Abstract
Objectives:
Biopsychosocial models emphasize the influence of parent/family factors on pediatric chronic pain. Little is known about how parent factors differ across the acute to chronic pain continuum, or contribute to youths’ pain experience in the acute pain period. The purpose of the study was to describe parent factors in youth with acute musculoskeletal pain (n=84) compared to youth with chronic pain (n=60) and youth without pain (n=61). Further, within the acute pain sample, we tested parent factors as predictors of child pain characteristics, as well as the moderating role of child sex on associations.
Methods:
Participants were 205 youth (ages 10–17) and one biological parent. Children reported on their own pain and activity limitations. Parents reported on their own chronic pain, somatization, and protective pain responses.
Results:
Parents of youth with acute pain had higher prevalence of chronic pain and greater somatization than parents of youth without pain. Parents of youth with acute and chronic pain did not differ. Linear regressions within the acute pain sample revealed presence of parent chronic pain and protective behavior were associated with child pain. Moreover, parent somatization was associated with child activity limitations. Within the acute pain sample, associations between parent protectiveness and child pain were moderated by child sex, with relationships stronger for female children.
Discussion:
Findings highlight the importance of parent factors on pain experiences of youth with acute musculoskeletal pain. Future longitudinal research can elucidate temporal associations that underlie how parent factors may impact transition from acute to chronic pain.
Keywords: Acute pain, child, adolescents, parent, risk factors
Introduction
Musculoskeletal (MSK) pain (pain in muscles, bones, ligaments, tendons, joints, and nerves) is a common presenting complaint for youth seeking medical care during childhood and adolescence [1, 2]. Between 8% and 32% of youth report weekly MSK pain and up to 39% experience monthly MSK pain [41]. For many youth, MSK pain resolves during a relatively brief period; however, for a subsample, pain persists beyond the expected course of healing, and even into early adulthood [3, 4]. Individual risk factors for onset of MSK pain (e.g., health-related factors, sociodemographic characteristics) and prognostic factors for pain persistence (e.g., negative emotional states) have been identified [5]. However, little is known about factors that contribute to youths’ acute MSK pain experience.
Most of the research on biopsychosocial factors impacting children’s pain experience has been performed in samples where pain has persisted over time. For example, recent models of parent and family factors in pediatric chronic pain and associated disability emphasize the influence of social learning processes on youths’ chronic pain experience [6–8]. Specifically, individual parent factors including parent chronic pain history, psychological distress, and protective responses to their child’s pain have been found to be associated with increased pain-related disability in youth [6, 9]. These factors are thought to impact children’s experiences through modeling and reinforcement of pain distress. Indeed, a recent meta-analysis of population-based studies indicated increased risk for pain among offspring of parents with chronic pain [9]. Further, parent somatization and catastrophizing about their own pain has been associated with parenting behaviors in response to their child’s pain and encouraging children’s illness behavior [10–12]. Parent protective responses to children’s pain may include providing excessive attention to pain, giving special privileges, and permitting activity avoidance. In youth with chronic pain, higher parent protectiveness is associated with increased child functional disability and somatic symptoms [10, 13, 14]. Similarly, higher parent somatic complaints are associated with greater child somatic complaints [15, 16].
Studies examining parent responses to youth experiencing acute pain have largely been conducted through experimental pain laboratory tasks (e.g., cold pressor task). In one study of youth with and without chronic pain undergoing a painful lab task, findings revealed that for both groups, higher parent catastrophizing about their child’s pain was associated with an increased tendency to want to stop their child’s participation in the pain-inducing activity [12]. Additional laboratory studies have found that children report greater pain intensity and pain-related fear when provided increased reassurance, apologies, and empathy from parents during needle procedures or laboratory pain tasks [17, 18]. Taken together, these data suggest the potential transmission of threat from the parent to child through protective parenting behaviors. Furthermore, directly relevant to clinical acute pain samples, a small body of literature examining acute postsurgical pain in children suggests that parent factors may serve as risk factors for poor pain-related outcomes following pediatric surgery [19–22]. Specifically, greater parent catastrophizing about their child’s pain predicted greater pain intensity among children 2 weeks post-surgery and 12 months later [19, 21].
Research in healthy children and chronic pain samples suggests that parent influences on the child’s pain experience may differ by child sex, with the strongest associations being for female children [17, 23–25]. For example, parental response to pain and parental anxiety sensitivity were related to girls’ pain intensity in the setting of a laboratory pain task; this association was not apparent for boys [17, 24]. Youth sex has also been identified as a moderator of parent behaviors and children’s pain experiences among youth with chronic pain. In youth with functional abdominal pain, parent attention had a stronger effect on gastrointestinal symptoms in girls than boys [25]. Additionally, protective parenting behaviors mediated the relationship between maternal anxiety and children’s pain sensitivity in a laboratory task for girls with chronic pain, but not for boys [23].
