Abstract
Exposure to violence and substance abuse are salient public health concerns among Indigenous people (i.e., American Indian and Canadian First Nations). Despite this, little research has examined the association between the two among community-based reservation/reserve samples, or factors within the broader social environment that may moderate this association. As such, the purpose of the study is to examine ecological moderators of the association between direct (i.e., dating violence victimization) and indirect (i.e., current perceptions of community violence and prospective caretaker-reported victimization exposure) exposure to violence and meeting diagnostic criteria for a substance use disorder among a large longitudinal sample of Indigenous youth and their caretakers in the upper-Midwest of the United States and Canada (N = 521). Data come from the last two waves of the study, when the adolescents were between the ages of 16–19. The results show relatively high rates of direct and indirect violence exposure by late adolescence. Logistic regression models with added interaction terms were examined to test moderating effects. Per capita family income and remote location both amplified the positive association between current community violence exposure and substance use disorder risk. Family warmth and support buffered the association between caretaker victimization exposure and substance use disorder risk, whereas dating violence victimization exposure amplified this association. The findings are contextualized for Indigenous communities, and substance abuse prevention and intervention implications are discussed.
Keywords: American Indian, First Nations, Violence, Substance Abuse, Victimization
Substance abuse and violence are two leading health concerns among North American Indigenous (i.e., American Indian and Canadian First Nations) communities, and are directly and indirectly (e.g., increases fatal suicide and accident incidents) associated with the leading causes of early mortality among Indigenous adolescents (Espy et al., 2014). Indigenous youth initiate use of substances at earlier ages, progress to regular use at faster rates, and are at high risk for developing a substance use disorder (SUD) during adolescence compared to other racial/ethnic groups (Whitbeck, Sittner Hartshorn, & Walls, 2014a). Moreover, Indigenous people in the United States and Canada experience high per capita rates of direct and indirect violent victimization, particularly intimate partner violence and sexual assault (Breiding et al., 2014; Perreault, 2011). Decades of research show that exposure to violence and substance abuse are strongly related (Buka, Stichick, Birdthistle, & Earls, 2001). Despite this, there is little research examining this association among community-based samples of Indigenous youth, which undermines our ability to conceptualize, adapt, and move toward prevention and intervention.
Although exposure to violence and substance abuse are salient concerns among Indigenous communities, the association between the two is probabilistic, rather than deterministic. That is, not everyone who is exposed to some form of direct or indirect violence develop substance use problems. Instead, this association is complex and conditional upon various facets of the social environments in which people are embedded. Consequently, understanding the multilevel conditions under which violence exposure is likely to lead to substance abuse is not only important for substance use prevention and intervention efforts, but also for disrupting the multiple cascading effects caused by direct and vicarious victimization exposure (Hamby et al., 2018). To better understand this association among Indigenous youth, the purpose of the study is to examine moderators of the association between current perceptions of community violence, cumulative caretaker victimization exposure, and lifetime dating violence victimization and meeting criteria for a SUD among a large (N = 521) longitudinal study of Indigenous youth and their caretakers in the upper-Midwest of the United States and Canada.
Ecological Stress Process Model
To examine moderators of the association of violence exposure and SUD risk, the current study draws from an ecological stress process model (Foster & Brooks-Gunn, 2009; Pearlin, 1989). Direct and indirect forms of violence exposure are conceptualized as stressors that occur across levels of social ecology (e.g., community, family, and interpersonal) and may have direct or cumulative effects to produce negative health outcomes. Adolescents are also embedded in multiple ecological contexts, which likely augment how they react to experiences within their environment (Bronfenbrenner, 1979). Ecological models consider interactive effects within and across systems that influence the effects of exposure to violence. A bulk of the stress literature focuses on coping resources within family and individual contexts that buffer the effects of violence exposure on health outcomes. In addition to these coping resources, this study incorporates moderators that may amplify or exacerbate the association between stress and substance abuse (e.g., Agnew, 2006). Although stated in more detail below, risk factors and other negative experiences are hypothesized to amplify the positive association between exposure to violence and victimization and SUD risk, whereas protective factors and positive experiences are expected to buffer this association. Understanding both positive and negative moderating effects may provide a more comprehensive picture of how violence exposure influences SUD risk, which can help aid in targeting and adapting factors that could be strengthened (e.g., buffers) or reduced (e.g., amplifiers)—a key goal of prevention and intervention programming.
Exposure to Violence and Substance Use
In the first part of this review, we focus on indirect exposure to violence within community and family contexts, and direct exposure to violence within dating relationships, which are conceptualized individually as stressors and collectively as moderators of one another. Little research has examined subjective measures of community violence among rural communities in general (Lynch, 2003) and Indigenous communities specifically. Limited evidence suggests that Indigenous youth perceive their communities to be more dangerous than other racial/ethnic groups (Friese, Grube, & Seninger, 2015); however, these studies use data from national and statewide studies, which likely over represent urban Indigenous youth. Adolescents’ subjective interpretation of their environments as detrimental, as evinced by subjective interpretations of community violence, may result in enduring emotional and physiological arousal (Buka et al., 2001; Fowler et al., 2009), which may increase the odds of misusing substances to cope (Cooley-Quille et al., 2001). Indeed, a limited body of evidence among Indigenous youth suggests that neighborhood disorder, including perceptions of violence, are associated with more frequent alcohol and marijuana use (Friese et al., 2015; Nalls, Mullis, & Mullis, 2009). Hypothesis 1: Taken together, current perceptions of community violence are expected to increase the odds of a SUD.
Indigenous people in the U.S. and Canada experience high rates of violent victimization, particularly intimate partner violence and sexual assault (Breiding et al., 2014; Perreault, 2011). Moreover, Manson and colleagues (2005) found that Indigenous adults reported witnessing violence against a family member at higher rates than found in the National Comorbidity Study. Prospective studies indicate that vicarious victimization of a family member or people occupying central positions in social networks increases the odds of a later SUD (Carliner, Gary, McLaughlin, & Keyes, 2017), which may be a result of trying to cope with negative emotions and anticipatory strains (e.g., witnessing violent victimization may result in a person anticipating being victimized themselves) emanating from witnessing and/or hearing about victimization experiences of close others (Agnew, 2006). Research among Indigenous youth shows vicarious victimization exposure increases the odds of poly-drug use (Brockie et al., 2015). Studies among various Indigenous communities also suggest that childhood adversity experienced within the family, including family violence exposure, is a strong predictor of substance use in adulthood (Boyd-Ball et al., 2006). Hypothesis 2: As such, caretaker victimization exposure is expected to increase the odds of meeting criteria for a SUD.
Among Indigenous adolescent samples, lifetime estimates of dating violence victimization range from 7% to 31% (Ackard & Neumark-Sztainer, 2002; Hautala, Sittner Hartshorn, Armenta, & Whitbeck, 2017). These data sources, with the exception of Hautala and colleagues (2017), likely underestimate prevalence rates because they measured dating violence with one direct question, rather than multiple behaviorally-specific questions. Dating violence victimization has been linked with increased substance use (Haynie et al., 2013) and SUD risk (Exner-Cortens, Eckenrode, & Rothman 2013). Although no research has examined the consequences of dating violence victimization among Indigenous youth specifically, studies among Indigenous youth and young adults show that direct violent victimization increases the odds risky substance use behavior (Brockie et al. 2015). Hypothesis 3: Consequently, dating violence victimization is expected to increase the odds of meeting criteria for a SUD.
