Abstract
BACKGROUND:
Home time, the number of days alive and spent out of hospital and skilled nursing facility, has been proposed as a patient-centered outcome that can be readily calculated in administrative claims data.
OBJECTIVES:
To compare home time against existing patient-centered outcome measures.
DESIGN:
Retrospective cohort study.
SETTING:
Community.
PARTICIPANTS:
4,594 Medicare beneficiaries 65 years or older with complete survey and claims data in the Medicare Current Beneficiary Survey 2010–2011.
MEASUREMENTS:
Home time was calculated from the 2011 claims data (range: 0 to 365 days). The 1-year incidence of patient-centered outcomes (poor self-rated health, mobility impairment, depression, limited social activity, and difficulty in self-care) was measured. The minimum clinically important difference (MCID) was derived by contrasting the mean home time between those who experienced functional decline or death and those who did not.
RESULTS:
The mean home time was 355.8 days (standard deviation: 42.1 days); 84.1% had a home time of 365 days and 5.7% had ≤336 days. The incidence of poor self-rated health ranged from 2% (home time 365 days) to 21% (home time <337 days). Similarly, the corresponding incidence risks were 11% to 59% for mobility impairment, 5% to 19% for depression, 17% to 67% for limited social activity, and 13% to 68% for difficulty in self-care. The risk of mobility impairment, depression, and difficulty in self-care increased steeply after home time loss ≥15 days. The MCID of home time was 18.6 days.
CONCLUSION:
A loss in home time is associated with decline in several patient-centered outcome measures in community-dwelling Medicare beneficiaries. These results provide empirical evidence to promote adoption of home time and its clinical interpretation for database studies of medical interventions.
Keywords: home time, patient-centered outcome, administrative claims data
INTRODUCTION
Patient-centered outcomes measure health status that is meaningful to patients, such as quality of life, functional status, and independent living.1 Consideration of these outcomes is essential for shared decision-making about medical therapy as they incorporate the patient’s point of view on treatment benefits, harms, and burden. Although patient-centered outcomes are increasingly collected in clinical studies of older adults, they are not reliably available for database studies.
Recently, the number of days alive and spent out of hospitals and skilled nursing facilities (SNFs) in a given time period, also known as “home time”, has been proposed as a measure of quality of life.2 Home time can be conveniently obtained from administrative claims data and has been endorsed by patients as a meaningful health outcome3–11, and can be more intuitively understood. However, not all hospitalizations and SNF stays represent poor health or low quality of life in older adults. In fact, some hospitalizations (e.g., knee replacement for severe osteoarthritis, treatment of acute infections) may be beneficial for maintaining independence. Moreover, little evidence exists on how a reduction in home time relates to changes in commonly used patient-centered outcome measures in older adults, such as self-rated health, functional status, mood, and social activity limitations.
The objective of our study was to examine the distribution of home time in a representative sample of community-dwelling Medicare beneficiaries and its association with changes in known patient-centered outcome measures. Knowledge about thresholds beyond which a further reduction in home time is clearly associated with worsening patient-centered outcomes will promote future application and interpretation.
METHODS
Data Source and Study Population
This study used the 2010–2011 data from the Medicare Current Beneficiary Survey (MCBS). The MCBS is a rotating panel survey of a nationally representative sample of Medicare beneficiaries.12,13 The beneficiaries participated in 12 rounds of survey over 4 years, and the survey data are linked to their Medicare claims data. During the annual fall interviews, beneficiaries or their proxies are asked about health status, including patient-centered outcome measures (see Measurements of Patient-Centered Outcomes below). We included 4,594 community-dwelling Medicare beneficiaries 65 years or older whose claims data were available for the entire calendar year of 2011. Home time was calculated from the 2011 claims data and compared against the changes in patient-centered outcomes between 2010 and 2011 fall interviews. This study was determined as exempt by the Institutional Review Board of the Brigham and Women’s Hospital.
Calculation of Home Time
Home time was calculated by subtracting the total number of days spent in hospitals and SNFs (including rehabilitation facility) from the total number of follow-up days in the 2011 claims data. It can range from 0 days (i.e., spending all days before death in a hospital or SNF) to 365 days (i.e., spending the entire year at home without any hospitalizations or SNF stays). We categorized beneficiaries into 5 groups of home time: 365 days (no loss in home time), 358–364 days (1 to 7-day loss), 351–357 days (8 to 14-day loss), 337–350 days (15 to 28-day loss), <337 days (>28-day loss), and deceased.