The impact of parent and family influences on pediatric chronic pain is well-established [42] but examination of these influences in pediatric acute pain populations is nascent and thus the primary focus of the current study. To fill this gap, the current study compared rates of parent chronic pain, somatization, and protective parenting behaviors in youth with acute pain to parents of youth with chronic MSK pain and parents of youth without pain. We hypothesized that parents of youth with acute and chronic MSK pain would have elevated rates of parent chronic pain, somatic complaints, and protective behavior, compared to parents of youth without pain. Next, to fill the gap in knowledge of youth with acute clinical pain, we tested associations between parent factors and youths’ pain intensity and activity limitations in the acute pain sample, as well as the moderating role of child sex on these associations. This moderation model was selected given data within chronic pain samples suggesting differing effects of parent protective behaviors on female versus male children. We hypothesized that the presence of parent chronic pain, higher parent somatic symptoms, and greater protective parenting behaviors would be associated with greater pain and activity limitations in youth with acute MSK pain. Based on prior literature, we also hypothesized that associations between parent factors and child symptoms would differ by child sex such that greater parent protective behaviors would be associated with greater child pain intensity and activity limitations due to pain for girls, but not for boys.
Methods
The current study was conducted at an academic medical center in the northwestern United States. Study procedures were approved by the Institutional Review Board, and all participants provided consent or assent prior to undergoing any study procedures. Participants were 205 dyads (youth ages 10–17 and a participating biological parent) taking part in a larger longitudinal study. Of these participants, 84 youth had acute MSK pain (<1 month duration), 60 youth had chronic MSK pain, and 61 youth were without pain. Previous manuscripts have reported pain characteristics, psychological functioning, and sleep characteristics in this sample, highlighting daily sleep-pain associations and contributions of conditioned pain modulation to pain outcomes [26–28]. This is the first paper to examine associations among parent factors and child symptoms.
Youth with acute pain were recruited from the emergency department (n = 45) or orthopedic clinic (n = 39) following evaluation of a new MSK pain complaint. Inclusion criteria included the presence of MSK pain for less than one month at time of enrollment. Youth with acute pain were excluded if they had another current chronic pain condition (e.g., chronic headaches, recurrent abdominal pain), if serious pathology (e.g., infection, cancer) was associated with the source of the pain, or if they underwent a surgical procedure or had a previous injury (e.g., broken bone) at the pain site. Participants with chronic MSK pain were recruited following an initial evaluation for MSK pain in a specialty pediatric pain clinic. Inclusion criteria included a diagnosis of chronic MSK pain in the limb(s), back, or neck with pain present for 3 months or longer, pain occurring at least weekly, and pain-related functional disability. Youth with chronic pain were excluded if their MSK pain was associated with a serious pathology (e.g., cancer, inflammatory arthritis). Youth without pain were recruited via community advertisements and well-child visits to primary care practices. Inclusion criteria for youth without pain were no history of chronic pain and no recurrent pain complaints (e.g., headaches, abdominal pain). Participants in all groups (youth and their parent) were required to be able to independently complete written questionnaires and be proficient in English to participate. Inclusion criteria for all parents were that they were a biological parent (either mother or father).
Procedure
Potentially eligible participants with acute or chronic MSK pain were identified from clinic schedules or in person at the emergency department (acute pain sample only) where youth were seeking evaluation for pain. Families were then contacted via phone, invited to participate in the research study, and were screened for eligibility. Eligible youth and their parents participated in an in-person study visit during which they completed questionnaire measures. Youth completed questionnaires on pain characteristics, and parents completed sociodemographic information and reported on their own pain history, somatic symptoms, and responses to their child’s pain. Parents and their children completed questionnaires in separate rooms to ensure privacy of responses. Families were compensated with gift cards for study completion. Reimbursement for parking costs and/or bus passes was also provided to limit potential financial barriers to participation. Recruitment and data collection occurred from 9/2012 – 4/2016.
Questionnaire Measures
Sociodemographics
Parents reported on their child’s age, sex, race, and ethnicity. Parents also reported on their relationship to their child (e.g., biological mother), parent race and ethnicity, parent education, and household income.
Child pain characteristics
Pain characteristics were assessed using a self-report of pain intensity, pain frequency, primary pain location, and presence of a fracture. Youth reported their “usual pain intensity” over the past week using an 11-point Numerical Rating Scale (0 = “no pain” to 10 = “worst pain ever”) [29, 30]. Youth also reported pain frequency over the past week using an ordinal scale of 0–4 (0 = “not at all” to 4 = “daily”).
