Abstract
Objectives:
The high predictive validity of self-rated health (SRH) is a major strength of this widely used population health measure. Recent studies, however, noted that the predictive validity varies across population subgroups. The aim of this study is to examine respondents’ age as a moderator of SRH predictive validity with respect to subsequent mortality risk.
Method:
Using data from the National Health Interview Survey–Linked Mortality Files (NHIS-LMF) 1986–2006, we estimate Cox proportional hazard models of all-cause and cause-specific mortality for adults aged 45–84 years as a function of their health ratings ( N = 574,008).
Results:
The data show significant age moderation of the predictive validity of SRH across all levels of ratings: the hazard ratios for mortality decline by about a half between the ages of 50 and 80 years. This attenuation appears primarily among earlier birth cohorts; there is no significant age attenuation in more recent cohorts—however, this may be in part attributed to the earlier ages when the respondents are observed.
Discussion:
The findings of declining predictive validity of SRH across age imply that individuals may evaluate their health differently as they age. The results also suggest caution in using SRH to capture age-related health changes in the older population.
Keywords: Age, Birth cohorts, Mortality, Predictive validity, Self-rated health, U.S. adults
How does age moderate the predictive validity of self-rated health (SRH)? SRH has been widely used for more than half a century to measure health status, trends, and disparities ( Jylhä, 2009 ). Numerous studies have established the high predictive validity of SRH for mortality ( Idler & Benyamini, 1997 ). More recently, however, researchers noted systematic group differences in the SRH–mortality association. SRH predicts mortality better among men, non-Hispanic Whites, and adults with higher socioeconomic status (SES) than among women, minorities, and respondents with lower SES, respectively ( Benyamini & Idler, 1999 ; Dowd & Zajacova, 2007 ; Lee et al., 2007 ).
An important potential moderator of the SRH–mortality relationship is age. Age is a key predictor of health status, as well as mortality, and may thus influence the relationship between the two. There is a well-developed body of research on the determinants of the health judgment in older adults. Older respondents are known to evaluate their health differently—more positively—compared with younger respondents ( Idler, 1993 ). This may occur if older adults rely on peer comparisons and thus form their judgment relative to the high level of health problems among their age peers ( Leinonen, Heikkinen, & Jylhä, 2001 ). Older adults also seem to weigh their mental/social well-being more heavily in their health ratings ( French, Sargent-Cox, & Luszcz, 2012 ; Schneider et al., 2004 ; Schnittker, 2005 ).
The predictive validity depends, however, not on the average level of SRH in a sample but on the relative position of thresholds respondents use to delineate the categories. At the same time, the evidence of age-related changes in the average level of SRH suggests that age may also moderate the relative categories within SRH, or the placement of thresholds across categories of SRH, which would result in a changed predictive validity of SRH vis-à-vis mortality. If respondents change their ratings more at some levels of health than at other levels, then SRH may become better or worse at distinguishing the underlying health status and the SRH–mortality link may become stronger or weaker with age.
The question of validity of the SRH measure is critical. Given its extensive use in aging research and clinical practice, lower predictive validity among older adults would mean that health reports by these participants may not be as useful for capturing their actual health status and future health needs as health assessments of younger patients. In addition, SRH is often used in longitudinal research to measure health changes. If respondents rate their health differently as they age, then the observed changes in SRH may be biased. More broadly, understanding how age moderates the SRH validity contributes to the important task of learning what the health ratings capture. Systematic age differences suggest that respondents alter the evaluation process as they age, and we can glean insight into whether their evaluation process becomes more finely tuned to their physical health or less so. This in turn can be used in further work to drill down into what exactly the SRH captures—a key question in our aging society where the health status of older adults is of immense public interest.
Surprisingly little work examined age as a moderator of the predictive validity of SRH. Two analyses of European adults found SRH to be a weaker predictor of mortality in older respondents ( Helweg-Larsen, Kjøller, & Thoning, 2003 ; van Doorslaer & Gerdtham, 2003 ). In contrast, Korean respondents aged 65 and older evidenced a slightly stronger SRH–mortality association than did adults aged 35–64 years ( Khang & Kim, 2010 ). In the United States, SRH collected in the early 1970s predicted mortality among middle-aged men but not among older men or women of any age, net of detailed information on the diagnosed conditions Idler and Angel (1990) . We believe that a comprehensive examination of the moderating impact of age is overdue, especially given substantially improved health conditions and longevity of older adults over the last few decades.
