Abstract
Background:
Current guidelines for adult hearing-aid fittings recommend the use of a prescriptive fitting rationale with real-ear verification that considers the audiogram for the determination of frequency specific gain and ratios for wide dynamic range compression. However, the guidelines lack recommendations for how other common signal processing features (e.g. noise reduction, frequency lowering, directional microphones) should be considered during the provision of hearing-aid fittings and fine-tunings for adult patients.
Purpose:
The purpose of this survey was to identify how audiologists make clinical decisions regarding common signal processing features for hearing-aid provision in adults.
Research Design:
An online survey was sent to audiologists across the United States. The 22 survey questions addressed four primary topics including demographics of the responding audiologists, factors affecting selection of hearing-aid devices, the approaches used in the fitting of signal processing features and the strategies used in the fine tuning of these features.
Study Sample:
A total of 251 audiologists who provide hearing aid fittings to adults completed the electronically-distributed survey. The respondents worked in a variety of settings including private practice, physician offices, university clinics, and hospitals/medical centers.
Data Collection and Analysis:
Data analysis was based on a qualitative analysis of the question responses. The survey results for each of the four topic areas (demographics, device selection, hearing aid fitting, and hearing aid fine tuning) are summarized descriptively.
Results:
Survey responses indicate that audiologists vary in the procedures they use in fitting and fine-tuning based on the specific feature, such that the approaches used for the fitting of frequency specific gain differs from other types of features (i.e. compression time constants, frequency lowering parameters, noise reduction strength, directional microphones, feedback management). Audiologists commonly rely on prescriptive fitting formulas and probe microphone measures for the fitting of frequency specific gain and rely on manufacturer’s default settings and recommendations for both the initial fitting and the fine-tuning of signal processing features other than frequency specific gain.
Conclusions:
The survey results are consistent with a lack of published protocols and guidelines for fitting and adjusting signal processing features beyond frequency-specific gain. To streamline current practice, a transparent evidence based tool that enable clinicians to prescribe the setting of other features from individual patient characteristics would be desirable.
Keywords: adults, audiologist, guidelines, hearing aids, hearing loss, signal processing features, survey
Introduction
As a common treatment for adults with hearing loss, hearing aids provide amplification and signal processing with the goals of improving audibility, listener comfort, speech intelligibility and sound quality. Key factors influencing satisfaction among adults who use hearing aids relate to sound quality (e.g., clarity, naturalness and richness) and to the effectiveness of advanced hearing aid features (Abrams & Kihm, 2015). Common features in commercial hearing aids include wide dynamic range compression (WDRC), noise reduction, frequency lowering, directional microphones, and feedback management (e.g., Kates, 2008).
Guidelines from both the American Academy of Audiology (Valente et al., 2006) and the American Speech-Language-Hearing Association (ASHA: ASHA Ad Hoc Committee on Hearing Aid Selection and Fitting, 1998) provide audiologists with sets of recommendations for the treatment of adults with hearing loss including the fitting of hearing aids. Both guidelines recommend the use of a prescriptive fitting rationale with real-ear probe microphone verification, using the audiogram as the basis for the determination of frequency specific gain and compression ratios (c.f. Moore et al., 2010; Polonenko et al. 2010; Keidser et al., 2011). Specific mention is also made in the AAA guidelines of the effect of cognitive status on the selection of WDRC time constants; that is, those with limited cognitive abilities may not benefit from fast time constants (c.f., Lunner and Sundewall-Thoren, 2007; Rudner et al., 2009; Souza et al., 2015). However, neither guideline provides recommendations for how to consider parameter settings for other common hearing-aid features when INITIALLY FITTING A HEARING AID OR WHEN fine-tuning a hearing aid.
Additional resources beyond the traditional guidelines are available for clinical service providers when considering hearing-aid features. Several studies show that optimum settings of hearing aid signal processing parameters may depend on a complex interplay between the signal processing feature, individual patient factors, and listening conditions (e.g., Gatehouse et al., 2003; Galster and Rodemerk, 2013; Keidser et al., 2013; Hopkins et al., 2014; Souza et al. 2015). In addition, several studies have explored the effects of WDRC on noise reduction (e.g. Anderson et al., 2009; Brons, Houben, & Dreschler, 2015) and on spectral enhancement (Franck et al., 1999), and show that the effects of one algorithm are modified when it is implemented in combination with a second signal processing algorithm. These studies also suggest that assessments beyond the audiogram may provide evidence to guide the customization of signal processing features for individual patients such as measures of loudness perception and speech in noise evaluations. Audiologists may also gain information regarding how to fit and adjust specific signal processing features through brand-specific materials from manufacturers (e.g., Galster et al., 2011), through articles in trade journals ( e.g., Appleby, 2012; Chung, 2014), from fitting tutorials (e.g., Alexander, 2016a,b) and from patient report (e.g., Galster et al., 2011; Jenstad, Van Tasell, & Ewert, 2003).