Child activity limitations
The Child Activity Limitations Interview (CALI-21) was used to assess child activity limitations due to pain [31]. This 21-item self-report questionnaire asked youth to rate “how difficult or bothersome” it was to do activities because of pain over the past 7 days. Items were rated on a five-point Likert scale (0 = “not difficult” to 4 = “extremely difficult”). A total score was calculated by summing ratings for all 21 items (range from 0 – 84), with higher scores indicating greater pain-related disability or activity limitations due to pain. The CALI-21 child version has demonstrated reliability and validity in assessing pain-related disability in school-aged children and adolescents [31]. In the current study, Cronbach’s alpha was α =.72.
Parent chronic pain
Chronic pain in parents was measured using a single self-report item in which parents were asked to report on the presence or absence (yes or no) of current chronic pain, specified as a “current pain problem present for the last 3 months or greater”.
Parent somatization
Parent somatization was measured using the somatization subscale of the Brief Symptom Inventory-18 (BSI-18) [32]. The 6-item subscale assesses somatic symptoms (e.g., feeling weak, trouble getting breath) using probes asking how “distressed or bothered” the parent was by these symptoms in the past 7 days. Items were rated on a 5-point Likert scale (0 = “not at all” to 4 = “extremely”). The BSI-18 has demonstrated adequate reliability and convergent validity with the longer version of the BSI and other related measures [32, 33]. Previous studies have also demonstrated adequate psychometric properites for the somatization subscale, specifically [32]. In the current study, Cronbach’s alpha was α =.71.
Parent protective response to pain
Parent protective behaviors were measured using the protect subscale from the 4-factor model of the Adult Responses to Children’s Symptoms (ARCS) [34, 35]. The 13-item subscale assesses protective parenting behavior in response to their child’s pain. For example, items address how often parents “bring your child special treats or little gifts,” “let your child stay home from school,” and “give your child special privileges.” Responses are rated on a 5-point Likert scale (0 = “never” to 4 = “always”). The protect subscale score was computed by calculating the mean ratings for all items with higher values indicative of greater protective behavior. Previous research validating this measure has found the protect subscale to be associated with pain and pain-related disability in pediatric pain samples [36]. In the current study, Cronbach’s alpha was α =.88.
Data Analysis
Data were analyzed using SPSS version 22.0. Sociodemographic variables were described using means and standard deviations for continuous data and proportions for categorical data. Group differences in parent factors (current chronic pain status, somatization, and protective behaviors) by child pain group (acute, chronic, without pain) were examined using chi-square and ANOVA with pairwise deletion of missing variables. In the acute pain group only, associations between parent factors and child pain characteristics were examined using two hierarchical linear regression models—one predicting child pain intensity, and the other predicting child activity limitations due to pain. Listwise exclusion of cases (n = 2) with missing variables was used for regression analyses. Predictors included parent current chronic pain status (yes/no), parent somatization, and parent protective responses to pain. Both models controlled for child sex, child age, child fracture status (yes/no) and parent’s relationship to the child (mother versus father). To examine our final aim, two additional regression models tested child sex as a moderator of the association between parent protective behaviors and both child pain intensity and activity limitations in exclusively the acute pain sample.
Results
Descriptive data.
A total of 205 children participated in the study (84 acute pain, 60 chronic pain, and 61 without pain) with their parents. Demographic characteristics of each group are presented in Table 1. Across groups, parent participants were mostly biological mothers, college educated, non-Hispanic/Latino, and identified as White, and child participants were mostly female, non-Hispanic/Latino, and identified as White. Groups differed on child age, child sex, child and parent race, parent education, and household income. Specifically, the chronic pain group was comprised of more girls and youth were older than the other two cohorts. The acute pain group was comprised of more nonwhite parents and children compared to the other two cohorts. Parents of children without pain had higher education attainment and higher household income than the other two cohorts.
Table 1.
