Abstract
Western populations are becoming increasingly sedentary and the incidence of nonalcoholic fatty liver disease (NAFLD) is increasing and becoming one of the most common causes of liver disease worldwide. Also, NAFLD is considered one the new emerging risk factors for development of tumors of the gastro-intestinal tract, particularly hepatocellular carcinoma (HCC). Visceral obesity is an important risk factor for the onset of NAFLD. An accumulation of ectopic fat, including visceral obesity and fatty liver leads to a dysfunction of the adipose tissue with impaired production of adipocytokines which, in turn, favor an increase in pro-inflammatory cytokines. In this review, we discuss how the obesity-related chronic state of low-grade inflammation and the presence of NAFLD lead to the emergence of a microenvironment favorable to the development of cancer.
Keywords: NAFLD, adipocytokines, inflammation, obesity, cancer
Introduction
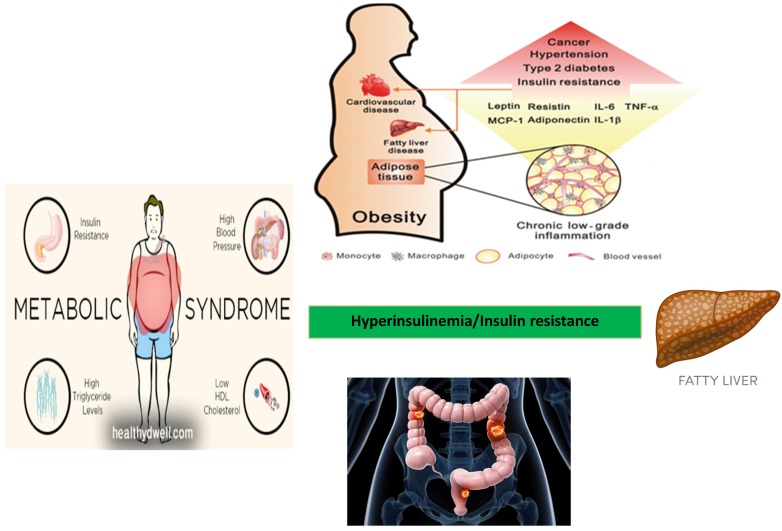
Fatty liver (triglyceride content > 5% of organ weight) is the most common liver disease found in the obese. It is classified as non-alcoholic fatty liver disease (NAFLD) if independent from the alcohol consumption. In addition, NAFLD is strongly associated with features of the metabolic syndrome, including obesity, insulin resistance, type 2 diabetes (DM2) and dyslipidemia 1,2. NAFLD represents a new emerging risk factors for the onset of extra-hepatic tumors, particularly in the development of tumors of the gastro-intestinal tract 3,4. Risk factors associated with the development of NAFLD include bad eating habits associated with a sedentary lifestyle. Therefore, patients with NAFLD are strongly recommended to follow a regimen including dietary restrictions associated with physical activity. Bad eating habits and sedentary lifestyle are increasing in Western Countries and NAFLD is accordingly becoming one of the most common causes of liver disease worldwide 5,6. The prevalence of NAFLD is 15-30% of the general population and it is close to 50-90% in obese subjects. This prevalence correlates with the obesity rate. In fact, hepatic steatosis is found in 65% of subjects with grade I-II obesity (BMI = 30-39.9 kg/m2) and in 85% of patients with grade III obesity (BMI = 40-59 kg/m2). The prevalence of NAFLD and its inflammatory progression into non-alcoholic steatohepatitis (NASH) varies according to age, gender and degree of obesity 7. Since NAFLD represents a spectrum of disease and histological patterns, a staging encompassing both the histological findings and the prognostic aspects has been proposed (Table 1). In the stages of NAFLD progression, classes I and II are considered substantially benign and reversible if the patients are adequately treated. Despite considered a benign condition in most cases, NAFLD can progress towards cirrhosis and liver failure (class III and IV) in a discrete percentage of subjects over a period of about two decades 8. It is worth mentioning that a significant proportion of patients develop NAFLD despite having a normal body mass index (BMI) and few metabolic syndrome features. Patients with NAFLD are generally asymptomatic and NAFLD is often diagnosed during an occasional ultrasound evaluation of the abdomen. Indeed, several cases of NAFLD are associated with other metabolic disorders, including hypertriglyceridaemia, hypercholesterolemia, and hypertension, thus configuring the clinical pattern of the so-called "metabolic syndrome" 9. Visceral obesity is an important risk factor for the onset of NAFLD. An accumulation of ectopic fat, including visceral obesity and fatty liver leads to dysfunction of adipose tissue with impaired production of adipocytokines. This in turn will favor an increase in pro-inflammatory cytokines such as TNF-α (Tumor Necrosis Factor-alfa) and a decrease in anti-inflammatory adipokines such as adiponectin 10. Thus, the prevalence of NAFLD increases with the increase of the body mass index (BMI). NAFLD is currently considered the liver manifestation of the metabolic syndrome (MS) which represents, as shown by numerous studies, a condition that increases the risk of cancer, particularly for the gastrointestinal tract 11,12. It is becoming clear that insulin resistance associated with the metabolic syndrome and the consequent activation of the inflammatory cascade jointly with the development of NAFLD may act as promoting factors for cancer development 13,14. Thus, insulin resistance and metabolic syndrome represent common risk factors for both NAFLD and cancer (Figure 1).