The extent to which audiologists use these varied sources of guidance in adult hearing aid fittings has not been well documented. Thus, the purpose of this study was to use a survey to characterize how audiologists currently consider signal processing features in the provision of hearing aids to adults including in the initial fitting of the device and in the fine-tuning of the device. Given the lack of specific recommendations for the fitting of common signal processing features in currently available guidelines, it was hypothesized that audiologists depend on information obtained from manufacturers and their own expertise in the fitting of common signal processing features in hearing aids.
Methods
Survey
The Qualtrics Survey Platform was used to implement the survey. This survey was created using principles described by Swoboda et al. (1997) including simplicity, completeness, relevance, and neutrality. Additionally, we considered the length of time it would take to complete the survey, as the literature shows that longer surveys are less likely to be completed (e.g. Sheean and McMillan, 1999). For our survey, the introductory email followed the recommendations of Swoboda et al (1997) and included information about who was conducting the survey and the fact that it was scientific (as opposed to commercial). In addition, the email also indicated that no identifying information would be collected from survey respondents. A link to the online survey was included in the introductory email. Only one email invitation was sent to each email address. The survey questions were written by the study authors who are certified/licensed audiologists active in amplification research and clinical service provision. Initial drafts of the survey were reviewed and edited by ten additional clinical and research audiologists for completeness, ease of understanding, and relevance. All of the additional reviewing audiologists and researchers were active in the field of amplification. The survey included objective questions in multiple choice and rank ordering formats. A copy of the survey can be found in Supplemental AppendixS1, supplemental to the online version of the article.
The survey questions addressed four primary topics. The first topic (4 questions) related to the demographics of respondents and asked about career timeline, number of hearing aid fittings completed in a month, and certification and licensure. The second area (1 question) related to hearing aid selection, and asked about the importance of signal processing features in the selection of a specific device for an individual patient. The final two sections (8 questions each) explored how decisions are made regarding the fitting and fine tuning of common signal processing features. The survey was approved by the University of Colorado Institutional Review Board.
The survey took approximately five minutes, on average, to complete. Skipping questions did not limit participation or completion of the survey.
Recipients
This study focused on clinical audiologists who perform hearing aid fittings on adults. Between January-February 2016, links to the survey were emailed to 1124 individual audiologists. Email addresses were obtained through publically available membership directories for professional organizations in the United States of America (USA) associated with audiology and amplification. The survey link was also posted to the electronic mailing lists of professional organizations in the USA associated with audiology and amplification. In addition, the survey link was sent to state-level audiology and/or speech and hearing associations for dissemination to their members. Additional audiologists may have responded to the survey through electronic discussion boards, or because their state association sent them the survey link. A total of 251 audiologists responded to the survey as of the closing date (February 19, 2016). Due to the nature of the survey dissemination (posting links, electronic mailing lists), it is not possible to determine the total number of audiologists who received the survey invitation, and hence, to calculate the response rate.
Results
The survey results for each of the four topic areas (demographics, device selection, hearing aid fitting, and hearing aid fine-tuning) are summarized descriptively. The percentage of responses for each section of the survey were calculated by considering how many individuals who completed some portion of the survey completed each section. For demographic questions, >97% of respondents answered these questions. The selection and fitting questions had responses for >95% of survey respondents. Fine-tuning questions had responses by >90% of survey respondents.
Demographics of Survey Respondents
Of the 251 respondents, three indicated that they do not fit any adults with hearing aids each month, and as such, their surveys were excluded from further analysis. Of the remaining 248 responses, 20% fit 1–5 adults a month, 36% reported fitting between 6–10 adults a month, 33% reported fitting up to 20 adults a month, and 10% reported fitting more than 20 adults in a month. Survey respondents were questioned regarding the number of years they have been fitting hearing aids on adult patients. Most respondents (75%) reported service provision of more than 10 years. For the remaining respondents, 2% reported <1 yr, 15% reported 1–5 yr, and 8% reported 6–10 yr of clinical service provision.
