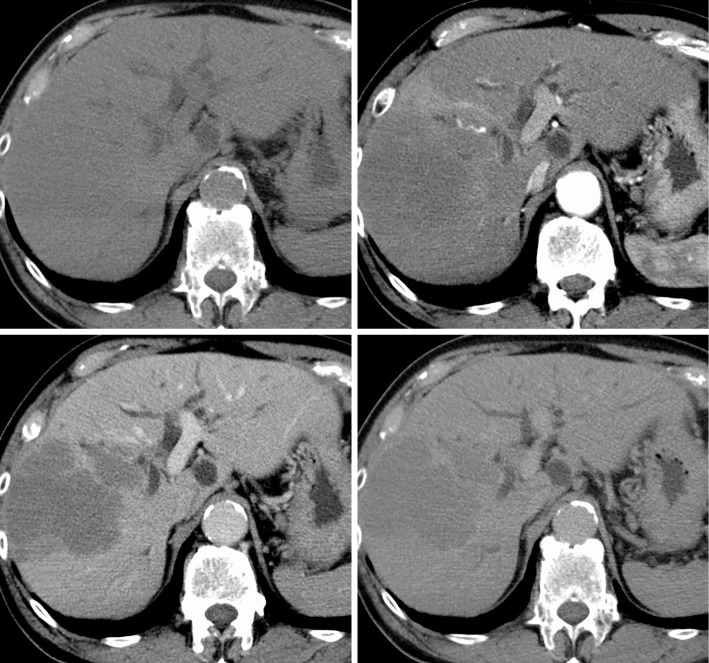
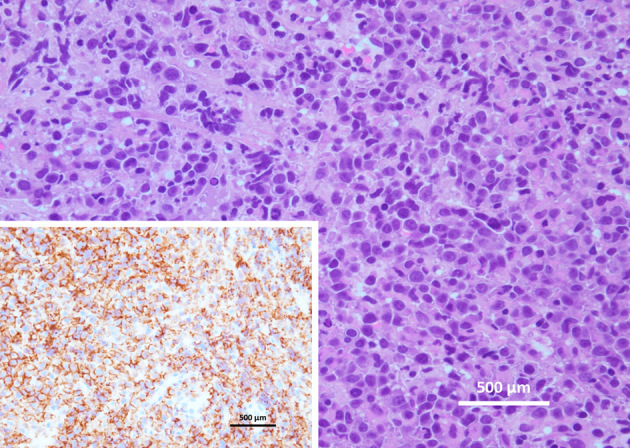
A 78-year-old man with obstructive jaundice and osteolytic left scapular tumor was referred to our hospital. Serum carcinoembryonic antigen (CEA), CA19-9, and soluble interleukin 2 receptor were 3.6 IU/L (reference range: 0-5), 128 IU/L (reference range: 0-37), and 2,940 IU/L (reference range: 145-519), respectively. Dynamic contrast-enhanced computed tomography showed a low-density mass in the right anterior segment of the liver and dilation of the left intrahepatic bile duct (Picture 1). We performed a transpapillary biliary biopsy and drainage (Picture 2). Histologically, the tumor was composed of cleaved lymphocytes. A liver needle biopsy confirmed diffuse large B-cell lymphoma (DLBCL) that was positive for CD20 (Picture 3), BCL6, MUM1, and MYC/BCL2 and negative for CD5, CD10, and TdT. The Ki-67 index was approximately 90%. 18F-Fluorodeoxyglucose-position emission tomography showed no abnormal uptake except for in the liver [maximum standardized uptake value (SUV max) 28] and left scapular tumor (SUV max 3.3) after palliative radiotherapy for bone metastasis. The findings of a bone marrow biopsy were normal. We diagnosed the tumor as primary hepatic DLBCL (NOS, ABC, MYC/BCL2 double expressor). The patient was treated with combination chemotherapy, including pirarubicin, cyclophosphamide, vincristine, and prednisolone following rituximab. Chemotherapy resulted in a partial response via a reduction in the overall tumor size by more than 50% (89.8×58.7 mm to 42×28 mm). The patient was then transferred to another hospital in order to receive further treatments. Primary hepatic lymphoma (PHL) complicated with obstructive jaundice is rare and can mimic a diagnosis of intrahepatic cholangiocellular carcinoma (1). PHL should be considered in the differential diagnosis of patients presenting with biliary obstruction.
Picture 1.
Picture 2.

Picture 3.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
The authors would like to thank Dr. Yutaka Akiyama (Pathology Division, Faculty of Medicine, University of Miyazaki Hospital) and Dr. Kotaro Arita (Department of Hematology, Faculty of Medicine, University of Toyama) for their clinical advice.
References
- 1. Abe H, Kamimura K, Kawai H, et al. Diagnostic imaging of hepatic lymphoma. Clin Res Hepatol Gastroenterol 39: 435-442, 2015. [DOI] [PubMed] [Google Scholar]