Measurements of Patient-Centered Outcomes
The following patient-centered outcomes were collected from the 2010 and 2011 fall interviews: poor self-rated health (poor self-rated general health compared to others same age), mobility impairment (any difficulty walking ¼ miles), depression (having been told by health care providers having depression in the past year), limited social activity (limited social activity due to health in the past month), and difficulty in self-care (any difficulty in bathing, dressing, eating, transferring, walking, toileting). These measures were analyzed as dichotomized variables. In addition, the total functional limitation score was calculated by counting the number of the following 17 tasks that beneficiaries reported difficulty with: 6 self-care activities listed above, telephone use, light house work, heavy house work, meal preparation, shopping, managing money, stooping/crouching/kneeling, lifting 10 pounds, extending arms above shoulder, writing, and walking a ¼ mile.
Statistical Analysis
Characteristics at the time of 2010 survey were compared across the home time categories (365 days, 358–364 days, 351–357 days, 337–350 days, <337 days, and deceased) using the analysis of variance or Kruskal-Wallis test for continuous variables and chi-square test for categorical variables. To examine how home time is associated with patient-centered outcomes, we assessed the proportions of incident cases of poor self-rated health, mobility impairment, depression, limited social activity, and difficulty in self-care at the 2011 survey among those without respective outcomes at the 2010 survey.
We also determined a minimum clinically important difference (MCID)14 in home time using the total functional limitation score or death as an anchor. MCID was defined as a mean difference in home time between beneficiaries who had stable or less functional limitations and those who had more functional limitations or died during the year. Those with maximum limitations at the 2010 survey (i.e., those who could not decline further) were excluded. Analyses were conducted in SAS 9.4 (SAS Institute Inc, Cary, NC) and a 2-sided p-value <0.05 was considered statistically significant.
RESULTS
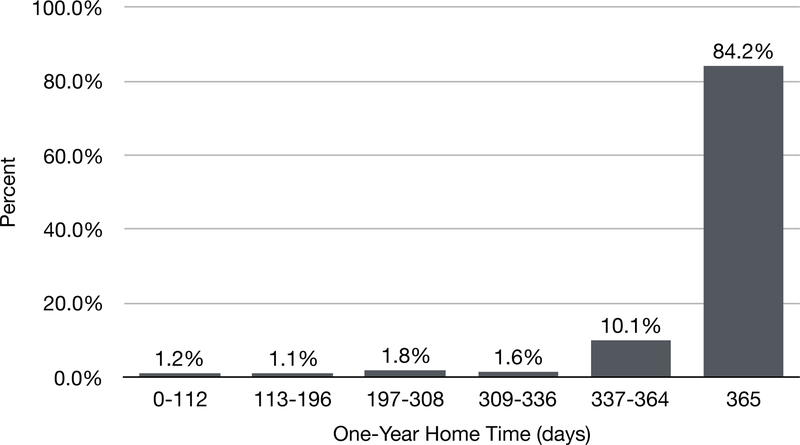
The mean home time of 4,594 community-dwelling Medicare beneficiaries was 355.8 days (standard deviation: 42.1 days). The distribution was left-skewed (Figure 1) with a large majority (84.1%) having 365 days of home time. The beneficiaries who had shorter home time or died within the year were older and more likely to have poor self-rated health, mobility impairment, depression, limited social activity, difficulty in self-care, and functional limitations at baseline (Table 1).
Figure 1.
Distribution of Home Time in Community-Dwelling Medicare Beneficiaries from the Medicare Current Beneficiary Survey 2011
Table 1.