The clinical setting of our survey respondents showed a variety of locations. The largest percentage of respondents worked in a private practice (53%), with the next largest group employed in an ENT/physician office (19%). Other work sites included colleges or universities (10%), hospitals or medical centers (both VA (3%) and non-VA (8%)), and franchise or retail chains (4%). The demographic variables of years of service and clinical work setting were consistent with national estimates of demographic variables for practicing audiologists (ASHA, 2015).
Device Selection
A number of factors – including the availability of specific signal processing features – may influence the selection of a particular device for an individual patient. In the survey, we asked respondents to indicate how important a number of pre-chosen possible factors were in making a specific device selection (Table 1). Survey respondents indicated that the most important factors influencing device selection were the degree of hearing loss, the patient’s listening environments, the specific signal processing features of the device, and the audiologist’s comfort and experience with a particular manufacturer.
Table 1.
Importance rating of factors associated with device selection.
| Factor | Very important | Somewhat important | Not Important |
|---|---|---|---|
| Clinic is a single-brand facility | 3% | 12% | 85% |
| My experience and comfort with this instrument | 73% | 25% | 2% |
| Price of device to clinic | 31% | 46% | 23% |
| Price of device to patient | 49% | 41% | 11% |
| Manufacturer customer service/relationship with rep | 53% | 35% | 13% |
| Degree of hearing loss | 78% | 21% | 1% |
| Patient listening environment | 87% | 12% | 0% |
| Specific signal processing features | 81% | 19% | 0% |
Hearing Aid Fitting
We asked respondents to identify their strategies for performing the initial fitting of a hearing aid on a patient. The survey was divided into tools used in the general fitting of a hearing aid (e.g. audiometric evaluation, probe measurements) and in the fitting of specific signal processing features (e.g. prescriptive fitting rationales, manufacturers “first fit”).
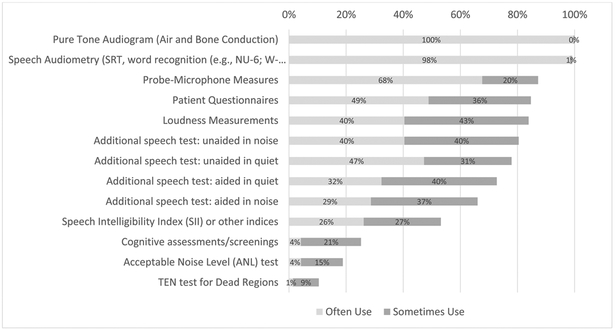
Respondents were asked to indicate if they “often use”, “sometimes use”, or “never use” a variety of clinical measures in the initial fitting of hearing aids. As shown in Figure 1, all of the audiologists reported routinely using information from the audiological evaluation including air and bone conduction thresholds, speech reception thresholds, and suprathreshold word recognition. Other commonly used tools included probe microphone measures, patient questionnaires, loudness measures, and additional speech tests (both aided and unaided). Approximately half of the respondents reported often or sometimes using the Speech Intelligibility Index (SII). Less than 25% of audiologists reported routinely using cognitive screenings and other special tests such as the Acceptable Noise Level (ANL) test (Nabelek et al, 2006) and the Threshold Equalizing Noise (TEN) test for dead regions (Moore et al., 2004).
Figure 1.
Percentage of respondents who often or sometimes used the identified tool in the initial fitting of hearing aids.
In the initial fitting of a hearing aid, a number of signal processing features are typically enabled. As shown in Table 2, we asked respondents to identify their primary strategy for performing the initial fitting of different signal processing features. In general, many audiologists rely on the manufacturers’ first fit for the fitting of different signal processing features, with the exception of frequency-specific gain. For frequency specific gain, 51% indicated using a prescriptive fitting method and 35% indicate using manufacturers’ first fit. In the initial fitting of other types of signal processing, the majority of audiologists reported using manufacturers’ first fit for WDRC time constants (80%), noise suppression (58%), feedback management (69%), and directional microphones (66%). Fewer audiologists reported using their own expertise or other approaches in the initial fitting of these features. Regarding frequency lowering, 40% used manufacturers’ first fit, 36% used their own expertise or other approach, and 17% disabled this feature at the initial fitting.