When examining age patterns in the SRH–mortality associations, other time dimensions—especially birth cohorts—need to be considered as potential confounders. Older respondents come from earlier birth cohorts, and cohorts could also drive systematic differences in the SRH evaluation process. Health literacy, for instance, is higher in more recent cohorts, which could contribute to a better understanding of one’s health and more precise SRH judgments. The overall health levels have increased across birth cohorts, changing the peer reference groups’ health and thus possibly the respondents’ own health evaluation as well ( Idler, 1993 ).
In this study, we use a large, nationally representative data with up to 20 years of follow up to present a comprehensive analysis of age variation in the predictive power of SRH on mortality. To the best of our knowledge, this is the first such analysis for the U.S. population since 1990. SRH is used in aging research and clinical work alike as a holistic indicator of general health. It is therefore imperative to know whether SRH predicts longevity the same way at different ages.
Methods
Data
We used data from the National Health Interview Survey–Linked Mortality Files (NHIS-LMF) 1986–2006. The NHIS is a large, annual cross-sectional survey of the noninstitutionalized U.S. population. The NHIS-LMF links adult respondents interviewed during the period of 1986–2004 to mortality records in the National Death Index through 2006.
The analytic sample includes respondents aged 45–84 years at the time of the interview. The upper age limit was selected because the NHIS top-coded age at 85 years since the 1997 survey. The lower limit captures adults in middle adulthood and excludes fewer than 5% of deaths that occur at younger ages ( Arias, 2010 ). We excluded 2,094 respondents (0.4%) who were missing SRH information. The final sample comprised 574,008 respondents.
Measures
SRH and age were the key predictors. SRH was measured on a 5-point scale from excellent (reference) to poor . Age was measured in single years. For age-stratified analysis, age was categorized in decades (45–54, 55–64, 65–74, and 75–84 years). Models with age by SRH interaction terms had age centered on 65 years and measured in decades in order to obtain more easily interpretable hazard ratios.
All-cause mortality and cause-specific mortality comprised the outcomes. For cause-specific mortality, we included leading causes of death: heart disease, cancer, respiratory disease, cerebrovascular disease, diabetes, and accidents.
Covariates included gender; race/ethnicity, categorized as non-Hispanic White (reference), non-Hispanic Black, Hispanic, and other; Census region of residence, coded as Northeast (reference), Midwest, South, and West; the year of interview; marital status, categorized as married (reference), divorced, widowed, and never married; and educational attainment, coded as less than high school, high school and some college, and bachelor’s degree or higher. Finally, birth cohort–stratified analyses grouped birth years into 15-year intervals.
Analysis
We estimated a series of Cox proportional hazard (PH) models of all-cause and cause-specific mortality as a function of SRH. Duration of follow up was in 3-month increments. The Cox PH model is the most widely used approach to survival analysis and is optimal for our research questions. First, we stratified the sample by 10-year age groups to evaluate the association between SRH and mortality across age categories. Second, all-sample models that included SRH by age interaction terms tested whether age was a significant moderator of the SRH–mortality association. Further Cox PH models were estimated for cause-specific mortality and with additional covariates. Next, we considered the role of birth cohorts, estimating Cox PH models stratified by three birth cohort groups. Finally, to get a more complete picture of the age–period–cohort patterns, we estimated Cox PH models of all-cause mortality on dichotomized SRH (poor/fair vs excellent to good) separately for each combination of interview year and 2-year age groups (340 models for each gender, from a model for respondents interviewed in 1986 at ages of 45–46 years to a model for respondents interviewed in 2002 at ages of 83–84 years), captured the hazard ratios from these models, and smoothed them to a 3D surface using generalized additive models ( Wood, 2006 ). The resulting figures display the age–period–cohort pattern in the predictive validity of SRH on mortality. The Supplementary Material shows all analyses conducted separately by sex because of previous research that showed large sex differences in the SRH–mortality links ( Benyamini, Blumstein, Lusky, & Modan, 2003 ). All Cox PH models were adjusted for the NHIS-LMF complex sampling design and estimated using Stata 13.0.
