Abstract
Introduction:
Hippotherapy has recently emerged as a horse-based rehabilitative therapy to improve balance, coordination, and strength in patients with a wide range of medical conditions. Although several studies have demonstrated its effectiveness in restoring balance and gait in patients who have suffered cerebrovascular accidents (CVA), few studies have reported on adverse events associated with the treatment.
Case Presentation:
This case report describes a female post-stroke patient who fell from a horse during a hippotherapy session. She suffered a closed right zygomaticomaxillary complex fracture and ruptured globe injury. The patient’s orbital injuries were surgically repaired, yet ultimately left her with no light perception in the affected eye and required enucleation.
Conclusion:
Ocular and orbital injuries following hippotherapy are potentially blinding yet preventable. As such, practitioners should weigh the risks and benefits of hippotherapy, particularly in patients with unstable gait, and advise that additional safety precautions are taken to avoid these devastating injuries.
Keywords: Equine-Assisted Therapy, Accidental Falls, Eye Injuries
Introduction
Hippotherapy is a horse-based rehabilitative therapy that utilizes natural equine movements to improve a patient’s balance, coordination, and strength. Although its origins date back to the 1960’s, hippotherapy has more recently emerged as an adjunctive therapy for patients with a host of medical conditions including depression, autism, cerebral palsy, multiple sclerosis, and stroke.1–3
A recent randomized trial1 demonstrated that hippotherapy was more effective than treadmill exercises in restoring balance and gait for patients who have suffered a cerebral vascular accident (CVA). Despite literature establishing the benefits of hippotherapy and increasing usage, very little has been reported on adverse events while engaging in hippotherapy. This case report describes a blinding and preventable ocular injury sustained by a post-stroke patient while participating in hippotherapy.
Case Description
A 66-year old female presented to a level I trauma center after falling from a horse while participating in a therapeutic horseback riding session. The patient had a history of brain cancer diagnosed six years prior treated with chemotherapy and radiation, a right-sided CVA two years prior, and seizures. Notably, she had left-sided motor weakness and slurred speech due to her prior CVA. In the three weeks prior to presentation, she began attending hippotherapy sessions with a trained therapist once a week. With each session, she wore a protective riding helmet without a face mask or grill.
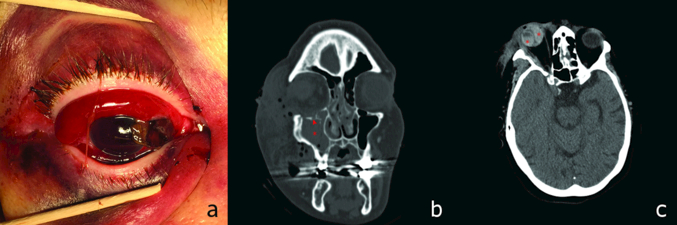
As the patient was being loaded onto the riding saddle for her third session, the horse moved and the patient fell, striking the right side of her face on a metal pole before landing on the ground. Upon presentation to the trauma center, she complained primarily of right knee pain but was also noted to have severe periorbital edema and ecchymosis of the right eye. On examination, visual acuity testing showed no light perception in the affected right eye and 20/30 in the left eye. Examination in the right eye was also remarkable for severely restricted extraocular movements, 360 degrees of subconjunctival hemorrhage, and hyphema obscuring the pupil (Figure 1a). Ocular examination of the left eye was unremarkable.
Figure 1: Intraoperative Examination and Head and Face CT.
a) Perioperatively, an 8-mm vertical full-thickness scleral laceration with uveal prolapse was observed in superonasal aspect of right eye. b) Face CT (coronal view) showed closed right zygomaticomaxillary complex fracture with 8-mm inferior displacement of the orbital floor (arrowhead) and minimal displacement of the lateral orbital wall. Complete opacification of the right maxillary sinus (*) but no herniation of the right inferior rectus muscle was demonstrated. c) Face CT (axial view) showed significant right orbital proptosis with asymmetric right global enlargement and extraconal hematoma. Biconvex internal hyperattenuation within the vitreous was noted (*), suggesting possible retinal detachment.
Head computerized tomography (CT) demonstrated no acute intracerebral injury. Face computerized tomography (CT) scan revealed a closed right zygomaticomaxillary complex fracture (Figure 1b-1c).
The patient was urgently taken to the operating room for exploration and surgical repair of her ruptured globe under general anesthesia (Figure 1a). Uveal tissue was reposited and excised as necessary, and the laceration was sutured. At the end of the case, the eye was noted to be watertight and without leak. The patient was started on moxifloxacin and prednisolone acetate drops postoperatively.
Postoperatively she had no light perception in the affected eye and subsequently underwent enucleation one month after the initial injury. One year post-operatively, the patient reports falling a few times since the surgery without significant injury. She has not ridden a horse since the injury.