Clinical Characteristics According to Home Time Categories in Community-Dwelling Medicare Beneficiaries in the Medicare Current Beneficiary Survey 2010.a
| Characteristics | One-year home time (home time loss) among survivors | Deceased | ||||
|---|---|---|---|---|---|---|
| 365 days (0 days) | 358–364 days (1–7 days) | 351–357 days (8–14 days) | 337–350 days (15–28 days) | <337 days (>28 days) | ||
| Sample size, n | 3862 | 327 | 71 | 59 | 75 | 200 |
| Home time, days, mean ± SD | 365.0 ± 0.0 | 361.9 ± 1.7 | 354.2 ± 2.2 | 344.3 ± 3.9 | 315.4 ± 22.0 | 187.6 ± 99.9 |
| Age, mean ± SD | 77.3 ± 7.3 | 78.6 ± 6.8 | 79.6 ± 7.3 | 78.6 ± 6.5 | 80.9 ± 6.8 | 82.6 ± 7.8 |
| Female, n (%) | 2201 (57.0) | 170 (52.0) | 40 (56.3) | 33 (55.9) | 45 (65.0) | 105 (52.5) |
| White race, n (%) | 3304 (85.6) | 296 (90.5) | 64 (90.1) | 50 (84.7) | 62 (82.7) | 171 (85.5) |
| Poor self-rated health, n (%) | 132 (3.4) | 19 (5.8) | 8 (11.3) | 7 (11.9) | 8 (10.7) | 26 (13.3) |
| Mobility impairment, n (%) | 854 (22.1) | 107 (32.8) | 37 (52.1) | 29 (49.2) | 46 (61.3) | 108 (55.1) |
| Depression, n (%) | 374 (9.7) | 31 (9.5) | 12 (16.9) | 7 (11.9) | 12 (16.0) | 28 (14.3) |
| Limited social activity, n (%) | 1053 (27.3) | 134 (41.1) | 32 (45.1) | 31 (53.4) | 44 (58.7) | 114 (58.2) |
| Difficulty in self-care, n (%) | 997 (25.9) | 116 (35.6) | 39 (54.9) | 29 (49.2) | 53 (70.7) | 118 (60.2) |
| Functional limitations, mean ± SD | 3.4 ± 3.5 | 4.6 ± 3.9 | 5.4 ± 4.4 | 5.8 ± 3.8 | 7.2 ± 4.1 | 7.4 ± 4.7 |
Abbreviation: SD, standard deviation.
All comparisons were statistically significant (p<0.05).
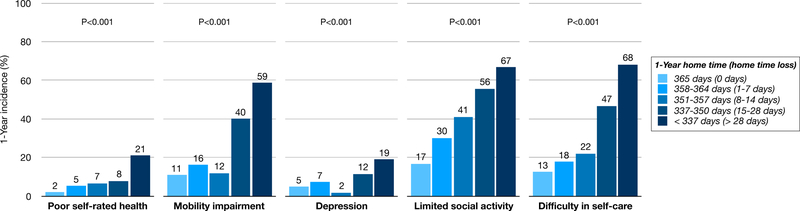
Home time was inversely associated with increased risks of worsening patient-centered outcomes among surviving beneficiaries (Figure 2). The proportion of individuals with impaired outcomes increased incrementally with decreasing home time. The incidence of poor self-rated health ranged from 2% (home time 365 days) to 21% (home time <337 days). Similarly, the corresponding incidence risks were 11% to 59% for mobility impairment, 5% to 19% for depression, 17% to 67% for limited social activity, and 13% to 68% for difficulty in self-care. Notably, the risk of mobility impairment, depression, and difficulty in self-care increased steeply after home time loss ≥15 days.
Figure 2.
Home Time and One-Year Incidence of Worsening Patient-Centered Outcomes in the Medicare Current Beneficiary Survey 2011
To determine a MCID of home time, we compared the mean home time between beneficiaries who experienced worsening functional limitation or death (345.3 ± 62.0 days) and those who did not (363.9 ± 6.3 days) during the calendar year. We deduced the MCID of home time as 18.6 days (p<0.001). That is, a mean home time reduction of 18.6 days or more is associated with worsening functional limitations or death.
DISCUSSION
In a representative sample of community-dwelling Medicare beneficiaries, reduction in home time was positively associated with poor self-rated health, mobility impairment, depressed mood, limited social activity, and difficulty in self-care. Although these findings may seem unsurprising, we found that loss in home time of 15 days or more was particularly associated with incident mobility impairment, depression, and difficulty in self-care. Our study provides empirical evidence to adopt home time as a patient-centered outcome for database studies in which other patient-centered outcomes may not be directly measurable. Based on our MCID estimate, a medical intervention that extends home time 18.6 days or more in 1 year can be considered to offer a meaningful benefit in patient-centered outcomes.