Sociodemographic characteristics and parent pain-related factors by child pain group.
| Acute Pain (n =84) |
Chronic Pain (n = 60) |
Without Pain (n = 61) |
p | ||
|---|---|---|---|---|---|
| Child demographics | |||||
| Child age, M (SD) | 13.84(1.94) | 14.58(2.19) | 13.64(2.07) | .03 | |
| Child sex, n(%) | .01 | ||||
| Female | 51(61%) | 51(85%) | 40(66%) | ||
| Male | 33(39%) | 9(15%) | 21(34%) | ||
| Child ethnicity, n(%) | .05 | ||||
| Hispanic/Latino | 15(18%) | 6(10%) | 4(7%) | ||
| Non-Hispanic | 61(73%) | 52(87%) | 56(92%) | ||
| Not reported | 8(9%) | 2(3%) | 1(2%) | ||
| Child race, n(%) | <.01 | ||||
| White | 45(53%) | 46(77%) | 49(80%) | ||
| Non-White | 38(45%) | 14(23%) | 12(20%) | ||
| Not reported | 1(1%) | 0(0%) | 0(0%) | ||
| Parent sociodemographics | |||||
| Relationship, n(%) | .29 | ||||
| Biological mother | 77(92%) | 51(85%) | 51(84%) | ||
| Biological father | 7(8%) | 9(15%) | 10(16%) | ||
| Parent ethnicity, n(%) | .10 | ||||
| Hispanic/Latino | 12(14%) | 4(7%) | 4(7%) | ||
| Non-Hispanic | 66(79%) | 54(90%) | 57(93%) | ||
| Not reported | 6(7%) | 2(3%) | 0(0%) | ||
| Parent race, n(%) | .03 | ||||
| White | 59(70%) | 52(87%) | 52(85%) | ||
| Non-White | 25(30%) | 8(13%) | 9(15%) | ||
| Parent education, n(%) | <01 | ||||
| High school or less | 6(7%) | 8(13%) | 1(2%) | ||
| Vocational school/some college | 25(30%) | 23(38%) | 9(15%) | ||
| College/advanced degree | 53(63%) | 29(48%) | 51(85%) | ||
| Household income, n(%) | <.01 | ||||
| <$29,999 | 15(18%) | 14(23%) | 2(3%) | ||
| $30,000 to 69,999 | 23(27%) | 19(32%) | 10(16%) | ||
| >$70,000 | 44(52%) | 26(43%) | 48(79%) | ||
| Not reported | 2(2%) | 1(2%) | 1(2%) | ||
Among the acute pain sample, primary pain locations were leg/foot (52%, n = 44), arm/hand (25%, n = 21), and back/spine (11%, n = 9) pain. Approximately one-third of children sustained a fracture (31%, n = 26). Sports injuries were reported to be the primary etiology of pain complaints, followed by non-sports accidents and spontaneous onset/no identified cause. Among youth with chronic pain, primary pain locations were back/spine (28%, n = 17), leg/foot (27%, n = 16), and arm/hand (10%, n = 6) pain. Participants with acute pain did not differ by referral source (emergency department versus orthopedics clinic) on any variables of interest (sociodemographics, parent factors, pain intensity, or activity limitations).
Differences among parent factors by child pain group (acute, chronic, no pain).
Chi-square analyses revealed significant group differences on parent current chronic pain status, λ2 (2, 204) = 27.81, p < .001 such that parents of youth with acute or chronic pain had higher rates of chronic pain compared to parents of youth without pain. In particular, current chronic pain was reported by 60% of parents of youth with acute pain, 63% of parents of youth with chronic pain, and only 21% of parents of youth without pain. Furthermore, a one-way ANOVA revealed a significant difference in parent somatization by child pain status, F(2, 199) = 7.68, p = .001. Specifically, parents of youth with acute pain (M = 2.42, SD = 3.17) had significantly higher somatization than parents of youth without chronic pain (M = 0.98, SD = 1.72), p = .01. Somatization between parents of youth with acute pain and youth with chronic pain (M = 2.90, SD = 3.17) was not different, p = .59. Protective parenting behaviors did not significantly differ by group, F(2,201) = 1.17, p = .31.
Associations among parent factors and child pain intensity within the acute pain sample
Average child-reported pain intensity in the acute pain group was M = 4.79, SD = 2.16. Linear regression was used to examine parent factors (presence of current chronic pain, somatization, and protective behaviors) as predictors of child-reported pain intensity, controlling for child age, child sex, fracture status, and parent relationship to child. Results are presented in Table 2. Results revealed a significant association between parent protective behaviors and child self-report of pain intensity, β = .23, p =.04 in youth with acute pain. The association between parent current chronic pain status and child self-report of pain intensity was also significant, β = .24, p =.045. Specifically, the presence of current parental chronic pain and greater parent protective behaviors were associated with higher child-reported pain intensity. Associations between parent somatization and child pain intensity were not significant.
Table 2.