Discussion
Equine-related trauma is common and well-documented in the healthy adult population,4 with most injuries caused by falls from horseback and resulting in contusions or abrasions. Although most of these injuries involve the head or craniofacial region and upper extremities, ocular trauma has also been reported. A retrospective review5 of maxillofacial injuries related to interactions with horses reported one globe injury out of 62 injuries reviewed. Open globe injury is of particular concern, as it is a sight-threatening complication of ocular trauma that results in profound vision loss in greater than 70% of patients.6 Enucleation is often performed after repair of an open globe injury due to pain or to reduce the risk of sympathetic ophthalmia.7
Post-stroke hippotherapy candidates may be more vulnerable to injury than the general population due to increased risk of fall. A prospective study8 conducted in 2014 found that 25% of post-stroke patients fell during the six months after discharge. The increased fall risk of post-stroke patients or other patients with gait instability may be explained by reduced reaction time, impaired stepping, and poor balance.9,10 In a retrospective analysis9 of patients over a three-year period, Inness et al. observed that 71% of post-stroke patients had impaired stepping reactions. As these impairments are well-recognized in patients partaking in hippotherapy, extensive precautions have been taken, and injuries related to hippotherapy have been reported as infrequently as one per 4,850 hours of therapy.11 Furthermore, previously reported injuries have been neither permanent nor disabling.11 To our knowledge, this is the first case report to describe ocular and orbital injury related to hippotherapy specifically.
Hippotherapy is often offered to particularly vulnerable patient populations, including those who have had strokes, spinal cord injury and traumatic brain injury. Practitioners should be aware of ocular and orbital injuries following hippotherapy that may result in permanent visual impairment, as illustrated by this case report. Fortunately, risk-benefit ratio of hippotherapy may be improved with safety measures such as protective headgear that includes a face mask or grill. Particularly in patients with unstable gait, practitioners should weigh the risks and benefits of hippotherapy. If these high risk patients do partake in hippotherapy, additional safety precautions should be taken to avoid injury.
Learning Points.
Hippotherapy is a horse-based rehabilitative therapy used to improve balance, coordination, and strength in patients with a wide range of medical conditions.
Ocular and orbital injuries are a potentially sight-threatening but preventable complications associated with the hippotherapy.
Practitioners should weigh the risks and benefits of hippotherapy for patients with unstable gait and recommend the use of a protective face mask or grill to reduce the risk of orbital injury.
Acknowledgements
The authors of this paper thank Dr. Uttam Bodanapally, M.D. for providing and selecting the representative CT images for this case report.
Financial Support:
Dr. Saeedi is funded by an NIH career Development Award (K23 EY025014).
Footnotes
Institutional Review Board Statement: IRB approval was not necessary for the research in question
Conflicts of Interest:
Mr. Chang reports no sources of financial support or relevant conflicts of interest for the present work.
Ms. Chang reports no sources of financial support or relevant conflicts of interest for the present work.
Dr. Andrews reports no sources of financial support or relevant conflicts of interest for the present work.
Dr. Saeedi reports no relevant conflicts of interest for the present work.
This case report has not previously been presented in any other scientific meeting or publication.
References
- 1).Lee CW, Kim SG, Yong MS. Effects of hippotherapy on recovery of gait and balance ability in patients with stroke. J Phys Ther Sci 2014;26:309–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Bronson C, Brewerton K, Ong J, Palanca C, Sullivan SJ. Does hippotherapy improve balance in persons with multiple sclerosis: a systematic review. Eur J Phys Rehabil Med 2010; 46: 347–353 [PubMed] [Google Scholar]
- 3).Sunwoo H, Chang WH, Kwon JY, Kim TW, Lee JY, Kim YH. Hippotherapy in adult patients with chronic brain disorders: a pilot study. Ann Rehabil Med 2012;36(6):756–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Loder RT. The demographics of equestrian-related injuries in the United States: injury patterns, orthopedic specific injuries, and avenues for injury prevention. J Trauma 2008;65(2):447–60. [DOI] [PubMed] [Google Scholar]
- 5).Ueeck BA, Dierks EJ, Homer LD, Potter B. Patterns of maxillofacial injuries related to interaction with horses. J Oral Maxillofac Surg 2004;62(6):693–6. [DOI] [PubMed] [Google Scholar]
- 6).Margo JA, Feldman S, Addis H, Bodanapally UK, Ellish N, Saeedi O. Open Globe Injuries Presenting With Normal or High Intraocular Pressure. Eye Contact Lens. 2016;42(4):256–261. [DOI] [PubMed] [Google Scholar]
- 7).Savar A, Andreoli MT, Kloek CE, Andreoli CM. Enucleation for open globe injury. Am J Ophthalmol 2009. April;147(4):595–600.e1. 10.1016/j.ajo.2008.10.017. Epub 2009 Feb 1. [DOI] [PubMed] [Google Scholar]
- 8).Jalayondeja C, Sullivan PE, Pichaiyongwongdee S. Six-month prospective study of fall risk factors identification in patients post-stroke. Geriatr Gerontol Int 2014;14: 778–785. 10.1111/ggi.12164 [DOI] [PubMed] [Google Scholar]
- 9).Inness EL, Mansfield A, Lakhani B, Bayley M, Mcilroy WE. Impaired reactive stepping among patients ready for discharge from inpatient stroke rehabilitation. Phys Ther 2014;94(12):1755–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Mansfield A, Inness EL, Komar J, et al. Training rapid stepping responses in an individual with stroke. Phys Ther 2011. ;91:958–969. [PMCID: PMC3107441] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Cook R Low injury rate in hippotherapy practice. Hippotherapy. 2013;Summer Issue:19–20 [Google Scholar]