Abstract
We encountered a patient with autosomal dominant polycystic kidney disease (ADPKD) complicated with emphysematous polycystic renal infection (EPRI). A 44-year-old woman visited our hospital for a fever, appetite loss, and gross hematuria. Because the patient was suffering from end-stage renal disease (ESRD), she was immediately hospitalized for hemodialysis. Multiple emphysematous infected cysts were noted in the right kidney, and antibiotic therapy and three rounds of cystic drainage were performed. However, the patient did not respond to treatment. Therefore, laparoscopic right nephrectomy was performed. ADPKD with comorbid EPRI is unresponsive to conservative treatment, and we believe that nephrectomy should be considered.
Keywords: autosomal dominant polycystic kidney disease (ADPKD), cystic infection, emphysematous pyelonephritis, emphysematous polycystic renal infection, nephrectomy
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is a genetic disease in which proliferating multiple cysts in the kidneys and liver can develop. In ADPKD, cystic infection is a common complication. However, ADPKD patients develop emphysematous infections in rare cases and may require urgent nephrectomy. In general, most emphysematous infections are emphysematous pyelonephritis (EPN). Gas production in the renal parenchyma and around the kidney is noted. It becomes severe in some cases, and the mortality rate is high (13.5%) (1). A number of EPN cases associated with ADPKD have been reported (2-12). In addition, cases of emphysematous polycystic renal infection (EPRI) associated with comorbid emphysematous infections of ADPKD, in which gas production within the cysts is observed, have been reported (13-17).
We herein report a case of ADPKD with a comorbid EPRI that required surgical treatment.
Case Report
A 44-year-old woman who had a family history of ADPKD (mother) first visited our hospital in 2008 to undergo a detailed examination for back pain and gross hematuria. Abdominal ultrasonography showed multiple bilateral renal cysts, and the patient was diagnosed with ADPKD based on these findings and her family history. In 2013, her serum creatinine level was 1.8 mg/dL. Thereafter, she discontinued hospital visits of her own accord. In July 2016, she visited our hospital due to a fever, loss of appetite, and gross hematuria. Laboratory findings showed an elevated white blood cell count (WBC: 25,680/μL), strongly positive C-reactive protein (CRP: 12.3 mg/dL) and advanced renal failure (blood urea nitrogen 218 mg/dL, serum creatinine 17.0 mg/dL). The patient was immediately admitted for a further examination and treatment for end-stage renal disease (ESRD) and suspected cystic infection.
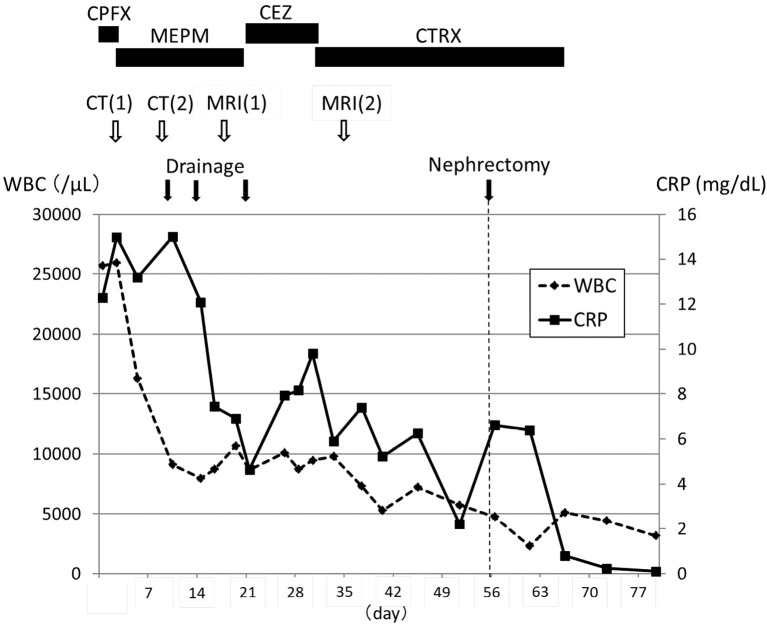
The clinical course after admission is shown in Fig. 1. On admission, the patient was highly obese with a body mass index (BMI) of 34.2 kg/m2. However, her HbA1c was 5.4%, and the patient had no history of diabetes mellitus. Her blood pressure was 112/81 mmHg, heart beat 101/min, and body temperature 36℃. The palpebral conjunctiva was pale, and the abdomen was distended, but there was no tenderness, back pain, or knocking pain. Mild edema was noted in her lower legs.