Linear regressions of parent factors associated with child pain characteristics in the acute pain sample.
| Criterion | Model | Predictors | F | Beta | β | Adj R2 | 95% CI |
|---|---|---|---|---|---|---|---|
| Pain intensity | 1 | 2.40 | .07 | ||||
| Child age | .17 | .15 | −.09, .42 | ||||
| Child sex | .77 | .17 | −.22, 1.76 | ||||
| Fracture status | −.36 | −.08 | −1.44, .73 | ||||
| Relation to child | −1.43 | −.19 | −3.24, .37 | ||||
| 2 | 2.43* | .11 | |||||
| Child age | .20 | .17 | −.05, .45 | ||||
| Child sex | .69 | .15 | −.28, 1.66 | ||||
| Fracture status | −.35 | −.08 | −1.43, .73 | ||||
| Relation to child | −1.24 | −.16 | −3.01, .53 | ||||
| Parent chronic pain | 1.06 | .24* | .03, 2.08 | ||||
| Parent somatization | −.10 | −.15 | −.26, .06 | ||||
| Protective parenting | .76 | .23* | .02, 1.51 | ||||
| Activity limitations | 1 | .17 | −.04 | ||||
| Child age | .31 | .05 | −1.09, 1.70 | ||||
| Child sex | 1.10 | .05 | −4.42, 6.61 | ||||
| Fracture status | 1.94 | .08 | −4.11, 7.99 | ||||
| Relation to child | −1.16 | −.03 | −11.25, 8.93 | ||||
| 2 | .96 | −.004 | |||||
| Child age | .33 | .06 | −1.05, 1.71 | ||||
| Child sex | .88 | .04 | −4.57, 6.32 | ||||
| Fracture status | 2.01 | .08 | −4.05, 8.07 | ||||
| Relation to child | −.55 | −.01 | −10.54, 9.44 | ||||
| Parent chronic pain | −.70 | −.03 | −6.42, 5.01 | ||||
| Parent somatization | 1.02 | .28* | .15, 1.89 | ||||
| Protective parenting | −.02 | −.001 | −4.09, 4.06 |
p < .05
Associations among parent factors and child activity limitations within the acute pain sample
Average child-reported activity limitations in the acute pain group were M = 15.80, SD = 11.56. A linear regression model examined parent factors (current chronic pain, somatization, and protective behaviors) as predictors of child-reported activity limitations due to pain, controlling for child age, child sex, fracture status, and parent relationship to child. Results revealed parent somatization was associated with child activity limitations, β = .28, p =.02. Specifically, higher parent somatization was associated with higher child-reported activity limitations. However, neither parent chronic pain status nor protective parenting behavior were associated with child activity limitations due to pain.
Child sex as a moderator of the association between parent protective behaviors and child pain intensity and activity limitations within the acute pain sample
The interaction between child sex and protective parenting on child-reported pain intensity and activity limitations due to pain was tested using two moderation models. Results revealed the interaction among parent protective behavior and child sex was significantly associated with child pain intensity, β = .84, p =.02. Specifically, protective parenting behavior had a stronger association with pain intensity for girls versus boys (see Figure 1). Child sex did not moderate associations among protective parenting and child activity limitations.
Figure 1.
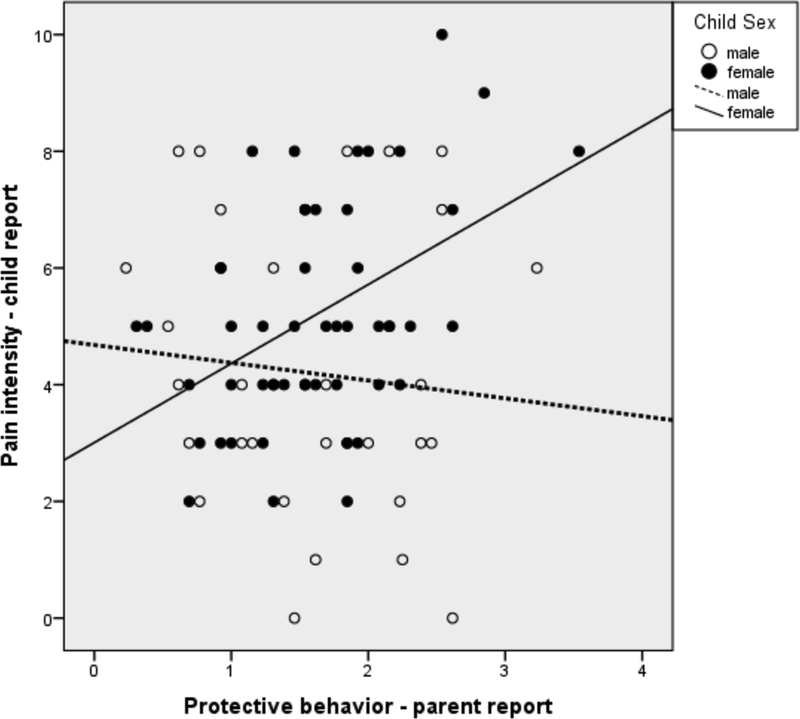
Child sex as a moderator of the association between parent protective behavior and child pain intensity in the acute pain sample.
