Abstract
Objective
To examine whether psychosocial health mediates the association between food insecurity and grade point average (GPA) among college and university students.
Design
Data for the present study are from a longitudinal cohort study. Structural equation modelling (SEM) was used to test the proposed mediation hypothesis. Food insecurity was measured using the US Department of Agriculture’s Six-Item Short Form. Psychosocial health was operationalized as a latent factor with three indicators: depression, anxiety and hope. Validated scales were used to measure each indicator. GPA was self-reported.
Setting
Seven colleges and universities in Georgia, USA.
Participants
Students aged 18–25 years were recruited via email and surveyed every four months over a two-year period (analytic n 2377).
Results
Approximately 29 % of students were food insecure. In the final SEM, food insecurity was associated (standardized β, se) with poorer psychosocial health (0·22, 0·03, P<0·0001) and poorer psychosocial health was associated with a lower GPA (−0·21, 0·03, P<0·0001). The indirect effect of food security status on GPA, as mediated by psychosocial health, was significant (−0·05, 0·01, P<0·0001) and accounted for 73 % of the total effect. After accounting for psychosocial health, the direct effect of food security status on GPA was not significant (−0·02, 0·02, P=0·43).
Conclusions
Psychosocial health may be an important mechanism through which food insecurity affects academic performance among college and university students. Multicomponent interventions that address immediate food security needs as well as co-occurring mental health and academic concerns are needed to ensure student success.
Keywords: Food insecurity, College and university students, Psychosocial health, Academic performance
Education is a widely recognized social determinant of health, conferring multiple economic and psychosocial advantages across the life course( 1 – 4 ). In the USA, state and federal student aid programmes have significantly increased the accessibility of higher education over the past 50 years( 5 ). As a result, the demographic composition of US college and university student bodies has changed considerably, with more low-income, first-generation and racial/ethnic minority students enrolled than ever before( 5 ). Limited research has focused on the social and economic challenges these students face, and the impact these challenges might have on student health and well-being( 6 ). An increasing number of studies have documented a high prevalence of food insecurity, or a lack of ‘access, at all times, to enough food for an active, healthy life’( 7 ), on college and university campuses across the USA( 8 ). Associated with numerous poor health( 9 – 11 ) and academic outcomes( 12 – 14 ), food insecurity may hinder student achievement and undermine the potential for increased educational access to reduce health disparities.
A recent systematic review estimated that the average prevalence of food insecurity on US college and university campuses is 33 %( 8 ), nearly three times the national prevalence of 12·3 % in 2015( 7 ). Across studies, food insecurity was more common among students who were financially independent, caring for dependent children, younger and from racial/ethnic minority groups( 8 ). Although existing research is largely descriptive, a growing body of evidence suggests that food insecurity is associated with poorer health and academic outcomes among college and university students. Food-insecure students were more likely to report their health as fair or poor at universities in Oregon, USA( 15 ), Brisbane, Australia( 16 ), and Alberta, Canada( 17 ), and food insecurity was associated with higher odds of stress( 18 ) and depression( 18 , 19 ) among university freshman in Arizona, USA. Regarding academic performance, food insecurity was inversely associated with grade point average (GPA) among students attending a rural university in Oregon, USA( 15 ), two community colleges in Maryland, USA( 20 ), and four public universities in Illinois, USA( 21 ).
To date, no studies have examined the specific pathways through which food insecurity may affect academic performance among college and university students. Existing research on the relationship between food insecurity and academic achievement has primarily focused on early childhood( 22 ). Food insecurity has been prospectively associated with lower mental proficiency in toddlers( 23 ), as well as impaired reading and mathematical performance( 12 ) and inadequate standardized test scores( 24 ) among school-aged children. The psychological and emotional stress that often results from the experience of food insecurity is hypothesized to be a key mediator of this association( 12 , 14 , 22 , 25 , 26 ). Although few studies have explicitly tested this hypothesis, psychosocial factors have been found to mediate the association between food insecurity and various health outcomes including weight status( 27 ), sleep quality( 28 ) and child cognitive development( 23 ). The exploration of similar pathways among college and university students may help to elucidate the complex mechanisms that likely underlie early evidence for the association of food insecurity with poorer health and academic outcomes.
Using a longitudinal design, the present study leverages a life-course perspective on health( 29 – 31 ) and aims to fill an important gap in the literature regarding the associations between food insecurity and the risk of poor health and academic performance. Within a diverse group of college and university students in Georgia, USA, we aimed to: (i) assess the prevalence of food insecurity and identify sociodemographic characteristics associated with higher risk; (ii) assess the associations of food insecurity with indicators of psychosocial health including depression, anxiety and hope, and with GPA; and (iii) examine whether psychosocial health mediates the association between food insecurity and GPA. The present study is the first to examine the pathways through which food insecurity may impact academic performance among post-secondary students.
Methods
Study population and data collection
Data are from Project DECOY, a six-wave longitudinal cohort study examining tobacco use among college and university students in Georgia, USA. Study sampling, recruitment and retention procedures are described in detail elsewhere( 32 ). Briefly, eligible students (i.e. those between the ages of 18 and 25 years, enrolled as a student at least part-time and able to speak English) were sampled from seven Georgia colleges and universities. Three thousand students were randomly selected from each of three colleges/universities with student populations over 3000, and a census approach was used to recruit students from the remaining four colleges/universities with student populations less than 3000. A total of 15 607 students were contacted via email and recruited over a period of 48 h to 1 week, depending upon the college/university and the amount of time needed to reach the targeted recruitment goal at each institution. The total response rate within the recruitment time frame was 22·9 % (3574/15 607) and met sample size targets. One week after completion of the baseline survey, participants were asked via email to confirm their participation in the study, of whom 95·6 % (3418/3574) confirmed their participation and were enrolled in the study. The present study uses data from the baseline survey and Waves 2–4, which had retention rates of 86·9 % (n 2969), 83·9 % (n 2867) and 85·5 % (n 2922), respectively. For analyses, we retained participants who participated in all three waves (n 2645). An additional 268 participants (10·1 %) were excluded as they were missing data on covariates; missing data were not associated with the outcome. The final analytic sample size was 2377. Web-based surveys were used to collect data every four months between autumn 2014 and summer 2016. The baseline survey was administered in October/November 2014, and Waves 2–4 were administered in February/March 2015, June/July 2015 and October/November 2015, respectively. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Boards of Emory University, ICF Macro International, Albany State University, Berry College, University of North Georgia and Valdosta State University. Electronic informed consent was obtained from all subjects.