Conventionally, clinical studies evaluate the benefit of a medical therapy using time-to-event outcomes (e.g., hospitalization or death). The treatment effect is summarized in relative risks or hazard ratios. This conventional analysis has a few important limitations. Because this analysis examines time to the first event, subsequent events (e.g., recurrent hospitalizations) are ignored. If treatment reduces the risk of recurrent events, the benefit of treatment is not fully quantified.15 Moreover, if the outcome of interest is non-fatal event (e.g., hospitalization), the time-to-event analysis can be complicated by competing risk by death. Although competing risk can be statistically handled,16 the interpretation of hazard ratios is not straightforward. In general, hazard ratios or relative risk measures are not intuitively understood by lay persons and may exaggerate treatment benefits.17,18 They do not represent quality of life.
Home time overcomes several limitations of the time-to-event analysis. Home time, which quantifies the number of days alive and spent at home, can accommodate recurrent events, avoid competing risk, and reflect quality of life (i.e., being at home is considered better than staying in a hospital or nursing facility). For most lay persons, interpretation of treatment effect summarized as a gain or loss in home time is more intuitive than relative risks or hazard ratios. For these reasons, home time has been examined in relation to mortality in heart failure3–5 as well as global disability and modified Rankin score in stroke6−11 in administrative claims datasets. For example, warfarin therapy in Medicare beneficiaries with atrial fibrillation who was hospitalized for ischemic stroke was associated with a 48-day gain in home time over 2 years.10 Our results suggest that such a gain in home time (24 days per 1 year) is likely to be clinically meaningful in terms of functional status and other patient-centered outcomes.
There are some caveats to consider in interpreting the results of our study. First, we were unable to determine the quality of home time or symptom severity. Home time might represent proactive hospice enrollment near end-of-life or mask difficulty of seeking appropriate medical care due to socioeconomic barriers. Nevertheless, time spent at home is generally acknowledged to provide individuals more psychological comfort and improved quality of life than time at a healthcare facility.19,20 Second, the home time measured in this study encompassed the calendar year of 2011 (January to December); however, patient-centered outcomes were measured during the interviews conducted in the fall. Thus, the survey may have not captured changes in patient-centered outcomes after the 2011 fall survey. Lastly, we used death or functional limitations as an anchor to calculate MCID. Although our choice of anchor is justified as they represent failing health in older population, use of a different anchor may result in a different MCID value.
In conclusion, our results from a nationally representative cohort of community-dwelling Medicare populations provide empirical evidence to promote adoption of home time and its clinical interpretation for database studies of medical interventions. Since home time is readily calculated from administrative claims data, intuitively interpreted, and well correlated with existing patient-centered outcomes, more routine use of home time in addition to conventional summary measures of treatment effect can help to improve the value of medical care to older adults.
Editor’s Note.
I really like this paper because it describes a simple person-centered measure relevant to the quality of life of older people that can be obtained from administrative claims data. Most people would prefer to spend their time at home rather than in a hospital or a nursing facility. This study demonstrates the validity of this measure as a proxy for quality of life by showing its relationships with self-rated health, mobility and self-self-care difficulties, and limited social activity. However, more research is needed to further validate this measure, as not all time spent at home is high quality time, especially among vulnerable older people. Lack of resources – both financial and social, caregiver stress, unsafe home environments, and limited access to optimal health care for unstable medical conditions are all common and could also be associated with higher home time. With these caveats, I agree with the authors that home time may be a useful addition to other measures that can help improve the value of health care to the population served by geriatrics health professionals.
-Joseph G. Ouslander, MD
ACKNOWLEDGMENTS
Funding sources: This research was funded by the Paul B. Beeson Clinical Scientist Development Award in Aging (K08AG051187) from the National Institute on Aging, American Federation for Aging Research, John A. Hartford Foundation, and Atlantic Philanthropies.
DK has received funding for this research by the Paul B. Beeson Clinical Scientist Development Award in Aging (K08AG051187) from the National Institute on Aging, American Federation for Aging Research, John A. Hartford Foundation, and Atlantic Philanthropies.