Discussion
Minimal research has explored parent and family factors that contribute to youths’ pain experiences in the acute pain period. Recent models of pediatric chronic pain have emphasized the role of social learning processes, including influences of parent chronic pain status, somatic complaints, and parent protective behavior in response to child pain. However, the impact of parent factors on child pain intensity and activity limitations due to pain in a clinical sample of youth with acute MSK pain has received limited attention.
Findings from the current study revealed significant differences by child pain group on several parent variables. Specifically, parents of youth with acute MSK pain had higher rates of current chronic pain and somatic symptoms than parents of youth without pain. Parent factors were similar among parents of youth with acute and chronic MSK pain. These findings are novel in that they are the first to describe parent factors frequently observed as important in chronic pain populations (i.e., parent chronic pain and somatic complaints) are also present at higher rates within an acute MSK pain sample. While data are cross-sectional and thus causation cannot be established, these data lend preliminary support for the idea that intergenerational transmission of risk for pain may be important even during the acute pain period [8]. Moreover, it is possible that parents who have pain themselves may be more likely to seek medical care for their children when they are experiencing acute pain complaints. Future research with larger samples of youth with acute MSK pain will be needed to explore the potential role that parents’ own symptoms play in their interpretation of their child’s pain experiences, and their subsequent actions related to seeking medical care.
Second, the present study examined parent factors, including current chronic pain, somatization, and protective behaviors, as predictors of child pain intensity and activity limitations within the acute pain period. The significant association between both parent chronic pain status and parent protective behavior, and child pain intensity lends further support to the role of social learning processes. Even in the acute pain period, children whose parents have chronic pain tend to report greater pain intensity. Furthermore, the association between parent protective behavior and child pain intensity is consistent with findings in both healthy and chronic pain samples [17, 23–25, 37, 38]. Taken together, these findings suggest that parental modeling of pain behaviors and potential reinforcement of pain may be associated with children’s MSK pain experience during the acute pain period. However, we would be remiss to ignore possible bidirectional associations between child and parent factors. Children with higher pain intensity may solicit more protective behaviors from their parents, particularly following an emergency department visit. Future studies will be needed to elucidate directionality among these variables.
Interestingly, in youth with acute MSK pain, only parent somatization was significantly associated with child activity limitations. Observing somatic behaviors may influence the lens through which adolescents view their own pain experience via two pathways. First, parent somatization may lead to modeling of illness behavior [39]. Second, parental modeling may impact youths’ beliefs about their ability to engage in activity when somatic symptoms are present [40]. More nuanced associations among parent modeling of pain/somatic symptoms and child activity limitations during the acute pain period may be examined in future studies. For instance, different types of activity participation (e.g., school attendance, sports participation) may be impacted differently by various parent factors. As such, this idea may explain our unexpected finding that protective parenting behavior was not significantly associated with child activity limitations. This could be related to the measure of activity limitations (CALI-21) used in the current study. This measure includes routine activities (as well as vigorous activities) some of which may have elicited fewer protective behaviors (e.g., schoolwork, eating regular meals, playing with friends) in this sample. Additional research with a larger sample size will permit examination of how individual questionnaire items may be differently associated with parent protectiveness to further explore this hypothesis.
In light of previous research yielding support for sex differences in associations between parent factors and child pain and disability in chronic pain samples and healthy youth, our final aim tested moderation models of parent protective behavior on child pain intensity and activity limitations between boys and girls. Child sex moderated the relationship between parent protective behavior and pain intensity, but not activity limitations. Specifically, girls in the acute pain sample reported higher pain intensity when their parent reported engaging in more protective behavior. Because girls are at increased risk for development of chronic pain compared to boys [41], this finding may have important clinical implications for screening of risk factors in females with new-onset MSK pain complaints and may be a potential behavioral target for clinical interventions.
The current findings should be interpreted in light of various limitations. First, this study used a heterogeneous sample of youth with a range of acute and chronic MSK pain complaints. Though all youth with acute pain were experiencing new-onset MSK pain and fracture status was controlled for, pain location and/or pain etiology may have impacted results. The current sample size did not permit examination of pain location on these associations. Second, this study did not examine other potentially relevant family and parent factors, such as family structure, level of family functioning, or dyadic interactions between parents and youth. When assessing how parental protectiveness affects child disability, the amount and quality of contact the child has with the parent may be informative. This study is also limited in that the data are cross-sectional and causation cannot be gleaned from results. Furthermore, our findings are subject to the inherent limitations of self-report research (e.g., response bias, introspective ability). Finally, given the limited racial/ethnic diversity in the current sample, and the inclusion of only biological parents, our findings may not necessarily reflect associations across a range of racial/ethnic groups or among non-biological parents and their children.