Figure 1.
The clinical course after admission. The vertical dotted line indicates the day of nephrectomy. CPFX: ciprofloxacin, MEPM: meropenem, CEZ: cefazolin, CTRX: ceftriaxone, CT: computed tomography, MRI: magnetic resonance imaging, WBCs: white blood cells, CRP: C-reactive protein
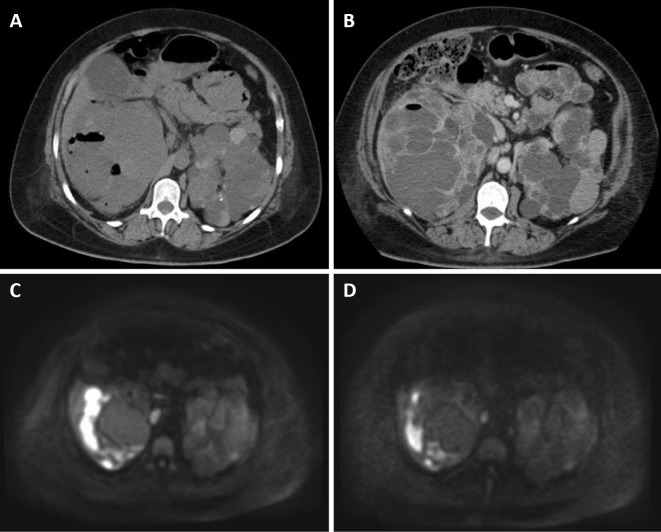
Since the laboratory findings depicted a state of ESRD with severe azotemia, hyperkalemia, and metabolic acidosis on admission, hemodialysis was emergently started. Ciprofloxacin was started because of the suspicion of cystic infection. On the third hospital day, abdominal computed tomography (CT) showed that the cysts on the upper pole of the right kidney were poorly defined and gaseous with opacity in the surrounding fat tissue and peritoneal thickening (Fig. 2A). The patient was diagnosed with EPRI. Therefore, ciprofloxacin was changed to meropenem. On the ninth hospital day, the cysts were less gaseous, but wall thickening and elevated adipose concentration were indicated on abdominal contrast-enhanced CT, suggesting that some infected cysts remained (Fig. 2B). Echography-guided drainage was performed. On the 13th hospital day, CT-guided drainage was performed. On the 15th hospital day, meropenem was changed to cefazolin, because drug eruption appeared that might have been caused by meropenem and because Escherichia coli detected in the drained fluid showed antimicrobial susceptibility to cefazolin. Since magnetic resonance imaging (MRI) on the 18th hospital day showed that infected cysts yet remained (Fig. 2C), CT-guided drainage was again performed on the 21st hospital day. Drainage was performed three times in total.
Figure 2.
Abdominal computed tomography (CT) and magnetic resonance imaging (MRI). A: Abdominal CT on the 3rd hospital day, showing gas within the cyst in the right kidney. The cysts on the upper pole of the right kidney are poorly defined and gaseous with opacity in the surrounding fat tissue and peritoneal thickening, diagnosed as cystic infection. B: Abdominal contrast-enhanced CT on the 9th hospital day, still showing gas within the cyst in the right kidney. The cysts became less gaseous after the administration of antibiotics, but infected cysts remained. C: Abdominal MRI (diffusion-weighted image) on the 18th hospital day, showing high intensities in the right kidney. D: Abdominal MRI (diffusion-weighted image) on the 35th hospital day, still showing high intensities in the right kidney.