Table 1.
Histological classification of NAFLD
| Class | Histological framework |
|---|---|
| Class I | Simple fatty liver disease |
| Class II | Fatty liver with lobular inflammation |
| Class III | Fatty liver with lobular inflammation and balloniform hepatocytes |
| Class IV | Fatty liver with lobular inflammation, balloniform hepatocytes, Mallory bodies and fibrosis (stage 1-4) |
Figure 1.
Relationship between metabolic syndrome, NAFLD, and development of colorectal adenoma and carcinoma.
Natural history of NAFLD
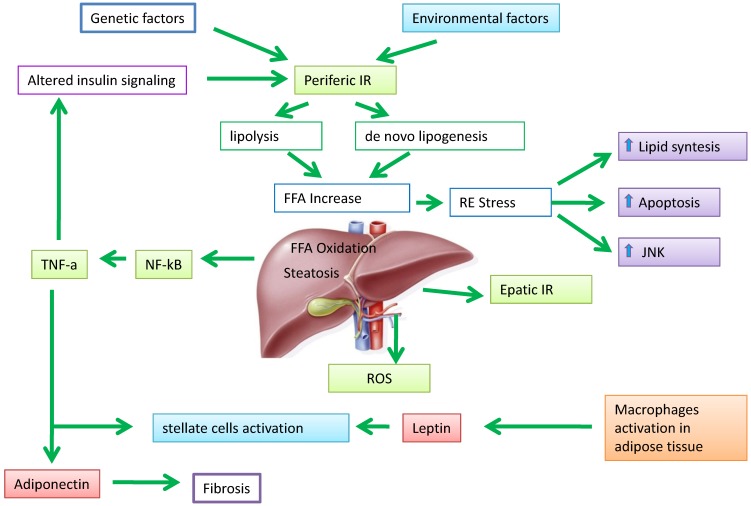
Hepatic steatosis develops when the amount of fatty acids that accumulate in liver cells exceeds the consumption. This imbalance between inputs and outputs, with an intrahepatic deposit of triglycerides, can occur as a result of four mechanisms: i) increased inflow of fatty acids (FA) from the peripheral circulation; ii) increased hepatic synthesis of FA (de novo lipogenesis); iii) reduced intrahepatic and peripheral FA oxidation; IV) reduced triglycerides release in the circulation through the VLDL. All these mechanisms contribute to the pathogenesis of hepatic steatosis supported by metabolic alterations 15,16. The actors involved in this process are numerous, but the primary role is played by the adipose tissue expansion and particularly by hypertrophic adipocyte and insulin resistance generated at hepatic and muscular level 17. Elevated serum levels of free fatty acids (FFAs) and cholesterol, insulin resistance, and adipocyte proliferation are generally present in obesity associated with bad dietary habits and bad lifestyle. Insulin resistance worsens adipocyte function and induces hepatic de novo lipogenesis. In addition, insulin resistance promotes the release of proinflammatory adipokines including interleukin (IL)-6, IL-1β and tumor necrosis factor (TNF)-α. These adipokines can in turn worsen the state of insulin resistance 18,19. This condition results in an increased of hepatic flux of FFAs and leads to accumulation of triglycerides (TGs), mitochondrial dysfunction, reactive oxygen species (ROS) production, and eventually hepatic inflammation and fibrogenesis 20. Recent findings support the evidence that increased FFA levels leads to an accumulation of certain types of lipid derivatives including ceramides, which inhibit the action of insulin 21. Ceramides can be considered mediators of insulin resistance and lipotoxicity. Elevated plasma levels of ceramide are detectable in obese subjects and may contribute, for example, to insulin resistance through activation of TNF-α and other inflammatory mediators 22. This corroborates the role of ceramide in the pathogenesis of NAFLD with a direct pro-inflammatory effects. In addition, the development of liver dysfunction, hepatic insulin resistance and steatosis in rodents are associated with increased levels of ceramide in both liver and peripheral blood 23. Additionally, adiponectin lowers the hepatic content of ceramide by improving the blood glucose homeostasis through its receptor-associated ceramidase activity 24. Ectopic fat deposition is “lipotoxic” and has been linked to the severity of insulin resistance. Holland and colleagues demonstrated that ceramide metabolism influences the insulin-sensitizing effects of adiponectin on the liver which is its primary target tissue 25. Adiponectin displays anti-lipotoxic effects that are thought to protect tissues (i.e. the liver and muscle) from the accumulation of triglycerides. Decreased adiponectin levels may impair ceramide clearance by facilitating ceramide accumulation within the tissue 26. An increase in hepatic ceramides is associated to elevated levels of plasma ceramides in obese patients and may promote insulin resistance at level of skeletal muscle. Taken together, these data indicate that insulin resistance represents one of the key factors in the pathogenesis of NAFLD (Figure 2).