The three types of violence exposure indicators appear to be prevalent among Indigenous youth and exist at the community, family, and interpersonal levels of social ecology. In light of high rates of violence exposure among Indigenous people, understanding how multiple forms of violence interact to influence salient health outcomes is paramount to developing comprehensive prevention and intervention programming. Social stress theories argue that exposure to multiple forms of stress are especially deleterious to health (Lloyd & Turner, 2008). There is also a growing body of evidence which indicates that poly-victimization, defined as exposure to multiple forms of victimization in multiple contexts, has a more adverse effect on health than exposure to one form of victimization or violence exposure within one context (Hamby et al., 2018). A complementary area of research focuses on a “double whammy” phenomenon (Hughes, Parkinson, & Vargo, 1989), in which the effects of youths’ exposure to direct forms of violent victimization are greater when they experience vicarious (indirect) forms of violence and victimization as well. Recent evidence suggests that multiple forms of violence exposure have a greater effect on general substance use and SUD risk than single forms or no victimization exposure (Wright, Fagan, & Pinchevsky, 2013). Hypothesis 4: Taken together, the hypothesized positive association between each violence exposure indicator and SUD risk is expected to be stronger in the presence of additional forms violence exposure.
Moderators of Exposure to Violence and Victimization Community Moderators
Exposure to various forms of violence may be considered as stressors that have both direct and interactive effects with one another on SUD risk. In this section, we review possible moderators across ecological contexts that may condition the association between violence and victimization exposure and SUD risk. Community violence, and violence exposure in general, within rural communities has received little empirical attention for youth. Moreover, gradations of rurality have yet to be explored in any detail, which may be relevant for understanding how and when exposure to violence is associated with substance abuse. The rural context and dense social ties of many reservations/reserves (Whitbeck et al., 2014a) may make violence exposure particularly relevant because crime and victimization incidents are likely widely known by others and its effects likely spread beyond the individuals who directly experience violent victimization. Although all of the participating communities in the current study are rural, several are considered “remote,” meaning they are not accessible by road at all times of the year, and are a prohibitive distance from larger population centers. As a result, this argument may be more salient for youth residing in these communities. Hypothesis 5: Consequently, we expect the association between violence exposure and SUD to be stronger for those living in a remote community, compared to those living in rural, non-remote communities.
Family Moderators
Extended familial contexts are central to Indigenous adolescent development and a key source of resilience (Whitbeck et al., 2014a). Social stress theories emphasize the role of warm and supportive relations among family members as a buffer against stressors such as violence and victimization exposure (Pearlin, 1989). Prior research among non-Indigenous samples indicate that family support buffers the association between exposure to violence and victimization within community (Ozer, Lavi, Douglas, & Wolf, 2017), family (Tajima, Herrenkohl, Moylan, & Derr, 2011), and dating relationships (Holt & Espelage, 2005) on multiple health outcomes. Hypothesis 6: As such, the positive association between violence exposure and SUD is expected to decrease in magnitude for those with high levels of family warmth and support.
In addition to family processes, sociodemographic characteristics of the family may also moderate the association between violence exposure and substance abuse risk. Limited evidence suggests that family financial strain and poverty are modest risk factors for Indigenous adolescent substance abuse (Whitbeck et al., 2014a). Drawing from previous arguments, exposure to multiple sources of stress (e.g., low income and exposure to violence) have a more adverse effect on health than exposure to single forms or no stress (Lloyd & Turner, 2008). Conversely, a modest body of evidence suggests that high income has a protective effect and may buffer the effects of some forms of adversity on negative health outcomes (Schieman, Pearlin, & Meersman, 2006). Hypothesis 7: Consequently, the effect of violence exposure on SUD risk is expected to be greater at low levels of family income.
Peer Moderators
Peers have a strong influence on adolescent development and risk behavior. The rural and cultural context of reservations/reserves shapes the size, composition, and duration of peer networks such that youth grow up with small, enduring, tight-knit peer groups (Whitbeck et al., 2014a). As a result, risky peer groups likely have a strong, less malleable influence on risk behaviors such as substance use. Social stress theories indicate that prosocial relationships may buffer the association between exposure to stress and health (Pearlin, 1989). Delinquent peer associations, however, may be conceptually distinct from prosocial peer relations, rather than the opposite end of a single continuum. Conversely, delinquent peer groups are expected to amplify the effect of stressors such as violence and victimization on health because peers may promote substance use as a way of coping with stress (Agnew, 2006). Although there is mixed support for this moderating effect, prior research shows that delinquent peer associations amplify the effect of violence exposure on externalizing behavior (Buka et al., 2001). Hypothesis 8: As such, the association between exposure to violence and SUD risk is expected to be stronger at high levels of delinquent peer associations compared to low levels.
Individual Moderators
Two individual-level factors may be important moderators of the association between violence exposure and SUD risk. Emotional well-being shapes how adolescents respond to stressors in their environment (Agnew, 2006). For example, adolescents high in depressive symptoms may be irritable and withdrawn, which promote feelings of hopelessness and nothing to lose attitudes (Armenta et al., 2014). Moreover, those high in internalizing symptoms may be more prone to manifest stressful experiences in the form of inward directed outcomes (i.e., substance use), rather than outward directed outcomes (e.g., aggression). Hypothesis 9: As a result, depressive symptoms are expected to amplify the positive association between exposure to violence and SUD risk.
In addition, the effect of violence exposure on adverse outcomes may vary by gender. Although males are exposed to violence at greater rates, females appear to be more adversely affected by violence and victimization exposure (Buka et al., 2001). Despite this, the moderating effect of gender in the extant literature is inconsistent, with some research finding no gender effect, and some suggesting that type of violence exposure matters more or less by gender (Lynch, 2003). Hypothesis 10: As such, exposure to violence is expected to have a stronger effect on SUD risk for females compared to males.
Method
Sample
The data for the current study come from a collaborative longitudinal study of Indigenous youth and their caretakers from seven U.S. reservation and Canadian First Nations reserve communities (see also Whitbeck et al., 2014a). Although participants were sampled from different communities, all participants are part of the same cultural group and share a common cultural tradition and language. As part of confidentiality agreements with each community, the names of the cultural group and the specific reservations and reserves are not identified, nor are there any attempts to make comparisons across locations. Prior to the start of the project, permission to conduct research at each location was obtained through tribal resolutions. In each community, tribal council-appointed advisory boards were responsible for handling personnel issues and advising the research teams on all aspects of the project. All participating staff were approved by the advisory boards and were either enrolled tribal members or spouses of enrollees. Interviewers for this project were trained annually concerning methodological guidelines of in-person interviews and all were certified for work with human subjects.