Results
Table 1 shows sample characteristics at the interview and mortality follow-up information. The distribution of SRH varied by age: about 30% of respondents aged 45–64 years reported excellent health and 31% reported very good health compared with 13% and 22% among respondents aged 75–84 years, respectively. During the follow up, 7% of the adults aged 45–54 years died compared with 57% of the oldest group. Supplementary Table 1 shows all covariates and follow-up information, including the distribution of causes of death.
Table 1.
Characteristics of the National Health Interview Survey–Linked Mortality Files (NHIS-LMF) Analysis Sample, by Age Group ( N = 574,008)
| 45–54 years | 55–64 years | 65–74 years | 75–84 years | |
|---|---|---|---|---|
| Proportion of the sample (%) | 37.7 | 27.5 | 22.0 | 12.8 |
| Self-rated health (%) | ||||
| Excellent | 30.3 | 22.9 | 16.8 | 12.5 |
| Very good | 30.8 | 27.0 | 24.8 | 22.5 |
| Good | 26.2 | 29.8 | 33.7 | 34.1 |
| Fair | 9.2 | 13.7 | 17.6 | 21.4 |
| Poor | 3.6 | 6.5 | 7.3 | 9.6 |
| Follow-up information | ||||
| Died during follow up (%) | 7.3 | 18.4 | 37.4 | 56.7 |
| Duration of follow up ( SE ) | 10.4 (.04) | 10.3 (.04) | 9.3 (.04) | 7.1 (.03) |
| N | 215,279 | 158,385 | 128,066 | 72,278 |
Note. Source: NHIS-LMF 1986–2006. Descriptive statistics adjusted for complex sample design. Descriptive statistics for all covariates and follow-up information are given in Supplementary Table 1 .
Table 2 summarizes results from age- and gender-adjusted Cox PH models stratified by 10-year age groups. The results corroborate the strong link between health ratings and mortality: the SRH hazard ratios are significant in all age groups, meaning that any health rating worse than excellent predicts significantly higher mortality hazard than the excellent reference. There is a clear stepwise pattern across the models, however, whereby the hazard ratios are smaller for older respondents at each level of SRH relative to excellent . For instance, at ages of 45–54 years, respondents who evaluated their health as good had 2.5 times the hazard of dying compared with those in excellent health; the hazard was 1.6 times higher among respondents aged 75–84 years. Across all SRH levels from very good to poor , the predictive power declined by more than a half between the ages of 50 and 80 years.
Table 2.
Hazard Ratios of Age-Adjusted All-Cause Mortality on Self-Rated Health (SRH), by Age Group
| 45–54 years | 55–64 years | 65–74 years | 75–84 years | |
|---|---|---|---|---|
| SRH (ref. = excellent ) | ||||
| Very good | 1.46*** | 1.22*** | 1.27*** | 1.20*** |
| Good | 2.49*** | 1.94*** | 1.97*** | 1.60*** |
| Fair | 5.61*** | 4.23*** | 3.44*** | 2.51*** |
| Poor | 14.52*** | 10.11*** | 7.84*** | 4.69*** |
| Covariates | ||||
| Age | 1.07*** | 1.08*** | 1.08*** | 1.09*** |
| Female | 0.60*** | 0.62*** | 0.58*** | 0.59*** |
Notes. ref. = reference. Hazard ratios from age-adjusted Cox proportional hazard models are shown. All estimates are adjusted for the complex sampling design of the National Health Interview Survey.
*** p < .001.
Table 3 tests whether these age patterns are statistically significant and whether they can be explained by key demographic and socioeconomic characteristics of the respondents. Results from Model 1 answer the first question: the moderating impact of age is statistically significant (all age by SRH interaction terms are significant). Models 2 and 3 show that the influence of age is not due to sociodemographic differences in respondent characteristics: the interaction terms (and the main SRH terms) remain largely unchanged when controlling for race/ethnicity, region, interview year, marital status, and education.
Table 3.