Future studies may explore if/how parent factors predict long-term pain outcomes and pain persistence in youth. Comparison of families recruited from non-urgent care settings (e.g., from pediatrician office visits) to those seeking urgent care (e.g., from the emergency department) for a new acute pain complaint may reveal differences in factors that predict longer- term outcomes. Relatedly, daily assessment of parent protectiveness following the initial medical visit may provide temporal information regarding change in parenting behaviors following pain onset. Finally, future studies may examine how parent factors such as protectiveness and somatization impact youths’ pain experiences across developmental periods (i.e., childhood versus adolescence).
In conclusion, the present study provides preliminary support for associations between parent factors and youths’ experience of acute MSK pain. Parents of these youth not only differed in their own pain presentation, but parent factors were also found to be significant predictors of children’s pain intensity and activity limitations due to pain. This effect appeared to be particularly significant for girls, with results indicating that parent protective behavior had a stronger impact on pain intensity for girls compared to boys. Future longitudinal research in a larger cohort is needed to provide mechanistic information to elucidate how parent factors influence child pain-related outcomes over time.
Supplementary Material
Footnotes
Conflicts of Interest and Sources of Funding: This study was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award No. K23HD071946 (PI: Amy Lewandowski Holley). Tonya M. Palermo is supported by NIH K24HD060068.
The authors declare no conflict of interest.
References
- 1.Jordan KP, Kadam UT, Hayward R, et al. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010;11:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Inocencio J Epidemiology of musculoskeletal pain in primary care. Arch Dis Child 2004;89:431–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brattberg G Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain 2004;8:187–199. [DOI] [PubMed] [Google Scholar]
- 4.Hestbaek L, Leboeuf-Yde C, Kyvik KO et al. The course of low back pain from adolescence to adulthood: eight-year follow-up of 9600 twins. Spine 2006;31:468–472. [DOI] [PubMed] [Google Scholar]
- 5.Huguet A, Tougas ME, Hayden J, et al. Systematic review with meta-analysis of childhood and adolescent risk and prognostic factors for musculoskeletal pain. Pain 2016;157:2640–2656. [DOI] [PubMed] [Google Scholar]
- 6.Palermo TM, Eccleston C. Parents of children and adolescents with chronic pain. Pain 2009;146:15–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rabbitts JA, Holley AL, Karlson CW et al. Bidirectional associations between pain and physical activity in adolescents. Clin J Pain 2014;30:251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stone AL, Wilson AC. Transmission of risk from parents with chronic pain to offspring: an integrative conceptual model. Pain 2016;157:2628–2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins KS, Birnie KA, Chambers CT, et al. Offspring of parents with chronic pain: a systematic review and meta-analysis of pain, health, psychological, and family outcomes. Pain 2015;156:2256–2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Langer SL, Romano JM, Levy RL, et al. Catastrophizing and parental response to child symptom complaints. Child Health Care 2009;38:169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Langer SL, Romano JM, Mancl L, et al. Parental catastrophizing partially mediates the association between parent-reported child pain behavior and parental protective responses. Pain Res Treat 2014;2014:751097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caes L, Vervoot T, Eccleston C, et al. Parental catastrophizing about child’s pain and its relationship with activity restriction: the mediating role of parental distress. Pain 2011;152: 212–222. [DOI] [PubMed] [Google Scholar]
- 13.Sieberg CB, Williams S, Simons LE. Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J Pediatr Psychol 2011;36:1043–1051. [DOI] [PubMed] [Google Scholar]
- 14.Simons LE, Claar RL, Logan DL. Chronic pain in adolescence: parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. J Pediatr Psychol 2008;33:894–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolff N, Darlington AS, Hunfeld J, et al. Determinants of somatic complaints in 18-month-old children: the generation R study. J Pediatr Psychol 2010;35:306–316. [DOI] [PubMed] [Google Scholar]
- 16.Craig TK, Cox AD, Klein K. Intergenerational transmission of somatization behaviour: a study of chronic somatizers and their children. Psychol Med 2002;32:805–816. [DOI] [PubMed] [Google Scholar]
- 17.Chambers CT, Craig KD, Bennett SM. The impact of maternal behavior on children’s pain experiences: an experimental analysis. J Pediatr Psychol 2002;27:293–301. [DOI] [PubMed] [Google Scholar]