At the beginning of the study, each community provided a list of families of tribally-enrolled children ages 10–12 years who lived on or within 50 miles of the reservation/reserve. All families with an eligible child were contacted to participate in the study, at which point the interviewer presented the family with a traditional gift, an overview of the project, and an invitation to participate. The response rate for the first wave of the study was 79.1%. For families who agreed to participate, both the target child and at least one adult caretaker were given $20 upon completion of the interviews. Families were interviewed once per year for eight years starting in 2002 and ending in 2011. Recruitment and incentive procedures were approved by the community advisory boards and the University of Nebraska institutional review board.
The data for the current study were drawn primarily from the last two years of the study (Waves 7 and 8), when the youth were between the ages of 16–19. The focus on late adolescence was chosen for practical and empirical reasons. The measure of dating violence victimization was first assessed in the seventh wave of the study and community violence exposure was only assessed in Wave 8. In addition, research shows a “sleeper effect” of family and community violence exposure on adolescent outcomes that becomes more salient in late adolescence/early adulthood (Fowler et al., 2009). One variable, caretaker victimization exposure, is a cumulative measure drawn from Waves 2, 3, 5, and 7 (see below). A total of 606 participants completed Wave 7 and/or Wave 8 (89.6% of the original Wave 1 sample). A total of 174 respondents (28.7%) were missing data on at least one of the measures included in the analyses. Multiple imputation by chained equations (White, Royston, & Wood, 2011) was used in Stata Version 13 (StataCorp, 2013) to account for missing data (logistic regression specification for binary variables and linear regression for continuous variables). Analyses were based on 50 imputed datasets and pooled regression estimates and standard errors using Rubin’s rules. Although the dependent variable was used in the imputation equation, cases with missing data on the dependent variable (n = 83) were excluded from the imputation-based analyses (see von Hippel 2007) for a final analytic sample of 521 participants.
Measures
Substance use disorders.
Past year SUD were assessed at Wave 8 with the Diagnostic Interview Schedule for Children (DISC-IV; Shaffer et al., 2000). The DISC-IV is an interviewer-administered instrument that does not require formal clinical training. Standardized scoring algorithms were used to obtain diagnoses of nicotine dependence, alcohol abuse and dependence, marijuana abuse and dependence, and other substance abuse and dependence based on the criteria outlined in the Diagnostic and Statistical Manual for Mental Disorders (4th ed., text rev; DSM-IV-TR; American Psychiatric Association 2000). In accordance with recent iterations of the DSM (American Psychiatric Association, 2013), both abuse and dependence criteria were combined. Participants who met past year criteria for a SUD were coded as one and those who did not were coded as zero. In order of frequency, the most common past year SUDs were for alcohol abuse/dependence, marijuana abuse/dependence, nicotine dependence, and other drug abuse/dependence (see Whitbeck et al. [2014b] for specific past year prevalence rates). A control for lifetime SUD at Wave 6 was also included using the same measurement instrument (diagnostic data not collected at Wave 7).
Perceived community violence.
Current perceptions of community violence were assessed with 10 items measured at Wave 8 of the study. Respondents were asked how often in the past 12 months there was violence in their community (i.e., a fight in which a weapon was used, violence between neighbors, gang fights, sexual assault or rape, robbery, mugging or physical assault, murder, harassment, threats, and vandalism). Response options ranged from (0) never to (2) often. The items were summed to create a scale of community violence exposure (α = .89).
Caretaker victimization exposure.
At Waves 2, 3, 5, and 7, caretakers were asked whether or not (0 = no; 1 = yes) in the past 12 months they were robbed or burglarized, had something valuable lost or stolen, were physically attacked or assaulted, were threatened with a weapon, and whether anyone was violent toward another family member. At each wave, the yes responses were summed to create an index of caretaker victimization exposure. To account for accumulation of experiences across time and to differentiate between intermittent and persistent victimization exposure (Foster & Brooks-Gunn, 2009), each index was summed to create a cumulative victimization scale at Wave 7. For a small subset of adolescents with two caretakers who participated in the study, the caretaker with the highest score was used. Preliminary analyses showed a non-linear association between caretaker victimization and adolescent SUD risk such that the odds of meeting criteria for a SUD was most pronounced at moderate-high levels of caretaker victimization compared to lower levels. Because a third of the caretakers reported no victimization during the period under examination, the continuous measure was split into three dummy variables (tertile split) to create no victimization exposure (32.0%), moderate victimization exposure (37.0%), and high victimization exposure categories (31.0%). No victimization served as the reference group.
Dating violence victimization.
Lifetime experiences of dating violence victimization were assessed at Wave 7 using 12 adapted items from the Safe Dates Physical Violence scales, which were designed for use with adolescents (Foshee, 1996). Respondents were asked in self-reported questionnaires whether a person they have been on a date with had ever used physical violence against them (i.e., slapped; physically twisted arm; slammed or held against a wall; kicked, choked, pushed, grabbed, or shoved; threw something; burned; hit with a fist; hit with hard object; beat up; assaulted with gun or knife). Respondents were asked only to report experiences that their dating partner initiated and were not done to the respondent in self-defense. Response options ranged from (0) never to (3) five or more times. The 12 items were summed together to create an overall dating violence victimization frequency score (α = .90). To account for the heavy positive skew and aid in interpretation, the victimization scale was dichotomized (0 = no dating violence victimization; 1 = any lifetime dating violence victimization).
Family warmth and support.
A measure of family warmth and support was created at Wave 7 using items adapted from the original Iowa Youth and Families Study (Conger & Elder, 1994). Adolescents were asked how often someone in their family provided warmth and support, which included items such as having someone to talk to, being part of family decisions, and getting praise for positive behavior. Response options ranged from (0) never to (2) always. Items were summed to create a scale of family warmth and support (α = .78)
Delinquent peer associations.
Delinquent peer associations were measured at Wave 7 by asking participants to indicate how many of their three best friends they believe smoke cigarettes, drink alcohol, have gotten into trouble at school, have gotten into trouble with the police, and are sexually active. Responses options ranged from (0) none to (3) three. Composite scale scores were computed by averaging across the items (α = .80).
Depressive symptoms.
A 19-item version of the Centers for Epidemiological Studies Depression scale (CES-D; Radloff, 1977) was used at Wave 7 to assess depressive symptoms. Prior analyses (Armenta et al., 2014) using this dataset indicated that one item was not psychometrically associated with the underlying depressive symptoms construct (you felt everything you did was an effort), and was dropped from the scale. Respondents were asked how often in the past week they experienced various symptoms of depression. Positively worded items were reversed coded such that higher values on each item were associated with more frequent depressive symptoms (0 = never to 3 = 5–7 days). The 19 items were summed to create a scale of depressive symptoms (α = .86).
Demographic variables.
Four demographic variables were included as statistical controls and possible moderators of the association between violence exposure and SUD risk. Remote location (0 = non-remote; 1 =remote), defined as locations that are not fully accessible by road at all times of the year and a prohibitive distance from a larger community (community-level moderator), per capita family income (per $1,000—continuous family-level moderator), gender (male = 0; female = 1), and age (continuous) were included (individual-level moderators). Because each of these variables either changed at a constant rate (i.e., age), remained the same (i.e., gender and remote location), or showed little within and/or between person change across the study (i.e., per capita family income), we used Wave 1 demographic information.