Exposure: food security status
We assessed food security status at Wave 3 using the US Department of Agriculture’s US Household Food Security Survey Module Six-Item Short Form( 33 ). The six survey items increase in severity, ranging from ‘The food I bought just didn’t last, and I didn’t have money to get more. Was that often, sometimes, or never true for you in the last 12 months?’ to ‘In the last 12 months were you ever hungry, but didn’t eat because there wasn’t enough money for food?’ Following US Department of Agriculture coding guidelines, participants who responded affirmatively to two or more questions were classified as food insecure; all others were classified as food secure. When tested against the US Department of Agriculture’s full eighteen-item scale, the six-item scale correctly classified 97·7 % of households( 34 ).
Mediator: psychosocial health
Our hypothesized mediator, psychosocial health, was operationalized as a latent factor with three indicators: depression, anxiety and hope. For the structural equation modelling (SEM), each indicator was coded such that a higher score indicates poorer psychosocial health.
Depression. Depression was measured at Wave 4 using the nine-item Patient Depression Questionnaire (PHQ-9)( 35 ). The PHQ-9 is a measure of depression severity, which asks participants how often, in the previous two weeks, they have experienced nine symptoms of depression. Example symptoms include ‘little interest or pleasure in doing things’, ‘trouble falling or staying asleep, or sleeping too much’ and ‘feeling bad about yourself or that you are a failure or have let yourself or your family down’. Answer choices and scores include: ‘not at all’=0, ‘several days’=1, ‘more than half the days’=3 and ‘nearly every day’=3. Scores for each of the nine items are then summed to create a continuous variable ranging from 0 to 27. Cronbach’s α in the analytic sample was 0·90.
Anxiety. Anxiety was measured at Wave 4 using the eighteen-item Anxiety Sensitivity Index – 3 (ASI-3)( 36 ). The ASI-3 measures anxiety sensitivity, or a fear of arousal-related sensations. Participants are asked to indicate the extent to which they agree with eighteen statements including ‘When my chest feels tight, I get scared that I won’t be able to breathe properly’, ‘It scares me when I blush in front of people’ and ‘When I have trouble thinking clearly, I worry that there is something wrong with me’. Answer choices and scores include: ‘very little’=0, ‘little’=1, ‘some’=2, ‘much’=3 and ‘very much’=4. If participants have not had a particular experience, they are asked to answer based on how they anticipate feeling if they were to have such an experience. Index items are summed to create a continuous variable ranging from 0 to 72. Cronbach’s α in the analytic sample was 0·93.
Hope. Hope was measured at Wave 3 using the six-item Adult State Hope Scale( 37 ). The scale measures participant hope, or belief in their capacity to take action towards reaching their goals and belief in their capacity to generate routes to reach those goals. Participates indicate the degree to which, at present, each item is true or false. Example items include ‘At the present time, I am energetically pursuing my goals’, ‘There are lots of ways around any problem that I am facing right now’ and ‘I can think of many ways to reach my current goals’. Answer choices and scores include: ‘definitely false’=1, ‘mostly false’=2, ‘somewhat false’=3, ‘slightly false’=4, ‘slightly true’=5, ‘somewhat true’=6, ‘mostly true’=7 or ‘definitely true’=8. Scale items are summed to create a continuous variable ranging from 6 to 48. Cronbach’s α in the analytic sample was 0·91. (Note that, in order to minimize respondent burden, not all measures could be included at all waves. However, test–retest reliability exceeds 0·73 over 8- to 10-week periods among college students( 38 – 41 ).)
Outcome: grade point average
At Wave 4, participants self-reported their GPA in response to the question ‘Which of the below is the closest reflection of your GPA?’ There were six possible responses: ‘4·0 or mostly As’; ‘3·5 or half As and half Bs’; ‘3·0 or mostly Bs’; ‘2·5 or half Bs and half Cs’; ‘2·0 or mostly Cs’; and ‘less than 2·0 or less than a C average’. GPA was treated as a continuous variable in all analyses.
Control variables: sociodemographic and socio-economic characteristics
Self-reported sociodemographic and socio-economic characteristics used as covariates in analyses include: gender (male; female); age (continuous); race/ethnicity (Black; White; Asian; Hispanic; other); type of college/university attended (technical college; public university; private college/university; Historically Black Colleges and Universities (HBCU)); parent’s educational attainment (high-school diploma or less; some college or associate’s degree; bachelor’s degree or higher); living situation (college/university housing; living at home with parents; living off-campus, but not with parents); employment status (not employed; employed part-time; employed full-time); receiving Supplemental Nutrition Assistance Program (SNAP) benefits (yes; no); monthly discretionary budget (≤$US 200; $US 201–400; $US 401–600; ≥$US 601); and parental status (yes; no).
Adverse childhood experiences (ACE; 0; 1; 2; 3; ≥4)( 42 ) was also included as a covariate in all analyses. Defined as abuse, neglect or household dysfunction occurring in the first 18 years of life( 43 ), ACE are a well-established predictor of food insecurity( 44 ), psychosocial health( 45 ) and academic performance( 46 ). Accordingly, we controlled for ACE in all analyses to reduce any bias in our estimated direct and indirect effects introduced by exposure–outcome, mediator–outcome or exposure–mediator confounding( 47 ).