There were no positive bacteria on any cultures, including those for blood, urine, and fluid from drainage. The patient continued to suffer from a fever of 37.5℃ or higher, and her CRP levels increased again. Cefazolin was changed to ceftriaxone. MRI on the 35th hospital day showed that there infected cysts yet remained compared to MRI on the 18th hospital day (Fig. 2D). We therefore decided that the patient could not be treated with antimicrobial agents and drainage alone and planned nephrectomy. However, the patient hesitated to undergo surgery, so we continued antibiotics with ceftriaxone. Although the CRP levels decreased to 2 mg/dL, the patient continued to suffer from a fever of 37℃ or higher. Therefore, with her informed consent, we performed laparoscopic right nephrectomy on the 56th hospital day. After surgery, the fever immediately subsided, and both the WBC and CRP normalized. The patient was discharged on the 88th hospital day.
Discussion
Generally, emphysematous infection in the kidney in which gas production is noted in the renal parenchyma is EPN (1). Regarding the patient background in EPN, the incidence is higher in women (male-to-female ratio =1:6) and more prevalent in Asian countries. It has been reported that 95% of EPN patients are diabetic, 25-40% suffer from comorbid urinary tract obstruction, and neurogenic bladder is also considered a risk factor. Elevated tissue glucose levels, insufficient blood flow, and an impaired immune function have been reported as etiological factors, while E. coli and Klebsiella pneumoniae, among others, have been reported as causative bacteria (18). Regarding treatment, Ubee et al. reported that, although conservative treatment with antimicrobial agents or percutaneous catheter drainage (PCD) is effective in most cases, some cases may require nephrectomy (1).
In ADPKD, 11 cases of EPN have been reported (2-12) (Table 1A). In addition, five cases of EPRI, in which gas production is noted within the cysts, have also been reported as a comorbid emphysematous infection of ADPKD (13-17) (Table 1B). EPN presents with imaging findings of gas within the parenchyma, while EPRI presents with imaging findings of gas within cysts. Table 2 shows a comparison between comorbid EPN and EPRI of ADPKD. In both cases, the incidence is lower among women than with common EPN. Furthermore, most EPN patients are diabetic. Increased tissue glucose levels are believed to play a role in the mechanism of onset. However, a characteristic of EPRI is that the patients had no comorbid diabetes, and all were suffering from ESRD, with only one side of the kidneys affected in all patients. In addition to an impaired immune function due to ESRD, cysts with high intracystic glucose levels may be an etiological factor (19). More specifically, similar to EPN, the causative bacteria may be drawn to areas with high tissue glucose levels, and areas with high glucose levels within the cysts may become infected as well. Regarding the treatment of EPRI, three out of five cases underwent urgent or elective nephrectomy, and the mortality was high, with two of the five cases dying (Table 1B). The patient in the present study also underwent treatment with a number of antimicrobial agents and PCD but was unresponsive to treatment. However, the patient's condition improved after nephrectomy.
Table 1.
| (A) Case reports of emphysematous pyelonephritis (EPN) | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| age | sex | DM | renal function | laterality | gas within the cyst | gas within the parenchyma | bacteria | drainage | urgent nephrectomy | nephrectomy | outcome | reference | ||||||||||||||
| 1 | 47 | F | unknown | Cr 4.5 mg/dL | right | - | + | E. coli | - | - | + | recover | 2 | |||||||||||||
| 2 | 51 | M | + | HD | bilateral | - | + | E. coli | - | + | + | recover | 3 | |||||||||||||