Analytic Strategy
A correlations matrix of all variables included in the analyses, with estimates combined across 50 imputed datasets, was included to examine bivariate associations among the independent variables. In addition, imputed means for continuous predictor variables and proportions for categorical predictors were assessed across Wave 8 SUD status. Multivariate logistic regression models were estimated to examine moderating effects between violence/victimization exposure and SUD risk. In Model 1, all variables were included in the analysis. A total of 28 interaction terms were tested by multiplying each of the violence/victimization exposure measures together and with all of the other variables in the model. Within each imputed dataset, interaction terms were created and results were based on pooled estimates (passive method). Each interaction was tested separately (see Models 2–5 for significant interactions), and significant interactions were probed using the mimrgns add-on in Stata (Klein, 2014) to estimate marginal effects and predicted probabilities with imputed data.
Results
The bottom of Table 1 presents the descriptive statistics for all variables included in the analyses. The sample was evenly split by gender (female = 51%) and approximately one in ten adolescents reside in a remote community. Most notably, one-quarter (26.0%) of the youth met criteria for a past year SUD at the last wave of the study, and on average, respondents reported perceiving 5.92 (out of 10 possible) forms of violence in their communities in the past year. Just over two-thirds (68%) of respondents had a caretaker who experienced some form of victimization during the study, and approximately one-third (31%) experienced physical dating violence victimization by Wave 7.
Table 1.
Descriptive Statistics and Correlations Matrix (N = 521)a
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Past Year SUD(W8) | 1.00 | ||||||||||||
| 2. Lifetime SUD (W6) | .32* | 1.00 | |||||||||||
| 3. Community Violence Exposure | .23* | .14* | 1.00 | ||||||||||
| 4. Moderate Caretaker Vic. Exposure | .01 | .07 | .06 | 1.00 | |||||||||
| 5. High. Caretaker Vic. Exposure | .13* | .11* | .08 | −.55 | 1.00 | ||||||||
| 6. Dating Violence Victimization | .22* | .24* | .12* | .06 | .09* | 1.00 | |||||||
| 7. Family Warmth and Support | −.15* | −.07 | −.06 | −.02 | −.02 | −.11* | 1.00 | ||||||
| 8. Delinquent Peer Associations | .32* | .35* | .26* | .04 | .12* | .29* | −.12* | 1.00 | |||||
| 9. Depressive Symptoms | .19* | .18* | .20* | .07 | .04 | .26* | −.23* | .27* | 1.00 | ||||
| 10. Female | −.01 | .04 | .06 | −.11* | .03 | −.05 | .11* | .03 | .13* | 1.00 | |||
| 11. Age(Wl) | −.00 | .11* | .04 | −.03 | .01 | .04 | .08 | .11* | −.06 | −.02 | 1.00 | ||
| 12. Per Capita Family Income (Wl) | −.06 | −.16* | −.08 | −.03 | −.09* | −.05 | .06 | −.13* | −.11* | −.04 | .00 | 1.00 | |
| 13. Remote Location (Wl) | .01 | .01 | −.12* | .02 | −.13* | .09* | −.13* | .02 | .06 | .01 | −.07 | .04 | 1.00 |
| Proportion Missingb | 0.14 | 0.05 | 0.17 | 0.03 | 0.03 | 0.07 | 0.07 | 0.07 | 0.06 | 0.00 | 0.00 | 0.03 | 0.00 |
| Full Sample Mean or Proportionb | 0.26 | 0.33 | 7.39 | 0.35 | 0.32 | 0.31 | 6.40 | 1.59 | 11.14 | 0.51 | 11.08 | 5.37 | 0.10 |
| Full Sample S.D.b | 4.36 | 2.05 | 0.74 | 7.89 | 0.83 | 3.96 | |||||||
| Imputed Sample Mean or Proportiona | 0.26 | 0.33 | 7.33 | 0.37 | 0.31 | 0.31 | 6.43 | 1.60 | 11.42 | 0.53 | 11.08 | 5.41 | 0.11 |
| 95% CI Lower Limit | 0.22 | 0.29 | 6.95 | 0.33 | 0.27 | 0.27 | 6.25 | 1.53 | 10.69 | 0.48 | 11.01 | 5.07 | 0.08 |
| 95% CI Upper Limit | 0.29 | 0.37 | 7.72 | 0.41 | 0.35 | 0.35 | 6.62 | 1.67 | 12.14 | 0.57 | 11.15 | 5.75 | 0.13 |
Note: W8 – Wave 8; W7 – Wave 6; W1 – Wave 1; S.D. – Standard Deviation; CI – Confidence Interval
N = 521; Estimates combined over 50 imputed datasets
N = 606
p < .05
There were several significant associations among the independent variables (see top of Table 1). Community violence exposure was positively associated with dating violence victimization, delinquent peer associations, and depressive symptoms, and negatively associated with remote location (p < .05). High caretaker victimization exposure was significantly and positively correlated with dating violence victimization and delinquent peer associations, and negatively correlated with per capita family income and remote location (p < .05). Adolescent dating violence victimization was positively correlated with delinquent peer associations, depressive symptoms, and remote location, and negatively associated with family warmth and support (p < .05). Delinquent peer associations and depressive symptoms were each negatively correlated with family warmth and support, and positively correlated with each other (p < .05). Depressive symptoms were positively associated with female gender, and negatively associated with income (p < .05).
Table 2 presents the means for continuous predictor variables and the proportions for categorical variables across SUD status at the last wave of the study. As hypothesized, the means for community violence exposure were significantly higher in the past year SUD group compared to the no past year SUD group (M = 9.08 and 6.74, respectively). In addition, the proportion of respondents with a caretaker who experienced high rates of victimization was lowest in the no past year SUD group, and highest in the past year SUD group. In bivariate analyses not shown, the only significant contrast was between the no caretaker victimization group and the high caretaker victimization group, with the latter having higher odds of past year SUD than the former. There were no significant differences between the moderate caretaker victimization group and the other two groups. The proportion of respondents who experienced dating violence victimization was higher in the past year SUD group than the no past year SUD group (0.49 vs. 0.25, respectively). For prior lifetime SUD diagnosis, family warmth and support, delinquent peer associations, and depressive symptoms means/proportions were significantly different across SUD status in the expected directions. None of the four demographic variables varied significantly across past year SUD status.
Table 2.