Analysis
Descriptive statistics were calculated for each variable to check for outliers and assess the normality of distributions for continuous variables. Chi-square test statistics were calculated to assess differences in sociodemographic characteristics by food security status. Prior to specifying the structural equation model (SEM), bivariate analyses and linear regression models were run between the exogenous variable, food security status, and each endogenous variable (i.e. depression, anxiety, hope and GPA) to confirm the presence of significant associations warranting further investigation in an SEM framework. In addition, a logistic regression model, with food security status as the outcome, was estimated to identify sociodemographic characteristics associated with food security status. Regression models were adjusted for all sociodemographic characteristics detailed above. Descriptive statistics and adjusted regression models were calculated in the statistical software package SAS version 9.4 and SEM was performed using MPlus 8 (Muthén & Muthén: Los Angeles, CA, USA).
For the SEM analysis, we used a two-step modelling approach(48). Before specifying the structural regression model, we used confirmatory factor analysis to estimate the measurement portion of the model. Each indicator variable of the latent psychosocial health factor (i.e. depression, anxiety and hope) had an adequate standardized factor loading (i.e. >0·30). Because this was a saturated measurement model, no model fit indices could be obtained. We then estimated the structural regression model to test the hypothesized direct and indirect effects. All models were estimated using maximum likelihood estimation. Model fit was assessed using the following indices: standardized root-mean-square residual (a value below 0·08 indicates good model fit); root-mean-square error of approximation (a value below 0·05 indicates good model fit); comparative fit index (a value greater than or equal to 0·95 indicates good model fit); and χ2 test (although P<0·05 is considered to indicate good model fit, the test is sensitive to sample size and was expected to be significant). Modification indices were examined, and model re-specifications considered on theoretical grounds. We report standardized parameter estimates and corresponding P values (significance assessed at P<0·05).
Results
Student sociodemographic and socio-economic characteristics
The majority of students were women (64 %) and the average age was 21 years old (Table 1). Approximately 62 % of students self-identified as White, 20 % as Black, 8 % as Hispanic, 7 % as Asian and 3 % as another race/ethnicity. Over half of students had parents who had received a bachelor’s degree or higher, while 29 % had parents who had completed some college, and 16 % had parents who had obtained a high-school diploma or less. Slightly over a quarter of students were not employed, while approximately half were working part-time and the remaining quarter were working full-time. Students lived in a variety of residence types, with 38 % living in university housing, 23 % living in their parent’s home and 39 % living in another type of off-campus housing. Overall, 29 % of students were food insecure. Prevalence of low and very low food insecurity varied by college/university type: 23 % of private college/university students, 33 % of HBCU students, 34 % of public university students and 37 % of technical college students.
Table 1.
Sociodemographic characteristics of college and university students (n 2377) from seven institutions in Georgia, USA, autumn 2014–autumn 2015
| n or Mean | % or sd | ||
|---|---|---|---|
| Type of college/university | |||
| Public | 674 | 28·36 | |
| Private | 1067 | 44·89 | |
| HBCU | 251 | 10·56 | |
| Technical | 385 | 16·2 | |
| Gender | |||
| Female | 1527 | 64·24 | |
| Male | 850 | 35·76 | |
| Age (years), mean and sd | 21·01 | 1·93 | |
| Race/ethnicity | |||
| Black/African American | 484 | 20·36 | |
| White | 1471 | 61·88 | |
| Asian | 159 | 6·69 | |
| Hispanic | 184 | 7·74 | |
| Other | 79 | 3·32 | |
| Parent’s education level | |||
| High school or less | 383 | 16·11 | |
| Some college or associate’s degree | 682 | 28·69 | |
| Bachelor’s degree or higher | 1312 | 55·19 | |
| Employment status | |||
| Not employed | 600 | 25·24 | |
| Employed part-time | 1214 | 51·07 | |
| Employed full-time | 563 | 23·69 | |
| Residence type | |||
| University housing | 908 | 38·19 | |
| Parent’s home | 546 | 22·97 | |
| Other off-campus housing | 923 | 38·83 | |
| Children | |||
| ≥1 | 100 | 4·21 | |
| 0 | 2277 | 95·79 | |
| Receiving SNAP benefits | |||
| Yes | 249 | 10·48 | |
| No | 2128 | 89·52 | |
| Discretionary budget (per month) | |||
| ≤$US 200 | 1307 | 54·99 | |
| $US 201–400 | 660 | 27·77 | |
| $US 401–600 | 214 | 9·00 | |
| ≥$US 601 | 196 | 8·25 | |
| Adverse childhood experiences | |||
| 0 | 1158 | 48·70 | |
| 1 | 502 | 21·12 | |
| 2 | 285 | 11·99 | |
| 3 | 166 | 6·98 | |
| ≥4 | 266 | 11·19 | |
HBCU, Historically Black Colleges and Universities; SNAP, Supplemental Nutrition Assistance Program.
Data presented are n and % unless indicated otherwise.