Hazard Ratios of All-Cause Mortality on Self-Rated Health (SRH) by Age With Covariates, ( N = 574,008)
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| SRH (ref. = excellent ) | |||
| Very good | 1.28*** | 1.28*** | 1.27*** |
| Good | 1.97*** | 1.97*** | 1.96*** |
| Fair | 3.75*** | 3.76*** | 3.67*** |
| Poor | 8.58*** | 8.59*** | 8.25*** |
| SRH by age a | |||
| Very good * age | 0.95* | 0.95* | 0.96* |
| Good * age | 0.87*** | 0.87*** | 0.88*** |
| Fair * age | 0.76*** | 0.76*** | 0.78*** |
| Poor * age | 0.67*** | 0.67*** | 0.69*** |
| Covariates | |||
| Age a | 2.66*** | 2.65*** | 2.58*** |
| Female | 0.60*** | 0.60*** | 0.55*** |
| Race/ethnicity (ref. = non-Hispanic White) | |||
| Non-Hispanic Black | 1.09*** | 1.02 | |
| Hispanic | 0.74*** | 0.72*** | |
| Other | 0.73*** | 0.72*** | |
| Region (ref. = Northeast) | |||
| Midwest | 0.99 | 1.00 | |
| South | 0.96** | 0.97 | |
| West | 0.96* | 0.97 | |
| Survey year | 0.99*** | 0.99*** | |
| Marital status (ref. = married) | |||
| Divorced/separated | 1.38*** | ||
| Widowed | 1.25*** | ||
| Never married | 1.44*** | ||
| Education (ref. = high school) | |||
| Less than high school | 1.00 | ||
| Some college or more | 0.92*** | ||
Notes. ref. = reference. Hazard ratios from Cox proportional hazard models are shown. All estimates are adjusted for the complex sampling design of the National Health Interview Survey.
a Age is centered on 65 years and incremented in decades in order to obtain easier-to-interpret sizes of the main and interaction terms.
* p < .05. ** p < .01. *** p < .001.
Table 4 shows results from six cause-specific PH models. All but three of the 24 SRH by age interaction terms are statistically significant and all are in the same direction: older respondents have a lower predictive validity of SRH compared with younger respondents for all major causes of death.
Table 4.
Cox Proportional Hazard (PH) Models of Cause-Specific Mortality on Self-Rated Health (SRH) by Age
| CVD | Respiratory | Cancer | Cerebrovascular | Diabetes | Accidents | |
|---|---|---|---|---|---|---|
| SRH (ref. = excellent ) | ||||||
| Very good | 1.27*** | 1.40*** | 1.09*** | 1.30*** | 1.76*** | 1.04 |
| Good | 1.82*** | 2.14*** | 1.35*** | 1.80*** | 2.97*** | 1.26*** |
| Fair | 3.17*** | 4.15*** | 1.81*** | 2.64*** | 7.05*** | 1.77*** |
| Poor | 5.60*** | 9.34*** | 2.99*** | 4.30*** | 14.93*** | 2.75*** |
| SRH by age a | ||||||
| Very good * age | 0.93*** | 0.86*** | 0.94*** | 0.93 | 0.84* | 0.93 |
| Good * age | 0.85*** | 0.76*** | 0.88*** | 0.85*** | 0.75*** | 0.93 |
| Fair * age | 0.73*** | 0.65*** | 0.80*** | 0.74*** | 0.63*** | 0.80*** |
| Poor * age | 0.63*** | 0.58*** | 0.76*** | 0.68*** | 0.58*** | 0.70*** |
| Covariates | ||||||
| Age a | 3.33*** | 3.69*** | 2.03*** | 3.78*** | 2.64*** | 1.86*** |
| Female | 0.58*** | 0.59*** | 0.61*** | 0.84*** | 0.80*** | 0.47*** |
Notes. CVD = cardiovascular disease; ref. = reference. Hazard ratios from age-adjusted Cox PH models are shown. All estimates are adjusted for the complex sampling design of the National Health Interview Survey.
a Age is centered on 65 years and incremented in decades in order to obtain easier-to-interpret sizes of the main and interaction terms.
* p < .05. *** p < .001.