Estimated Proportions and Means of Predictor Variables Within Past Year SUD Status (N = 521)
| No Past Year SUD | Past Year SUD | |
|---|---|---|
| Proportion or Mean [95% CI] | Proportion or Mean [95% CI] | |
| Lifetime SUD (W6)* | ||
| No SUD | 0.76 [0.71, 0.80] | 0.41 [0.32,0.49] |
| Any SUD | 0.24 [0.20, 0.29] | 0.59 [0.51, 0.68] |
| Community Violence Exposure* | 6.74 [6.31, 7.17] | 9.08 [8.31, 9.85] |
| Caretaker Victimization* | ||
| No Caretaker Vic. Exposure | 0.36 [0.31, 0.40] | 0.21 [0.14,0.28] |
| Moderate Caretaker Vic. Exposure | 0.37 [0.32, 0.42] | 0.38 [0.30, 0.46] |
| High Caretaker Vic. Exposure | 0.28 [0.23, 0.32] | 0.41 [0.33,0.49] |
| Dating Violence Victimization* | ||
| No Dating Violence | 0.75 [0.71, 0.80] | 0.51 [0.42,0.60] |
| Any Dating Violence | 0.25 [0.20, 0.29] | 0.49 [0.40, 0.58] |
| Family Warmth and Support* | 6.61 [6.40,6.83] | 5.91 [5.54,6.27] |
| Delinquent Peer Associations* | 1.46 [1.38, 1.54] | 2.01 [1.90,2.11] |
| Depressive Symptoms* | 10.49 [9.69,11.28] | 14.10 [12.55, 15.66] |
| Gender | ||
| Male | 0.47 [0.42, 0.52] | 0.49 [0.40, 0.57] |
| Female | 0.53 [0.48, 0.58] | 0.51 [0.43,0.60] |
| Age(Wl) | 11.08 [11.00, 11.16] | 11.07 [10.94, 11.21] |
| Per Capita Family Income (Wl) | 5.55 [5.15, 5.95] | 5.02 [4.36, 5.68] |
| Remote Location (Wl) | ||
| Non-Remote Location | 0.89 [0.86, 0.92] | 0.89 [0.83, 0.94] |
| Remote Location | 0.11 [0.08,0.14] | 0.11 [0.06,0.17] |
Note: Estimates combined over 50 imputed datasets. SUD = substance use disorder; CI – confidence interval; W6 – Wave 6; W1 – Wave 1
means and proportions are significantly different (p < .05)
Table 3 presents the logistic regression models predicting past year SUD. In Model 1, all variables were entered simultaneously. As expected, current community violence exposure (OR = 1.09, p < .01), delinquent peer associations (OR = 2.05, p < .001), and meeting lifetime criteria for a SUD at Wave 6 (OR = 3.00, p < .001) increased the odds of a SUD, whereas family warmth and support was marginally associated with decreased odds (OR = 0.89, p = .06). Contrary to expectations, caretaker victimization exposure, dating violence victimization, depressive symptoms, and all demographic control variables were not associated with meeting criteria for a SUD.
Table 3.
Logistic Regression Models Predicting Past Year Substance Use Disorders (N = 521)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Community Violence Exposure | 1.09 [1.03,1.15]** | 1.01 [0.92,1.11] | 1.06 [1.00,1.13]* | 1.09 [1.03,1.15]** | 1.09 [1.03,1.16]** |
| Moderate Caretaker Victimizationa | 1.09 [0.61,1.97] | 1.08 [0.60,1.95] | 1.09 [0.60,1.98] | 0.98 [0.48,2.01] | 1.99 [0.28,14.34] |
| High Caretaker Victimizationa | 1.54 [0.85,2.80] | 1.57 [0.86,2.86] | 1.51 [0.83,2.76] | 0.88 [0.40,1.91] | 14.59 [2.00,106.32]** |
| Dating Violence Victimization | 1.54 [0.93,2.54]# | 1.51 [0.91,2.51] | 1.56 [0.94,2.60]# | 0.69 [0.22,2.16] | 1.59 [0.95,2.64]* |
| Family Warmth and Support | 0.89 [0.79,1.00] | 0.90 [0.80, 1.01]# | 0.88 [0.78, 1.00]* | 0.89 [0.79,1.00]# | 1.06 [0.84,1.33] |
| Delinquent Peer Associations | 2.05 [1.38, 3.04]*** | 2.09 [1.40,3.10]*** | 2.11 [1.41,3.16]*** | 2.07 [1.39,3.09]*** | 2.02 [1.36,3.00]** |
| Depressive Symptoms | 1.01 [0.98,1.04] | 1.01 [0.98,1.04] | 1.01 [0.98,1.04] | 1.01 [0.98,1.04] | 1.01 [0.98,1.04] |
| Lifetime SUD Wave 6 | 3.00 [1.86,4.86]*** | 3.14 [1.93,5.10]*** | 3.07 [1.89,5.01]*** | 2.95 [1.81,4.81]*** | 3.06 [1.87,4.99]*** |
| Female | 0.90 [0.57,1.43] | 0.84 [0.52 1.34] | 0.91 [0.57,1.44] | 0.92 [0.58,1.46] | 0.94 [0.59,1.49] |
| Age | 0.87 [0.66,1.15] | 0.84 [0.63,1.11] | 0.86 [0.65,1.14] | 0.85 [0.64,1.13] | 0.88 [0.68,1.17] |
| Per Capita Family Income | 1.03 [0.97,1.09] | 0.91 [0.79,1.04] | 1.04 [0.97,1.10] | 1.02 [0.96,1.09] | 1.03 [0.96 1.09] |
| Remote Location | 1.03 [0.49,2.15] | 1.13 [0.53,2.39] | 0.12 [0.02,1.02]# | 1.09 [0.52,2.30] | 1.05 [0.50,2.21] |
| Community Violence x Income | 1.02 [1.00,1.03]* | ||||
| Community Violence x Remote | 1.33 [1.03,1.72]* | ||||
| Mod. Caretaker Vic. x Dating Violence | 1.72 [0.45,6.63] | ||||
| High Caretaker Vic x Dating Violence | 4.69 [1.16,18,95]* | ||||
| Mod. Caretaker Vic x Warmth and Supp. | 0.91 [0.68,1.23 | ||||
| High Caretaker Vic x Warmth and Supp. | 0.70 [0.52,0.94]* | ||||
| F-Test | 6.69*** | 6.24*** | 6.25*** | 5.93*** | 5.96*** |
| Pseudo R2 | 0.19 | 0.20 | 0.20 | 0.20 | 0.20 |
Note: Analyses based on 50 imputed datasets and pooled estimates. OR – odds ratio; CI – confidence interval; SUD = substance use disorder
No caretaker victimization is the reference group
p < .10;
p < .05;
p < .01;
p < .001
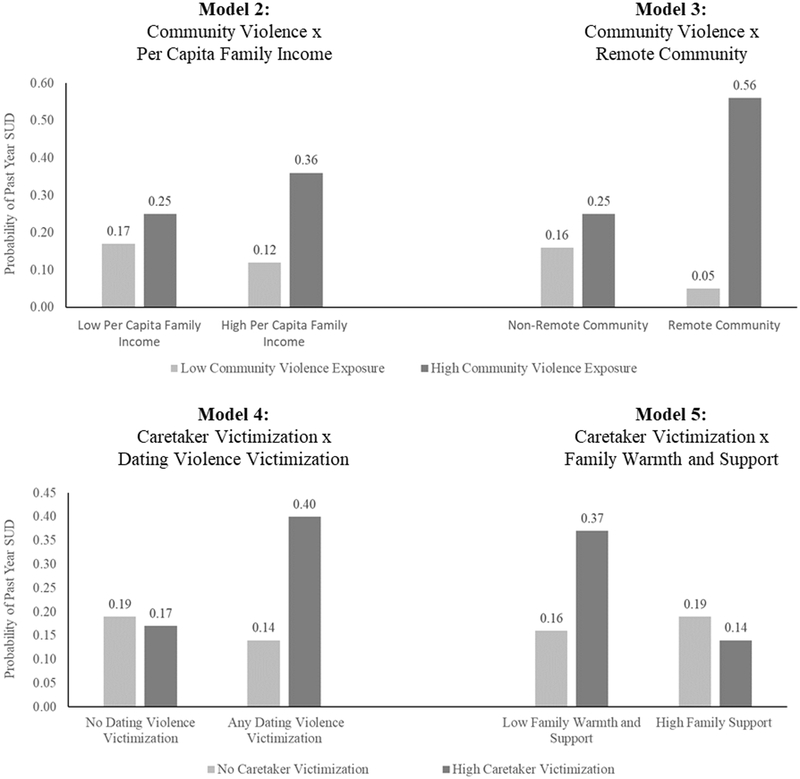
Twenty-eight interaction terms were tested separately to examine moderators of the association between exposure to violence and SUD risk, four of which were significant (see Table 3) – a number greater than expected by chance alone. Two variables moderated the effect of current community violence exposure. In model 2, the interaction term for community violence exposure x per capita family income was significant (OR = 1.02, p < .05). The top right portion of Figure 1 shows the predicted probabilities of past year SUD at high (1 S.D. above the mean) and low levels (1 S.D. below the mean) for both community violence exposure and per capita family income, with all other covariates fixed at their means. Contrary to expectations, the predicted probability of past year SUD was highest at high community violence exposure and high per capita family income.