Sociodemographic and socio-economic characteristics associated with food security status
In adjusted logistic regression models, numerous student sociodemographic and socio-economic characteristics were associated with food security status (Table 2). Compared with students working full-time, students who were not employed had lower odds of food insecurity (OR=0·73; 95 % CI 0·55, 0·96, P=0·02), and students who were living off-campus had higher odds of food insecurity than those who were living in university housing (OR=1·42; 95 % CI 1·08, 1·87, P=0·01). In addition, students receiving SNAP benefits (OR=2·36; 95 % CI 1·72, 3·23, P<0·0001) and students with lower monthly discretionary budgets had higher odds of food insecurity (≤$US 200 v. ≥$US 601: OR=1·89; 95 % CI 1·28, 2·80, P=0·001; $US 201–400 v. ≥$US 601: OR=1·50; 95 % CI 1·00, 2·26, P=0·05). Students whose parents had obtained a high-school diploma or less, or whose parents had completed some college or an associate’s degree, had higher odds of food insecurity than students whose parents had a bachelor’s degree or higher (OR=1·64; 95 % CI 1·24, 2·16, P=0·001; OR=1·45; 95 % CI 1·16, 1·83, P=0·001, respectively). Finally, compared with students who did not report any adverse childhood experiences, students who reported at least one ACE had increasingly higher odds of food insecurity with each additional ACE experienced (1 v. 0 ACE: OR=1·50; 95 % CI 1·17, 1·92, P=0·001; 2 v. 0 ACE: OR=1·73; 95 % CI 1·29, 2·33, P=0·0003; 3 v. 0 ACE: OR=2·10; 95 % CI 1·47, 3·00, P<0·0001; ≥4 v. 0 ACE: OR=3·12; 95 % CI 2·32, 4·20, P<0·0001). College/university type was not associated with food security status after adjusting for other covariates.
Table 2.
Sociodemographic characteristics associated with food security status among college and university students (n 2377) from seven institutions in Georgia, USA, autumn 2014–autumn 2015
| OR | 95 % CI | P value | |
|---|---|---|---|
| Type of college/university (ref.=private) | |||
| Public | 1·28 | 0·99, 1·66 | 0·06 |
| HBCU | 0·82 | 0·54, 1·25 | 0·35 |
| Technical | 1·37 | 0·98, 1·91 | 0·07 |
| Gender (ref.=male) | |||
| Female | 1·06 | 0·86, 1·30 | 0·61 |
| Age | 0·98 | 0·93, 1·04 | 0·56 |
| Race/ethnicity (ref.=White) | |||
| Black/African American | 1·20 | 0·89, 1·63 | 0·23 |
| Asian | 1·21 | 0·79, 1·84 | 0·38 |
| Hispanic | 1·30 | 0·92, 1·85 | 0·14 |
| Other | 1·45 | 0·88, 2·39 | 0·15 |
| Parent’s education level (ref.=bachelor’s degree or higher) | |||
| High school or less | 1·64 | 1·24, 2·16 | 0·001 |
| Some college or associate’s degree | 1·45 | 1·16, 1·83 | 0·001 |
| Employment status (ref.=employed full-time) | |||
| Not employed | 0·73 | 0·55, 0·96 | 0·02 |
| Employed part-time | 0·82 | 0·65, 1·04 | 0·11 |
| Residence type (ref.=university housing) | |||
| Parent’s home | 0·91 | 0·67, 1·23 | 0·54 |
| Other off-campus housing | 1·42 | 1·08, 1·87 | 0·01 |
| Children (ref. 0) | |||
| ≥1 | 0·73 | 0·45, 1·18 | 0·19 |
| Receiving SNAP benefits (ref.=no) | |||
| Yes | 2·36 | 1·72, 3·23 | <0·0001 |
| Discretionary budget (per month) (ref.=≥$US 601) | |||
| ≤$US 200 | 1·89 | 1·28, 2·80 | 0·001 |
| $US 201–400 | 1·50 | 1·00, 2·26 | 0·05 |
| $US 401–600 | 1·05 | 0·64, 1·73 | 0·84 |
| Adverse childhood experiences (ref.=0) | |||
| 1 | 1·50 | 1·17, 1·92 | 0·001 |
| 2 | 1·73 | 1·29, 2·33 | 0·0003 |
| 3 | 2·10 | 1·47, 3·00 | <0·0001 |
| ≥4 | 3·12 | 2·32, 4·20 | <0·0001 |
Ref., reference category; HBCU, Historically Black Colleges and Universities; SNAP, Supplemental Nutrition Assistance Program.
P<0·05 indicates statistical significance.
Adjusted associations between food insecurity, psychosocial health and grade point average
In adjusted linear regression models, food insecurity was associated with each indicator of psychosocial health as well as with GPA (Table 3). Food insecurity was associated with a 1·83-point increase in depression score (se=0·25, P<0·0001), a 3·68-point increase in anxiety score (se=0·69, P<0·0001) and a 2·16-point decrease in hope score (se=0·36, P<0·0001). Food insecurity was associated with a 0·14-point decrease in GPA (se=0·04, P=0·002).
Table 3.
Adjusted linear regression models of the associations between food insecurity, psychosocial health and grade point average (GPA) in college and university students (n 2377) from seven institutions in Georgia, USA, autumn 2014–autumn 2015
| β | se | P value | |
|---|---|---|---|
| Depression (score range: 0–27) | 1·83 | 0·25 | <0·0001 |
| Anxiety (score range: 0–72) | 3·68 | 0·69 | <0·0001 |
| Hope (score range: 6–48) | −2·16 | 0·36 | <0·0001 |
| GPA (range<2·0–4·0) | −0·14 | 0·04 | 0·002 |
P<0·05 indicates statistical significance.
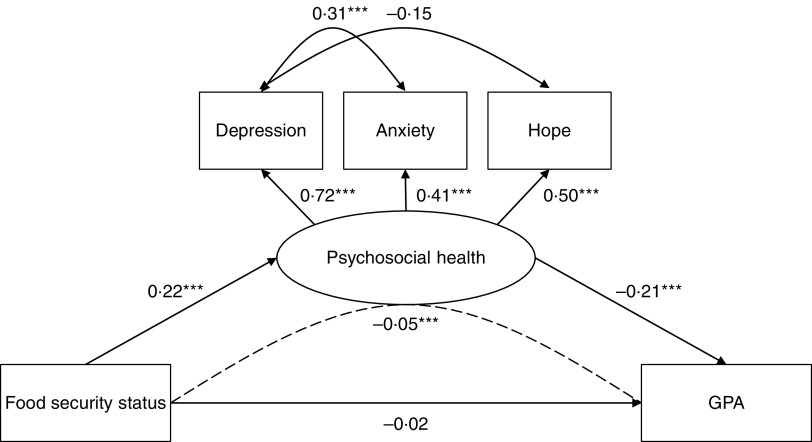
Structural equation model
Our final SEM achieved good model fit (Fig. 1). Empirically derived modification indices suggested the addition of covariance between depression and anxiety, as well as between depression and hope, to improve model fit. We included these changes as they were theoretically sound and did not affect our a priori hypothesis. Except for the χ 2 test, all fit indices met standard thresholds for good model fit.