REFERENCES
- 1.American Geriatrics Society Expert Panel on the Care of Older Adults with M. Patient-centered care for older adults with multiple chronic conditions: a stepwise approach from the American Geriatrics Society: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc 2012;60(10):1957–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Groff AC, Colla CH, Lee TH. Days Spent at Home-A Patient-Centered Goal and Outcome. N Engl J Med 2016;375(17):1610–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ariti CA, Cleland JG, Pocock SJ, et al. Days alive and out of hospital and the patient journey in patients with heart failure: Insights from the candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) program. Am Heart J 2011;162(5):900–906. [DOI] [PubMed] [Google Scholar]
- 4.Greene SJ, O’Brien EC, Mentz RJ, et al. Home-Time After Discharge Among Patients Hospitalized With Heart Failure. J Am Coll Cardiol 2018;71(23):2643–2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wasywich CA, Gamble GD, Whalley GA, Doughty RN. Understanding changing patterns of survival and hospitalization for heart failure over two decades in New Zealand: utility of ‘days alive and out of hospital’ from epidemiological data. Eur J Heart Fail 2010;12(5):462–468. [DOI] [PubMed] [Google Scholar]
- 6.Fonarow GC, Liang L, Thomas L, et al. Assessment of Home-Time After Acute Ischemic Stroke in Medicare Beneficiaries. Stroke 2016;47(3):836–842. [DOI] [PubMed] [Google Scholar]
- 7.O’Brien EC, Xian Y, Xu H, et al. Hospital Variation in Home-Time After Acute Ischemic Stroke: Insights From the PROSPER Study (Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research). Stroke 2016;47(10):2627–2633. [DOI] [PubMed] [Google Scholar]
- 8.Yu AYX, Rogers E, Wang M, et al. Population-based study of home-time by stroke type and correlation with modified Rankin score. Neurology 2017;89(19):1970–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Brien EC, Greiner MA, Xian Y, et al. Clinical Effectiveness of Statin Therapy After Ischemic Stroke: Primary Results From the Statin Therapeutic Area of the Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) Study. Circulation 2015;132(15):1404–1413. [DOI] [PubMed] [Google Scholar]
- 10.Xian Y, Wu J, O’Brien EC, et al. Real world effectiveness of warfarin among ischemic stroke patients with atrial fibrillation: observational analysis from Patient-Centered Research into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) study. BMJ 2015;351:h3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra NK, Shuaib A, Lyden P, et al. Home time is extended in patients with ischemic stroke who receive thrombolytic therapy: a validation study of home time as an outcome measure. Stroke 2011;42(4):1046–1050. [DOI] [PubMed] [Google Scholar]
- 12.Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Financ Rev 1994;15(4):153–163. [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Medicare & Medicaid Services. Medicare Current Beneficiary Survey (online) Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/index.html Accessed September 5, 2018.
- 14.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials 1989;10(4):407–415. [DOI] [PubMed] [Google Scholar]
- 15.Anker SD, McMurray JJ. Time to move on from ‘time-to-first’: should all events be included in the analysis of clinical trials? Eur Heart J 2012;33(22):2764–2765. [DOI] [PubMed] [Google Scholar]
- 16.Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol 2009;170(2):244–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uno H, Claggett B, Tian L, et al. Adding A New Analytical Procedure With Clinical Interpretation in the Tool Box of Survival Analysis. Ann Oncol 2018. [DOI] [PMC free article] [PubMed]
- 18.Zipkin DA, Umscheid CA, Keating NL, et al. Evidence-based risk communication: a systematic review. Ann Intern Med 2014;161(4):270–280. [DOI] [PubMed] [Google Scholar]
- 19.Fowler E, MacRae S, Stern A, et al. The built environment as a component of quality care: understanding and including the patient’s perspective. Jt Comm J Qual Improv 1999;25(7):352–362. [DOI] [PubMed] [Google Scholar]
- 20.Hack TF, McClement SE, Chochinov HM, et al. Assessing Symptoms, Concerns, and Quality of Life in Noncancer Patients at End of Life: How Concordant Are Patients and Family Proxy Members? J Pain Symptom Manage 2018. [DOI] [PubMed]