Figure 2.
The pathogenesis of NAFLD. Peripheral insulin resistance (IR) promotes increased production of free fatty acids (FFA) direct in the liver, resulting in an imbalance between oxidation/divestiture and uptake/synthesis of FFA, and then steatosis liver. The fabric fat secretes adipokines such as leptin, able to adjust the adipocyte metabolism and numerous insulin-mediated processes. Adiponectin plays a role in anti-inflammatory and anti-steatotic; its secretion It is in part regulated by TNF-α under the control of NF-kB.
Adipose tissue in the pathogenesis of NAFLD
In patients with NAFLD, the total amount of triglyceride pool in the liver originates from three sources: i) adipose tissue (60%); ii) remnant chylomicrons (15%) mostly from dietary fats; iii) hepatic lipogenesis or de novo lipogenesis (approximately 25%). Regarding the aliquot from adipocytes, 75-80% of triglyceride originates from the subcutaneous adipose tissue whereas the remaining portion is derived from the visceral adipose tissue and conveyed to the liver via the portal vein (the portal hypothesis) 27,28. According to this hypothesis, the omental fat, which drains directly into the portal vein, contributes significantly to the flow of FFA to the liver as a consequence of the high lipolytic activity of the fat present therein. From the pathogenic point of view, the portal hypothesis is intriguing for several reason. For example, the visceral adipose tissue has a secretory profile different from that of subcutaneous adipose tissue characterized by abundant release of inflammatory cytokines. These cytokines are drained directly from the portal vein and poured out in the liver before reaching any other organ 29. Therefore, the anatomical contiguity places the liver as the first barrier to the visceral adipose tissue. In physiological conditions, the liver is already subject to a high metabolic activity from which derives a large release of free radicals. In the presence of fatty liver, the oxidative metabolism increases further and even more if hyperglycemia and insulin resistance are present. The abnormal release of free radicals can be compensated until saturation is reached by the antioxidant barrier 30. When the protective systems are exhausted, ROSs begin to oxidize hepatocytes and other hepatic cells, which in turn activate protective mechanisms by triggering the inflammatory response 31. This results in an increased expression of TNF-α, IL-1, IL-6 and other inflammatory cytokines which contribute to acceleration of the damage and the more rapid progression of the disease 32,33.