Finally, Table 5 disaggregates by birth cohort and shows that the diminishing predictive validity of SRH with age occurs primarily (or only) in the older birth cohort; the moderating impact of age on more recent birth cohorts is largely not significant, with hazard ratios of the interaction terms close to 1 in absolute size.
Table 5.
Cox Proportional Hazard (PH) Models of All-Cause Mortality on Self-Rated Health (SRH) by Age, Stratified by 15-Year Birth Cohorts
| 1910–1924 | 1925–1939 | 1940–1955 | |
|---|---|---|---|
| SRH (ref. = excellent ) | |||
| Very good | 1.33*** | 1.30*** | 1.36 |
| Good | 2.12*** | 2.03*** | 2.07*** |
| Fair | 3.39*** | 4.06*** | 5.22*** |
| Poor | 8.90*** | 9.23*** | 12.20*** |
| SRH by age a | |||
| Very good * age | 0.91 | 1.08 | 0.96 |
| Good * age | 0.81*** | 1.04 | 0.89 |
| Fair * age | 0.80*** | 0.93 | 0.97 |
| Poor * age | 0.63*** | 0.88* | 0.89 |
| Covariates | |||
| Age a | 2.69*** | 2.13*** | 2.06*** |
| Female | 0.59*** | 0.61*** | 0.60*** |
Notes. ref. = reference. Hazard ratios from Cox PH models are shown. All estimates are adjusted for the complex sampling design of the National Health Interview Survey. The mortality hazards by SRH converge with duration. The maximum and average durations were necessarily shorter in the more recent interview waves and thus, to some degree, among younger birth cohorts than in the older interview waves and thus older cohorts. This effect obviously affects cohort-stratified results more than all-sample results. To equalize duration across cohorts and eliminate its confounding, we estimated cohort-stratified models for 5-year follow up. Results from unrestricted follow up, available in the Supplementary Material , also show no significant moderating effect of age in younger cohorts.
a Age is centered on 65 years and incremented in decades in order to obtain easier-to-interpret sizes of the main and interaction terms.
* p < .05. *** p < .001.
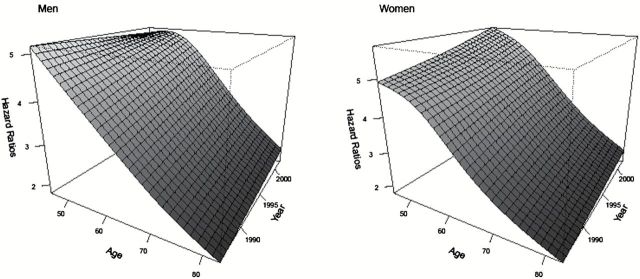
Figure 1 shows the age by period patterns in the predictive validity of dichotomized SRH on all-cause mortality for men and women. The predominant pattern in both genders is the diminishing predictive power of SRH across age at all time periods.
Figure 1.
Hazard ratios of mortality for poor/fair self-rated health (SRH) by age and period. The plots show the hazard ratios for poor/fair SRH relative to excellent-to-good SRH. The hazard ratios are captured from Cox proportional hazard models estimated separately for each age/time period combination, and the surface is smoothed using Generalized Additive Models.
Discussion
The findings reveal a strong moderating impact of age on the predictive validity of SRH among U.S. adults aged 45–84 years: SRH predicts mortality significantly better at younger ages than at older ages. The age effect is substantively large: SRH, at all levels from very good to poor , has at least twice as large hazard ratios for adults assessing their health at ages of 45–54 years than at ages of 75–84 years. For instance, respondents aged 45–54 years who rate their health as poor have about 5 times the hazard of dying compared with respondents with excellent health; the hazard declines to 2.2 among respondents aged 80 years.
The moderating influence of age was not explained by race/ethnic composition, region of residence, marital status, or educational attainment. Also, the age effect was not driven by only some causes of death but occurred across all leading causes of death. In fact, it is noteworthy that although the main effects of SRH (predictive validity at age 65 years) vary tremendously across different causes of death, the modifying effect of age is relatively similar across the causes. Additional analyses shown in the Supplementary Material show that period (year of interview) also did not have a pronounced influence on the age moderation, although later time periods were associated with stronger overall SRH hazard ratios as others found ( Schnittker & Bacak, 2014 ).