Fig. 1.
Final structural equation model testing whether psychosocial health mediates the association between food security status and grade point average (GPA) among college and university students (n 2377) from seven institutions in Georgia, USA, autumn 2014–autumn 2015: ———, direct effects; – – – – –, indirect effects; path coefficients are standardized; ***P<0·0001 (model fit: χ 2=131·92 (df=50), P<0·0001; standardized root-mean-square residual=0·01; root-mean-square error of approximation=0·03 (90 % CI 0·02, 0·03); comparative fit index=0·95; R 2 (GPA)=0·17)
The final SEM supported our hypothesis that psychosocial health fully mediates the association between food security status and GPA. Food insecurity was associated with poorer psychosocial health (standardized β=0·22, se=0·03, P<0·0001) and poorer psychosocial health was associated with a lower GPA (standardized β=−0·21, se=0·03, P<0·0001). The total effect of food security status on GPA was significant (standardized β=−0·06, se=0·02, P=0·002). When decomposed into indirect and direct effects, the indirect effect of food security status on GPA, as mediated by psychosocial health, was significant (standardized β=−0·05, se=0·01, P<0·0001) and accounted for 73 % of the total effect. After accounting for psychosocial health, the direct effect of food security status on GPA was not significant (standardized β=−0·02, se=0·02, P=0·43). The full SEM, including covariates, accounted for approximately 17 % of the variance in GPA (R 2=0·17).
Discussion
The present study examined associations among food insecurity, psychosocial health and academic performance among college and university students in Georgia, USA. Approximately 29 % of students experienced food insecurity during the previous 12 months, and food insecurity was associated with poorer psychosocial health and academic performance. Notably, we found that psychosocial health fully mediated the association between food insecurity and academic performance. Our findings support and extend growing evidence for the high prevalence of food insecurity on college and university campuses and its deleterious effects on student health and success( 6 , 8 ). As the first study to use a longitudinal design to identify a potential mechanism through which food insecurity affects academic performance, our study offers useful insights for the development, targeting and implementation of programmatic and policy interventions that seek to reduce food insecurity and its consequences.
The prevalence of food insecurity in our sample was comparable to the recently estimated US college and university prevalence of 33 %( 8 ). Although the proportion of students in our sample experiencing food insecurity was highest among those attending technical college (37 %), it was still nearly one-quarter among private college/university students. Across college/university types, the rising cost of college attendance has outpaced spending on financial aid( 49 ); coupled with the shifting demographics of college enrolment, these financial constraints have created more economically vulnerable student bodies and are key factors underlying substantial socio-economic disparities in degree completion( 50 ). In a nationally representative survey of young adults who had completed some higher education, the inability to afford tuition and fees, and the need to work in order to make money were the top reasons reported for leaving prior to obtaining a degree( 51 ). Broton and Goldrick-Rab( 49 ) invoke Maslow’s( 52 ) hierarchy of needs in their discussion of food and housing insecurity among college and university students: if students’ basic needs are not met, they will be unable to engage in the higher-level learning required of them in college.
Similar to previous studies, we found that students who were employed, living off-campus without parents and receiving SNAP benefits experienced higher odds of food insecurity( 15 ). Representing various dimensions of socio-economic status, these factors illustrate the difficulties that students of lower socio-economic status face in fulfilling their basic material needs, despite working, budgeting and taking advantage of available benefits( 49 ). From a life-course perspective( 29 – 31 ), lower parental educational attainment and ACE may confer additional vulnerability to food insecurity. ACE have been associated with a higher likelihood of experiencing food insecurity among adult women and are hypothesized to negatively affect the formation of stable social relationships, educational attainment and the ability to maintain employment – factors that may buffer against food insecurity( 44 ). Given the well-documented and far-reaching negative effects of ACE on adult health and well-being( 42 ), this association may warrant further investigation in college populations. Screening students for ACE, if done using trauma-informed and non-stigmatizing approaches( 53 ), may help identify students at higher risk for food insecurity and other adverse health behaviours and outcomes.
Food insecurity was associated with all three indicators of psychosocial health: depression, anxiety and hope. Our findings are consistent with the limited literature on food insecurity and psychosocial health among college and university students( 18 , 19 ), as well as broader literature on the associations between food insecurity and mental health. Food insecurity has been repeatedly associated with higher levels of depression, anxiety and stress in developed( 11 ) and developing country settings( 54 ), and is hypothesized to contribute to poor mental health by acting as a ‘toxic’ stressor( 26 ) that disrupts physiological functioning and impairs mental health( 55 ). Other stressors experienced during college, when students are establishing independence from their families and learning to balance multiple responsibilities such as school, work and personal relationships( 56 ), may compound food insecurity-related stress. Additional research is needed to understand the temporal relationships between food insecurity and psychosocial health among college and university students. Only one other study has examined the longitudinal effects of food insecurity in this population( 18 ). While the authors did not find evidence that food insecurity was prospectively associated with psychosocial health, they did find that food insecurity was concurrently associated with stress and depression. Understanding the temporal features of student food insecurity (e.g. frequency, seasonality, duration), and the time frames within which health effects occur, can help guide the development and targeting of mental health promotion and treatment efforts to high-risk students.