NAFLD and cancer: the adipocytokine network
Based on their effect on NAFLD, adipokines are generally divided into adipokines promoting the onset of NAFLD and adipokines inhibiting the development of NAFLD. A crosstalk between these two groups of adipokines can result either in a beneficial or harmful effect on NAFLD progression 34,35. However, the ultimate effect is generally temporary because both endogenous factors (e.g. genetic components) and exogenous factors (e.g. eating habits and lifestyles) determine continuous changes in the metabolic environment followed by dynamic changes of the adipokine profile with different effects on NAFLD evolution. For example, an antagonist relationship exists between adiponectin (with inhibitory action) and TNF-α (with promoting action) showing opposite effects on insulin resistance and NAFLD 36,37. Under normal conditions, there is an equilibrium between the two adipokine groups. This homeostatic equilibrium can be altered by hypertrophy or hyperplasia of adipocytes, and can lead to a chronic state of inflammation, insulin resistance and development of NAFLD 38. The expansion of adipose tissue, independently of other concomitant factors, deprives patients with NAFLD of the anti-inflammatory and antifibrotic effects of adiponectin, effects which are inversely related to total adiposity 39. Adiponectin is a potent cytokine exerting insulin sensitizing, anti-inflammatory and anti-steatotic activity in hepatocytes through increasing oxidation of free fatty acids and decreasing gluconeogenesis, FFA flow and de novo lipogenesis 40,41. In addition, adiponectin protects hepatocytes from apoptosis in the NAFLD-associated hepatic inflammatory microenvironment 42. TNF-α is another important pro-inflammatory cytokine in NAFLD which promotes insulin resistance 43. The excessive release of TNF-α from both the hypertrophic adipocytes and Kuppfer cells is one of the early events of hepatic damage. In fact, TNF-α stimulates the production of other chemo-attractant cytokines in the hepatocytes, which in turn recruit inflammatory cells 44,45. High levels of TNF-α and low levels of adiponectin are favorable conditions for the development of insulin resistance and NAFLD 46. These two adipokines involved in the pathogenesis of NAFLD mutually inhibit the synthesis and activity of each other by targeting metabolic equilibrium 47. However, these adipokines are thought to be involved in the link between obesity, NAFLD and development of both intra and extra hepatic tumors 48-50. In particular, adiponectin exerts antitumor activity by activating the AMP protein kinase (AMPK), an inhibitor of tumor cell growth that stimulates the caspase signaling pathway leading to apoptosis of endothelial cells 51,52. In addition, adiponectin exerts its anti-tumor action by inhibiting TNF-α, involved in both tumor proliferation and angiogenesis 53,54. Accordingly, insulin is becoming a relevant factor in the regulation of cell proliferation, apoptosis and tumor angiogenesis 55,56. Leptin is another adipocitokine involved in the onset of NAFLD 57. Leptin plays a dual role in NAFLD. On one hand, it seems to have a protective role for hepatic steatosis, especially in the early stages of the disease. On the other hand, it could act as an inflammatory and fibrinogenic factor as the disease progresses. As visceral adipose tissue increases, leptin levels concomitantly increase. This should limit the expansion of fat mass in order to avoid the formation of insulin resistance. In this sense, leptin should exert an anti-steatotic effect on the hepatocytes 58,61. If adipose tissue expands, a state of leptin resistance occurs. Accordingly, leptin is no longer able to compensate insulin resistance and the progression of steatosis 62. In this context, leptin may exert non-beneficial effects by acting as a fibrinogenic and pro-inflammatory adipokine. Leptin is considered an adipocytokine acting as molecular link between obesity and cancer 63-65. Low levels of adiponectin and high levels of leptin are associated with the processes of mitogenesis, tumor growth and cell motility when adipose tissue dysfunction occurs. Furthermore, an increase in leptin stimulates the release of pro-inflammatory cytokines such as TNF-α and IL-6, which in turn give rise to an inflamed microenvironment which favors tumor development and up-regulation of angiogenesis promoting factors (i.e. VEGF and HIF-1α) 66-68.
Conclusion
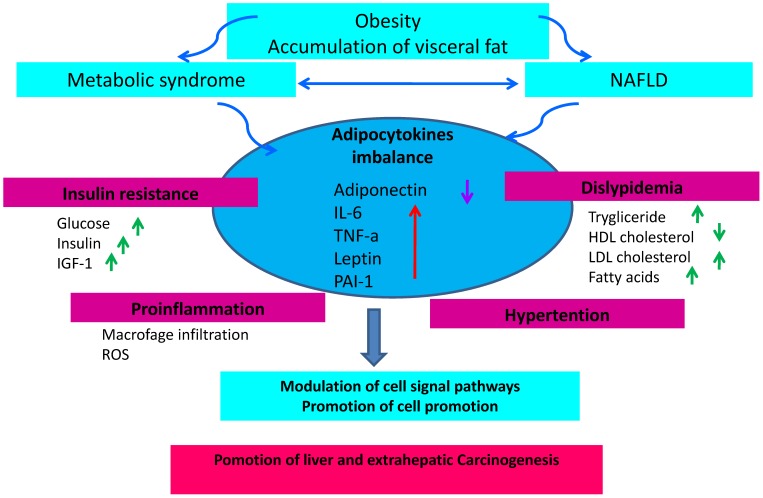
The incidence of NAFLD is increasing in accordance with the increasing prevalence of metabolic syndrome and obesity. In addition, NAFLD and predisposition to cancer is still matter of debate. Consequently, the question arises as to whether the increasing NAFLD incidence accounts for the increase of certain type of cancer (particularly liver and colon cancer). NAFLD is frequently associated with visceral obesity, diabetes and dyslipidemia, and it is related to clinical and biological markers of insulin resistance. Insulin resistance associated with the metabolic syndrome and the consequent activation of the inflammatory cascade underlying the development of NAFLD represents a favorable background for cancer development (Fig. 3). The prevention of an excessive increase of adipose tissue is therefore important to avoid the promotion of a pro-inflammatory activity sustained by an adverse adipokine profile predisposing to an increased risk of cancer. In conclusion, in overweight or obese patients with NAFLD, a program of cancer prevention aimed at quenching the inflammatory cascade and improve insulin sensitivity should be mandatory. It is therefore advisable for these subjects to adopt correct lifestyles including healthy eating habits and avoid sedentariness.