| 3 | 50 | F | + | unknown | bilateral | unknown | unknown | unknown | - | - | - | recover | 4 | |||||||||||||
| 4 | 64 | M | + | Cr 5.9 mg/dL | bilateral | - | + | E. coli | - | - | - | recover | 5 | |||||||||||||
| 5 | 44 | M | + | Cr 2.9 mg/dL | left | - | + | unknown | + | - | - | recover | 6 | |||||||||||||
| 6 | 51 | F | + | Cr 3.1 mg/dL | right | - | + | E. coli | - | + | + | recover | 7 | |||||||||||||
| 7 | 76 | F | + | PD | right | - | + | E. coli | - | - | + | recover | 8 | |||||||||||||
| 8 | 42 | M | + | post transplant | bilateral | - | + | E. coli | - | - | + | recover | 9 | |||||||||||||
| 9 | 43 | M | - | HD | bilateral | + | + | E. coli | - | - | + | recover | 10 | |||||||||||||
| 10 | 51 | M | - | HD | right | + | + | E. coli | - | - | + | recover | 11 | |||||||||||||
| 11 | 57 | M | + | Cr 1.3 mg/dL | bilateral | + | + | E. coli | + | - | - | recover | 12 | |||||||||||||
| (B) Case reports of emphysematous polycystic renal infection (EPRI) | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| age | sex | DM | renal function | laterality | gas within the cysts | gas within the parenchyma | bacteria | drainage | urgent nephrectomy | nephrectomy | outcome | reference | ||||||||||||||
| 1 | 65 | F | unknown | post transplant | right | + | - | clostridium perfringens | - | + | + | recover | 13 | |||||||||||||
| 2 | 40 | M | unknown | HD | right | + | - | unknown | - | + | + | death | 14 | |||||||||||||
| 3 | 57 | M | - | ESRD | right | + | - | E. coli | - | + | + | death | 15 | |||||||||||||
| 4 | 62 | F | - | HD | left | + | - | E. coli | + | - | - | recover | 16 | |||||||||||||
| 5 | 61 | M | - | PD | left | + | - | klebsiella pneumoniae | - | - | - | recover | 17 | |||||||||||||
| 6 | 44 | F | - | ESRD | right | + | - | E. coli | + | - | + | recover | present study | |||||||||||||
DM: Diabetes mellitus, HD: Hemodialysis, ESRD: End stage renal disease, PD: Peritoneal Dialysis, E. coli: Escherichia coli
Table 2.
Comparison between EPN and EPRI Complicated with ADPKD.
| EPN | EPRI | |||
|---|---|---|---|---|
| mean age (year) | 52.4 | 54.8 | ||
| female | 4/11 (36%) | 3/6 (50%) | ||
| DM | 8/10 (80%) | 0/4 (0%) | ||
| ESRD | 5/11 (45%) | 6/6 (100%) | ||
| bilateral | 6/11 (55%) | 0/6 (0%) | ||
| gas in the cysts | 3/10 (30%) | 6/6 (100%) | ||
| gas in the parenchyma | 10/10 (100%) | 0/6 (0%) | ||
| E. coli | 9/11 (82%) | 3/6 (50%) | ||
| drainage | 2/11 (18%) | 2/6 (33%) | ||
| urgent nephrectomy | 2/11 (18%) | 3/6 (50%) | ||
| nephrectomy | 7/11 (64%) | 4/6 (67%) | ||
| death | 0/11 (0%) | 2/6 (33%) |
EPN: emphysematous pyelonephritis, DM: Diabetes mellitus, EPRI: emphysematous polycystic renal infection, DM: Diabetes mellitus, ESRD: End stage renal disease, E. coli: Escherichia coli
In conclusion, ADPKD with comorbid EPRI is resistant to conservative treatment compared to common EPN, and we believe nephrectomy should be considered as soon as conservative treatment is judged not to be effective.
All procedures performed in the patient study were in accordance with the 1964 Declaration of Helsinki and its later amendments or with comparable ethical standards.
Informed consent was obtained from the patient.
Author's disclosure of potential Conflicts of Interest (COI).
Hitoshi Kataoka: Employment, Otsuka Pharmaceutical, Chugai Pharmaceutical, Kyowa Hakko Kirin, MSD and JMS. Ken Tsuchiya: Honoraria, Otsuka Pharmaceutical; Travel fees, Otsuka Pharmaceutical. Toshio Mochizuki: Employment, Otsuka Pharmaceutical, Chugai Pharmaceutical, Kyowa Hakko Kirin, MSD and JMS; Honoraria, Otsuka Pharmaceutical; Travel fees, Otsuka Pharmaceutical.
Financial Support
This report was supported in part by a Grant-in-Aid for Intractable Renal Diseases Research, Research on rare and intractable diseases; and Health and Labor Sciences Research Grants from the Ministry of Health, Labor and Welfare of Japan.