Table 2.
Most common approach used by respondents in the fitting of signal processing features. Respondents were instructed to choose one approach.
| Gain | WDRC Time Constants |
Noise Suppression |
Feedback | Directional Mic |
Frequency Lowering |
|
|---|---|---|---|---|---|---|
| Approach | ||||||
| Prescriptive (NAL-NL1/2; DSL v 5/m[i/o]) | 44%^ | NA | NA | NA | NA | NA |
| Manufacturer's "first fit" | 40%^ | 80%* | 58%* | 69%* | 67%* | 35%^ |
| My own expertise | 14%^ | 18%^ | 38%^ | 25%^ | 30%^ | 36%^ |
| Other approach | 1% | 2% | 3% | 3% | 3% | 6% |
| Do not use at initial fit | 0% | 0% | 2% | 3% | 0% | 17%^ |
A * in cells indicates approach most commonly used by a majority (>50%) of audiologists;
a ^ in cells indicates most common approach used by some (10-50%) audiologists;
NA indicates the approach is not applicable.
Hearing Aid Fine-Tuning
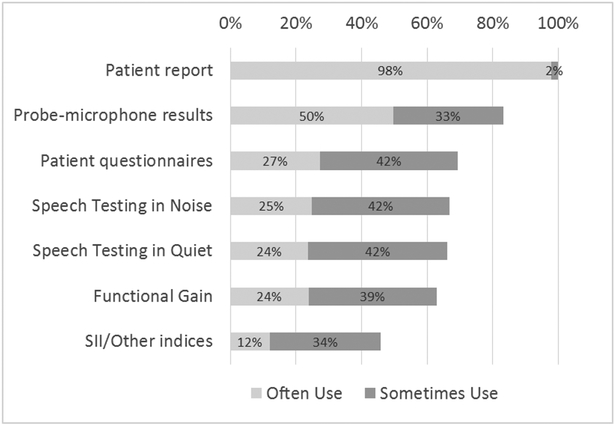
Figure 2 summarizes several tools and strategies used by respondents in the fine-tuning process. All of the audiologists reported that they rely on patient report. Most audiologists reported routinely using probe microphone measures (83%). Respondents also reported using patient questionnaires often (27%) and sometimes (42%). Similarly, speech testing in quiet and in noise was often used (25%) and sometimes used (42%). Functional gain was often (24%) and sometimes (39%) used in fine-tuning. Less than 46% of audiologists reported routinely using the SII. When considering fine-tuning features at follow-up visits, respondents again indicated using a variety of strategies, as shown in Table 3. In the fine-tuning of signal processing features the majority of audiologists reported that they rely on patient reports for fine-tuning WDRC gain (98%), noise suppression (96%), feedback management (81%), directional microphones (86%), and frequency lowering (82%). Audiologists also reported that they rely on their own expertise for fine-tuning WDRC gain (95%), noise suppression (91%), feedback management (87%), and directional microphones (87%), and frequency lowering (80%). Reports regarding strategies used for fine-tuning of WDRC time constants were more variable with 35% of audiologists reporting they do not fine-tune this feature. Of those who do fine tune time constants, common tools included patient report (48%), their own expertise (52%), and manufacturers’ software recommendations (46%). In general, audiologists reported that they were much less likely to use measures based on individual patient factors for the fine tuning of any signal processing features (i.e. loudness measures, cognitive screening, measures for dead regions, and noise tolerance). No consistent trends were observed between the survey responses for device selection, fitting, and fine-tuning and audiologists’ demographic characteristics (i.e. number of years of clinical service provision and clinical work site).
Figure 2.
Percentage of respondents who often or sometimes used the identified tool in the fine tuning of hearing aids.
Table 3.