Figure 3.
The state of chronic low-grade inflammation due to obesity and the presence of NAFLD leads to the emergence of a micro-environment favorable to the development of cancer and the onset of insulin resistance due to activation of the axis that regulates the insulin growth factor-1 IGF-1 and insulin resulting in hyperinsulinemia. Through its proliferative and anti-apoptotic effects, this process can increase mutations that promote carcinogenesis.
References
- 1.Dietrich P, Hellerbrand C. Non-alcoholic fatty liver disease, obesity and the metabolic syndrome. Best Pract Res Clin Gastroenterol. 2014;28(4):637–653. doi: 10.1016/j.bpg.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Milić S, Lulić D, Štimac D. Non-alcoholic fatty liver disease and obesity: biochemical, metabolic and clinical presentations. World J Gastroenterol. 2014;20(28):9330–9337. doi: 10.3748/wjg.v20.i28.9330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim GA, Lee HC, Choe J, Association between non-alcoholic fatty liver disease and cancer incidence rate. J Hepatol; 2017. S0168-8278(17): 32294-32298. [DOI] [PubMed] [Google Scholar]
- 4.Derra A, Bator M, Menżyk T, Kukla M. Underrated enemy - from nonalcoholic fatty liver disease to cancers of the gastrointestinal tract. Clin Exp Hepatol. 2018;4(2):55–71. doi: 10.5114/ceh.2018.75955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aller R, Fernández-Rodríguez C, Lo Iacono O. et al. Management of non-alcoholic fatty liver disease (NAFLD). Clinical practice guideline. Gastroenterol Hepatol. 2018;41(5):328–349. doi: 10.1016/j.gastrohep.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Kwak MS, Kim D. Non-alcoholic fatty liver disease and lifestyle modifications, focusing on physical activity. Korean J Intern Med. 2018;33(1):64–74. doi: 10.3904/kjim.2017.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ipsen DH, Lykkesfeldt J, Tveden-Nyborg P. Molecular mechanisms of hepatic lipid accumulation in non-alcoholic fatty liver disease. Cell Mol Life Sci; 2018. doi: 10.1007 / s00018-018-2860-6. Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koo SH. Nonalcoholic fatty liver disease: molecular mechanisms for the hepatic steatosis. Clin Mol Hepatol. 2013;19(3):210–215. doi: 10.3350/cmh.2013.19.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2(11):901–910. doi: 10.1016/S2213-8587(14)70032-4. [DOI] [PubMed] [Google Scholar]
- 10.Hohenester S, Christiansen S, Nagel JM. et al. Lifestyle intervention for morbid obesity: effects on liver steatosis, inflammation and fibrosis. Am J Physiol Gastrointest Liver Physiol. 2018. 2018;315(3):G329–G338. doi: 10.1152/ajpgi.00044.2018. [DOI] [PubMed] [Google Scholar]
- 12.Brown JC, Harhay MO, Harhay MN. Nonalcoholic fatty liver disease and mortality among cancer survivors. Cancer Epidemiol. 2017;48:104–109. doi: 10.1016/j.canep.2017.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanna C, Rosso C, Marietti M, Non-Alcoholic Fatty Liver Disease and Extra-Hepatic Cancers. Int J Mol Sci; 2016. p. 17. (5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Del Campo JA, Gallego P, Grande L. Role of inflammatory response in liver diseases: Therapeutic strategies. World J Hepatol. 2018;10(1):1–7. doi: 10.4254/wjh.v10.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Z, Yu R, Xiong Y. et al. A vicious circle between insulin resistance and inflammation in nonalcoholic fatty liver disease. Lipids Health Dis. 2017;16(1):203. doi: 10.1186/s12944-017-0572-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Satapathy SK, Sanyal AJ. Epidemiology and Natural History of Nonalcoholic Fatty Liver Disease. Semin Liver Dis. 2015;35(3):221–235. doi: 10.1055/s-0035-1562943. [DOI] [PubMed] [Google Scholar]