The age moderation was evident primarily among older birth cohorts. Specifically, the moderating effect was strong and significant in cohorts born during the period of 1910–1924, whereas in younger birth cohorts, age did not lower the predictive validity of SRH. This finding has potential important implications for the utility of health judgments among older adults. It suggests that adults from more recent cohorts form their health judgments in such a way that they are comparable across age. This would make SRH a particularly useful measure for capturing age-related health changes in the population and for predicting longevity even among elderly respondents. However, there is an alternative explanation of the cohort effects that will need to be examined in future studies: the age effects may be more pronounced at the oldest ages. The more recent birth cohorts were interviewed while individuals were middle-aged or young-old, when conceivably the age effect is not pronounced.
We note several limitations of this study. With respect to data, only noninstitutionalized U.S. adults are included, resulting in positively health-selected older respondents. This selection could influence the SRH values of the oldest respondents ( Idler, 1993 ), but given the low institutionalization rate of adults younger than 85 years of age, we do not believe that this phenomenon is likely to substantially bias the findings. With respect to the interpretation of the findings, we were not able to fully resolve the discrepant findings from the cohort-stratified models that suggested no moderating impact of age in younger cohorts versus the results from the age-and-period–stratified models ( Figure 1 ) that seemed to show a clear impact of age even in more recent time periods and cohorts. Additional years of follow up will help to clarify the age patterns among the more recent birth cohorts in the future. Finally, the predictive validity of SRH for mortality was captured by examining relative risks. This perspective is well suited for the question. However, the absolute (average) mortality hazard increases sharply in old age, and this presents a methodological quandary. When baseline hazard is low, then even relatively small absolute difference in hazards translates into sizeable relative hazard ratios. In contrast, when the absolute baseline hazard is high, then even large absolute hazard differences may not translate into large relative coefficients. A part of the age-moderation effects may thus be attributable to this methodological consideration. This alternative explanation needs to be addressed by examining concurrent validity of SRH with respect to numerous objective health indicators with varied baseline prevalence rates across age.
This study contributes to the literature on the predictive validity of SRH by providing new evidence that respondents, especially those born in older cohorts, may form their health evaluation in a systematically different way as they age such that their health judgments become less discriminating and less able to predict longevity. This interpretation of the findings should be recognized by health researchers and practitioners. They should be more cautious about using the SRH information to determine the overall health status among the older adults. The results further suggest that we also need to exercise caution when comparing health ratings of older adults across different ages because their ratings may not be fully comparable—in other words, some of the differences may be due to systematic reporting tendencies. This study presents a unique contribution to the body of research on how respondents form their health judgment: the thresholds across the levels of SRH appear to shift across age groups. This finding may be leveraged in future studies by examining how older adults determine the thresholds and thus help understand how health ratings are formed and what they mean.
Funding
None.
Supplementary Material
Acknowledgments
A. Zajacova and H. Woo jointly planned this study. A. Zajacova was responsible for analyses and drafting the paper; H. Woo contributed to designing the analytic plan and revised the manuscript.
We have received many useful comments during the process of writing and revising this study. In particular, we thank Ellen Idler, Tetyana Pudrovska, the three anonymous reviewers, as well as the Journal Editors, for their insightful questions and suggestions.
