrel entitled “Genetic and Environmental Effects on PTSD, Depression, and Alcohol Misuse.” Dr. Beckham was supported by Award #11S-RCS-009 from the CSR&D Service of VA ORD. Mr. Hicks was supported by Award #R01CA196304–02S1 from the National Cancer Institute of the National Institutes of Health. This research was also supported in part by the VA Mid- Atlantic Mental Illness Research, Education and Clinical Center (MIRECC) and the Research and Development and Mental Health Services of the Durham VA Medical Center. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government.
References
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, … Brent DA (2011). Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: findings from the TORDIA study. Journal of the American Academy of Child and Adolescent Psychiatry, 50(8), 772–781. doi: 10.1016/j.jaac.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown G (1996). Beck Depression Inventory-II San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Bentley KH, Nock MK, & Barlow DH (2014). The four-function model of nonsuicidal self-injury: Key directions for future research. Clinical Psychological Science, 2, 638–656. [Google Scholar]
- Bresin K, & Schoenleber M (2015). Gender differences in the prevalence of nonsuicidal self-injury: A meta-analysis. Clinical Psychology Review, 38, 55–64. [DOI] [PubMed] [Google Scholar]
- Briere J, & Gil E (1998). Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. The American Journal of Orthopsychiatry, 68(4), 609–620. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD, Wertenberger E, Young-McCaughon S, & Peterson A (2015). Nonsuicidal self-injury as a prospective predictor of suicide attempts in a clinical sample of military personnel. Comprehensive Psychiatry, 59, 1–7. doi: 10.1016/j.comppsych.2014.07.009 [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, & Brown MZ (2006). Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behav Res Ther, 44, 371–394. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1994). Structured Clinical Interview for Axis I DSM-IV Disorders (Version 2nd). New York, NY: Biometrics Research Department. [Google Scholar]
- Gratz KL (2001). Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology & Behavioral Assessment, 23(4), 253–263. doi: 10.1023/A:1012779403943 [DOI] [Google Scholar]
- Gratz KL, Chapman AL, Dixon-Gordon KL, & Tull MT (2016). Exploring the association of deliberate self-harm with emotional relief using a novel Implicit Association Test. Personality Disorders: Theory, Research, and Treatment, 7, 91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Dixon-Gordon KL, Chapman AL, & Tull MT (2015). Diagnosis and Characterization of DSM-5 Nonsuicidal Self-Injury Disorder Using the Clinician-Administered Nonsuicidal Self- Injury Disorder Index. Assessment, 22(5), 527–539. doi: 10.1177/1073191114565878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Moore KE, & Tull MT (2016). The role of emotion dysregulation in the presence, associated difficulties, and treatment of borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 7, 344–353. doi: 10.1037/per0000198 [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, & Levy R (2014). Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine, 44, 2099–2112. [DOI] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, & Mora CA (1989). Clinical evaluation of a measure to assess combat exposure. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1, 53–55. doi: 10.1037/1040-3590.1.1.53 [DOI] [Google Scholar]
- Kimbrel NA, Calhoun PS, & Beckham JC (2017). Nonsuicidal self-injury in men: A serious problem that has been overlooked for too long. World Psychiatry, 16, 108–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Gratz KL, Tull MT, Morissette SB, Meyer EC, DeBeer BB, Silvia PJ, Calhoun PC, & Beckham JC (2015). Non-suicidal self-injury as a predictor of active and passive suicidal ideation among Iraq/Afghanistan veterans. Psychiatry Research, 227, 360–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, & Morissette SB (2016). Nonsuicidal self- injury and suicide attempts in Iraq/Afghanistan war veterans. Psychiatry Research, 243, 232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Johnson ME, Clancy C, Hertzberg M, Collie C, Van Voorhees EE, … Beckham JC (2014). Deliberate self-harm and suicidal ideation among male Iraq/Afghanistan-era veterans seeking treatment for PTSD. Journal of Traumatic Stress, 27(4), 474–477. doi: 10.1002/jts.21932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED (2007). The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review, 27, 226–239. [DOI] [PubMed] [Google Scholar]
- Klonsky ED (2011). Non-suicidal self-injury in United States adults: Prevalence, sociodemographics, topography and functions. Psychological Medicine, 41(9), 1981–1986. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, & Glenn CR (2013). The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. Journal of Abnormal Psychology, 122(1), 231–237. doi: 10.1037/a0030278 [DOI] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. doi: 10.1037/1040-3590.19.3.309 [DOI] [PubMed] [Google Scholar]
- Miller D (1994). Women Who Hurt Themselves New York: Basic Books. [Google Scholar]
- Resnick HS, & Weaver T (1994). Habit Questionnaire. Unpublished mansucript Charleston, SC: Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston SC. [Google Scholar]
- Sacks MB, Flood AM, Dennis MF, Hertzberg MA, & Beckham JC (2008). Self-mutilative behaviors in male veterans with posttraumatic stress disorder. Journal of Psychiatric Research, 42(6), 487–494. doi: 10.1016/j.jpsychires.2007.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Kranzler A, Fehling KB, & Panza E (2015). Nonsuicidal self-injury disorder: The path to diagnostic validity and final obstacles. Clinical Psychology Review, 38, 79–91. doi: 10.1016/j.cpr.2015.03.003 [DOI] [PubMed] [Google Scholar]
- Whitlock J, Exner-Cortens D, & Purington A (2014). Assessment of nonsuicidal self-injury: Development and initial validation of the Non-Suicidal Self-Injury–Assessment Tool (NSSI-AT). Psychological Assessment, 26(3), 935. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Muehlenkamp J, Purington A, Eckenrode J, Barreira P, Baral Abrams G, … Chin C (2011). Nonsuicidal self-injury in a college population: General trends and sex differences. Journal of American College Health, 59(8), 691–698. [DOI] [PubMed] [Google Scholar]