- 17.Marengo A, Jouness RI, Bugianesi E. Progression and Natural History of Nonalcoholic Fatty Liver Disease in Adults. Clin Liver Dis. 2016;20(2):313–324. doi: 10.1016/j.cld.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 18.Itoh H, Kanayama N. Developmental Origins of Nonalcoholic Fatty Liver Disease (NAFLD) Adv Exp Med Biol. 2018;1012:29–39. doi: 10.1007/978-981-10-5526-3_4. [DOI] [PubMed] [Google Scholar]
- 19.Altamirano-Barrera A, Barranco-Fragoso B, Méndez-Sánchez N. Management strategies for liver fibrosis. Ann Hepatol. 2017;16(1):48–56. doi: 10.5604/16652681.1226814. [DOI] [PubMed] [Google Scholar]
- 20.Lambertucci F, Arboatti A, Sedlmeier MG. et al. Disruption of tumor necrosis factor alpha receptor 1 signaling accelerates NAFLD progression in mice upon a high-fat diet. J Nutr Biochem. 2018;58:17–27. doi: 10.1016/j.jnutbio.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Tsochatzis EA, Papatheodoridis GV, Archimandritis AJ. Adipokines in nonalcoholic steatohepatitis: from pathogenesis to implications in diagnosis and therapy. Mediators Inflamm. 2009;2009:831670. doi: 10.1155/2009/831670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Apostolopoulou M, Gordillo R, Koliaki C. et al. Specific Hepatic Sphingolipids Relate to Insulin Resistance, Oxidative Stress, and Inflammation in Nonalcoholic Steatohepatitis. Diabetes Care. 2018;41(6):1235–1243. doi: 10.2337/dc17-1318. [DOI] [PubMed] [Google Scholar]
- 23.Ordoñez M, Presa N, Trueba M. et al. Implication of Ceramide Kinase in Adipogenesis. Mediators Inflamm. 2017;2017:9374563. doi: 10.1155/2017/9374563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watt MJ, Barnett AC, Bruce CR. et al. Regulation of plasma ceramide levels with fatty acid oversupply: evidence that the liver detects and secretes de novo synthesised ceramide. Diabetologia. 2012;55(10):2741–2746. doi: 10.1007/s00125-012-2649-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holland WL, Miller RA, Wang ZV. et al. Receptor-mediated activation of ceramidase activity initiates the pleiotropic actions of adiponectin. Nat Med. 2011;17(1):55–63. doi: 10.1038/nm.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holland WL, Xia JY, Johnson JA. et al. Inducible overexpression of adiponectin receptors highlight the roles of adiponectin-induced ceramidase signaling in lipid and glucose homeostasis. Mol Metab. 2017;6(3):267–275. doi: 10.1016/j.molmet.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reibe-Pal S, Febbraio MA. Adiponectin serenades ceramidase to improve metabolism. Mol Metab. 2017;6(3):233–235. doi: 10.1016/j.molmet.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karim MF, Al-Mahtab M, Rahman S. et al. Non-alcoholic Fatty Liver Disease (NAFLD) A Review. Mymensingh Med J. 2015;24(4):873–880. [PubMed] [Google Scholar]
- 29.Fuchs CD, Claudel T, Trauner M. Role of metabolic lipases and lipolytic metabolites in the pathogenesis of NAFLD. Trends Endocrinol Metab. 2014;25(11):576–585. doi: 10.1016/j.tem.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 30.Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1S):S47–64. doi: 10.1016/j.jhep.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 31.Masarone M, Rosato V, Dallio M. et al. Role of Oxidative Stress in Pathophysiology of Nonalcoholic Fatty Liver Disease. Oxid Med Cell Longev. 2018;2018:9547613. doi: 10.1155/2018/9547613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perumpail BJ, Khan MA, Yoo ER. et al. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol. 2017;23(47):8263–8276. doi: 10.3748/wjg.v23.i47.8263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abenavoli L, Peta V. Role of adipokines and cytokines in non-alcoholic fatty liver disease. Rev Recent Clin Trials. 2014;9(3):134–140. doi: 10.2174/1574887109666141216102458. [DOI] [PubMed] [Google Scholar]