Importantly, we found that psychosocial health fully mediated the association between food insecurity and GPA. While our study is the first to identify a mechanism through which food insecurity affects academic performance, the individual pathways identified are supported by existing literature. In addition to previously identified negative associations between food insecurity and GPA( 15 , 20 , 21 ), depression( 57 , 58 ), anxiety( 57 ) and low hope( 59 ) have been associated with poorer academic performance, including GPA and degree completion, among college students. Poor mental health, particularly anxiety and depression, is hypothesized to hinder academic performance through various factors, such as reduced energy, difficulty making decisions, difficulty concentrating and decreased interest in the future( 57 ). While addressing the underlying socio-economic conditions and life-course exposures that give rise to food insecurity among college students is imperative, it must be accompanied by efforts to alleviate existing food insecurity and intervene on the psychosocial mechanisms through which it affects academic performance.
With the increased attention that campus food insecurity has received in the academic literature( 8 ) as well as the popular press( 60 , 61 ), a number of colleges and universities have begun to acknowledge and address student food insecurity. Campus-based food pantries, which procure, store and distribute free food directly to students in need, and student financial literacy programmes have been the most common responses to student food insecurity( 8 ). The College and University Food Bank Alliance was started in 2012 to support colleges/universities in developing and sustaining student food pantries, and currently has over 600 members( 62 ). The majority of college students are ineligible for SNAP, the primary tool for preventing and alleviating food insecurity in the USA. * As a result, several campuses and organizations have advocated for expanding SNAP eligibility and ensuring that campus food vendors are enrolled in the electronic benefits transfer system and able to accept SNAP benefits( 8 ). For food-insecure students, these critical solutions can provide the immediate support needed to meet basic food needs. However, multicomponent interventions that also address co-occurring mental health and academic concerns will likely be required to comprehensively address the needs of food-insecure students.
Strengths and limitations
The present study has several notable strengths. Most importantly, it was the first to use a longitudinal design to assess the association between food insecurity and academic performance, and identify the potential mediating role of psychosocial health, among college/university students. While existing research has largely examined bivariate associations using cross-sectional data, we used SEM with indicators measured at two time points to test our mediation hypothesis. Our study was further strengthened by a large sample size and the ability to compare across multiple types of colleges and universities. The majority of existing research is based on smaller samples collected from individual institutions. In addition, we used well-established indicators of psychosocial health, which demonstrated excellent reliability in our sample.
Despite these strengths, our study was subject to several important limitations. While we used existing literature to support our conceptualization of food insecurity as a predictor of psychosocial health, the causal relationship is likely bidirectional( 11 ). Future research should employ more advanced longitudinal study designs and analytical techniques to further understand the dynamic relationship between food insecurity and psychosocial health. Additionally, our data set required the use of mediator and outcome variables measured at the same time point, as well as one indicator of psychosocial health measured concurrently with food insecurity. Ideally, we would have measured hope at Wave 4 with the other psychosocial health indicators, but the importance of minimizing participant burden precluded us from doing so. However, as discussed, the Hope Scale has demonstrated high test–retest reliability over 8- to 10-week periods in college populations( 38 – 41 ). While our study advances existing literature by measuring food insecurity prior to health and academic outcomes, future studies should include additional waves of data to more definitively support the temporal relationships between the exposure, mediator and outcome. Another limitation is that GPA was self-reported. Objectively measured GPA, as well as additional indicators of academic performance, can advance our understanding of how food insecurity affects academic performance among college and university students. In addition, although the sample was comprised of diverse young adults in terms of race, ethnicity and socio-economic backgrounds; diverse college types (e.g. private, public, technical, HBCU); and students in rural and urban settings, the sample was comprised of college students from Georgia, limiting the generalizability of our results to the broader young adult population. Finally, despite the sample characteristics being representative of age and racial/ethnic characteristics of the student populations, the sample was comprised of a slightly higher proportion of women than is representative of the student population.
Conclusions
Food insecurity is a significant problem on college and university campuses, and has important implications for psychosocial health and academic performance. Our study provides initial evidence that the experience of food insecurity hinders academic performance through its harmful effects on psychosocial health. For higher education to fulfil its potential as an engine of social mobility, immediate efforts to address student food insecurity are needed to ensure that all students have the resources they need to succeed. Programmes and policies should prioritize students at greatest risk for food insecurity, including those who have experienced life-course and current socio-economic disadvantage. The development and evaluation of multicomponent interventions, which jointly address food insecurity and its consequences, will be an important next step in understanding and addressing food insecurity among college and university students.
Acknowledgements
Acknowledgements: The authors would like to thank their Campus Advisory Board members across the state of Georgia in developing and assisting in administering this survey. They also would like to thank ICF International for their scientific input and technical support in conducting this research. Financial support: This research was supported by the National Cancer Institute (Principal Investigator: C.J.B., grant number 1R01CA179422-01). I.G.R. was supported by the National Heart, Lung, and Blood Institute (NHLBI) Predoctoral T32 Multidisciplinary Research Training to Reduce Inequities in Cardiovascular Health (grant number 5T32HL130025). The funders had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: I.G.R. formulated the research question, conducted the analyses and drafted the manuscript. R.H. provided oversight and support for all statistical analyses and aided in the interpretation of results. C.J.B. designed and implemented the study. All authors provided feedback on multiple drafts of the manuscript and approved the version submitted for publication. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Boards of Emory University, ICF Macro International, Albany State University, Berry College, University of North Georgia and Valdosta State University. Electronic informed consent was obtained from all subjects.
Footnotes
Students may be eligible for SNAP if they work at least 20 h/week, participate in a state- or federally-financed work study programme, receive public assistance benefits under a Title IV-A programme, care for a dependent household member under the age of 6 years, or care for a dependent household member between the ages of 6 and 12 years, and do not have adequate child care( 63 ).