- 18.Schechter NL, Zempsky WT, Cohen LL, et al. Pain reduction during pediatric immunizations: evidence-based review and recommendations. Pediatrics 2007;119:e1184–1198. [DOI] [PubMed] [Google Scholar]
- 19.Rabbitts JA, Groenewald CB, Tai GG, et al. Presurgical psychosocial predictors of acute postsurgical pain and quality of life in children undergoing major surgery. J Pain 2015;16:226–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rabbitts JA, Zhou C, Groenewald CB, et al. Trajectories of postsurgical pain in children: risk factors and impact of late pain recovery on long-term health outcomes after major surgery. Pain 2015;156:2383–2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page MG, Campbell F, Isaac L, et al. Parental risk factors for the development of pediatric acute and chronic postsurgical pain: a longitudinal study. J Pain Res 2013;6:727–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Esteve R, Marquina-Aponte V, Ramirez-Maestre C. Postoperative pain in children: association between anxiety sensitivity, pain catastrophizing, and female caregivers’ responses to children’s pain. J Pain 2014;15:157–168. [DOI] [PubMed] [Google Scholar]
- 23.Evans S, Payne LA, Seidman L, et al. Maternal anxiety and children’s laboratory pain: the mediating role of solicitousness. Children 2016;3:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsao JC, Lu Q, Myers CD, et al. Parent and child anxiety sensitivity: relationship to children’s experimental pain responsivity. J Pain 2006;7:319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walker LS, Williams SE, Smith CA, et al. Parent attention versus distraction: impact on symptom complaints by children with and without chronic functional abdominal pain. Pain 2006;122:43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lewandowski Holley A, Wilson AC, Cho E et al. Clinical phenotyping of youth with new-onset musculoskeletal pain: a controlled cohort study. Clin J Pain 2017;33:28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holley AL, Wilson AC, Palermo TM. Predictors of the transition from acute to persistent musculoskeletal pain in children and adolescents: a prospective study. Pain 2017;158:794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewandowski Holley A, Rabbitts J, Zhou C, et al. Temporal daily associations among sleep and pain in treatment-seeking youth with acute musculoskeletal pain. J Behav Med 2017;40:675–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.von Baeyer CL, Spagrud LJ, McCormick JC, et al. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain 2009;143:223–227. [DOI] [PubMed] [Google Scholar]
- 30.Castarlenas E, Jensen MP, von Baeyer CL, et al. Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents: a systematic review. Clin J Pain 2017;33:376–383. [DOI] [PubMed] [Google Scholar]
- 31.Palermo TM, Lewandowski AS, Long AC, et al. Validation of a self-report questionnaire version of the Child Activity Limitations Interview (CALI): The CALI-21. Pain 2008;139:644–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Derogatis LR. Brief Symptom Inventory (BSI)-18: Administration, scoring and procedures manual. Minneapolis: NCS Pearson, 2001. [Google Scholar]
- 33.Zabora J, BrintzenhofeSzoc K, Jacobsen P, et al. A new psychosocial screening instrument for use with cancer patients. Psychosomatics 2001;42:241–246. [DOI] [PubMed] [Google Scholar]
- 34.Van Slyke DA, Walker LS. Mothers’ responses to children’s pain. Clin J Pain 2006;22:387–391. [DOI] [PubMed] [Google Scholar]
- 35.Noel M, Palermo TM, Essner B, et al. A developmental analysis of the factorial validity of the parent-report version of the Adult Responses to Children’s Symptoms in children versus adolescents with chronic pain or pain-related chronic illness. J Pain 2015;16:31–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Claar RL, Guite JW, Kaczynski KJ, et al. Factor structure of the Adult Responses to Children’s Symptoms: validation in children and adolescents with diverse chronic pain conditions. Clin J Pain 2010;26:410–417. [DOI] [PubMed] [Google Scholar]
- 37.Connelly M, Bromberg MH, Anthony KK, et al. Use of smartphones to prospectively evaluate predictors and outcomes of caregiver responses to pain in youth with chronic disease. Pain 2017;158:629–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsao JC, Lu Q, Kim SC, et al. Relationships among anxious symptomatology, anxiety sensitivity and laboratory pain responsivity in children. Cogn Behav Ther 2006;35:207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol 1991;19:379–394. [DOI] [PubMed] [Google Scholar]
- 40.Goodman JE, McGrath PJ. Mothers’ modeling influences children’s pain during a cold pressor task. Pain 2003;104:559–565. [DOI] [PubMed] [Google Scholar]
- 41.King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 2011;152:2729–2738. [DOI] [PubMed] [Google Scholar]
- 42.Palermo TM, Valrie CR, Karlson, CW. Family and parent influences on pediatric chronic pain: a developmental perspective. American Psychologist 2014;69:142–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