- 34.Stojsavljević S, Gomerčić Palčić M, Virović Jukić L. et al. Adipokines and proinflammatory cytokines, the key mediators in the pathogenesis of nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20(48):18070–18091. doi: 10.3748/wjg.v20.i48.18070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Polyzos SA, Kountouras J, Mantzoros CS. Adipokines in nonalcoholic fatty liver disease. Metabolism. 2016;65(8):1062–1079. doi: 10.1016/j.metabol.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Jarrar MH, Baranova A, Collantes R. et al. Adipokines and cytokines in non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2008;27(5):412–421. doi: 10.1111/j.1365-2036.2007.03586.x. [DOI] [PubMed] [Google Scholar]
- 37.Rabe K, Lehrke M, Parhofer KG, Broedl UC. Adipokines and insulin resistance. Mol Med. 2008;14(11-12):741–751. doi: 10.2119/2008-00058.Rabe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Antuna-Puente B, Feve B, Fellahi S. et al. Adipokines: the missing link between insulin resistance and obesity. Diabetes Metab. 2008;34(1):2–11. doi: 10.1016/j.diabet.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 39.Divella R, De Luca R, Abbate I. et al. Obesity and cancer: the role of adipose tissue and adipo-cytokines-induced chronic inflammation. J Cancer. 2016;7(15):2346–2359. doi: 10.7150/jca.16884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neuman MG, Cohen LB, Nanau RM. Biomarkers in nonalcoholic fatty liver disease. Can J Gastroenterol Hepatol. 2014;28(11):607–618. doi: 10.1155/2014/757929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ma H, You GP, Cui F. et al. Effects of a low-fat diet on the hepatic expression of adiponectin and its receptors in rats with NAFLD. Ann Hepatol. 2015;14(1):108–117. [PubMed] [Google Scholar]
- 42.Buechler C, Wanninger J, Neumeier M. Adiponectin, a key adipokine in obesity related liver diseases. World J Gastroenterol. 2011;17(23):2801–2811. doi: 10.3748/wjg.v17.i23.2801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Finelli C, Tarantino G. What is the role of adiponectin in obesity related non-alcoholic fatty liver disease? World J Gastroenterol. 2013;19(6):802–812. doi: 10.3748/wjg.v19.i6.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nieto-Vazquez I, Fernández-Veledo S, Krämer DK. et al. Insulin resistance associated to obesity: the link TNF-alpha. Arch Physiol Biochem. 2008;114(3):183–194. doi: 10.1080/13813450802181047. [DOI] [PubMed] [Google Scholar]
- 45.Sato A, Nakashima H, Nakashima M, Involvement of the TNF and FasL produced by CD11b Kupffer cells/macrophages in CCl4-induced acute hepatic injury. PLoS One; 2014. p. 9. (3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Su L, Li N, Tang H. et al. Kupffer cell-derived TNF-α promotes hepatocytes to produce CXCL1 and mobilize neutrophils in response to necrotic cells. Cell Death Dis. 2018;9(3):323. doi: 10.1038/s41419-018-0377-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen Z, Yu R, Xiong Y. et al. A vicious circle between insulin resistance and inflammation in nonalcoholic fatty liver disease. Lipids Health Dis. 2017;16(1):203. doi: 10.1186/s12944-017-0572-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adolph TE, Grander C, Grabherr F, Adipokines and Non-Alcoholic Fatty Liver Disease: Multiple Interactions. Int J Mol Sci; 2017. p. 18. (8). pii: E1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Duan XF, Tang P, Li Q. et al. Obesity, adipokines and hepatocellular carcinoma. Int J Cancer. 2013;133(8):1776–1783. doi: 10.1002/ijc.28105. [DOI] [PubMed] [Google Scholar]
- 50.Booth A, Magnuson A, Fouts J. et al. Adipose tissue, obesity and adipokines: role in cancer promotion. Horm Mol Biol Clin Investig. 2015;21(1):57–74. doi: 10.1515/hmbci-2014-0037. [DOI] [PubMed] [Google Scholar]