Figure 1.
Predicted probabilities (i.e., marginal effects) of past year substance use disorder for significant interaction effects (see Table 3) holding all other covariates at their means. Top left: Community violence x per capita family income (see Table 3, Model 2); Top right: community violence x remote community (see Table 3, Model 3); Bottom left: Caretaker victimization x dating violence (see Table 3, Model 4); Bottom right: Caretaker victimization x Family Warmth and Support (see Table 3, Model 5). For continuous measures (i.e., community violence, per capita family income, and family warmth and support), low corresponds with one standard deviation below the mean and high corresponds with one standard deviation above the mean.
In model 3, the interaction term for community violence exposure x remote location was significant (OR = 1.33, p < .05). Post hoc analyses showed that the marginal effect of community violence exposure was significant across remote and non-remote levels, but, as hypothesized, the effect was stronger for those residing in a remote location. The top left portion of Figure 1 shows the predicted probabilities of past year SUD across non-remote and remote communities at high (1 S.D. above the mean) and low levels (1 S.D. below the mean) of community violence exposure, with all other covariates fixed at their means.
Two variables moderated the effect of caretaker victimization exposure on SUD risk. In model 4, the interaction term for caretaker victimization x dating violence victimization was significant at high levels of caretaker victimization exposure, compared to no caretaker victimization exposure (OR = 4.69, p < .05), but not at moderate levels of caretaker violence exposure. Post hoc analyses showed that the marginal effect of dating violence victimization was only significant, and positive in direction, for respondents whose caretakers experienced high victimization, compared to no or moderate victimization. The bottom left portion of Figure 1 shows the predicted probabilities by high caretaker victimization compared to no victimization exposure across dating violence victimization status, with all other covariates fixed at the mean.
In model 5, the interaction term for caretaker victimization exposure x family warmth and support was significant only at high levels of caretaker victimization (OR = 0.70, p < .05). Post hoc analyses showed that the marginal effect of warmth and support was only significant, and negative in direction, at high levels of caretaker victimization, and non-significant at no caretaker victimization. The bottom right portion of Figure 1 shows the predicted probabilities of no caretaker victimization and high caretaker victimization at high (1 S.D. above the mean) and low (1 S.D. below the mean) levels of family warmth and support. As hypothesized, the probability of past year SUD was low at high caretaker victimization and high levels of family warmth and support. The probability of past year SUD was highest at high caretaker victimization and low levels of family warmth and support. No other interaction terms were statistically significant.
Discussion
North American Indigenous groups experience high rates of adversity across multiple contexts, which are a residual consequence of historical processes stemming from European colonization (Evans-Campbell, 2008). Violence and problematic substance use are contemporary manifestations of this ongoing historical trauma (Evans-Campbell, 2008), and are directly and indirectly associated with the leading causes of mortality among Indigenous youth (Espy et al., 2014). Given the salience of both violence exposure and substance abuse among Indigenous groups, it is surprising that little research exists examining the relationship between the two, especially among community-based reservation/reserve samples of one cultural group. The purpose of the study was to examine moderators of the association between violence and victimization exposure and meeting criteria for a SUD. Drawing from a general ecological model derived from social stress theories (Foster & Brooks-Gunn, 2009), moderators of this association were analyzed across contexts.
As hypothesized, current perceptions of community violence exposure increased the odds of meeting criteria for an SUD, even after accounting for additional forms of violence exposure and other factors associated with SUD risk. Prior research among Indigenous adolescents focusing on neighborhood disorder indirectly supports this finding for general substance use frequency. The findings in the study add to literature by showing current perceptions of community violence as a correlate for substance abuse/dependence among reservation/reserve youth. Those who perceive their communities to be unsafe and dangerous may be constantly reminded of their vulnerability, which increases emotional and physiological arousal (Cooley-Quille et al., 2001). To reduce negative feelings emanating from this vulnerability and perceived powerlessness, youth may turn to alcohol and other substances to cope (Fowler et al., 2009).
This effect, however, was conditional upon remote location and per capita family income. As hypothesized, community violence exposure had a stronger effect on past year SUD risk for youth living in a remote location compared to a non-remote community. The reservation/reserve communities in this study are small and isolated from larger population centers. The rural context and isolation from other communities makes community violence exposure relevant because crime and victimization incidents are likely widely known by others and their effects likely spread beyond individuals who directly experience violence. Moreover, this underscores the need to examine community violence exposure within diverse geographical contexts, which has yet to receive adequate attention in the broader literature (Buka et al., 2001; Lynch, 2003). Contrary to expectations, per capita family income strengthened the association between current perceptions of community violence exposure and SUD risk, rather than the reverse. Income is inversely associated with stress exposure across contexts (Pearlin, 1989), and it may be that at low levels of income, additional exposures to stressors, particularly ones that are not directly experienced, have less of an impact. At higher levels of income, exposure to stressors may be perceived as more salient—some might consider it as threatening to perceived status relative to others (Schieman, et al., 2006)—which are consequently impactful on health behavior.
In addition, the results showed that adolescent participants whose caretakers experienced more frequent or multiple types of victimization throughout the study had higher odds of developing a SUD compared to those whose caretakers experienced no victimization or intermittent (moderate) victimization. This finding has important implications for substance use prevention and intervention and community well-being. Identifying caretakers who are at risk for repeated victimization experiences may help identify youth within those families who are at risk for developing substance use problems. Although this direct association was no longer significant once all other variables were added, it was significant conditional upon adolescent family warmth and support and dating violence victimization.