References
- 1. Cohen AK & Syme SL (2013) Education: a missed opportunity for public health intervention. Am J Public Health 103, 997–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Oreopoulos P & Petronijevic U (2013) Making college worth it: a review of the returns to higher education. Future Child 23, 41–65. [DOI] [PubMed] [Google Scholar]
- 3. Mirowsky J & Ross CE (2003) Education, Social Status, and Health. New York: Taylor & Francis. [Google Scholar]
- 4. Hayward MD, Hummer RA & Sasson I (2015) Trends and group differences in the association between educational attainment and US adult mortality: implications for understanding education’s causal influence. Soc Sci Med 127, 8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baum S, Kurose C & McPherson M (2013) An overview of American higher education. Future Child 23, 17–39. [DOI] [PubMed] [Google Scholar]
- 6. Broton K & Goldrick-Rab S (2016) The dark side of college (un)affordability: food and housing insecurity in higher education. Change 48, 16–25. [Google Scholar]
- 7. Coleman-Jensen A, Rabbitt M, Gregory C et al. (2016) Household Food Security in the United States in 2015. Economic Research Report no. ERR-237. Washington, DC: US Department of Agriculture, Economic Research Service. [Google Scholar]
- 8. Bruening M, Argo K, Payne-Sturges D et al. (2017) The struggle is real: a systematic review of food insecurity on postsecondary education campuses. J Acad Nutr Diet 117, 1767–1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gundersen C & Ziliak JP (2015) Food insecurity and health outcomes. Health Aff (Millwood) 34, 1830–1839. [DOI] [PubMed] [Google Scholar]
- 10. Laraia BA (2013) Food insecurity and chronic disease. Adv Nutr 4, 203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bruening M, Dinour LM & Chavez JBR (2017) Food insecurity and emotional health in the USA: a systematic narrative review of longitudinal research. Public Health Nutr 20, 3200–3208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jyoti DF, Frongillo EA & Jones SJ (2005) Food insecurity affects school children’s academic performance, weight gain, and social skills. J Nutr 135, 2831–2839. [DOI] [PubMed] [Google Scholar]
- 13. Belsky DW, Moffitt TE, Arseneault L et al. (2010) Context and sequelae of food insecurity in children’s development. Am J Epidemiol 172, 809–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alaimo K, Olson CM & Frongillo EA Jr (2001) Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics 108, 44–53. [PubMed] [Google Scholar]
- 15. Patton-Lopez MM, Lopez-Cevallos DF, Cancel-Tirado DI et al. (2014) Prevalence and correlates of food insecurity among students attending a midsize rural university in Oregon. J Nutr Educ Behav 46, 209–214. [DOI] [PubMed] [Google Scholar]
- 16. Gallegos D, Ramsey R & Ong KW (2013) Food insecurity: is it an issue among tertiary students? Higher Educ 67, 497–510. [Google Scholar]
- 17. Farahbakhsh J, Hanbazaza M, Ball GDC et al. (2017) Food insecure student clients of a university-based food bank have compromised health, dietary intake and academic quality. Nutr Diet 74, 67–73. [DOI] [PubMed] [Google Scholar]
- 18. Bruening M, van Woerden I, Todd M et al. (2018) Hungry to learn: the prevalence and effects of food insecurity on health behaviors and outcomes over time among a diverse sample of university freshmen. Int J Behav Nutr Phys Act 15, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bruening M, Brennhofer S, van Woerden I et al. (2016) Factors related to the high rates of food insecurity among diverse, urban college freshmen. J Acad Nutr Diet 116, 1450–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Maroto ME, Snelling A & Linck H (2015) Food insecurity among community college students: prevalence and association with grade point average. Community Coll J Res Pract 39, 515–526. [Google Scholar]
- 21. Morris LM, Smith S, Davis J et al. (2016) The prevalence of food security and insecurity among Illinois university students. J Nutr Educ Behav 48, 376–382 e371. [DOI] [PubMed] [Google Scholar]
- 22. Perez-Escamilla R & Pinheiro de Toledo Vianna R (2012) Food insecurity and the behavioral and intellectual development of children: a review of the evidence. J Appl Res Child 3, 9. [Google Scholar]
- 23. Zaslow M, Bronte-Tinkew J, Capps R et al. (2009) Food security during infancy: implications for attachment and mental proficiency in toddlerhood. Matern Child Health J 13, 66–80. [DOI] [PubMed] [Google Scholar]
- 24. Faught EL, Williams PL, Willows ND et al. (2017) The association between food insecurity and academic achievement in Canadian school-aged children. Public Health Nutr 20, 2778–2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Whitaker RC, Phillips SM & Orzol SM (2006) Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 118, e859–e868. [DOI] [PubMed] [Google Scholar]
- 26. Knowles M, Rabinowich J, Ettinger de Cuba S et al. (2016) ‘Do you wanna breathe or eat?’: parent perspectives on child health consequences of food insecurity, trade-offs, and toxic stress. Matern Child Health J 20, 25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Willis DE & Fitzpatrick KM (2016) Psychosocial factors as mediators of food insecurity and weight status among middle school students. Appetite 103, 236–243. [DOI] [PubMed] [Google Scholar]
- 28. Bermudez-Millan A, Perez-Escamilla R, Segura-Perez S et al. (2016) Psychological distress mediates the association between food insecurity and suboptimal sleep quality in Latinos with type 2 diabetes mellitus. J Nutr 146, 2051–2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Halfon N & Hochstein M (2002) Life course health development: an integrated framework for developing health, policy, and research. Milbank Q 80, 433–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ben-Shlomo Y & Kuh D (2002) A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol 31, 285–293. [PubMed] [Google Scholar]
- 31. Lynch J & Smith GD (2005) A life course approach to chronic disease epidemiology. Annu Rev Public Health 26, 1–35. [DOI] [PubMed] [Google Scholar]
- 32. Berg CJ, Haardorfer R, Lewis M et al. (2016) DECOY: Documenting Experiences with Cigarettes and Other Tobacco in Young Adults. Am J Health Behav 40, 310–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. US Department of Agriculture (2012) US Household Food Security Survey Module: Six-item Short Form. Washington, DC: US Department of Agriculture, Economic Research Service. [Google Scholar]
- 34. Blumberg SJ, Bialostosky K, Hamilton WL et al. (1999) The effectiveness of a short form of the household food security scale. Am J Public Health 89, 1231–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kroenke K, Spitzer RL & Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Taylor S, Zvolensky MJ, Cox BJ et al. (2007) Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess 19, 176–188. [DOI] [PubMed] [Google Scholar]
- 37. Snyder CR, Sympson SC, Ybasco FC et al. (1996) Development and validation of the State Hope Scale. J Pers Soc Psychol 70, 321–335. [DOI] [PubMed] [Google Scholar]
- 38. Edwards LM, Rand KL, Lopez SJ et al. (2007) Understanding hope: a review of measurement and construct validity research. In Oxford Handbook of Methods in Positive Psychology, pp. 83–95. New York: Oxford University Press. [Google Scholar]
- 39. Harney P (1989) The Hope Scale: exploration of construct validity and its influence on health. Master’s Thesis, University of Kansas at Lawrence.