- 51.Derra A, Bator M, Menżyk T. et al. Underrated enemy - from nonalcoholic fatty liver disease to cancers of the gastrointestinal tract. Clin Exp Hepatol. 2018;4(2):55–71. doi: 10.5114/ceh.2018.75955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nagaraju GP, Aliya S, Alese OB. Role of adiponectin in obesity related gastrointestinal carcinogenesis. Cytokine Growth Factor Rev. 2015;26(1):83–93. doi: 10.1016/j.cytogfr.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 53.Zhang L, Wen K, Han X. et al. Adiponectin mediates antiproliferative and apoptotic responses in endometrial carcinoma by the AdipoRs/AMPK pathway. Gynecol Oncol. 2015;137(2):311–320. doi: 10.1016/j.ygyno.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 54.Hajri T, Tao H, Wattacheril J. et al. Regulation of adiponectin production by insulin: interactions with tumor necrosis factor-α and interleukin-6. American Journal of Physiology - Endocrinology And Metabolism. 2011;300(2):E350–E360. doi: 10.1152/ajpendo.00307.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huang M, Chen Z, Xu D. et al. Adiponectin inhibits proliferation and induces apoptosis in colorectal cancer HCT116 cells. Chinese Journal of Cellular and Molecular Immunology. 2018;34(3):253–259. [PubMed] [Google Scholar]
- 56.Djiogue S, Nwabo Kamdje AH, Vecchio L. et al. Insulin resistance and cancer: the role of insulin and IGFs. Endocr Relat Cancer. 2013;20(1):R1–R17. doi: 10.1530/ERC-12-0324. [DOI] [PubMed] [Google Scholar]
- 57.Cao Y. Angiogenesis and vascular functions in modulation of obesity, adipose metabolism, and insulin sensitivity. Cell Metab. 2013;18(4):478–489. doi: 10.1016/j.cmet.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 58.Polyzos SA, Aronis KN, Kountouras J. et al. Circulating leptin in non-alcoholic fatty liver disease: A systematic review and meta-analysis. Diabetologia. 2016;59:30–43. doi: 10.1007/s00125-015-3769-3. [DOI] [PubMed] [Google Scholar]
- 59.Boutari C, Tziomalos K, Athyros VG. The adipokines in the pathogenesis and treatment of nonalcoholic fatty liver disease. Hippokratia. 2016;20(4):259–263. [PMC free article] [PubMed] [Google Scholar]
- 60.Boutari C, Perakakis N, Mantzoros CS. Association of Adipokines with Development and Progression of Nonalcoholic Fatty Liver Disease. Endocrinol Metab (Seoul) 2018;33(1):33–43. doi: 10.3803/EnM.2018.33.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.de Luis DA, Perez Castrillon JL, Duenas A. Leptin and obesity. Minerva Med. 2009;100:229–236. [PubMed] [Google Scholar]
- 62.Asrih M, Veyrat-Durebex C, Poher AL. et al. Leptin as a Potential Regulator of FGF21. Cell Physiol Biochem. 2016;38(3):1218–1225. doi: 10.1159/000443070. [DOI] [PubMed] [Google Scholar]
- 63.Zhang L, Song H, Ge Y, Temporal relationship between diet-induced steatosis and onset of insulin/leptin resistance in male Wistar rats. PLoS One; 2015. p. 10. (2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mullen M, Gonzalez-Perez RR. Leptin-Induced JAK/STAT Signaling and Cancer Growth. Vaccines (Basel); 2016. p. 4. (3) pii: E26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ray A, Cleary MP. The potential role of leptin in tumor invasion and metastasis. Cytokine Growth Factor Rev. 2017;38:80–97. doi: 10.1016/j.cytogfr.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ackerman SE, Blackburn OA, Marchildon F. et al. Insights into the Link Between Obesity and Cancer. Curr Obes Rep. 2017;6(2):195–203. doi: 10.1007/s13679-017-0263-x. [DOI] [PubMed] [Google Scholar]
- 67.Park J, Morley TS, Kim M. et al. Obesity and cancer—mechanisms underlying tumour progression and recurrence. Nat Rev Endocrinol. 2014;10(8):455–465. doi: 10.1038/nrendo.2014.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Iyengar NM, Gucalp A, Dannenberg AJ. et al. Obesity and Cancer Mechanisms: Tumor Microenvironment and Inflammation. J Clin Oncol. 2016;34(35):4270–4276. doi: 10.1200/JCO.2016.67.4283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Himbert C, Delphan M, Scherer D. et al. Signals from the Adipose Microenvironment and the Obesity-Cancer Link-A Systematic Review. Cancer Prev Res (Phila) 2017;10(9):494–506. doi: 10.1158/1940-6207.CAPR-16-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]