Familial contexts are an important source of cultural and personal resilience (Whitbeck et al., 2014a). Victimization experienced by caretakers, however, may undermine their ability to provide warmth and support to other family members (Burnette & Cannon, 2014), which in turn, may magnify the effect caretaker victimization has on adolescent substance use problems. Indeed, the results indicate that the relationship between caretaker victimization exposure and adolescent SUD odds was strongest when family warmth and support was weakest. Conversely, high family warmth and support appeared to buffer the association between high caretaker victimization exposure and adolescent SUD risk, which supports prior research (Tajima et al., 2011). Given the salience of extended family processes for Indigenous adolescent development (Whitbeck et al., 2014a), promoting strong family relationships across the early life course may have positive consequences extending beyond violence and victimization exposure and substance abuse.
About one-third of the adolescents in this sample experienced some form of physical dating violence victimization, which increased the odds of past year SUD (see Hautala et al. [2017] for prevalence comparisons). One explanation for this association may be that adolescents who experience dating violence victimization also tend to perpetrate dating violence (Hautala et al., 2017). Externalizing problems such as perpetrating aggressive behavior are strong risk factors for SUDs (Whitbeck et al., 2014b). Post hoc analyses (results available upon request), however, indicate that it is victimization only, compared to perpetration only or mutual dating violence, that has the most consistent association with SUD risk.
The only moderator of the association between dating violence victimization and SUD risk was caretaker victimization. As expected, the probability of meeting diagnostic criteria for a past year SUD was highest when adolescents experienced dating violence victimization and lived with a caretaker who experienced high levels of victimization. This finding aligns with a growing body of research which indicates that cumulative (poly)victimization experiences have a greater effect on substance use outcomes than no exposure to victimization or single victimization incidents (Wright et al., 2013). Alternative explanations may also account for this moderating relationship. Classic victimization models such as routine activities/lifestyles theory suggest that those most at risk for victimization tend to engage in risky behavior that places them at heightened risk (Laurtisen & Laub, 2007). Consequently, caretaker victimization exposure may be a proxy for risky family environments, which have been shown to amplify the effect of violence exposure on health outcomes (Hanson et al., 2006).
Contrary to expectations, delinquent peer associations, depressive symptoms, and gender did not moderate the association between violence exposure and meeting criteria for a SUD. Delinquent peer associations, however, had a direct positive association with SUD odds, which supports prior research among Indigenous youth (Whitbeck et al., 2014a). One reason for the lack of moderating effects may be that these factors by themselves do not necessarily modify the effect of stress on substance abuse. Instead, it may be a unique configuration of these variables that has the potential to modify the association between victimization and substance use risk (e.g., Agnew, 2006). Another reason may be that these non-significant direct and moderating effects are age-graded and have stronger, more consistent effects at earlier ages compared to late adolescence/early adulthood. Moreover, delinquent peer associations and depressive symptoms may be better conceptualized as mechanisms through which violence exposure operates to influence substance abuse risk (i.e., mediators), rather than factors that modify its association with various outcomes (i.e., moderators).
Limitations
Three limitations warrant attention. First, the data come from one Indigenous cultural group and may not be generalizable to others. Moreover, the data for this study come from a rural reservation/reserve-based sample. Consequently, the results may not be generalizable to adolescents of the sample cultural group who reside in urban areas. Second, only a few types of violence and victimization exposure were assessed in the study for both the caretakers and adolescents, which limits our understanding of the extent of violence exposure across ecological contexts, its association with substance abuse, and potential ecological moderators. Similarly, the measures lack contextual indicators (e.g, caretaker gender) that would allow for a more a nuanced understanding of violence exposure experiences and their relevance for understanding substance abuse risk. For example, it is not clear whether or not the adolescents in the sample were aware of their caretaker’s victimization, which may partially explain why only high frequency and/or multiple types of caretaker victimization was associated with SUD risk. Future research would benefit by examining a more expansive set of measures with contextual indicators (e.g., timing, duration, severity) that may help elucidate the association between two highly important health risks among Indigenous youth. Third, the relationship between violence exposure and substance use is likely reciprocal in nature. Although proper temporal ordering was established between the caretaker victimization and dating violence victimization measures and SUD risk, the measure for community violence exposure was measured concurrently with meeting criteria for an SUD.
Conclusion
Exposure to violence and victimization are prevalent risk factors for SUDs among Indigenous youth, which together, portend short- and long-term consequences for individual and collective health. The results of the current study have multiple implications for prevention, intervention, and policy. First, exposure to violence occurs across levels of social ecology and likely are causes, consequences, and amplifiers of one another (Hamby et al., 2018). Substance use policy should focus on poly-victimization, rather than single forms of violence, and their linkages within Indigenous communities. Second, strengthening positive familial relations may have important implications for buffering the negative effects of exposure to violence among caretakers. Third, the results help identify characteristics and factors across ecological contexts (e.g., remoteness, family income, violence among caretakers) that increase the odds that exposure to violence leads to SUD, which may serve as markers for targeted interventions. Realizing these policy goals requires additional community-based research with Indigenous youth and young adults, and understanding the general and unique contexts that give rise to these patterns.
Acknowledgements:
The authors wish to thank Les Whitbeck, Melissa Walls, Lisa Kort-Butler, Dan Hoyt, Kirk Dombrowski, Jonathan Brauer, and Community Advisory Boards for their feedback on earlier drafts of the manuscript.