- 40. Gibb J (1990) The Hope Scale revisited: further validation of a measure of individual differences in the hope motive. Master’s Thesis, University of Illinois at Urbana-Champaign.
- 41. Yoshinobu L (1989) Construct validation of the Hope Scale: agency and pathways components. Master’s Thesis, University of Kansas at Lawrence.
- 42. Felitti VJ, Anda RF, Nordenberg D et al. (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. Am J Prev Med 14, 245–258. [DOI] [PubMed] [Google Scholar]
- 43. Centers for Disease Control and Prevention (2016) About the CDC–Kaiser ACE study. https://www.cdc.gov/violenceprevention/acestudy/index.html (accessed October 2018).
- 44. Sun J, Knowles M, Patel F et al. (2016) Childhood adversity and adult reports of food insecurity among households with children. Am J Prev Med 50, 561–572. [DOI] [PubMed] [Google Scholar]
- 45. Edwards VJ, Holden GW, Felitti VJ et al. (2003) Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry 160, 1453–1460. [DOI] [PubMed] [Google Scholar]
- 46. Romano E, Babchishin L, Marquis R et al. (2015) Childhood maltreatment and educational outcomes. Trauma Violence Abuse 16, 418–437. [DOI] [PubMed] [Google Scholar]
- 47. VanderWeele TJ (2016) Mediation analysis: a practitioner’s guide. Annu Rev Public Health 37, 17–32. [DOI] [PubMed] [Google Scholar]
- 48. Kline R (2011) Principles and Practices of Structural Equation Modeling, 3rd ed. New York: The Guilford Press. [Google Scholar]
- 49. Broton KM & Goldrick-Rab S (2018) Going without: an exploration of food and housing insecurity among undergraduates. Educ Res 47, 121–133. [Google Scholar]
- 50. Kena G, Musu-Gillette L, Robinson J et al. (2015) The Condition of Education 2015 (NCES 2015–144) . Washington, DC: US Department of Education, National Center for Education Statistics. [Google Scholar]
- 51. Johnson J & Rochkind J (2009) With their whole lives ahead of them: myths and realities about why so many students fail to finish college. https://www.publicagenda.org/files/theirwholelivesaheadofthem.pdf (accessed November 2018).
- 52. Maslow AH (1943) A theory of human motivation. Psychol Rev 50, 370–396. [Google Scholar]
- 53. Oral R, Ramirez M, Coohey C et al. (2016) Adverse childhood experiences and trauma informed care: the future of health care. Pediatr Res 79, 227–233. [DOI] [PubMed] [Google Scholar]
- 54. Weaver LJ & Hadley C (2009) Moving beyond hunger and nutrition: a systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol Food Nutr 48, 263–284. [DOI] [PubMed] [Google Scholar]
- 55. Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health et al . (2012) The lifelong effects of early childhood adversity and toxic stress. Pediatrics 129, e232–e246. [DOI] [PubMed] [Google Scholar]
- 56. Towbes LC & Cohen LH (1996) Chronic stress in the lives of college students: scale development and prospective prediction of distress. J Youth Adolesc 25, 199–217. [Google Scholar]
- 57. Eisenberg D, Golberstein E & Hunt JB (2009) Mental health and academic success in college. BE J Econ Anal Policy 9, 40. [Google Scholar]
- 58. Hysenbegasi A, Hass SL & Rowland CR (2005) The impact of depression on the academic productivity of university students. J Ment Health Policy Econ 8, 145–151. [PubMed] [Google Scholar]
- 59. Snyder CR, Shorey HS, Cheavens J et al. (2002) Hope and academic success in college. J Educ Psychol 94, 820–826. [Google Scholar]
- 60. Goldrick-Rab S (2018) It’s hard to study if you’re hungry. The New York Times, 14 January 2018. https://www.nytimes.com/2018/01/14/opinion/hunger-college-food-insecurity.html (accessed November 2018).
- 61. Dewey C (2018) The hidden crisis on college campuses: many students don’t have enough to eat. The Washington Post, 3 April 2018. https://www.washingtonpost.com/news/wonk/wp/2018/04/03/the-hidden-crisis-on-college-campuses-36-percent-of-students-dont-have-enough-to-eat/ (accessed November 2018).
- 62. College and University Food Bank Alliance (2018) Homepage. https://sites.temple.edu/cufba/ (accessed May 2018).
- 63. US Department of Agriculture (2016) Supplemental Nutrition Assistance Program (SNAP): Students. https://www.fns.usda.gov/snap/students (accessed May 2018).