References
- 1. Ubee SS, McGlynn L, Fordham M. Emphysematous pyelonephritis. BJU Int 107: 1474-1478, 2011. [DOI] [PubMed] [Google Scholar]
- 2. Chou YH, Tiu CM, Chen TW, Chen KK, Chang T. Emphysematous pyelonephritis in a polycystic kidney. Demonstration by ultrasound and computed tomography. J Ultrasound Med 9: 355-357, 1990. [DOI] [PubMed] [Google Scholar]
- 3. Schenkman E, Auriemma P. Bilateral emphysematous pyelonephritis with autosomal dominant polycystic kidney disease. J Urol 159: 1633-1634, 1998. [DOI] [PubMed] [Google Scholar]
- 4. Shimizu H, Hariu K, Kamiyama Y, et al. Bilateral emphysematous pyelonephritis with autosomal-dominant polycystic kidney disease successfully treated by conservative method. Urol Int 63: 252-254, 1999. [DOI] [PubMed] [Google Scholar]
- 5. Arun N, Hussain A, Kapoor MM, Abul F. Bilateral emphysematous pyelonephritis and emphysematous cystitis with autosomal-dominant polycystic kidney disease: is conservative management justified? Med Princ Pract 16: 155-157, 2007. [DOI] [PubMed] [Google Scholar]
- 6. Medagama UA, Aluvihare AP, Jayasinghe MW, Rosairo S, Fernando DJ. A gas forming renal abscess in a person with diabetes mellitus and adult polycystic kidney disease. Diabetes Res Clin Pract 75: 372-373, 2007. [DOI] [PubMed] [Google Scholar]
- 7. Azzini AM, Sette P, Castellano G, Dorizzi RM. A rare association of emphysematous pyelonephritis with unrecognized diabetes and polycystic kidney. Indian J Nephrol 19: 20-22, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gama KS, Perez CN, Simo VE, Serna MR. [Emphysematous pyelonephritis and radical nephrectomy in hepatorenal polycystosis]. Nefrologia : publicacion oficial de la Sociedad Espanola Nefrologia 30: 140-141, 2010(in Spanish, Abstract in English). [DOI] [PubMed] [Google Scholar]
- 9. Wong EK, Hartley R, Main J. Successful management of bilateral emphysematous pyelonephritis in end-stage polycystic kidneys: bilateral native nephrectomies and preservation of functioning renal transplant. NDT Plus 4: 452-453, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lakshminarayana G, Mathew A, Rajesh R, Kurien G, Unni VN. Bilateral emphysematous pyelonephritis in autosomal dominant polycystic kidney disease. Indian J Nephrol 22: 136-138, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yamanouchi M, Ubara Y, Takaichi K. Emphysematous cyst infection in autosomal dominant polycystic kidney disease. Clin Exp Nephrol 16: 505-506, 2012. [DOI] [PubMed] [Google Scholar]
- 12. Jaisuresh K, Bavaharan R. Successful conservative treatment of bilateral emphysematous pyelonephritis in autosomal dominant polycystic kidney disease. Indian J Nephrol 23: 229-231, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Van Zijl PS, Chai TC. Gas-forming infection from Clostridium perfringens in a renal cyst of a patient with autosomal dominant polycystic kidney disease. Urology 63: 1178-1179, 2004. [DOI] [PubMed] [Google Scholar]
- 14. Erkoc R, Sayarlioglu H, Ceylan K, Dogan E, Kara PS. Gas-forming infection in a renal cyst of a patient with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant 21: 555-556, 2006. [DOI] [PubMed] [Google Scholar]
- 15. Sooraj YS, Nainan GK, Joseph F, Thara P. Emphysematous polycystic renal infection. Indian J Nephrol 20: 205-206, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kim H, Park HC, Lee S, et al. Successfully treated Escherichia coli-induced emphysematous cyst infection with combination of intravenous antibiotics and intracystic antibiotics irrigation in a patient with autosomal dominant polycystic kidney disease. J Korean Med Sci 28: 955-958, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nagaraju SP, Gupta A, McCormick BB, Khandelwal A. Emphysematous polycystic infection in a patient on peritoneal dialysis. Saudi J Kidney Dis Transpl 25: 837-839, 2014. [DOI] [PubMed] [Google Scholar]
- 18. Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med 160: 797-805, 2000. [DOI] [PubMed] [Google Scholar]
- 19. Huseman R, Grady A, Welling D, Grantham J. Macropuncture study of polycystic disease in adult human kidneys. Kidney Int 18: 375-385, 1980. [DOI] [PubMed] [Google Scholar]