References
- Arias E . ( 2010. ). United States Life Tables, 2006 . National vital statistics reports . ( Vol. 58 ). Hyattsville, MD: : National Center for Health Statistics; . [PubMed] [Google Scholar]
- Benyamini Y. Blumstein T. Lusky A. , & Modan B . ( 2003. ). Gender differences in the self-rated health–mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? The Gerontologist , 43 , 396 – 405 . doi:10.1093/geront/43.3.396 [DOI] [PubMed] [Google Scholar]
- Benyamini Y. , & Idler E. L . ( 1999. ). Community studies reporting association between self-rated health and mortality: Additional studies, 1995 to 1998 . Research on Aging , 21 , 392 – 401 . doi:10.1177/0164027599213002 [Google Scholar]
- Dowd J. B. , & Zajacova A . ( 2007. ). Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? International Journal of Epidemiology , 36 , 1214 – 1221 . doi:10.1093/ije/dym214 [DOI] [PubMed] [Google Scholar]
- French D. J. Sargent-Cox K. , & Luszcz M. A . ( 2012. ). Correlates of subjective health across the aging lifespan: Understanding self-rated health in the oldest old . Journal of Aging and Health , 24 , 1449 – 1469 . doi:10.1177/0898264312461151 [DOI] [PubMed] [Google Scholar]
- Helweg-Larsen M. Kjøller M. , & Thoning H . ( 2003. ). Do age and social relations moderate the relationship between self-rated health and mortality among adult Danes? Social Science & Medicine , 57 , 1237 – 1247 . doi:10.1016/S0277-9536(02)00504-X [DOI] [PubMed] [Google Scholar]
- Idler E. L . ( 1993. ). Age differences in self-assessments of health: Age changes, cohort differences, or survivorship? Journal of Gerontology , 48 , 289 – 300 . doi:10.1093/geronj/48.6.S289 [DOI] [PubMed] [Google Scholar]
- Idler E. L. , & Angel R. J . ( 1990. ). Self-rated health and mortality in the NHANES-I Epidemiological Follow-up Study . American Journal of Public Health , 80 , 446 – 452 . doi:10.2105/AJPH.80.4.446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E. L. , & Benyamini Y . ( 1997. ). Self-rated health and mortality: A review of twenty-seven community studies . Journal of Health and Social Behavior , 38 , 21 – 37 . [PubMed] [Google Scholar]
- Jylhä M . ( 2009. ). What is self-rated health and why does it predict mortality? Towards a unified conceptual model . Social Science & Medicine , 69 , 307 – 316 . doi:10.1016/j.socscimed.2009.05.013 [DOI] [PubMed] [Google Scholar]
- Khang Y.-H. , & Kim H . ( 2010. ). Self-rated health and mortality: gender- and age-specific contributions of explanatory factors in South Korea . International Journal of Public Health , 55 , 279 – 289 . doi:10.1007/s00038-010-0121-z [DOI] [PubMed] [Google Scholar]
- Lee S. J. Moody-Ayers S. Y. Landefeld C. S. Walter L. C. Lindquist K. Segal M. R. , & Covinsky K. E . ( 2007. ). The relationship between self-rated health and mortality in older Black and White Americans . Journal of the American Geriatrics Society , 55 , 1624 – 1629 . doi:10.1111/j.1532-5415.2007.01360.x [DOI] [PubMed] [Google Scholar]
- Leinonen R. Heikkinen E. , & Jylhä M . ( 2001. ). Predictors of decline in self-assessments of health among older people—a 5-year longitudinal study . Social Science & Medicine , 52 , 1329 – 1341 . doi:10.1016/S0277-9536(00)00249-5 [DOI] [PubMed] [Google Scholar]
- Schneider G. Driesch G. Kruse A. Wachter M. Nehen H.-G. , & Heuft G . ( 2004. ). What influences self-perception of health in the elderly? The role of objective health condition, subjective well-being and sense of coherence . Archives of Gerontology and Geriatrics , 39 , 227 – 237 . doi:10.1016/j.archger.2004.03.005 [DOI] [PubMed] [Google Scholar]
- Schnittker J . ( 2005. ). When mental health becomes health: age and the shifting meaning of self-evaluations of general health . The Milbank Quarterly , 83 , 397 – 423 . doi:10.1111/j.1468-0009.2005.00407.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker J. , & Bacak V . ( 2014. ). The increasing predictive validity of self-rated health . PLoS One , 9 , 1 – 11 . doi:10.1371/journal.pone.0084933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doorslaer E. , & Gerdtham U.-G . ( 2003. ). Does inequality in self-assessed health predict inequality in survival by income? Evidence from Swedish data . Social Science & Medicine , 57 , 1621 – 1629 . doi:10.1016/S0277-9536(02)00559-2 [DOI] [PubMed] [Google Scholar]
- Wood S. N . ( 2006. ). Generalized additive models: An introduction with R . Boca Raton, FL: : Chapman & Hall; . [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.