Approaches used in fine tuning signal processing features. Respondents were instructed to choose all applicable approaches and were able to select more than one approach.
| Gain | WDRC Time Constant |
Noise Suppression |
Feedback | Directional Mic |
Frequency Lowering |
|
|---|---|---|---|---|---|---|
| Approach | ||||||
| I do not use/ No Approach | NA | 0% | 0% | 1% | 0% | 8% |
| No fine tuning | NA | 35%^ | 1% | 4% | 5% | 2% |
| Patient report | 98%* | 48%^ | 96%* | 81%* | 86%* | 82%* |
| Manufacturer's software recommendation | 42%^ | 46%^ | 55%* | 59%* | 50%^ | 49%^ |
| My own expertise | 95%* | 52%^ | 91%* | 87%* | 87% | 80% |
| Info: articles, conferences, colleagues | 51%* | 27%^ | 42%^ | 27%^ | 40%^ | 37%^ |
| Info: manufacturer | 37%^ | 22%^ | 36%^ | 29%^ | 35%^ | 31%^ |
| Loudness measures | 27%^ | 7% | 10%^ | 5% | 4% | 4% |
| TEN test for dead regions | 3% | 1% | 1% | 1% | 1% | 0% |
| Cognitive Assessments/Screenings | 3% | 3% | 3% | 0% | 1% | 3% |
| Acceptable Noise Level Tests | 5% | 3% | 4% | 2% | 1% | 2% |
A * in cells indicates approaches used by a majority (>50%) of audiologists;
a ^ in cells indicates approach used by some (10-50%) audiologists;
NA indicates the approach is not applicable (NA).
Discussion and Conclusions
This study considered the responses from 248 audiologists on adult hearing aid fitting and fine-tuning practices. We sought to determine the tools and strategies used by clinical service providers for making decisions about device selection and signal processing feature setting and manipulation. The results of the survey are consistent with current AAA and ASHA guidelines in that audiologists reported using basic audiometry results and consideration of patient lifestyle for the initial device selection. Audiologists reported that they consider the range of signal processing features that are available in a device. However, other factors were also relevant to the audiologist when choosing a hearing aid, including the price of the device and the relationship the audiologist has with the manufacturer.
When considering the fitting and fine-tuning of the hearing-aid features, respondents reported a willingness to embrace evidence-based practice. For example, the majority of responding audiologists reported at least sometimes using probe microphone measures and prescriptive formulas for the fitting of frequency-specific gain. However, our results indicate more variability in the approaches used for the fitting and fine-tuning of signal processing features beyond frequency-specific gain. For example, audiologists reported using “my own expertise” as a primary approach for fine-tuning. While this type of evidence (expert opinion) is not at the highest level, it is an integral form of evidence-based practice, especially in situations where higher levels of evidence are not available in the literature (Cox, 2005). Respondents also commonly used the manufacturer software suggestions and defaults for fitting and fine-tuning signal processing features. These suggestions and defaults are typically proprietary, and as such the level of evidence is difficult to discern (Cox, 2005). Ideally, audiologists would have access to, and utilize, transparent links between evidence from the clinical research literature to manufacturer recommendations for specific devices.
The survey results showed that audiologists were much less likely to consider patient factors beyond the audiogram. Very few respondents indicated using cognitive screening assessments, loudness measures, or other tests beyond the audiogram, even though those evaluations have been shown to provide information related to the benefits of particular signal processing features (e.g., Preminger et al., 2005; Mueller et al., 2006; Souza et al., 2015). Reasons contributing to this issue likely include a limited literature that provides guidance regarding the translation of these research findings into clinical practice. While there are some tools available for the fitting of a signal processing feature such as frequency lowering in isolation (e.g., Alexander, 2016a,b), no tool currently exists which considers the fitting and fine-tuning of signal processing features in combination as they are currently implemented in commercial hearing aids.
In consideration of the demographics of this survey, it is important to consider how the respondents are representative of the demographics of practicing audiologists in the United States. The majority of the respondents to this survey have greater than 10 yr of clinical experience. A second consideration is the clinical work setting of the audiologist. The respondents to this survey were similar to the demographics of practicing audiologists (ASHA, 2015) both in terms of years of service and in employment facility, indicating a representative sample of audiologists.
It is important to acknowledge the limitations of the current survey. One limitation was the relied on self-report of tools and strategies used, and sevice providers may have overestimated their use of some tools and strategies. For example, it has been reported that consistent use of probe microphone measures is typically completed by approximately 40% of audiologists (Mueller, 2005; Mueller and Picou, 2010). In contrast, our respondents indicated using probe microphone measures more frequently (50% indicate often using and an additional 33% indicate sometimes using). It may be that audiologists were familiar with best practice guidelines from AAA and ASHA and therefore reported more frequently using this technique, or it may be that individuals who chose to respond to a survey on hearing aid fitting practices did actually perform more real ear verification than the general population of audiologists. An additional consideration was the survey format. The use of questions that contained pre-selected choices rather than open-ended questions may have missed other less common approaches that audiologists may employ when considering hearing-aid features in adult hearing-aid services.