Grant Funding:
This study is based on a chapter of the first author’s doctoral dissertation work, which was supported by a J.J. and Elenor S. Ogle Fellowship at the University of Nebraska. This research was also supported by the National Institute on Drug Abuse under grants R01DA13580 and T32DA037183, the National Institute of Mental Health under grant R01MH67281, and the National Institute on Alcohol Abuse and Alcoholism under grant R01AA020299. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Ackard D, & Neumark-Sztainer D (2002). Date violence and date rape among adolescents: Associations with disordered eating behaviors and psychological health. Child Abuse & Neglect, 26, 455–473. [DOI] [PubMed] [Google Scholar]
- Agnew Robert. 2006. Pressured into Crime: An overview of general strain theory. Los Angeles, CA: Roxbury. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.). Washington, DC: APA. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, D.C.: APA. [Google Scholar]
- Armenta B, Sittner Hartshorn K, Whitbeck L, Crawford D & Hoyt D (2014). A longitudinal examination of the measurement properties and predictive utility of the center for epidemiological studies depression scale among North American Indigenous adolescents. Psychological Assessment, 26, 1347–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd-Ball A, Manson S, Noonan C, & Beals J (2006). Traumatic events and alcohol use disorders among American Indian adolescents and young adults. Journal of Traumatic Stress, 19, 937–947. [DOI] [PubMed] [Google Scholar]
- Breiding M, Smith S, Basile K, Walters M, Chen J, & Merrick M (2014). Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—National intimate partner and sexual violence survey, United States. Surveillance Summaries, 63, 1–18. [PMC free article] [PubMed] [Google Scholar]
- Brockie T, Dana-Sacco G, Wallen G, Wilcox H, & Campbell J (2015). The relationship of adverse childhood experiences to PTSD, depression, poly-drug use and suicide attempt in reservation-based Native American adolescents and young adults. American Journal of Community Psychology, 55, 411–421. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U (1979). The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University. [Google Scholar]
- Buka S Stichick T, Birdthistle I, & Earls F (2001). Youth exposure to violence: Prevalence, risks, and consequences. American Journal of Orthopsychiatry, 71, 298–310. [DOI] [PubMed] [Google Scholar]
- Burnette C, & Cannon C (2014). It will always continue unless we can change something: Consequences of intimate partner violence for Indigenous women, children, and families. European Journal of Psychotraumatology, 5, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carliner H, Gary D, McLaughlin K, Keyes K (2017). Trauma exposure and externalizing disorders in adolescents: Results from the National Comorbidity Survey Adolescent Supplement. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 755–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger R, & Elder G (1994). Families in troubled times: Adapting to change in rural America. Hawthorn, NY: Aldine de Gruyter. [Google Scholar]
- Cooley-Quille M, Boyd R, Frantz E, & Walsh J (2001). Emotional and behavioral impact of exposure to community violence in inner-city adolescents. Journal of Clinical Child & Adolescent Psychology, 30, 199–206. [DOI] [PubMed] [Google Scholar]
- Espy D, Jim M, Cobb N, Bartholomew M, Beck T, Haverkamp D, & Plescia M (2014). Leading causes of death and all-cause mortality in American Indian and Alaska Natives. American Journal of Public Health, 104 (Suppl 3), S303–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Exner-Cortens D, Eckenrode J, & Rothman E (2013). Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics, 131, 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Campbell T (2008). Historical trauma in American Indian/Native Alaska communities. Journal of Interpersonal Violence, 23, 316–338. [DOI] [PubMed] [Google Scholar]
- Foshee V (1996). Gender difference in adolescent dating abuse prevalence, types and injuries. Health Education Research, 11, 275–286. [Google Scholar]
- Foster H, & Brooks-Gunn J (2009). Toward a stress process model of children’s exposure to physical family and community violence. Clinical Child and Family Psychology Review, 12, 71–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler P, Tompsett C, Braciszewski J, Jacques-Tiura A, & Baltes B (2009). Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Development and Psychopathology, 21, 227–259. [DOI] [PubMed] [Google Scholar]
- Friese B, Grube J, & Seninger S (2015). Drinking among Native American and white youths: The role of perceived neighborhood and school environment. Journal of Ethnicity in Substance Abuse, 14, 287–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamby S, Taylor E, Jones L, Mitchell K, Turner H, & Newlin C (2018). From poly- victimization to poly-strengths: Understanding the web of violence can transform research on youth violence and illuminate the path to prevention and resilience. Journal of Interpersonal Violence, 33, 719–739. [DOI] [PubMed] [Google Scholar]
- Hanson R, Self-Brown S, Fricker-Elhai A, Kilpatrick D, Saunders B, & Resnick H (2006). The relations between family environment and violence exposure among youth: Findings from the National Survey of Adolescents. Child Maltreatment, 11, 3–15. [DOI] [PubMed] [Google Scholar]
- Hautala D, Sittner Hartshorn K, Armenta B, & Whitbeck L (2017). Prevalence and correlates of physical dating violence among North American Indigenous adolescents. Youth & Society, 49, 295–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynie D, Farhat T, Brooks-Russell A, Wang J, Barbieri B, & Ianotti R (2013). Dating violence perpetration and victimization among U.S. adolescents: Prevalence, patterns, and associations with health complaints and substance use. Journal of Adolescent Health, 53, 194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt M, & Espelage D (2005). Social support as a moderator between dating violence victimization and depression/anxiety among African American and Caucasian adolescents. School Psychology Review, 34, 309–328. [Google Scholar]
- Hughes H, Parkinson D, & Vargo M (1989). Witnessing spouse abuse and experiencing physical abuse: A “double whammy”? Journal of Family Violence, 4, 197–209. [Google Scholar]
- Klein D (2014). MIMRGNS: Stata module to run margins after mi estimate [computer software]. Boston, MA: Boston College of Economics. [Google Scholar]
- Lauritsen J, & Laub J (2007). Understanding the link between victimization and offending: New reflections on an old idea. Crime Prevention Studies, 22, 55–75. [Google Scholar]
- Lloyd D, & Turner RJ (2008). Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug and Alcohol Dependence, 93, 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch M (2003). Consequences of children’s exposure to community violence. Clinical Child and Family Psychology Review, 6, 265–274. [DOI] [PubMed] [Google Scholar]
- Manson S, Beals J, Klein S, Croy C, & AI-SUPERPFP Team. (2005). Social epidemiology of trauma among 2 American Indian reservation populations. American Journal of Public Health, 95, 851–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalls AM, Mullis R, & Mullis A (2009). American Indian youths’ perceptions of their environment and their reports of depressive symptoms and alcohol/marijuana use. Adolescence, 44, 965–978. [PubMed] [Google Scholar]
- Ozer E, Lavi I, Douglas L, & Wolf J (2017). Protective factors for youth exposed to violence in their communities: A review of family, school, and community moderators. Journal of Clinical Child & Adolescent Psychology, 46, 353–378. [DOI] [PubMed] [Google Scholar]
- Pearlin L (1989). The sociological study of stress. Journal of Health and Social Behavior, 30, 241–256. [PubMed] [Google Scholar]
- Perrault S (2011). Violent victimization of Aboriginal people in the Canadian provinces, 2009. Ottawa, ON: Statistics Canada. [Google Scholar]
- Radloff L (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Schieman S, Pearlin L, & Meersman S (2006). Neighborhood disadvantage and anger among older adults: Social comparisons as effect modifiers. Journal of Health and Social Behavior, 47, 156–172. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan M, & Schwab-Stone M (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP. [Google Scholar]
- Tajima E, Herrenkohl T, Moylan C, & Derr A (2011). Moderating the effects of childhood exposure to intimate partner violence: The roles of parenting characteristics and adolescent peer support. Journal of Research on Adolescence, 21, 376–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Hippel P (2007). Regression with missing Ys: An improved strategy for analyzing multiply imputed data. Sociological Methodology, 37, 83–117. [Google Scholar]
- Whitbeck L, Sittner Hartshorn K, & Walls M (2014a). Indigenous adolescent development: Psychological, social and historical contexts. New York, NY: Routledge. [Google Scholar]
- Whitbeck L, Sittner Hartshorn K, Crawford D, Walls M, Gentzler K, & Hoyt D (2014b). Mental and substance use disorders from early adolescence to young adulthood among Indigenous young people: Final diagnostic results from an 8-year panel study. Social Pyschiatry and Psychiatric Epidemiology, 49, 961–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White I, Royston P, & Wood A (2011). Multiple imputation using chained equations: Issues and guidance. Statistics in Medicine, 30, 377–399. [DOI] [PubMed] [Google Scholar]
- Wright E, Fagan A, Pinchevsky G (2013). The effects of exposure to violence and victimization across life domains on adolescent substance use. Child Abuse & Neglect, 37, 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]