The results of the survey highlight how audiologists considered hearing aid features in adult amplification fitting and fine-tuning. The results also indicate audiologists had a willingness to use evidence-based fitting and fine-tuning procedures. Such a willingness is consistent with recent reports regarding audiologists who provide pediatric amplification services (Moodie et al, 2016). To streamline the fitting and fine-tuning of hearing aids, next steps should include the development of clinical guidelines which consider the many signal-processing features currently in use in commercial devices. These guidelines should address individual patient factors and should be generalizable across devices and manufacturers.
Supplementary Material
Acknowledgements
This research was supported by the National Institutes of Health (R01 DC012289). We would like to thank Madison Sankovitz, Elizabeth Falconer and Elizabeth McNichols for assistance with data collection.
Abbreviations:
- ANL
Acceptable Noise Level
- ASHA
American Speech-Language Hearing Association
- SII
Speech Intelligibility Index
- TEN
Threshold Equalizing Noise
- WDRC
Wide Dynamic Range Compression
Footnotes
Portions of this study were presented at the Audiology Now conference of the American Academy of Audiology, April 2016, Phoenix, Az.
References
- Abrams HB, Kihm J. (2015) An Introduction to MarkeTrak IX: A New Baseline for the Hearing Aid Market. Hear Rev 22(6):16. [Google Scholar]
- Alexander J (2016a) Frequency Lowering Fitting Assistants. Purdue University EAR lab; Retrieved from http://web.ics.purdue.edu/~alexan14/fittingassistants.html [Google Scholar]
- Alexander J (2016b) Nonlinear frequency compression: Influence of start frequency and input bandwidth on consonant and vowel recognition. J Acoust Soc Am 139: 938–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson MC, Arehart KH, Kates JM. 2009The acoustic and perceptual effects of series and parallel processing. EURASIP J Adv Signal Process.. doi: 10.1155/2009/619805 [DOI] [Google Scholar]
- Appleby R (2012) Noise management in modern hearing aids fititngs, Hear Rev 19(5): 44–51. [Google Scholar]
- ASHA Ad Hoc Committee on Hearing Aid Section and Fitting. (1998) Guidelines for hearing aid fitting for adults. Am J Audiol 7: 5–13.26649513 [Google Scholar]
- American Speech-Language-Hearing Association (ASHA). (2015) 2014 Audiology Survey report: Survey methodology, respondent demographics, and glossary. Available from www.asha.org.
- Brons I, Houben R, Dreschler WA. (2015) Acoustical and Perceptual Comparison of Noise Reduction and Compression in Hearing Aids. J Speech Lang Hear Res 58(4):1363–76. doi: 10.1044/2015_JSLHR-H-14-0347. [DOI] [PubMed] [Google Scholar]
- Chung K (2014) Frequency compression: New research yields clues for patient selection. Hear J 67:14–16. [Google Scholar]
- Cox RM. (2005) Evidence-based practice in provision of amplification. .J Am Acad Audiol 16(7):419–438. [DOI] [PubMed] [Google Scholar]
- Franck BA 1, van Kreveld-Bos CS, Dreschler WA, Verschuure H. (1999) Evaluation of spectral enhancement in hearing aids, combined with phonemic compression. J Acoust Soc Am 106(3 Pt 1):1452–64. [DOI] [PubMed] [Google Scholar]
- Galster JA, Rodemerk KS. (2013) Individual variability in benefit from fixed and adaptive directional microphones. Semin Hear 34(1): 110–117. [Google Scholar]
- Galster JA, Valentine S, Dundas JA, Fitz K. (2011) Spectral iQ: Audibly improving access to high-frequency sounds. Eden Prairie, MN: White paper, Starkey Laboratories Inc. [Google Scholar]
- Gatehouse S, Naylor G, Elberling C. (2003) Benefits from hearing aids in relation to the interaction between the user and the environment. Int J Audiol 42(Suppl. 1): 77–85. [DOI] [PubMed] [Google Scholar]
- Hopkins K, Khanom M, Dickinson AM, Munro KJ. (2014) Benefit from non-linear frequency compression hearing aids in a clinical setting: The effects of duration of experience and severity of high-frequency hearing loss. Int J Audiol 53(4): 219–228. [DOI] [PubMed] [Google Scholar]
- Jenstad LM, Van Tasell DJ, & Ewert C (2003). Hearing aid troubleshooting based on patients’ descriptions. Journal of the American Academy of Audiology, 14(7), 347–360. [PubMed] [Google Scholar]
- Kates J (2008) Digital Hearing Aids, San Diego, CA: Plural Publishing. [Google Scholar]
- Keidser G, Dillon H, Flax Mm Ching T, Brewer S (2011) The NAL-NL2 prescription procedure. Audiol Res 1(24): 88–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keidser G, Dillon H, Convery E, Mejia J. (2013) Factors influencing individual variation in perceptual directional microphone benefit. J Am Acad of Audiol 24(10): 955–968. [DOI] [PubMed] [Google Scholar]
- Lunner T, Sundewall-Thoren E. (2007) Interactions between cognition, compression, and listening conditions: effects on speech-in-noise performance in a two-channel hearing aid. J Am Acad Audiol 18: 604–617. [DOI] [PubMed] [Google Scholar]
- Moodie S, Rall E, Leisha Eiten L, Lindley G, Gordey D, Davidson L, Bagatto M, Scollie S. (2016) Pediatric audiology in North America: Current clinical practice and how it relates to the American Academy of Audiology Pediatric Amplification Guideline Journal of the America Academy of Audiology Am Acad Audiol 27:166–187. [DOI] [PubMed] [Google Scholar]
- Moore BCJ, Glasberg BR, Stone MA. (2004) New version of the TEN test with calibrations in dB HL. Ear and Hearing 25, 478–487. [DOI] [PubMed] [Google Scholar]
- Moore BCJ, Glasberg BR, Stone MA. (2010) Development of a new method for deriving initial fittings for hearing aids with multi-channel compression: CAMEQ2-HF. Int J Audiol 49:216–227. [DOI] [PubMed] [Google Scholar]
- Mueller HG, Weber J, & Hornsby BW (2006). The effects of digital noise reduction on the acceptance of background noise. Trends in Amplification 10(2): 83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller HG, Picou EM. (2010) Survey examines popularity of real-ear probe-microphone measures. Hear J 63(5): 27–32. [Google Scholar]
- Mueller HG. (2005) Probe-mic measures: Hearing aid fitting’s most neglected element. Hear J 57(10): 33–41. [Google Scholar]
- Nabelek AK, Freyaldenhoven MC, Tampas JW, Burchfiel SB, Muenchen RA. (2006) Acceptable noise level as a predictor of hearing aid use. J Am Acad of Audiol 17(9): 626–639. [DOI] [PubMed] [Google Scholar]
- Polonenko MJ, Scollie S, Moodie S, Seewald R, Laurnagaray D, Shantz J, et al. (2010) Fit to targets, preferred listening levels, and self-reported outcomes for the DSL v5.0a hearing aid prescription for adults. Int J Audiol 48: 550–560. [DOI] [PubMed] [Google Scholar]
- Preminger JE, Carpenter R, Ziegler CH (2005). A clinical perspective on cochlear dead regions: intelligibility of speech and subjective hearing aid benefit. J Am Acad of Audiol 16(8): 600–613. [DOI] [PubMed] [Google Scholar]
- Rudner M, Foo C, Rönnberg J, Lunner T. (2009) Cognition and aided speech recognition in noise: specific role for cognitive factors following nine-week experience with adjusted compression settings in hearing aids. Scand J Psychol 50: 405–418. [DOI] [PubMed] [Google Scholar]
- Sheehan KB & McMillan SJ (1999). Response variation in e-mail surveys: An exploration. Journal of Advertising Research 39(4): 45–54. [Google Scholar]
- Souza PE, Arehart KH, Neher T. (2015) Working memory and hearing aid processing: literature findings, future directions, and Clinical Applications. Front Psychol 6: 1894 Published online 2015 December 16. doi: 10.3389/fpsyg.2015.01894. PMCID: PMC4679849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swoboda WJ, Muhlberger N, Weikunat R & Schneeweiss S (1997). Internet surveys by ¨ direct mailing. An innovative way of collecting data. Social Science Computer Review 15(3): 242–255. [Google Scholar]
- Valente M, Abrams H, Benson D, et al. (2006) Guidelines for the audiological management of adult hearing impairment. Audiol Today 18(5): 1–44. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.